Abstract
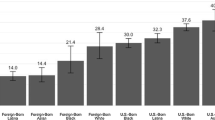
Research has demonstrated that the human papillomavirus (HPV) vaccine is a safe and effective way to decrease HPV-related cervical cancers; however, the vaccination rate in the USA is suboptimal. The current study examined racial and ethnic disparities in HPV vaccination among a nationally representative sample, including Native Hawaiian and Pacific Islanders (NHPI). This study also investigated the associations between nativity and vaccination, and sex differences between race/ethnicity and vaccination and nativity and vaccination. A cross-sectional study was conducted with a sample of adults aged 18–26 years drawn from the 2014 NHPI National Health Interview Survey (n = 2590) and the general 2014 National Health Interview Survey (n = 36,697). Log-binomial models were fitted to examine differences in vaccination. There was a statistically significant racial/ethnic difference in HPV vaccination (p = 0.003). More women than men were vaccinated (41.8% vs. 10.1%) (p < 0.001). There was a significant difference in HPV vaccination based on nativity: 27.4% of adults aged 18 to 26 years who were born in the USA and 27.7% born in a US territory received the HPV vaccine compared with 14.3% among those not born in the USA or a US territory (p < 0.001). The association of HPV vaccination with nativity and race/ethnicity differed by sex and showed several nuanced differences. Overall, the prevalence of HPV vaccination was low. The study’s findings demonstrate the need for public health strategies to increase vaccination rates among all populations, with the critical need to identify strategies that are effective for men, racial/ethnic minorities, and immigrant women born outside the USA.
Similar content being viewed by others
References
Grulich AE, Jin F, Conway EL, Stein AN, Hocking J. Cancers attributable to human papillomavirus infection. Sex Health. 2010;7(3):244–52.
Rahman M, Islam M, Berenson AB. Differences in HPV immunization levels among young adults in various regions of the United States. J Community Health. 2015;40(3):404–8.
Van Hilten LG. The HPV vaccine 10 years on: where are we now? 2016; Available from: https://www.elsevier.com/connect/the-hpv-vaccine-10-years-on. Accessed 7 May 2020.
Reasons to get vaccinated against HPV. 2020; Available from: https://www.cdc.gov/hpv/parents/vaccine/six-reasons.html. Accessed 7 May 2020.
HPV-associated cervical cancer rates by race and ethnicity. 2019; Available from: https://www.cdc.gov/cancer/hpv/statistics/cervical.htm. Accessed 7 May 2020.
HPV vaccine information for young women. 2016 2019–01-11T08:34:16Z/; Available from: https://www.cdc.gov/std/hpv/stdfact-hpv-vaccine-young-women.htm. Accessed 7 May 2020.
Gelman A, Miller E, Schwarz EB, Akers AY, Jeong K, Borrero S. Racial disparities in human papillomavirus vaccination: does access matter? J Adolesc Health. 2013;53(6):756–62.
Walker TY, Elam-Evans LD, Yankey D, Markowitz LE, Williams CL, Fredua B, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years-United States, 2018. MMWR Morb Mortal Wkly Rep. 2019;68(33):718–23.
Boersma P, Black LI. Human papillomavirus vaccination among adults aged 18-26, 2013-2018. 2020, National Center for Health Statistics. p. 1-8.
Williams WW, Lu PJ, O’Halloran A, Kim DK, Grohskopf LA, Pilishvili T, et al. Surveillance of vaccination coverage among adult populations-United States, 2015. MMWR Surveill Summ. 2017;66(11):1–28.
Vaccination coverage among adults in the United States. 2017 2018; Available from: https://www.cdc.gov/vaccines/imz-managers/coverage/adultvaxview/pubs-resources/NHIS-2017.html#box3. Accessed 7 May 2020.
Agénor M, Pérez AE, Peitzmeier SM, Borrero S. Racial/ethnic disparities in human papillomavirus vaccination initiation and completion among US women in the post-Affordable Care Act era. Ethn Health. 2020;25(3):393–407.
Daniel-Ulloa J, Gilbert PA, Parker EA. Human papillomavirus vaccination in the United States: uneven uptake by gender, race/ethnicity, and sexual orientation. Am J Public Health. 2016;106(4):746–7.
Pérez AE, Agénor M, Gamarel KE, Operario D. Nativity disparities in human papillomavirus vaccination among US adults. Am J Prev Med. 2018;54(2):248–58.
Boakye EA, et al. Differences in human papillomavirus (HPV) vaccine uptake by nativity status among men aged 18–34 years. Prev Med Rep. 2019;16:101010.
De P, Budhwani H. Human papillomavirus (HPV) vaccine initiation in minority Americans. Public Health. 2017;144:86–91.
Healy J, et al. Vaccination coverage among foreign-born and U.S.-born adolescents in the United States: successes and gaps–National Immunization Survey-Teen, 2012–2014. Vaccine. 2018;36(13):1743–50.
Williams WW, Lu PJ, O’Halloran A, Kim DK, Grohskopf LA, Pilishvili T, et al. Surveillance of vaccination coverage among adult populations-United States, 2014. MMWR Surveill Summ. 2016;65(1):1–36.
Lu PJ, et al. Adult vaccination disparities among foreign-born populations in the U.S., 2012. Am J Prev Med. 2014;47(6):722–33.
Srinivasan S, Guillermo T. Toward improved health: disaggregating Asian American and Native Hawaiian Pacific Islander data. Am J Public Health. 2000;90(11):1731–4.
McElfish P, et al. Diabetes and hypertension in Marshallese adults: results from faith-based health screenings. J Racial Ethn Health Disparities. 2017;4(6):1042–50.
Bond SM, Cartmell KB, Lopez CM, Ford ME, Brandt HM, Gore EI, et al. Racial and ethnic group knowledge, perceptions and behaviors about human papillomavirus, human papillomavirus vaccination, and cervical cancer among adolescent females. J Pediatr Adolesc Gynecol. 2016;29(5):429–35.
Griffioen AM, Glynn S, Mullins TK, Zimet GD, Rosenthal SL, Fortenberry JD, Kahn JA. Perspectives on decision making about human papillomavirus vaccination among 11- to 12-year-old girls and their mothers. Clinical Pediatrics. 2012;51(6):560–568.
Joseph NP, Clark JA, Mercilus G, Wilbur M, Figaro J, Perkins R. Racial and ethnic differences in HPV knowledge, attitudes, and vaccination rates among low-income African-American, Haitian, Latina, and Caucasian young adult women. J Pediatr Adolesc Gynecol. 2014;27(2).
National Center for Health Statistics, Survey Description, National Health Interview Survey, 2014. 2015, Centers for Disease Control and Prevention, National Center for Health Statistics: Hyattsville, MD.
National Center for Health Statistics. Native Hawaiian and Pacific Islander (NHPI) 2014, 2017; Available from: https://www.cdc.gov/nchs/nhis/nhpi.html. Accessed 7 May 2020.
National Center for Health Statistics. About the National Health Interview Survey. 2016; Available from: https://www.cdc.gov/nchs/nhis/about_nhis.htm. Accessed 7 May 2020.
National Center for Health Statistics. Native Hawaiian and Pacific Islander (NHPI) National Health Interview Survey (NHIS). 2017; Available from: https://www.cdc.gov/nchs/nhis/nhpi.html. Accessed 7 May 2020.
Kaminska O, Lynn P. Survey-based cross-country comparisons where countries vary in sample design: issues and solutions. J Off Stat. 2017;33(1):123–36.
Thompson EL, Rosen BL, Maness SB. Social determinants of health and human papillomavirus vaccination among young adults, National Health Interview Survey 2016. J Community Health. 2019;44(1):149–58.
StataCorp. Stata Statistical Software, S. LP, Editor. 2015: StataCorp.
Rao JNK, Scott AJ. On chi-square test for multiway contingency tables with cell proportions estimated from survey data. Ann Stat. 1984;12(1):40–60.
Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280(19):1690–1.
Lebrun L, Dubay L. Access to primary and preventive care among foreign-born adults in Canada and the United States. Health Serv Res. 2010;45(6 Pt 1):1693–719.
Derose K, et al. Review: immigrants and health care access, quality, and cost. Med Care Res Rev. 2009;66(4):355–408.
Bustamante A, Van der Wees P. Integrating immigrants into the U.S. health system. Virtual Mentor. 2012;14(1):318–23.
Hill H, et al. Vaccination coverage among children aged 19-35 months-United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(43):1171–7.
Scarinci I, Hansen B, Kim Y. HPV vaccine uptake among daughters of Latinx immigrant mothers: findings from a cluster randomized controlled trial of a community-based, culturally relevant intervention. Vaccine. 2020;38(25):4125–34.
Ferrer H, et al. Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC Public Health. 2014;14:700.
Bleser W, Miranda P, Jean-Jacques M. Racial/ethnic disparities in influenza vaccination of chronically-ill U.S. adults: the mediating role of perceived discrimination in healthcare. Med Care. 2016;54(6):570–7.
Sriram S, Ranganathan R. Why human papilloma virus vaccination coverage is low among adolescents in the US? A study of barriers for vaccination uptake. J Family Med Prim Care. 2019;8(3):866–70.
Joseph N, et al. Knowledge, attitudes, and beliefs regarding HPV vaccination: ethnic and cultural differences between African-American and Haitian immigrant women. Womens Health Issues. 2012;22(6):e571–9.
Dela Cruz M, et al. Human papillomavirus (HPV) vaccination motivators, barriers, and brochure preferences among parents in multicultural Hawai'i: a qualitative study. J Cancer Educ. 2017;32(3):613–21.
Parsons VL, Moriarity C, Jonas K, Moore TF, Davis KE, Tompkins L. Design and estimation for the National Health Interview Survey, 2006-2015. National Center for Health Statistics. Vital Health Stat 2(165). 2014.
2014 NHPI-NHIS, survey description document. 2014, Centers for Diesease Control and Prevention.
2014 NHIS, survey description document. 2015, Centers for Diesease Control and Prevention: Maryland.
Lawton MD, Nathan M, Asboe D. HPV vaccination to prevent anal cancer in men who have sex with men. Sex Transm Infect. 2013;89(5):342–3.
Gerend MA, Madkins K, Phillips G II, Mustanski B. Predictors of human papillomavirus vaccination among young men who have sex with men. Sex Transm Dis. 2016;43(3):185–91.
Portela M, Sommers BD. On the outskirts of National Health Reform: a comparative assessment of health insurance and access to Care in Puerto Rico and the United States. Milbank Q. 2015;93(3):584–608.
Pérez C, Ailshire JA. Aging in Puerto Rico: a comparison of health status among island Puerto Rican and mainland U.S. older adults. J Aging Health. 2017;29(6):1056–78.
Funding
Support for this study was partially supported by a Translational Research Institute grant (no. 1U54TR001629-01A1) through the National Center for Advancing Translational Sciences of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
All authors contributed to drafting and revising the manuscript. The conception and design of work was conducted by Pearl A. McElfish, PhD, Marie-Rachelle Narcisse, PhD, and Holly C. Felix, PhD. Data analysis was conducted by Marie-Rachelle Narcisse, PhD. All authors contributed in interpreting the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to declare.
Ethical Standards Disclosure
This study was ruled exempt as non-human subjects research by the University of Arkansas for Medical Sciences Institutional Review Board (IRB#206591).
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Analysis, interpretation, and/or conclusions based on the NHIS are solely those of the authors and do not represent those of the NCHS, which are responsible for the data.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McElfish, P.A., Narcisse, MR., Felix, H.C. et al. Race, Nativity, and Sex Disparities in Human Papillomavirus Vaccination Among Young Adults in the USA. J. Racial and Ethnic Health Disparities 8, 1260–1266 (2021). https://doi.org/10.1007/s40615-020-00886-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-020-00886-5