Abstract
Purpose of Review
The purpose of this review is to assess the toxicological consequences of crude oil vapor (COV) exposure in the workplace through evaluation of the most current epidemiologic and laboratory-based studies in the literature.
Recent Findings
Crude oil is a naturally occuring mixture of hydrocarbon deposits, inorganic and organic chemical compounds. Workers engaged in upstream processes of oil extraction are exposed to a number of risks and hazards, including getting crude oil on their skin or inhaling crude oil vapor. There have been several reports of workers who died as a result of inhalation of high levels of COV released upon opening thief hatches atop oil storage tanks. Although many investigations into the toxicity of specific hydrocarbons following inhalation during downstream oil processing have been conducted, there is a paucity of information on the potential toxicity of COV exposure itself.
Summary
This review assesses current knowledge of the toxicological consequences of exposures to COV in the workplace.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There were approximately 186,000 workers employed in August 2020 in the USA in the oil and gas extraction industry [1,2,3,4]. At several points in the production chain from the ground to the refinery, including drilling, storage, pipelines, and cleaning operation, workers are potentially exposed by inhalation to crude oil vapor (COV) or by getting crude oil on their skin [5,6,7,8,9,10,11]. Crude oil is a complex mixture of organic chemicals, metals, salts, and semivolatile species [1, 12]. The relative concentrations of the various components depend on the drilling fields, depth of drilling, and geographical location of extraction [1]. The rate of illness and injury in the upstream segment of the oil and gas extraction industry, which includes exploration, drilling, storage, and transportation of crude oil to refineries, is comparable to that of workers in all industries [13], but the rate of fatality is higher [14], and many physical hazards have been recognized. However, the adverse health effects of crude oil exposure in upstream workers are less clearly defined. There is abundant information regarding the short- and long-term health effects resulting in humans from exposure to crude oil components, but the majority of information on the health effects of raw COV exposure comes from its effects on cleanup workers after oil spills [15,16,17]. The purpose of this review is to assess the toxicological consequences of COV exposure in the workplace through evaluation of the most current epidemiologic and laboratory-based studies in the literature.
Epidemiologic Studies in Crude Oil–exposed Workers
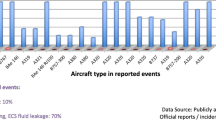
Workers in the oil and gas industry are exposed to hydrocarbon vapors (HCV) and volatile organic compounds (VOCs) while conducting routine tasks in or around petroleum storage tanks, such as manual gauging, sample collection, flow back operations, and tank cleaning and maintenance [18,19,20,21]. Opening of the thief hatch atop petroleum storage tanks results in the release of HCV/VOC plumes (> 100,000 ppm), which can result in worker exposure at or downwind from the tank [21,22,23,24,25]. From January 2010 to March 2015, nine oil worker deaths were attributed to a combination of oxygen deficiency and HCV/VOC inhalation following opening of thief hatches [26], with exposure to hydrogen sulfide being ruled out as a cause of death [27].
In a series of retrospective, cross-sectional follow-up analyses of petroleum company records, the overall rate of mortality of workers in all job categories was essentially comparable to that of the US population, although increases were observed for certain diseases (cancers and blood diseases) [28,29,30,31,32,33]. Cancer incidence (acute myelogenous leukemia and multiple myeloma) was correlated to historical crude oil exposure in one study [34]. In addition, morbidity studies of petroleum workers noted respiratory and heart diseases among the five most prevalent illnesses [35,36,37]. These studies did not consider the healthy worker effect (the notion that the health of workers is generally better than that of the overall population [38]), other comorbidities in their study designs, or upstream stream petroleum workers in their studies. Limited worker exposure data exists for the petroleum industry [39]. Because it can take 10 years or longer for coronary, respiratory, and other chronic disease to develop following occupational exposure, these studies were not able to directly link crude oil to the development of these diseases.
Important insights into the potential adverse health effects of inhaled COV on upstream petroleum workers are provided from the early and chronic symptoms occurring after oil tanker accidents, approximately 38 of which have occurred over the past few decades [39]. Because the petroleum product carried in each tanker varies from ship to ship, it is difficult to associate a particular set of symptoms with a specific type of oil. Adverse health effects in oil spill cleanup and recovery response workers were not investigated after every incident. Most often, the observed effects followed inhalation exposure to weathered petroleum, which lacks many volatile constituents. Many of the investigations involved short-term cross-sectional studies without obtaining biological samples (e.g., blood) or physiological measurements for analysis. Despite these caveats, early and follow-up investigations of cleanup workers and residents in proximity indicated that exposures were associated with a variety of acute, sub-chronic, and chronic symptoms including upper and lower respiratory, neurological (headache, nausea, vomiting, dizziness), liver function, hematological function, and ocular abnormalities [40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75]. Other outcomes, i.e., genotoxic [75,76,77], reproductive [78, 79], endocrine [80], and effects of skin exposure [81], have been reported in workers. Some acute effects of oil exposure appear to be reversible, such as lung function decrements in Deepwater Horizon cleanup workers [82].
It is of importance to note that chemical dispersants are employed to minimize damage to the environment during oil spill cleanup, and workers are potentially exposed. The bulk of the studies of the biological effects of dispersants address effects in non-mammalian species; investigations in mammals are limited in number (see, for example, [83]). In rodent models, inhalation exposure to COREXIT® EC9500A caused myriad toxicological responses in skin, the cardiovascular system, lungs, and brain [84,85,86,87,88]. Cleanup workers are potentially exposed to a mixed exposure consisting of weathered oil vapor and dispersant to varying degrees, each with its own toxicological profile. There exists a knowledge gap in the understanding of additive or possible synergistic interactions of oil vapor and dispersant exposure in crude oil cleanup workers.
Chronic exposure to crude oil over periods of years may lead to unrecognized morbidities. Follow-up studies indicate that persistent respiratory symptoms, markers of lung injury, and chromosome damage persisted in workers for at least 2 years following cleanup of bunker oil (heavy oil) from the 2002 Prestige spill [44, 52]. Decrements in lung function were observed after the Tasman Spirit (Iranian light crude) shipwreck [82]. Investigations into the long-term toxicological effects associated with cleanup of oil spills have been conducted, and some symptoms appear to have waned over time (years), for example, the respiratory symptoms [62, 63, 80]. On the other hand, elevated heart attack risk [65], reduced lung function in some cleanup workers [64], and genetic alterations [67] persisted for several years.
Studies performed to examine the long-term effects of crude oil exposure indicated that workers maintaining tanks in ships (jobs including inspection, cleaning, repair) experienced immune suppression characterized by decreases in IgM and IgA levels (Kirkeleit et al., 2006). Oil shale workers experience respiratory, neurological, cardiovascular, and other physical problems [81], and, in crude oil workers in the USSR, hypertension was observed [82]. Subsequently, cardiovascular morbidity was reported in a study of upstream oil workers [89]. Decrements in respiratory function are known to exist 1–3 years after acute inhalation exposure to aromatic hydrocarbons, which are also present in crude oil vapor (e.g., benzene, [90, 91]).
Hepatic Effects
The liver is an organ critical for biotransformation of xenobiotic agents, including hydrocarbons and other volatile components of crude oil [92], for removal from the body. Human exposure to crude oil is associated with changes in the liver and its function. Sonographic assessments of petroleum-induced hepatotoxicity among oil workers revealed enhanced echogenicity, fatty liver, and increased liver size [93, 94]. Assessment of liver function indices among volunteers participating in the Deepwater Horizon (DWH) oil spill cleanup operations showed increased liver marker enzymes, aspartate transaminase (AST) and alanine transaminase (ALT), which persisted in follow-up studies conducted 7 years after the initial assessment [56,57,58]. These long-term effects resulting from oil spill exposure suggest that oil spill response workers may be at risk for developing hepatotoxicity and altered liver function [56, 58, 93, 94].
Potential Toxicologic Mechanisms of Downstream Petroleum Products
Several investigations have examined the effects of upstream and downstream petroleum products in non-human mammalian systems or non-mammalian systems to define toxicity and potential mechanisms. Upstream production includes extraction and production, while downstream production includes post-production of crude oil activities at refineries, petrochemical plants, and storage tanks. The many adverse biological effects of downstream petroleum products [95, 96] are not summarized here, but information has been reported in the literature and made available by the petroleum industry [97,98,99]. Their relevance to modeling inhaled COV adverse health effects in humans is limited. A few inhalation studies of the effects of downstream petroleum products have been conducted [100,101,102], but we discovered only one [103] involving crude oil. Other identified studies rely, instead, on oral, dermal, or i.p. administration or the use of in vitro cells or cell lines. Table 1 summarizes the non-carcinogenic end points and cellular pathways induced by crude oil exposure in mammalian and in vitro systems.
A comprehensive review of the toxicology of oil in vertebrates is provided by Takeshita et al. [75]. Inhalation of a heavy distillate of coal liquid increased heart rate and blood pressure in response to isoproterenol [104], a β-adrenoceptor agonist. While the composition of coal distillate is very different from crude oil, both crude oil and coal distillate contain complex and aromatic hydrocarbon compounds, and therefore, the effects of distillate exposure could be predictive of COV’s adverse effects. Attempts have been made using animal organ/tissue end-points, none of them involving pathophysiological measurements, to predict the acute and repeated dose toxicity of petroleum mixtures in humans based upon knowledge of certain well-characterized PAH components [97, 105,106,107].
Pathophysiological Effects of COV Exposure in Animal Models
Until recently, comprehensive studies had not been undertaken to investigate the potential pathophysiological effects of COV inhalation on the respiratory, cardiovascular, central nervous, and immune systems and kidneys using mammalian animal models, although one investigation using rats and mice examined the pulmonary effects of a heavy fuel oil blend resembling the oil spilled from the Prestige oil tanker [108]. A great deal of information is known regarding the toxicities of the individual components found in crude oil [90, 91, 109, 110], but the toxicity of COV exposure, as occurs in workers, is not well understood.
Recently, investigations [92, 111,112,113,114,115,116,117,118] were conducted to evaluate the toxicity of inhaled COV generated from Deep Water Horizon (DWH) surrogate crude oil in a rat model to gain a greater understanding of the adverse health effects of COV inhalation in upstream petroleum workers [49, 74, 119]. The DWH surrogate crude oil provided by British Petroleum (BP) Exploration and Production, Inc., similar to the oil associated with the 2010 Deepwater Horizon spill from the Macondo Well in Mississippi Canyon Block 252, was characterized in McKinney et al. [95]. In vivo and in vitro endpoint measures were made 1 and 28 days after an acute, whole-body exposure to 300 ppm COV for 6 h, or 1, 28, and 90 days after a sub-chronic exposure (300 ppm VOCs for 6 h/days × 4 days/week × 4 weeks). The COV level used in the animal exposures brackets those that have been measured at thief hatches and flowback operations in the field.
Pulmonary Effects
Studies in the lung [114] indicated that no changes in respiratory system resistance, elastance, tissue damping, tissue elastance, Newtonian resistance, hysteresivity, or reactivity to inhaled methacholine (MCh) were elicited by COV inhalation. Ninety days after sub-chronic exposure to COV, the inhibitory effect of the airway epithelium on in vitro reactivity of airway smooth muscle to MCh was enhanced. Cholinergically mediated, neurogenic contractile responses of airways in vitro were unaffected following COV exposure. Investigation of ion transport by the tracheal epithelium revealed that neither basal resistance nor short-circuit current was modified by COV 28- and 90-day post-exposure, but Cl¯ and Na+ transport were enhanced 1 day post-exposure. No significant effects in lung vascular permeability were observed at any end point time following acute or sub-chronic inhalation of COV. No histological exposure-related morphologic alterations were observed in the lungs of the COV-exposed rats. Evidence of an inflammatory response was obtained from analysis of bronchioalveolar lavage fluid (BALF). There were no significant effects of COV on BALF lactate dehydrogenase activity, a common measure of cytotoxicity. At 1 day post-exposure to COV, there were significant increases in leptin, interleukins (IL)-1β and IL-10, IFN-γ-inducible protein (IP-10), and lipopolysaccharide-induced CXC chemokine (LIX), and, at 28 days, vascular endothelial growth factor (VEGF) was significantly increased. At 90-day post-exposure, COV exposure caused decreases in granulocyte–macrophage colony stimulating factor, interferon-γ, and neutrophil activating protein CXCL1. Examination of a large panel of cytokine mediators revealed no changes in their levels in BALF following COV inhalation. No changes in the total cells, alveolar macrophages, or neutrophils occurred at any of the post-exposure measurement periods. Oxidant production by macrophages was minimally affected. No significant changes in the global gene expression profiles were detected in the lungs of the acute COV-exposed animals at 1 day post-exposure. Significant differential expression of 47 genes and 52 genes was detected in the acute (300 ppm VOCs × 6 h/day × 1 day) 1 and 28 days and sub-chronic (300 ppm VOCs × 6 h/days × 4 days/week × 4 weeks) COV-exposed rat lungs at 28 days post-exposure, respectively. The changes in the lung gene expression profile detected in the absence of any detectable lung toxicity in the COV-exposed rat lungs were likely due to the greater sensitivity of the transcriptome to respond compared to pathophysiological, histological, and biochemical endpoints of target organ toxicity.
Cardiovascular and Renal Effects
Cardiovascular and renal effects of COV exposure were examined [115]. Acute COV exposure decreased left ventricular end-systolic pressure 1 day post-exposure and left ventricular end-diastolic pressure 28 days post-exposure. Dobutamine-induced vasoconstriction was not markedly affected 1 day following exposure, but was reduced 28 days following exposure. Diastolic and mean arterial pressures also were reduced 1 day following acute COV treatment. The acute exposure resulted in an increase in oxidative stress in COV-exposed animals 24 h after exposure, but by 28 days following exposure measures of oxidative stress was reduced in both groups of animals. Analysis in heart and kidney revealed a myriad of COV-induced, post-exposure changes in transcript levels of multiple inflammatory cytokines and enzymes at varying post-exposure time points: IL-6, hypoxia-induced factor-1α, TNF-α, inducible NO synthases, endothelial nitric oxide synthase, tumor necrosis factor, IL-1β, Il-6, tissue inhibitor of metalloproteinase, catalase, and superoxide dismutase. Protein markers that have been associated with the presence of cardiovascular or renal dysfunction also were measured after acute COV exposure. There were no significant exposure-related differences in concentrations of any of the proteins in the heart or kidneys.
Neurological Effects
Sriram et al. [117] investigated the effects of COV inhalation on several aspects of nervous system function. As alkanes, cycloalkanes/naphthenes, and aromatic hydrocarbons present in COV are membrane-perturbing compounds, it was hypothesized that they can affect neuronal membranes causing aberrant synaptic signaling and impaired neurotransmission, defects which can ultimately culminate in neural damage. Indeed, acute or sub-chronic exposure to COV was shown to cause brain region- and time-specific alterations in the levels of the biogenic neurotransmitters, norepinephrine (NE), epinephrine (EPI), dopamine (DA), and serotonin (5-hydroxytryptamine (5-HT) in the olfactory bulb (OB), striatum (STR), and/or midbrain (MB). Monoamines like DA, NE, EPI, and 5-HT are known to modulate olfactory function, regulate odor inputs, and play a role in depression and anxiety disorders. Acute or sub-chronic COV exposure altered the expression of several synaptic proteins including synaptophysin 1 (SYP), synaptotagmin (SYT), and/or tyrosine 3-monooxygenase/tryptophan 5-monooxygenase activation protein epsilon (YWHAE) in the brain. Specifically, sub-chronic COV exposure induced SYP and SYT protein expression in all brain regions examined. SYP and SYT are involved in synaptic transmission, and their increased expression is associated with long-term potentiation of synaptic mechanisms for altering neurotransmitter release and olfactory memory formation. Abnormal accumulation of synaptic proteins might result in modulation of neurotransmission and functional disturbances. SYP, a major synaptic vesicle protein, is also involved in vesicle sorting, priming, synaptic biogenesis, synapse formation, exocytosis, and endocytosis. It plays a key role in axonal neurotransmitter release, including release of DA. Dynamic changes in the expression of presynaptic and axonal proteins are known to precede dopaminergic neurotoxicity. Indeed, changes in the expression of dopaminergic and PD-related proteins, tyrosine hydroxylase (TH), Parkinson disease-5, autosomal dominant (PARK5; also known as ubiquitin carboxy-terminal hydrolase L1/UCHL1), and Parkinson disease 7, autosomal recessive early-onset (PARK7; also known as Parkinsonism-associated deglycase or oncogene DJ1) were also seen after COV exposure. Acute exposure to COV increased TH and PARK7 proteins in the dopaminergic brain areas, STR and MB. Sub-chronic COV exposure upregulated PARK5 and PARK7 proteins in the STR and MB. TH is the rate-limiting enzyme in the synthesis of DA. Modulation of its function or loss of TH protein is an index of dopaminergic injury. PARK genes are normally involved in affording neuroprotection against oxidative stress resulting from mitochondrial dysfunction. In humans, loss-of-function mutations in PARK genes are associated with early-onset Parkinsonism [118]. The increased expression of PARK5 and PARK7 in the STR and MB following COV exposure reflects a potential protective mechanism to clear over-expressed or defective/abnormal proteins, control oxidant damage, and maintain mitochondrial integrity.
Immunological Effects
The immunotoxicity of COV following acute and sub-chronic inhalation exposure was investigated [119]. The immune cell subsets present in lung lymph node (LLN), bronchoalveolar lavage, and spleen, along with total cellularity, were characterized. Acute COV inhalation exposure increased BALF cellularity, CD4 + and CD8 + cells, and absolute and percent CDllb + cells only at 1 day post-exposure. Sub-chronic inhalation exposure resulted in a decreased frequency of CD4 + T-cells at 1 day post-exposure and an increased number and frequency of B-cells at 28 days post-exposure in the LLN. A significant elevation in the number and frequency of B-cells was observed in the spleen at 1 day post-exposure. Exposure to COV, acutely and sub-chronically, suppressed NK cell function 1 d post exposure. No changes were observed at the other post exposure time points. Serum chemistries and complete blood counts were analyzed following COV exposure. No consistent hematological changes were observed at all the time points evaluated. The IgM response to SRBC was examined to evaluate whether exposure to COV was immunosuppressive. No significant change in the PFC/spleen or specific (PFC/106 cells) IgM antibody activity against SRBC was observed at any of the post-exposure time points.
Hepatic Effects
In the scientific literature, there are limited studies describing potential mechanisms involved in crude oil exposure–induced effects in the liver. Exposure of mice to the Prudhoe Bay crude oil resulted in an increase in liver weight, increased hepatic total protein, and increased total lipids [120]. Rats exposed to Nigerian bonny light crude oil (BLCO) exhibited hepatic degeneration, which was associated with reduced γ-glutamyl transferase activity and elevated levels of serum aminotransferases, glutathione, hydrogen peroxide, and malondialdehyde, suggesting oxidative stress [121]. BLCO has also been shown to inhibit calcium influx and induce mitochondrial DNA, leading to mitochondrial swelling and dysfunction in the liver of guinea pigs [122]. The various components of crude oil, e.g., BTEX and others, however, have been examined extensively for their effects on the liver [123,124,125,126].
Conclusions
The broadest conclusion from the studies with DWH surrogate crude oil was the lack of biological effects in several organ systems apart from the nervous and immune systems. Where changes were evident, the brain and immune systems appeared to be the most responsive. Surprisingly, measurement of diverse in vivo and in vitro markers of ventilatory and non-ventilatory lung function revealed that the lungs were refractory to the effects of COV administered acutely or sub-chronically, despite being a portal of entry of the vapor. COV exposure resulted in changes in the levels of several markers in the brain and kidney. These did not follow a strict post-exposure continuum time-dependence, nor were they relatable to acute vs. sub-chronic exposure paradigms. For the most part, COV-induced changes were overcome by 28–90 days post-exposure.
The profile of immune cell subsets in BALF at 1 day post-exposure revealed COV-induced alterations; other immune profiles were not affected. Whereas it can be safely assumed that inhaled COV triggered responses in other organ systems mostly after having entered the lungs, whole-body exposure of the animals to the vapor exposed their skin directly. Future studies using nose-only exposures to COV will be needed to ascertain whether responses comparable to those observed in the current investigation were triggered or influenced by a dermal exposure component, as could potentially be experienced in upstream oil workers.
The question of whether the findings made here are directly relevant to the adverse health effects observed in the DWH or other oil-spill cleanup workers can be raised. Here, it is difficult to draw definitive conclusions. First, the spilled oil to which the workers were exposed was weathered by the environment and, over time, its composition was changed. Second, chemical dispersants were employed to minimize damage to the environment and workers were potentially exposed to these in addition to weathered oil vapor. Oil spill cleanup workers experience mixed exposures consisting of weathered oil vapor and dispersant to varying degrees, whereas exposures in upstream oil workers consist of neat crude oil and its vapor. The findings made in each context cannot be extrapolated across exposure scenarios.
There is limited information about effects of COV at the molecular/cellular level in mammalian biological systems. Possible mechanisms, derived primarily in non-mammalian species include induction of hepatic enzymes and leukotriene formation, enzyme release from AMs, anti-estrogenic activity and ROS, altered gene expression, increased expression of nucleotide excision repair pathway genes, products of xenobiotic metabolism, DNA adduct formation, differential expression of miRNA, altered mitochondrial function, DNA damage, chromatin changes, aryl hydrocarbon receptor interaction, androgen and estrogen receptor interaction, oxidation/peroxidation systems, and decrease in rhodopsin mRNA expression and increase in hematopoietic regulator, runx1 (runt-related transcription factor 1). For example, in the heart, the decreases in ROS levels may have been involved in decrements of function, i.e., blood pressure changes. However, the various changes in airway epithelial ion transport are difficult to ascribe mechanistically to any of the biomarkers mentioned above; for example, there are no reports of the aryl hydrocarbon receptor as a component of the pathways regulating airway epithelial Na+ or Cl¯ channels. It remains for future studies to define the transduction pathways affected by COV in the organ systems that have been studied and those that have not, e.g., liver.
The way COV (inhaled or dermal) interacted with organs in the rat to alter function is unknown. Was COV taken up by the lungs (and skin) and distributed subsequently throughout the body, or were signals sent from the lung to other organs via the blood?
Much work remains to characterize further the toxicity of inhaled COV, i.e., its effects after longer exposure periods and over a range of exposure concentrations, and, accompanying that, its residual effects during longer post-exposure periods. Inasmuch as workers at oil well fracking sites are exposed to varying climate conditions, such that an exposure to a constant level of COV in the ambient air is not achieved, models that recapitulate cyclic/periodic exposures to the vapor could better estimate workplace exposure hazards to itinerant workers. Moreover, the composition of crude oil is geographic region-specific. The degree to which the toxicity of vapors derived from crude oils extracted at different gas/oil plays would give rise to similar biological effects is unknown but is important for worker safety.
References
Downey M. Oil 101. 1st ed. New York: Wooden Table Press LLC: 2009.
United States Department of Labor. Bureau of Labor Statistics, 2020a. Industries at a glance. Oil and gas extraction: NAICS 211. www.bls.gov/iag/tgs/iag211.htm.
United States Department of Labor. Bureau of Labor Statistics, 2020b. Fatal and nonfatal occupational injuries and illnesses in the oil and gas industry 2014. www.bls.gov/iif/oshwc/cfoi/osar0018.htm.
United States Department of Labor. Bureau of Labor Statistics, 2020c. Databases, tables & calculators by subject. https://data.bls.gov/timeseries/CES1021311201.
Runion HE. Occupational exposures to potentially hazardous agents in the petroleum industry. Occup Med. 1988;3:431–44.
Eide I. A review of exposure conditions and possible health effects associated with aerosol and vapour from low-aromatic oil-based drilling fluids. Ann Occup Hyg. 1990;34:149–57.
Moen BE, Hollund BE, Berntsen M, Flo R, Kyvik KR, Riise T. Occupational exposure of deck crews to carcinogenic agents on crude oil tankers. Am J Indust Med. 1995;27:555–64.
Verma D, Johnson DM, McLean JD. Benzene and total hydrocarbon exposures in the upstream petroleum oil and gas industry. Am Indust Hyg Assoc J. 2000;61:255–63.
Gardner R. Overview and characteristics of some occupational exposures and health risks on offshore oil and gas installations. Ann Occup Hyg. 2003;47:201–10.
Kirkeleit J, Riise T, Bratveit M, Moen BE. Increased risk of acute myelogenous leukemia and multiple myeloma in a historical cohort of upstream petroleum workers exposed to crude oil. Cancer Causes Control. 2008;19:13–23.
Zock JP, Rodríguez-Trigo G, Rodríguez-Rodríguez E, Pozo-Rodríguez F, Gómez F, Fuster C, Castaño-Vinyals G, Antó JM, Barberà JA. Long-term health effects of the Prestige oil spill (Galacia, Spain). Epidemiology. 2009;20:S242–3.
IARC Monographs on the evaluation of carcinogenic risk to humans: occupational exposures in petroleum refining: crude oil and major petroleum fuels. IARC, Lyon, 1–321.
United States Department of Labor. Bureau of Labor Statistics, 2020b. Fatal and nonfatal occupational injuries and illnesses in the oil and gas industry. 2014. http://www.bls.gov/iif/oshwc/cfoi/osar0018.htm. Accessed 27 June 2023.
National Institute for Occupational Safety and Health, 2020a. Fatalities in the oil and gas extraction industry (FOG). http://www.cdc.gov/niosh/topics/fog/default.html. Accessed 27 June 2023.
Niven K, McLeod R. Offshore industry: management of health hazards in the upstream petroleum industry. Occup Med. 2009;59:304–9.
Aguilera F, Mendez J, Pasaro E, Laffon B. Review on the effects of exposure to spilled oils on human health. J Appl Toxicol. 2010;30:291–301.
Laffon B, Pasaro E, Valdiglesias V. Effects of exposure to oil spills on human health: updated review. J Toxicol Environ Health B Crit Rev. 2016;19:105–28.
Esswein EJ, Snawder J, King B, Breitenstein M, Alexander-Scott M. Preliminary field studies on worker exposures to volatile chemicals during oil and gas extraction flowback and production testing operations. 2014; https://blogs.cdc.gov/niosh-science-blog/2014/08/21/flowback-2/. Accessed 27 June 2023.
Esswein EJ, Snawder J, King B, Breitenstein M, Alexander-Scott M, Kiefer M. Evaluation of some potential chemical exposure risks during flowback operations in unconventional oil and gas extraction: preliminary results. J Occup Environ Hyg. 2014;11(10):D174-84. https://doi.org/10.1080/15459624.2014.933960.
King, B., Esswein, E., Retzer, K., Snawder, J., Ridl, S., Breitenstein, M., Alexander-Scott, M. and Hill, R., 2015. UPDATE: Reports of worker fatalities during manual tank gauging and sampling in the oil and gas extraction industry. https://blogs.cdc.gov/niosh-science-blog/2015/04/10/flowback-3/
Snawder J, Esswein E, King B, Breitenstein M, Alexander-Scott M, Retzer K, Keifer M, Hill R. Reports of worker fatalities during flowback operations. 2014. https://blogs.cdc.gov/niosh-science-blog/2014/05/19/flowback/. Accessed 27 June 2023.
Jordan, T., 2015. Hydrocarbon exposures during tank gauging and sampling operations. www.stepsnetwork.com/member-presentations/file/Tank_GaugingMonitoring_Results%252Epdf
National Institute for Occupational Safety and Health/Occupational Safety and Health Administration. Hydrocarbon exposures during tank gauging and sampling operations. 2015. https://www.osha.gov/sites/default/files/publications/OSHA3843.pdf. Accessed 27 June 2023.
National Institute for Occupational Safety and Health. Fatalities in the oil and gas extraction industry (FOG). 2020. https://www.cdc.gov/niosh/topics/fog/publications.html. Accessed 27 June 2023.
National Institute for Occupational Safety and Health/Occupational Safety and Health Administration. Health and safety risks for workers involved in manual tank gauging and sampling at oil and gas extraction sites. 2015. https://www.osha.gov/Publications/OSHA3843.pdf. Accessed 27 June 2023.
Harrison RJ, Retzer K, Kosnett MJ, Hodgson M, Jordan TS, Kiefer M. Sudden deaths among oil and gas extraction workers resulting from oxygen deficiency and inhalation of hydrocarbon gases and vapors - United States, January 2010 - March 2015. Morb Mortal Wkly Rep. 2016;65:6–9.
Retzer K, Ridl S, Hill R. Oil and gas extraction worker fatalities. 2014 mid-year report: January 1, 2–014 - June 30, 2014. 2015. https://www.cdc.gov/niosh/docs/2015-239/pdfs/2015-239.pdf. Accessed 27 June 2023.
Divine BJ, Barron V, Kaplan SD. Texaco mortality study. I. Mortality among refinery, petrochemical, and research workers. J Occup Med. 1985;27:445–7.
Divine BJ, Hartman CM, Wendt JK. Update of the Texaco mortality study 1947–93: part I. Analysis of overall patterns of mortality among refining, research, and petrochemical workers. Occup Environ Med. 1999;56:167–73.
Divine BJ, Barron V. Texaco Mortality Study: II. Patterns of mortality among white males by specific job groups. Am J Indust Med. 1986;10:371–81.
Divine BJ, Barron V. Texaco mortality study: III. A cohort study of producing and pipeline workers. Am J Indust Med. 1987;11:189–202.
Schnatter AR, Theriault G, Katz AM, Thompson FS, Donaleski D, Murray N. A retrospective mortality study within operating segments of a petroleum company. Am J Indust Med. 1992;22:209–29.
Raabe GK, Collingwood KW, Wong O. An updated mortality study of workers at a petroleum refinery in Beaumont, Texas. Am J Indust Med. 1998;33:61–81.
Kirkeleit J, Ulvestad E, Riise T, Bratveit M, Moen BE. Acute suppression of serum IgM and IgA in tank workers exposed to benzene. Scand J Immunol. 2006;64:690–8.
Tsai SP, Dowd CM, Cowles SR, Ross CE. Prospective morbidity surveillance of shell refinery and petrochemical employees. Br J Ind Med. 1991;48:155–63.
Valentic D, Stojanovic D, Micovic V, Vukelic M. Work related diseases and injuries on an oil rig. Int Marit Health. 2005;56:56–66.
Park J, Lee CG, Ryu SY. Factors related to the prevalence of respiratory symptoms in workers in a petrochemical complex. J Occup Health. 2006;48:216–22.
Baillargeon J. Characteristics of the healthy worker effect. Occup Med. 2001;6:359–66.
Gaffney SH, Burns AM, Kreider ML, Unice KM, Widner TE, Paustenbach DJ, Booher LE, Gelatt RH, Panko JM. Occupational exposure to benzene at the ExxonMobil refinery in Beaumont, TX (1976–2007). Int J Hyg Environ Health. 2010;213:285–301.
Griest WH, Ho C, Guerin MR, Tyndall RL. Chemical comparison of weathered spilled oil and Exxon/Valdez hold oil from an occupational health standpoint. Govt Reports Announc Index (GRA&I). 1991;17:21.
Lyons RA, Temple JM, Evans D, Fone DL, Palmer SR. Acute health effects of the Sea Empress oil spill. J Epidemiol Community Health. 1999;53:306–10.
Morita A, Kusaka Y, Deguchi Y, Moriuchi A, Nakanaga Y, Iki M, Miyazaki S, Kawahara K. Acute health problems among the people engaged in the cleanup of the Nakhodka oil spill. Environ Res. 1999;81:185–94.
Suarez B, Lope V, Perez-Gomez B, Aragones N, Rodriguez-Artalejo F, Marques F, Guzman A, Viloria LJ, Carrasco JM, Martin-Moreno JM, Lopez-Abente G, Pollan M. Acute health problems among subjects involved in the cleanup operation following the Prestige oil spill in Asturias and Cantabria (Spain). Environ Res. 2005;99:413–24.
Zock JP, Rodriguez-Trigo G, Pozo-Rodriguez F, Barbera JA, Bouso L, Torralba Y, Anto JM, Gomez FP, Fuster C, Verea H. Prolonged respiratory symptoms in clean-up workers of the Prestige oil spill. Am J Respir Crit Care Med. 2007;176:610–6.
Zock JP, Rodríguez-Trigo G, Rodríguez-Rodríguez E, Espinosa A, Pozo-Rodríguez F, Gómez F, Fuster C, Castaño-Vinyals G, Antó JM, Barberà JA. Persistent respiratory symptoms in clean-up workers 5 years after the Prestige oil spill. Occup Environ Med. 2012;69:508–13.
Meo SA, Al-Drees AM, Rasheed S, Meo IM, Al-Saadi MM, Ghani HA, Alkandari JR. Health complaints among subjects involved in oil cleanup operations during oil spillage from a Greek tanker “Tasman Spirit.” Int J Occup Med Environ Health. 2009;22:143–8.
Meo SA, Al-Drees AM, Rasheed S, Meo IM, Khan MM, Al-Saadi MM, Alkandari JR. Effect of duration of exposure to polluted air environment on lung function in subjects exposed to crude oil spill into sea water. Int J Occup Med Environ Health. 2009;2:35–41.
Fontham ETH, Trapido E. Oil and water. Environ Health Perspect. 2010;118:A422-423.
Association NEH. National Environmental Health Association (NEHA) position on offshore oil drilling. J Environ Health. 2010;73:40.
Kim J. What are the potential physical health effects from the Gulf oil spill? 2010. https://www.medscape.com/viewarticle/725593. Accessed 27 June 2023.
Lee CH, Kang YA, Chang KJ, Kim CH, Hur JI, Kim JY, Lee JK. Acute health effects of the Hebei oil spill on the residents of Taean, Korea (Korean). J Prev Med Public Health. 2010;43:166–73.
Rodriguez-Trigo G, Zock JP, Pozo-Rodriguez F, Gomez FP, Monyarch G, Bouso L, Coll MD, Verea H, Anto JM, Fuster C, Barbera JA. Health changes in fishermen 2 years after clean-up of the Prestige oil spill. Ann Intern Med. 2010;153:489–98.
Sim MS, Jo IJ, Song HG. Acute health problems related to the operation mounted to clean the Hebei Spirit oil spill in Taean, Korea. Mar Pollut Bull. 2010;60:51–7.
Slomski A. Experts focus on identifying, mitigating potential health effects of Gulf oil leak. JAMA. 2010;304:621–2.
Solomon GM, Janssen S. Health effects of the Gulf oil spill. J Am Med Assoc. 2010;304:1118–9.
D’Andrea MA, Reddy GK. Crude oil spill exposure and human health risks. J Environ Occup Med. 2014;56:1029–41.
D’Andrea MA, Reddy GK. Health risks associated with crude oil spill exposure. J Am J Med. 2014;127:886.
D’Andrea MA, Reddy GK. The development of long-term adverse health effects in oil spill cleanup workers of the Deepwater Horizon offshore drilling rig disaster. Front Public Health. 2018;6:1–8.
O’Callaghan-Gordo C, Orta-Martínez M, Kogevinas M. Health effects of non-occupational exposure to oil extraction. Environ Health. 2016;15:56.
Levy BS, Nassetta WJ. The adverse health effects of oil spills: a review of the literature and a framework for medically evaluating exposed individuals. Int J Occup Environ. 2011;7:161–7.
Rusiecki J, Alexander M, Schwartz EG, Wang L, Weems L, Barrett J, Christenbury K, Johndrow D, Funk RH, Engel LS. The Deepwater Horizon oil spill coast guard cohort study. Occup Environ Med. 2023;2018(75):165–75. https://doi.org/10.1136/oemed-2017-104343. Accessed 27 June 2023.
Gam KB, Kwok RK, Engel LS, Curry MD, Stewart PA, Stenzel MR, McGrath JA, Jackson WB, Jensen RL, Lichtveld M, Miller AK, Sandler DP. Exposure to oil spill chemicals and lung function in Deepwater Horizon disaster response workers. J Occup Environ Med. 2018;60:e312–8.
Gam KB, Kwok RK, Engel LS, Curry MD, Stewart PA, Stenzel MR, McGrath JA, Jackson WB, Jensen RL, Keil AP, Lichtveld MY, Miller AK, Sandler DP. Lung function in oil spill response workers 1–3 years after the Deepwater Horizon disaster. Epidemiology. 2018;29:315–22.
Gam KB, Engel LS, Kwok RK, Curry MD, Stewart PA, Stenzel MR, McGrath JA, Jackson WB, Lichtveld MY, Sandler DP. Association between Deepwater Horizon oil spill response and cleanup work experiences and lung function. Environ Int. 2018;121(Pt 1):695–702.
Strelitz J, Sandler DP, Keil AP, Richardson DB, Heiss G, Gammon MD, Kwok RK, Stewart PA, Stenzel MR, Engel L. Exposure to total hydrocarbons during cleanup of the deepwater horizon oil spill and risk of heart attack across 5 years of follow-up. Am J Epidemiol. 2019;188:917–927. https://academic.oup.com/aje/article/188/5/917/5304463. Accessed 27 June 2023.
Kwok RK, Miller AK, Gam KB, Curry MD, Ramsey SK, Blair A, Engel LS, Sandler DP. Developing large-scale research in response to an oil spill disaster: a case study. Curr Environ Health. 2019;6:174–87.
Park M, Choi KH, Lee SH, Hur JI, Noh SR, Jeong WC, Cheong HK, Ha M. Health effect research on Hebei Spirit oil spill (HEROS) in Korea: a cohort profile. BMJ. 2019;9:1–13.
Alexander M, Engel LS, Olaiya N, Wang L, Barrett J, Weems L, Schwartz EG, Rusiecki JS. The Deepwater Horizon oil spill coast guard cohort study: a cross-sectional study of acute respiratory health symptoms. Environ Res. 2018;162:196–202.
Francés A, Hildur K, Barberà JA, Rodríguez-Trigo G, Zock JP, Giraldo J, Monyarch G, Rodriguez-Rodriguez E, de Castro RF, Souto A, Gómez FP, Pozo-Rodríguez F, Templado C, Fuster C. Persistence of breakage in specific chromosome bands 6 years after acute exposure to oil. PLoS One. 2016;11:e0159404.
National Institute for Occupational Safety and Health. Health hazard evaluation of Deepwater Horizon response workers. Health Effects Evaluation Report. 2010;1010–0115 & 2010–0129–3138. www.cdc.gov/niosh/hhe/reports/pdfs/2010-0115-0129-3138.pdf. Accessed 27 June 2023.
National Institute for Occupational Safety and Health, 2010d. Interim guidance for protecting Deepwater Horizon response workers and volunteers. www.cdc.gov/niosh/topics/oilspillresponse/protecting/general.html.
National Institute for Occupational Safety and Health, 2010e. NIOSH Reports of Deepwater Horizon response/unified area command illness and injury Data. https://www.cdc.gov/niosh/topics/oilspillresponse/data.html. Accessed 27 June 2023.
National Institute for Occupational Safety and Health, 2010f. Deep Water Horizon response. Making the most of federal Deepwater Horizon data for human Health. www.cdc.gov/niosh/topics/oilspillresponse/data.html. Accessed 27 June 2023.
National Environmental Health Association, 2010. Position on offshore oil drilling. https://neha.org/sites/default/files/publications/position-papers/NEHA_Off_Shore_Oil_Drilling_Position_Paper.pdf. Accessed 27 June 2023.
Takeshita R, Bursian SJ, Colegrove KM, Collier TK, Deak K, Dean KM, De Guise S, DiPinto LM, Elferink CJ, Esbaugh AJ, Griffitt RJ, Grosell M, Harr KE, Incardona JP, Kwok RK, Lipton J, Mitchelmore CL, Morris JM, Peters ES, Roberts AP, Rowles TK, Rusiecki JA, Schwacke LH, Smith CR, Wetzel DL, Ziccardi MH, Hall AJ. A review of the toxicology of oil in vertebrates: what we have learned following the Deepwater Horizon oil spill. J Toxicol Environ Health B Crit Rev. 2021;7:355–94.
Pérez-Cadahia B, Laffon B, Pasaro E, Mendez J. Genetic damage induced by accidental environmental pollutants. Sci World J. 2016;6:1221–37.
Pérez-Cadahia B, Laffon B, Valdiglesias V, Pasaro E, Mendez J. Cytogenetic effects induced by Prestige oil on human populations: the role of polymorphisms in genes involved in metabolism and DNA repair. Mutat Res. 2008;653:117–23.
Merhi ZO. Gulf Coast oil disaster: impact on human reproduction. Fertil Steril. 2010;94:1575–7.
De Celis R, Feria-Velasco A, González-Unzaga M, Torres-Calleja J, Pedrón-Nuevo N. Semen quality of workers occupationally exposed to hydrocarbons. Fertil Steril. 2000;73:221–8.
Villeneuve S, Cyr D, Lynge E, Orsi L, Sabroe S, Merletti F, Gorini G, Morales-Suarez-Varela M, Ahrens W, Baumgardt-Elms C, Kaerlev L, Eriksson M, Hardell L, Févotte J, Guénel P. Occupation and occupational exposure to endocrine disrupting chemicals in male breast cancer: a case-control study in Europe. Occup Environ Med. 2010;67:837–44.
Suárez B, Lope V, Pérez-Gómez B, Aragonés N, Rodríguez-Artalejo F, Marqués F, Guzmán A, Viloria LJ, Carrasco JM, Martín-Moreno JM, López-Abente G, Pollán M. Acute health problems among subjects involved in the cleanup operation following the Prestige oil spill in Asturias and Cantabria (Spain). Environ Res. 2005;99:413–24.
Lawrence LG, Keil AP, Garantziotis S, Umbach DM, Stewart PA, Stenzel MR, McGrath JA, Jackson WB, Kwok RK, Curry MD, Engel LS, Sandler DP. Lung function in oil spill responders 4–6 years after the Deepwater Horizon disaster. J Toxicol Environ Health. 2020;83:233–48.
Wise J, Wise JP. A review of the toxicity of chemical dispersants. Rev Environ Health. 2011;26:281–300.
Anderson SE, Franko J, Lukomska E, Meade BJ. Potential immunotoxicological health effects following exposure to COREXIT 9500A during cleanup of the Deepwater Horizon oil spill. J Toxicol Environ Health A. 2011;74:1419–30.
Roberts JR, Reynolds JS, Thompson JA, Zaccone EJ, Shimko MJ, Goldsmith WT, Jackson M, McKinney W, Frazer DG, Kenyon A, Kashon ML, Piedimonte G, Castranova V, Fedan JS. Pulmonary effects after acute inhalation of oil dispersant (COREXIT EC9500A) in rats. J Toxicol Environ Health A. 2011;74:1381–96.
Castranova V. Bioactivity of oil dispersant used in the Deepwater Horizon cleanup operation. J Toxicol Environ Health A. 2011;74:1367.
Krajnak K, Kan H, Waugh S, Miller GR, Johnson C, Roberts JR, Goldsmith WT, Jackson M, McKinney W, Frazer D, Kashon ML, Castranova V. Acute effects of COREXIT EC9500A on cardiovascular functions in rats. J Toxicol Environ Health A. 2011;74:1397–404.
Sriram K, Lin GX, Jefferson AM, Goldsmith WT, Jackson M, McKinney W, Frazer DG, Robinson VA, Castranova V. Neurotoxicity following acute inhalation exposure to the oil dispersant COREXIT EC9500A. J Toxicol Environ Health A. 2011;74:1405–18.
Johnston JE, Lim E, Roh H. Impact of upstream oil extraction and environmental public health: a review of the evidence. Sci Total Environ. 2019;657:187–99.
Meo SA, Al-Drees AM, Meo IM, Al-Saadi MM, Azeem MA. Lung function in subjects exposed to crude oil spill into sea water. Mar Pollut Bull. 2008;56:88–94.
Geller LI, Sakaeva SZ, Musina SS, Ostrovskaia RS, Belomyttseva LA, IaD K, Luk’ianova IS, IaP V, Popova RM, Moskatel’nikova EV. The prevalence of cardiovascular diseases among workers of some branches in oil industry on the role of occupational factors in the development of diseases of the cardiovascular system (Russian). Gig Tr Prof Zabol. 1965;9:11–7.
Gimranova GG, Bakiirov AB, Karimova LK. Complex evaluation of work conditions and health state of oil industry workers (Russian). Med Tr Prom Ekol. 2009:1–5.
Toxicological profile for polycyclic aromatic hydrocarbons. In: Agency for toxic substances and disease registry. https://wwwn.cdc.gov/TSP/ToxProfiles/ToxProfiles.aspx?id=122&tid=25. Accessed 18 Jan 2023.
Agency for Toxic Substances and Disease Registry, 2007. Toxicological profile for benzene. https://www.atsdr.cdc.gov/toxprofiledocs/index.html?id=40&tid=14. Accessed 27 June 2023.
McKinney W, Jackson MC, Law B, Fedan JS. Automated oil vapor inhalation exposure system. Inhal Toxicol. 2022;34:1–10.
Pérez CA, Bosia JD, Cantore MS, Chiera A, Cocozzella DR, Adrover RE, Borzi S, Curciarello JO. Liver damage in workers exposed to hydrocarbons. Gastroenterol Hepatol. 2006;29:334–7.
Anakwue AM, Anakwue R, Okeji M, Idigo F, Agwu K, Nwogu U. Sonographic assessment of petroleum-induced hepatotoxicity in Nigerians: does biochemical assessment underestimate liver damage? Afr Health Sci. 2017;17:270–7.
Robledo RF, Barber DS, Witten ML. Modulation of bronchial epithelial cell barrier function by in vitro jet propulsion fuel 8 exposure. Toxicol Sci. 1999;51:119–25.
Ritchie GD, Still KR, Alexander WK, Nordholm AF, Wilson CL, Rossi J, Mattie DR. A review of the neurotoxicity risk of selected hydrocarbon fuels. J Toxicol Environ Health B Crit Rev. 2001;4:223–312.
American Petroleum Institute. The relationship between the aromatic ring class content and selected endpoints of repeat-dose and developmental toxicity of high-boiling petroleum substances. 2008. http://www.petroleumhpv.org/~/media/PetroleumHPV/Documents/Publications/2008_mar31_pac_report.pdf. Accessed 27 June 2023.
American Petroleum Institute. Petroleum high production volume testing group. Crude Oil. 2018. www.petroleumhpv.org/ (website no longer available).
Disbennett DB, Kane ML. Health-related research at the American Petroleum Institute. Occup Med. 1988;3:569–80.
Gaworski CL, MacEwen JD, Vernot EH, Haun CC, Leahy HF. Evaluation of 90-day inhalation toxicity of petroleum and oil-shale diesel fuel marine (DFM). Final technical report, November 1977-January 1985. 1985. https://www.osti.gov/biblio/6072150. Accessed 27 June 2023.
Ngodigha EM. Haematological characteristics and performance of West African dwarf goats fed crude oil contaminated forage. Afr J Biotechnol. 2009;8:699–348.
Feuston MH, Mackerer CR, Schreiner CA, Hamilton CE. Systemic toxicity of dermally applied crude oils in rats. J Toxicol Environ Health. 1997;51:387–99.
Leighton FA. The systemic toxicity of Prudhoe Bay crude and other petroleum oils to CD-1 mice. Arch Environ Contam Toxicol. 1990;19:257–62.
Feuston MH, Low LK, Hamilton CE, Mackerer CR. Correlation of systemic and developmental toxicities with chemical component classes of refinery streams. Fund Appl Toxicol. 1994;22:622–30.
Sasser LB, Lundstrom DL, Zangar RC, Springer DL, Mahlum DD. Elevated blood pressure and heart rate in rats exposed to a coal-derived complex organic mixture. J Appl Toxicol. 1989;9:47–52.
Di Toro DM, McGrath JA, Stubblefield WA. Predicting the toxicity of neat and weathered crude oil: toxic potential and the toxicity of saturated mixtures. Environ Toxicol Chem. 2007;26:24–36.
Patterson J, Maier A, Vincent M, Dourson M. Peer consultation on relationship between PAC profile and toxicity of petroleum substances. Reg Toxicol Pharmacol. 2013;67(Suppl):S86-93.
Amor-Carro Ó, White KM, Fraga-Iriso R, Mariñas-Pardo LA, Núñez-Naveira L, Lema-Costa B, Villarnovo M, Verea-Hernando H, Ramos-Barbón D. Airway hyperresponsiveness, inflammation, and pulmonary emphysema in rodent models designed to mimic exposure to fuel oil-derived volatile organic compounds encountered during an experimental oil spill. Environ Health Perspect. 2020;128:27003–14.
Agency for Toxic Substances and Disease Registry, 1999. Toxicological profile for total petroleum hydrocarbons (TPH). https://www.atsdr.cdc.gov/toxprofiledocs/index.html?id=424&tid=75. Accessed 27 June 2023.
Agency for Toxic Substances and Disease Registry, 2016. Toxicological profile for hydrogen sulfide and carbonyl sulfide. https://www.atsdr.cdc.gov/toxprofiles/tp114.pdf. Accessed 27 June 2023.
Fedan JS, Thompson JA, Russ KA, Dey RD, Reynolds JS, Kashon ML, Jackson MC, McKinney W. Biological effects of inhaled crude oil vapor II. Pulmonary effects. Toxicol Appl Pharmacol. 2022;450:116154.
Krajnak K, Russ KA, McKinney W, Waugh S, Zheng W, Kan W, Kashon ML, Cumpston J, Fedan JS. Biological effects of inhaled vapors from crude oil IV. Cardiovascular effects. Toxicol Appl Pharmacol. 2022;447:116071.
Sager TM, Joseph P, Umbright CM, Hubbs AF, Barger M, Kashon ML, Fedan JS, Roberts JR. Biological effects of inhaled crude oil vapor. III. Pulmonary inflammation, cytotoxicity, and gene expression profile. Inhal Toxicol. 2023;18:1–13. https://doi.org/10.1080/08958378.2023.2224394.
Sriram K, Lin GX, Jefferson AM, McKinney W, Jackson MC, Cumpston JL, Cumpston JB, Leonard HD, Kashon ML, Fedan JS. Biological effects of inhaled crude oil vapor. VI. Altered biogenic amine neurotransmitters and neural protein expression. Toxicol Appl Pharmacol. 2022;449:116137.
Kolicheski A, Turcano P, Tamvaka N, McLean PJ, Springer W, Savica R, Rossa OA. Early-onset Parkinson’s disease: creating the right environment for a genetic disorder. J Parkinsons Dis. 2022;12:2353–67.
Weatherly LM, Shane HL, Baur R, Lukomska E, Roberts JR, Fedan JS, Anderson SE. Biological effects of inhaled crude oil vapor. V. Immunotoxicity. Toxicol Appl Pharmacol. 2022;449:116100.
Khan S, Irfan M, Rahimtula AD. The hepatotoxic potential of a Prudhoe Bay crude oil: effect on mouse liver weight and composition. Toxicology. 1987;46:95–105.
Adedara IA, Farombi EO. Lack of recovery from hepatic oxidative damage in rats treated with Nigerian bonny light crude oil. Cell Biochem Funct. 2012;30:480–6. https://doi.org/10.1002/cbf.2823.
Oruambo IF, Jones AB. Alterations in the concentrations of liver mitochondrial DNA, cytoplasmic total hydrocarbon and calcium in guinea pigs after treatment with Nigerian light crude oil. Int J Environ Res Public Health. 2007;4:23–7.
González-Jasso E, López T, Lucas D, Berthou F, Manno M, Ortega A, Albores A. CYP2E1 regulation by benzene and other small organic chemicals in rat liver and peripheral lymphocytes. Compar Study Toxicol Lett. 2003;144:55–67.
Malaguarnera G, Cataudella E, Giordano M, Nunnari G, Chisari G, Malaguarnera M. Toxic hepatitis in occupational to solvents. Rev World J Gastroenterol. 2012;18:2756–66.
Bolden AL, Schultz K, Pelch KE, Kwiatkowski CF. Exploring the endocrine activity of air pollutants associated with unconventional oil and gas extraction. Environ Health. 2018;17:26.
Davidson CJ, Hannigan JH, Bowen SE. Effects of inhaled combined benzene, toluene, ethylbenzene, and xylenes (BTEX): toward an environmental exposure model. Rev Environ Toxicol Pharmacol. 2021;81:103518.
Feuston MH, Hamilton CE, Schreiner CA, Mackerer CR. Developmental toxicity of dermally applied crude oils in rats. J Toxicol Environ Health. 1997;52:79–93.
Kahn S, Rahman AM, Payne JF, Rahimtula AD. Mechanisms of petroleum hydrocarbon toxicity: studies on the response of rat liver mitochondria to Prudhoe Bay Alaska USA crude oil and its aliphatic and heterocyclic fractions. Toxicology. 1986;42:131–42.
Kim Y, Jeong J, Chatterjee N, Yim UH, Kwon JH, Park MS, Choi J. Activation of the nucleotide excision repair pathway by crude oil exposure: a translational study from model organisms to the Hebei Spirit Oil Spill Cohort. Environ Pollut. 2019;254(Pt B):112997.
Bowen L, Riva F, Mohr C, Aldridge B, Schwartz J, Miles AK, Stott JL. Differential gene expression induced by exposure of captive mink to fuel oil: a model for the sea otter. EcoHealth. 2007;4:298–309.
Arcaro KF, Gierthy JF, Mackerer CR. Antiestrogenicity of clarified slurry oil and two crude oils in a human breast-cancer cell assay. J Toxicol Environ Health A. 2001;62:505–21.
Yilmaz B, Ssempebwa J, Mackerer CR, Arcaro KF, Carpenter DO. Effects of polycyclic aromatic hydrocarbon-containing oil mixtures on generation of reactive oxygen species and cell viability in MCF-7 breast cancer cells. J Toxicol Environ Health A. 2007;70:1108–15.
Dalbey W, Osimitz T, Kommineni C, Roy T, Feuston M, Yang J. Four-week inhalation exposures of rats to aerosols of three lubricant base oils. J Appl Toxicol. 1991;11:297–302.
Skyberg K, Skaug V, Gylseth B, Pedersen JR, Iversen OH. Subacute inhalation toxicity of mineral oils, C15–C20 alkylbenzenes, and polybutene in male rats. Environ Res. 1990;53:48–61.
Valdiglesias V, Kiliç G, Costa C, Amor-Carro O, Mariñas-Pardo L, Ramos-Barbón D, Méndez J, Pásaro E, Laffon B. In vivo genotoxicity assessment in rats exposed to Prestige-like oil by inhalation. J Toxicol Environ Health A. 2012;75:756–64.
Khan S, Payne JF, Rahimtula AD. Mechanisms of petroleum hydrocarbon toxicity: functional changes in rat liver mitochondria after exposure to a Prudhoe Bay crude oil. Toxicol Lett. 1986;32:141–6.
Khan S, Payne JF, Rahimtula AD. Mechanisms of petroleum hydrocarbon toxicity: destruction of liver microsomal and mitochondrial calcium pump activities by a Prudhoe Bay crude oil. J Biochem Toxicol. 1986;1:31–43.
Amat-Bronnert A, Castegnaro M, Pfohl-Leszkowicz A. Genotoxic activity and induction of biotransformation enzymes in two human cell lines after treatment by Erika fuel extract. Environ Toxicol Pharmacol. 2007;23:89–95.
Nagy E, Noren UG, Zeisig M, Ekstrom LG, Moller L. DNA adduct formation and physiological effects from crude oil distillate and its derived base oil in isolated, perfused rat liver. Arch Toxicol. 2004;78:114–21.
Ovuru SS, Ezeasor DN. Morphological alterations in liver tissues from rabbits exposed to crude oil contaminated diets. Bull Environ Contam Toxicol. 2004;73:132–8.
Suleiman SA. Petroleum hydrocarbon toxicity in vitro: effect of n-alkanes, benzene and toluene on pulmonary alveolar macrophages and lysosomal enzymes of the lung. Arch Toxicol. 1987;59:402–7.
Oyebisi MA, Akhigbe RE, Anigbogu CN. Exposure to petroleum hydrocarbon: implications in lung lipid peroxidation and antioxidant defense system in rat. Toxicol Int. 2012;19:306–9.
Azeez OM, Akhigbe RE, Anigbogu CN, Ige SF, Saka WA. Variability in cardiovascular functions and baroflex sensitivity following inhalation of petroleum hydrocarbons. J Cardiovasc Dis Res. 2012;3:99–103.
George SE, Nelson GM, Kohan MJ, Warren SH, Eischen BT, Brooks LR. Oral treatment of Fischer 344 rats with weathered crude oil and a dispersant influences intestinal metabolism and microbiota. J Toxicol Environ Health A. 2001;63:297–316.
Vrabie CM, Candido A, van Duursen MB, Jonker MT. Specific in vitro toxicity of crude and refined petroleum products: II. Estrogen (alpha and beta) and androgen receptor-mediated responses in yeast assays. Environ Toxicol Chem. 2010;29:1529–36.
Anigbogu CN, Ojo O. Cardiovascular function and plasma lipid profiles in rats exposed to petroleum products and water contaminated with hydrocarbons. FASEB J Supple 1. 2009;23.
Burnham K, Bey M. Effects of crude oil and ultraviolet radiation on immunity within mouse skin. J Toxicol Environ Health. 1991;34:83–93.
Farombi EO, Adedara IA, Ebokaiwe AP, Teberen R, Ehwerhemuepha T. Nigerian Bonny light crude oil disrupts antioxidant systems in testes and sperm of rats. Arch Environ Contam Toxicol. 2010;59:166–74.
Mazet JA, Gardner IA, Jessup DA, Lowenstine LJ. Effects of petroleum on mink applied as a model for reproductive success in sea otters. J Wildl Dis. 2001;37:686–92.
Diamante G, Müller D, Amaral G, Menjivar-Cervantes N, Xu EG, Volz DC, Bainy ACD, Schlenk D. Developmental toxicity of hydroxylated chrysene metabolites in zebrafish embryos. Aquat Toxicol. 2017;189:77–86.
Khan AA, Coppock RW, Schuler MM, Sharma AK, Lillie LE. Induction of hepatic cytochrome P-450 and xenobiotic metabolizing enzymes in rats gavaged with an Alberta crude oil. J Toxicol Environ Health. 1989;28:297–307.
Khan AA, Coppock RW, Schuler MM. Effects of multiple exposures of small doses of Pembina Cardium crude oil and diesel in rats. Arch Environ Contam Toxicol. 2001;40:418–24.
Haim A, Kalir A. Enzymatic activity in crude oil contaminated rats. Comp Biochem Physiol. 1986;85:103–5.
Khan AA, Coppock RW, Schuler MM, Geleta L. Biochemical changes as early stage systemic biomarkers of petroleum hydrocarbon exposure in rats. Toxicol Lett. 2002;134:195–200.
Funding
Funding was provided by the National Institute for Occupational Safety and Health, Project Number 7927ZLDC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This review includes descriptions of previously published studies conducted by the authors that involved animal subjects and for which IACUC approval was obtained. This article does not contain any studies with human subjects performed by any of the authors.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health and Prevention. Mention of brand name does not constitute product endorsement.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fedan, J.S., Thompson, J.A., Sager, T.M. et al. Toxicological Effects of Inhaled Crude Oil Vapor. Curr Envir Health Rpt 11, 18–29 (2024). https://doi.org/10.1007/s40572-024-00429-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-024-00429-8