Abstract
Background
Though this is an era of imaging, many women with fetal congenital malformations are presenting beyond 20 weeks of pregnancy posing problems in decision making. This study was undertaken to determine the prevalence of congenital fetal malformations presenting to tertiary health care and to analyse the gestational age at presentation and spectrum of malformations and the clinical and socio-demographic factors.
Material and Methods
This was a retrospective analysis of hospitalised women with diagnosis of congenital fetal malformations (CFM) from January 2017 to December 2017. The data was retrieved from Medical Records Section after due permissions and analysed with respect to socio-demographic status, age, consanguinity, type of congenital anomaly and gestational age at presentation.
Results
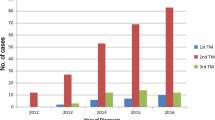
The prevalence of CFM was 1.56%. The majority (64%) of CFM were detected during the second trimester and 27% were detected in the 3rd trimester. The most common anomalies were CNS followed by multiple anomalies and 72% and 65% of them were live born respectively. The majority (90%) belonged to lower middle socioeconomic group and were from rural background (82%). The majority of women were less than 30 years of age (77.6%) and 38% were primigravidae. Consanguinity was present in 34%, medical disorders were associated in 29% and 3% had family history of congenital fetal anomalies.
Conclusion
The most common anomalies were CNS and majority were primigravidae. The most common medical disorder associated was diabetes. It is possible that they are deficient in folic acid and vitamin B12. Hence pre-conceptional control of medical disorders, nutritional counselling regarding intake of micronutrients and awareness programmes to take pre-conceptional folic acid and vitamin B12 are the need of the hour for prevention.
Similar content being viewed by others
References
WHO. Congenital anomalies. Fact sheets. www.who.int
Bhide P, Kar A. A National estimate of the birth prevalence of congenital anomalies in India: systematic review and meta-analysis. BMC Pediatr. 2018;18(1):175. https://doi.org/10.1186/s12887-018-1149-0.
Toufaily MH, Westgate MN, Lin AE, Holmes LB. Causes of congenital malformations. Birth Defects Res. 2018;110(2):87–91. https://doi.org/10.1002/bdr2.1105.
Czeizel AE. Birth defects are preventable. Int J Med Sci. 2005;2(3):91–2. doi: https://doi.org/10.7150/ijms.2.91. Epub 2005 Jul 1. PMID: 16007259; PMCID: PMC1168872.
Canals CA, Cavada CG, Nazer HJ. Identification of risk factors for congenital malformations. Rev Med Chil. 2014;142(11):1431–9. https://doi.org/10.4067/S0034-98872014001100010.
Jain S, Rani V, Sargawan R, Jain N. A demographic profile of women seeking MTP for gross congenital malformations in a tertiary referral hospital in North India. IJRCOG. 2018;7(11):4465–9.
Prema N, Sudhakaran R, Divya BV, Meerabai V, Maharani M. Prevalence and associated factors of congenital anomalies in a tertiary care centre in Tamilnadu. Obg Rev J Obstet Gynecol. 2016;2(4):55–63.
Marwah A, Marwah P. Profile of gross congenital malformations among live newborns and its associated risk factors from a tertiary care rural teaching Institute. Int J Res Med Sci. 2016;4(6):2394–7.
Ara A, Kumar D, Dewan D, Digra NC. Incidence of congenital anomalies in rural population of Jammu. A prospective study. Indian J Public Health. 2018;62:188–92.
Taksande A, Vilhekar K, Chaturvedi P, Jain M. Congenital malformations at birth in Central India: a rural medical college hospital based data. Indian J Hum Genet. 2010;16(3):159–63. https://doi.org/10.4103/0971-6866.73412.
Sarkar S, Patra C, Dasgupta MK, Nayek K, Karmakar PR. Prevalence of congenital anomalies in neonates and associated risk factors in a tertiary care hospital in eastern India. J Clin Neonatol. 2013;2(3):131–4.
Hadzagić-Catibusić F, Maksić H, Uzicanin S, Užičanin S, Heljić S, Zubčević S, et al. Congenital malformations of the central nervous system: clinical approach. Bosn J Basic Med Sci. 2008;8(4):356–60. https://doi.org/10.17305/bjbms.2008.2897.
Dursun A, Zenciroglu A, Hakan N, Karadag N, Karagol BS, Aydin B, et al. Distribution of congenital anomalies in a neonatal intensive care unit in Turkey. J Maternal-Fetal Neonatal Med. 2014;27(10):1069–74.
Ficara A, Syngelaki A, Hammami A, Akolekar R, Nicolaides KH. Value of routine ultrasound examination at 35–37 weeks in detection of fetal abnormalities. Ultrasound Obstet Gynecol. 2020;55:75–80.
Manegold G, Tercanli S, Struben H, Huang D, Kang A. Is a routine ultrasound in the third trimester justified? Additional fetal anomalies diagnosed after two previous unremarkable ultrasound examinations. Ultraschall Med. 2011;32(4):381–6.
Towner D, McGahan J, Rhee-Morris L. The dynamic fetal brain. J Clin Ultrasound. 2007;35:238–44.
Grandjean H, Larroquen D, Levi S. The performance of routine ultrasonographic screening of pregnancies in the Eurofetus study. Am J Obstet Gynecol. 1999;181:446–54.
Boyd PA, Devigan C, Khoshnood B, Loane M, Garne E, Dolk H. Survey of prenatal screening policies in Europe for structural malformations and chromosome anomalies, and their impact on detection and termination rates for neural tube defects and Down’s syndrome. BJOG. 2008;115:689–96.
Estrada CR Jr. Prenatal hydronephrosis: early evaluation. Curr Opin Urol. 2008;18:401–3.
Coelho GM, Bouzada MC, Pereira AK, Figueiredo EF, Leite MR, Olievera DS. Outcome of isolated antenatal hydronephrosis: a prospective cohort study. Pediatr Nephrol. 2007;22:1727–34.
Chaoui R. The four-chamber view: four reasons why it seems to fail in screening for cardiac abnormalities and suggestions to improve detection rate. Ultrasound Obstet Gynecol. 2003;22:3–10.
DeVore GR, Medearis AL, Bear MB, et al. Fetal echocardiography: factors that influence imaging of the fetal heart during the second trimester of pregnancy. J Ultrasound Med. 1993;12:659–63.
Axt-FliednerR Chiriac A, Gembruch U. First and early second trimester fetal heart scanning. Ultrashall Med. 2009;30:364–75.
Lotto R, Smith LK, Armstrong N. Clinicians’ perspectives of parental decision-making following diagnosis of a severe congenital anomaly: a qualitative study. BMJ Open. 2017;7:e014716. https://doi.org/10.1136/bmjopen-2016-014716.
US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. (2017) Folic acid supplementation for the prevention of neural tube defects: US preventive services task force recommendation statement. JAMA. 2017;317(2):183–9. https://doi.org/10.1001/jama.2016.19438.
Wilson RD, Genetics Committee, Wilson RD, et al. Pre-conception folic acid and multivitamin supplementation for the primary and secondary prevention of neural tube defects and other folic acid-sensitive congenital anomalies. J Obstet Gynaecol Can. 2015;37(6):534–52. https://doi.org/10.1016/s1701-2163(15)30230-9
ElKoumi MA, Al Banna EA, Lebda I. Pattern of congenital anomalies in newborn: a hospital-based study. Pediatr Rep. 2013;5:1–5.
Ameen KS, Alaf SK, Shabila NP. Pattern of congenital anomalies at birth and their correlations with maternal charecteristics in the maternity teaching hospital, Erbil city Iraq. BMC Pregnancy Childbirth. 2018;18:501. https://doi.org/10.1186/s12884-018-2141-2.
Author information
Authors and Affiliations
Contributions
Concept and data review, manuscript preparation: PD, Data collection, Data analysis, manuscript preparation: SG. Data analysis and manscript checking AMA.
Corresponding author
Ethics declarations
Conflict of interest
Myself, Papa Dasari and SonalGarg, Ashraf M Ali have no conflicts of interests to declare.
Ethics approval
Not applicable as it is a retrospective study; Approval taken for use of Medical records.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Garg, S., Dasari, P. & Ali, A.M. Clinical Profile of Women with Congenital Fetal Malformations: A Retrospective Cohort Study. J. Fetal Med. 8, 41–48 (2021). https://doi.org/10.1007/s40556-020-00287-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40556-020-00287-y