Abstract
Preterm premature rupture of membranes (PPROM) occurs in up to 3% of all pregnancies. Only few comparative studies have investigated potential risks and benefits between different tocolytic substances in women with PPROM. The aim of this study was to compare the neonatal short term outcome after tocolysis with Atosiban or Hexoprenaline in women with PPROM. This is a retrospective observational cohort study of women with PPROM between 24 and 32 weeks of gestation comparing neonatal and maternal outcome after tocolysis with atosiban or hexoprenaline. Outcome parameters were short term neonatal outcome, maternal tocolytic efficacy, effectiveness and tolerability and neonatal neurodevelopmental long-term outcome. Continuous variables were compared using t-Test or Mann–Whitney U test, as appropriate. For categorical variables Chi-square after Pearson and Fisher exact-test were used to compare the two groups. 93 women were included into this study with 42 women receiving hexoprenaline and 51 women receiving atosiban as primary tocolytic treatment. Mean gestational age was 29 weeks in both groups at the time PPROM. No differences were found for any short term neonatal outcome parameters, tocolytic efficacy, effectiveness and tolerability and neonatal neurodevelopmental long-term outcome. Both hexoprenaline and atosiban do not affect the short and long term neonatal outcome in women with PPROM for the time of lung maturation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preterm premature rupture of membranes (PPROM) is defined as the rupture of the amniotic membranes before 37 weeks of gestation and before the onset of labour [1]. Risk factors are multifactorial and predominantly include infection, smoking, vaginal bleeding, lower socioeconomic background and distension of the uterus [1]. PPROM occurs in up to 3% of all pregnancies and accounts for one-third of all preterm births [2,3,4], which is one of the leading causes for both perinatal morbidity and mortality. Associated perinatal morbidity includes respiratory distress syndrome, intraventricular haemorrhage, necrotizing enterocolitis and infection [4]. Recommended measures are antibiotic prophylaxis to prevent chorioamnionitis and corticosteroid therapy for long maturation. Tocolysis in women with PPROM is controversial because apart from a significant increase in the latency between PPROM and delivery no significant benefits have been proven [4]. However, for the time of lung maturation a temporary tocolysis is often considered as long as there are no signs of intraamniotic infection. Only a few comparative studies have investigated potential risks and benefits between different tocolytic substances in women with PPROM [4,5,6,7]. Most studies compared tocolysis with no tocolysis with betamimetics being the most common tocolytic agent. One study compared nifedipine or terbutaline with no significant differences in neonatal outcome but fewer side effect in the nifedipine group [8]. To date no study has compared differences between betamimetics and Atosiban. Atosiban is an oxytocin inhibitor and is commonly used for tocolysis. In women without PPROM Atosiban was not inferior to betamimetics [9]. The aim of this study was to compare the neonatal short term outcome after tocolysis with Atosiban or Hexoprenaline in women with PPROM between 24 and 31 weeks of gestation. Secondary outcome parameters were tocolytic efficacy, effectiveness and tolerability and neonatal neurodevelopmental long-term outcome.
Materials and Methods
Study Design
This is a retrospective observational cohort study of women with PPROM between 24 weeks 0 days and 31 weeks 6 days of gestation. All women, who presented at the outpatient clinic of the Medical University Graz with PPROM between 2003 and 2013 were included. PPROM was diagnosed clinically by a vaginal and abdominal ultrasound examination and verified by a positive AmniSure (Qiagen GmbH, Germantown, USA). Gestational age was confirmed by either a first trimester ultrasound or the first day of the last menstrual period. Maternal exclusion criteria for were signs of infection or manifest amniotic infection syndrome (AIS), preeclampsia, HELLP syndrome, maternal cardiovascular or liver diseases, and/or placental abruption. Fetal exclusion criteria were antepartum diagnosis of major fetal malformations necessitating termination of pregnancy, any multiple gestations and/or intrauterine death. For the period of lung maturation (2 doses of 12 mg ß-Methasone) [10] tocolysis was performed with either hexoprenaline or atosiban. Tocolytic treatment was assigned according to the physician’s preference or due to exclusion criteria for the specific tocolytic as per manufacturer’s instructions. Hexoprenaline was not given to women with allergy, or in case of asthma with intolerance to sulphite, hyperthyroidism, heart diseases, liver or kidney diseases, and/or narrow angle glaucoma; atosiban was not administered in case of a known allergy. Hexoprenaline was administered as a single intravenous loading dose (5 µg in .9% sodium chloride solution), followed by an intravenous infusion of 18 µg/h for 1 h. The dose was reduced hourly till a dose of 4.3 µg/h was reached and continued for further 44 h. Atosiban was given as a single loading intravenous dose, 6.75 mg in .9% sodium chloride solution, followed by an intravenous infusion of 18 mg/hour in .9% sodium chloride solution for the first 3 h and then 6 mg/hour for 45 h. Tocolysis was discontinued after 48 h of lung maturation. In case of drug failure and/or ongoing contractions within 48 h a crossover to the other tocolytic was performed. Prophylactic antibiotics were administered according to standard; usually up to 7 days after PPROM with a cephalosporin administered intravenously.
Outcome Parameters
The primary outcome parameter was a composite outcome parameter of short term neonatal outcome. The composite outcome consists of necessity of neonatal intensive care unit (NICU), presence of infant respiratory distress syndrome (IRDS), intraventricular haemorrhage (IVH), periventricular haemorrhage (PVH), retinopathy of prematurity (ROP) and neurological behaviour at the time of discharge. Secondary outcome parameters included maternal tocolytic efficacy, effectiveness and tolerability, neonatal short term outcome and neonatal neurodevelopmental long-term outcome. Maternal outcome parameters were defined as follows; tocolytic efficacy was defined as percentage of women, who did not require tocolytic crossover and were not delivered within 2 days after PPROM. Tocolytic effectiveness was defined as percentage of women, who were not delivered within 2 days after PPROM independent of the tocolytic given (even if a switch was necessary). Maternal side effects like palpitation, hypotension, flushing, nausea and vomiting, maternal tachycardia or unspecific side effects were recorded as long as the tocolytic agent was given. Induction of labor was either performed with vaginal dinoproston or systemic oxytocin according to the hospital’s local protocol. In regard to fetal long term outcome parameters the following parameters were analyzed: percentage of NICU admission, IRDS, IVH, PVH, periventricular leukomalacia (PVL), ROP, arterial hypotension and abnormal neurological behaviour. All parameters were defined according to previously described classifications [11,12,13,14,15,16]. With the corrected age of 2 years infants born with very low birth weight or any impairment at time of discharge were invited routinely for a neuro-developmental follow up. Neuro-developmental follow up included clinical examination and if applicable the Bayley Scales of Infant Development (BSID II) as standardised test [17].
Ethical Consideration
The study was approved by the local ethics committee of the Medical University Graz (IRB 26-090 ex 13/14 issued on 20.12.2013); since this is a retrospective chart review no written informed consent was obtained.
Statistical Analysis
Statistical analyses were performed using SPSS Statistics 23. Quantitative data are expressed as means and standard deviations, or median (minimum–maximum), depending on skewness and normality of the data. Continuous variables were compared using t-Test or Mann–Whitney U test, as appropriate. For categorical variables Chi-square after Pearson and Fisher exact-test were used to compare the two groups. Statistical significance was defined as a P value of < .05. Since this is a retrospective study including all available patients at our department no a priori power calculation was performed. A post hoc effect size calculation showed that we can detect an effect of d = .593 with a power of β = .8 using a significance level of α = .05 in the given population.
Results
Demographic Data
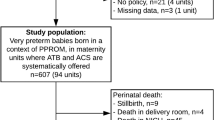
During the study period 121 women presented with PPROM. 28 women were excluded from the study: 17 (14%) had signs of infection or manifest amniotic infection syndrome (AIS), 8 (7%) had intrauterine growth restriction (IUGR) and 3 (2%) had fetal malformations. Out of the 93 women included into this study 42 women received hexoprenaline and 51 women received atosiban as primary tocolytic treatment. All women received initial lung maturation. Demographic parameters at time of PPROM are listed in Table 1. No significant differences were observed for most parameters except body mass index that was lower in the hexoprenaline group. Mean gestational age was 29 weeks in both groups at time of PPROM.
Obstetric Outcome
Table 2 shows the maternal outcome depending on the treatment group. Tocolytic therapy was well tolerated in both treatment groups with no significant differences between the two groups. The most common side effects were heart palpitations, hypotension and tachycardia. Approximately half of the women had normal vaginal delivery; 38% of the women in the hexoprenaline group and 47% in the atosiban group had secondary caesarean section without reaching significant difference between groups.
Tocolytic efficacy and effectiveness is presented in Table 3. In the total study group both tocolytic agents showed efficacy and effectiveness in approximately 50% of the cases; half of the neonates were delivered within 48 h of PPROM independently of medication. No significant differences were observed for the onset of labor after 28 weeks of gestation between the two treatment groups.
Short-term Neonatal Outcome
Neonatal outcome parameters are listed in Table 4. Length, weight and head circumferences were around the 50th centile with no significant differences between the two groups. Neither were there any differences for the Apgar scores or the umbilical cord blood values. None of the included neonates died. Neonatal morbidities did not show any significant differences between the two groups. At time of discharge from the hospital 13% of the infants in the hexoprenaline group and 9% in the atosiban group showed any form of neurological impairment, however without reaching significant difference between the groups. The primary outcome parameter- composite neonatal outcome as described above- did also not show a significant difference between the two groups.
Long-term Neonatal Outcome
In 37 infants a 2 year neuro-developmental follow up was performed (Supplementary Table 1). 11 out of 20 infants in the Hexoprenaline group (52%) and 5 out 16 (31%) in the atosiban group (p = .436) showed any form of neurodevelopmental impairment. The impairment was further classified into mild and severe disabilities; only 4/21 (19%) and 2/16 (13%) showed severe impairment in the hexoprenaline and atosiban group, respectively. The Bayley II test was performed in 54% of the infants; the results are also presented in supplementary Table 1. In the hexoprenaline group half of the infants showed mild impairment; the other half had normal test results. In the atosiban group only one infant had severe impairment, most infants did not show any impairment at 2 years with none of the results being significantly different.
Discussion
This retrospective observational cohort study was designed to investigate neonatal and maternal outcome parameters in women with PPROM treated with two different tocolytic agents: hexopreanline and atosiban. No differences were found for any short term neonatal outcome paramter; neither were there any differences for any of the secondary outcome parameters including tocolytic efficacy, effectivness and tolerability and neonatal neurodevelopmental long-term outcome.
Although evidence is conflicting [4], tocolysis after PPROM is recommended in some guidelines to prolong pregnancy to allow for lung maturation in the absence of infection [18]. In case of preterm labour betamimetics have been shown to realiably postpone preterm labour for 48 h, however, maternal side effects are often considerable [19]. Atosiban has been shown to have fewer side effects with similar tocolytic efficiacy and was suggested to be considered as first-line tocolysis in Europe, where it is currently licensed [20, 21]. In our study maternal side effects were quite low and not different between the two groups. However, since this is a retrospective analysis some side effects might not have been documented sufficiently.
This is the first study to report on differences in neonatal outcome after hexoprenaline or atosiban tocolysis in case of PPROM. Tocolytic therapy especially in PPROM is constantly under debate. Our data suggest that tocolytic therapy has no influence on mortality, since none of the neonates died. The missing mortality at all might be explained by the rather high mean gestational age of the included neonates and the fact that neonates at highest risk like manifest amniotic infection syndrome were excluded. No differences were seen for any short term neonatal outcome parameters between the two treatment groups. Number of neonatal morbidities were comparable to literature [22, 23] suggesting that the tocolytic agents do not affect short term neonatal outcome. However, these results need to be interpreted with caution since the sample size is too small in both groups.
Although neonatal morbidity is lessened with every day of pregnancy prolongation, especially before 28 weeks of gestation, tocolytic therapy was only given for the time of lung maturation. Several studies have demonstrated that longer tocolytic treatment has been associated with an increase of neonatal and maternal side effects [22,23,24].
The long term neuro-developmental outcome after 2 years showed good to moderate development with most of the infants having no or mild impairment; only 13–19% of the infants had severe neurological impairment. However these results need to be interpreted with caution due to the low number of infants with long term follow up. This low number of infants with follow-up is predominantly caused that healthy infants do not attend the developmental outpatient clinic. Larger follow up studies are needed and furthermore to determine any possible effects in the development during adoloscence.
Strengths of the study is the novelty of our data showing both maternal and neonatal outcome after therapy with two different tocolytic agents in women with PPROM.
Limitations of the study are the retrospective design, the relatively small sample size and physician’s choice of the tocolytic agent. This small sample size was caused by excluding patients with co-morbidities that made, however, the groups more homogenous und comparable. In addition both groups were rather similar concerning the outcome parameters suggesting not reaching significant differences with a larger sample size.
Conclusion
In conclusion, both hexoprenaline and atosiban seem to be well tolerated by women with PPROM for the time of lung maturation and do not affect the short and long term neonatal outcome. Larger prospective trials are needed to determine these findings and implications on long term neurodevelopmental effects in pregnancies with PPROM.
References
Parry S, Strauss JF 3rd. Premature rupture of the fetal membranes. N Engl J Med. 1998;338:663–70.
Rubens CE, Sadovsky Y, Muglia L, et al. Prevention of preterm birth: Harnessing science to address the global epidemic. Sci Transl Med. 2014;6:262sr265.
Mercer BM. Preterm premature rupture of the membranes. Obstet Gynecol. 2003;101:178–93.
Mackeen AD, Seibel-Seamon J, Muhammad J, et al. Tocolytics for preterm premature rupture of membranes. Cochrane Database Syst Rev. 2014;2:Cd007062.
de Heus R, Mol BW, Erwich JJ, et al. Adverse drug reactions to tocolytic treatment for preterm labour: prospective cohort study. BMJ. 2009;338:b744.
Doret M, Kayem G. Tocolysis for preterm labor without premature preterm rupture of membranes. J Gynecol Obstet Biol Reprod (Paris). 2016;45:1374–98.
Jorgensen JS, Weile LK, Lamont RF. Preterm labor: current tocolytic options for the treatment of preterm labor. Expert Opin Pharmacother. 2014;15:585–8.
Laohapojanart N, Soorapan S, Wacharaprechanont T, et al. Safety and efficacy of oral nifedipine versus terbutaline injection in preterm labor. J Med Assoc Thail. 2007;90:2461–9.
Papatsonis DN, Flenady V, Liley H. Maintenance therapy with oxytocin antagonists for inhibiting preterm birth after threatened preterm labour. Cochrane Database Syst Rev. 2013;10:CD005938.
Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2006. https://doi.org/10.1002/14651858.CD004454.pub2:Cd004454.
Bell MJ, Ternberg JL, Feigin RD, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
de Vries LS, Eken P, Dubowitz LM. The spectrum of leukomalacia using cranial ultrasound. Behav Brain Res. 1992;49:1–6.
Papile LA, Burstein J, Burstein R, et al. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Rubaltelli FF, Bonafe L, Tangucci M, et al. Epidemiology of neonatal acute respiratory disorders. A multicenter study on incidence and fatality rates of neonatal acute respiratory disorders according to gestational age, maternal age, pregnancy complications and type of delivery. Italian Group of Neonatal Pneumology. Biol Neonate. 1998;74:7–15.
Cooke RW. Factors associated with periventricular haemorrhage in very low birthweight infants. Arch Dis Child. 1981;56:425–31.
Kemper AR, Prosser LA, Wade KC, et al. A comparison of strategies for retinopathy of prematurity detection. Pediatrics. 2016. https://doi.org/10.1542/peds.2015-2256
Bayley N. Bayley scales of infant development: New York. New York: The Psychological Corporation; 1969.
Weiner CP, Renk K, Klugman M. The therapeutic efficacy and cost-effectiveness of aggressive tocolysis for premature labor associated with premature rupture of the membranes. Am J Obstet Gynecol. 1988;159:216–22.
Brownfoot FC, Crowther CA, Middleton P. Different corticosteroids and regimens for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2008. https://doi.org/10.1002/14651858.CD006764.pub2:Cd006764.
Moutquin JM, Sherman D, Cohen H, et al. Double-blind, randomized, controlled trial of atosiban and ritodrine in the treatment of preterm labor: a multicenter effectiveness and safety study. Am J Obstet Gynecol. 2000;182:1191–9.
[Anonymous]. Effectiveness and safety of the oxytocin antagonist atosiban versus beta-adrenergic agonists in the treatment of preterm labour. The Worldwide Atosiban versus Beta-agonists Study Group. BJOG 2001; 108:133–42.
Azria E, Kayem G, Langer B, et al. Neonatal mortality and long-term outcome of infants born between 27 and 32 weeks of gestational age in breech presentation: the EPIPAGE cohort study. PLoS ONE. 2016;11:e0145768.
Costeloe KL, Hennessy EM, Haider S, et al. Short term outcomes after extreme preterm birth in England: comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). BMJ. 2012;345:e7976.
Wolfensberger A, Zimmermann R, von Mandach U. Neonatal mortality and morbidity after aggressive long-term tocolysis for preterm premature rupture of the membranes. Fetal Diagn Ther. 2006;21:366–73.
Acknowledgements
Open access funding provided by Medical University of Graz. All contributing persons are listed as co-authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
There are no conflicts of interest to declare for any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ulrich, D., Schneider, V., Pichler, G. et al. Neonatal Outcome After Hexoprenaline Compared with Atosiban After Preterm Premature Rupture of Membranes. J. Fetal Med. 6, 171–176 (2019). https://doi.org/10.1007/s40556-019-00225-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40556-019-00225-7