Abstract
Purpose
This study aimed to develop and validate a nomogram for predicting the efficacy of transurethral surgery in benign prostatic hyperplasia (BPH) patients.
Methods
Patients with BPH who underwent transurethral surgery in the West China Hospital and West China Shang Jin Hospital were enrolled. Patients were retrospectively involved as the training group and were prospectively recruited as the validation group for the nomogram. Logistic regression analysis was utilized to generate nomogram for predicting the efficacy of transurethral surgery. The discrimination of the nomogram was assessed using the area under the receiver operating characteristic curve (AUC) and calibration plots were applied to evaluate the calibration of the nomogram.
Results
A total of 426 patients with BPH who underwent transurethral surgery were included in the study, and they were further divided into a training group (n = 245) and a validation group (n = 181). Age (OR 1.07, 95% CI 1.02–1.15, P < 0.01), the compliance of the bladder (OR 2.37, 95% CI 1.20–4.67, P < 0.01), the function of the detrusor (OR 5.92, 95% CI 2.10–16.6, P < 0.01), and the bladder outlet obstruction (OR 2.21, 95% CI 1.07–4.54, P < 0.01) were incorporated in the nomogram. The AUC of the nomogram was 0.825 in the training group, and 0.785 in the validation group, respectively.
Conclusion
The nomogram we developed included age, the compliance of the bladder, the function of the detrusor, and the severity of bladder outlet obstruction. The discrimination and calibration of the nomogram were confirmed by internal and external validation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Benign prostatic hyperplasia (BPH) is one of the most common urologic diseases, and it is also one of the main disorders causing lower urinary tract symptoms in aging males [1]. With the increasing life expectancy of male people, the number of elderly patients with BPH is also increasing. To date, transurethral surgery is one of the most effective ways for the treatment of BPH [2]. Whether it is possible to improve their urination status and quality of life through transurethral surgery is one of the most concerning issues for patients and clinicians before surgery. However, the prediction of the recovery of postoperative micturition function mainly depends on the experience of the surgeon. Currently, there are increasing studies focusing on preoperatively predicting the efficacy of BPH surgery; nevertheless, most studies have only applied one predictor for the prediction of the recovery of voiding function in patients with BPH after transurethral surgery [3, 4]. Additionally, previous studies revealed that the efficacy of transurethral surgery is affected by multiple factors [5,6,7]. It is obvious that the degree of influence of each predictor on urination recovery after BPH cannot be determined; besides, there may be a variety of unreported potential factors, thus predicting the patient's surgical outcome via a single predictor may not be ideal. Therefore, identifying predictors with a strong predictive ability and developing a risk model to predict the efficacy of transurethral surgery is of vital importance.
Nomogram is a graphical predictive method that combines different variables to generate a continuous scoring system and calculates the risk probability of a clinical event for each patient [8]. It meets clinical requirements for an integrated model, playing a significant part in the personalized treatment for patients and the prognosis prediction for clinicians. The nomogram has been successfully used in predicting lymph node metastasis and mortality of prostate cancer or bladder cancer in recent years [9, 10]. To date, a nomogram with enough statistical power to predict the recovery of voiding function in patients after surgery has yet to be designed.
In this study, we aimed to identify the predictors for the efficacy of transurethral surgery and establish a novel nomogram with internal and external validation for predicting the efficacy of transurethral surgery in BPH patients using data from the West China Hospital and West China Shang Jin Hospital.
Methods
Study design and participants
Patients included in the training group and the validation group underwent transurethral surgery from January 2019 to June 2022 at West China Hospital, Sichuan University and Shang Jin Hospital. Patients in the training group and validation group underwent greenlight photoselective vaporization of the prostate (PVP) and transurethral resection of the prostate (TURP). Patients who met the following inclusion criteria were recruited in this study: (1) diagnosis of lower urinary tract symptoms due to BPH causing BOO which is refractory to conservative therapy; (2) international prostate symptom scores > 12. The exclusion criteria were as follows: (1) suspect of prostatic or other cancer; (2) diagnosed with a urethral stricture; (3) diagnosis of neurogenic bladder or other neurologic disorder; and (4) history of bladder outlet obstruction surgery.
Data collection and variables recorded
Baseline characteristics included age, body mass index (BMI), lower urinary tract symptoms (LUTS) duration, International Prostate Symptom Score (IPSS), quality of life (QoL) score, history of urinary retention, and comorbidities including hypertension and diabetes. Preoperative characteristics included prostate volume (PV), post-void residual (PVR), and total prostate-specific antigen (tPSA), and urodynamic results included maximum flow rate (Qmax), bladder compliance, the function of detrusor, and the severity of bladder outlet obstruction (BOO). Urodynamic studies were carried out in the sitting position with a Laborie Triton equipment using the air‐charged catheters (Laborie &Co., version: Aquarius TT Triton) following GUP guidelines [11, 12]. We defined detrusor underactivity as a formulated bladder contractility index (BCI = PdetQmax + 5 Qmax) < 100. As for bladder compliance, the compliance was calculated based on the methods described previously [12], and the bladder with compliance < 15 ml/cm H2O was considered as non-compliant [13]. With regard to the BOO, the bladder outlet obstruction index (BOOI) was used (BOOI = PdetQmax − 2Qmax) and BOOI > 40 was considered as obvious BOO [14]. All patients were in a routine visit follow-up at 6 months after discharge, and patients with postoperative IPSSs more than 10 or Qol scores more than 3 and postoperative IPSS decrease < 10 were determined as incomplete recovery [4, 15, 16].
Statistical analysis
Categorical variables were expressed as numbers (percentage) and continuous variables were expressed as medians with ranges or means with standard deviations. Differences in baseline characteristics between groups for continuous variables were assessed using the variance analysis. Multivariate logistic regression analysis with the forward selection method was applied to determine the major predictors in the nomogram. Variables included in the multivariate logistic regression were those with a P value of < 0.05 in the univariate analysis. Variance Inflation Factor (VIF) was utilized for collinearity diagnosis of the covariates in the model, with tolerance < 0.1 and VIF > 4 considered indicative of multicollinearity.
In the nomogram, points were assigned by drawing a vertical line from the corresponding values of each predictor to the “Points” axis. The total point is the cumulative sum of the points assigned to each predictor. The probability of incomplete postoperative recovery is obtained by drawing a vertical line from the “Total points” axis to the “Risk” axis. The discriminative performance of the nomogram was measured by calculating the area under curve (AUC) of the receiver operating characteristic curve (ROC). Calibration was tested using a calibration plot, which described the fitting degree between actual and nomogram-predicted incomplete recovery. Then the nomogram was constructed by using the RMS package in the R (r4.1.3) software to visually score individual risk probabilities.
Results
The flow chart of patient inclusion is presented in Fig. 1. From July 2019 to June 2022, a total of 245 patients treated with transurethral surgery were included in the training group. And a total of 181 patients were included in the validation group. Detailed characteristics of the two groups are shown in Table 1. The number of patients had incomplete recovery in the training group and validation group was 65 (27%) and 52 (28%), respectively.
Univariate analysis detected age (P < 0.01, OR 1.08, 95% CI 1.04–1.12), diabetes (P = 0.020, OR 2.47, 95% CI 1.14–5.31), preoperative gross hematuria (P = 0.02, OR 0.48, 95% CI 0.27–0.87), Qmax (P = 0.017, OR 0.89, 95% CI 0.82–0.98), bladder compliance (P < 0.01, OR 3.96, 95% CI 2.17–7.24), damage of detrusor function (P < 0.01, OR 11.22, 95% CI 4.30–29.20), and the severity of BOO (P < 0.01, OR 4.08, 95% CI 2.21–7.54) as independent predictors for incomplete recovery of urination function (Table 2). After multivariate analysis, four predictors were left, age (P < 0.01, OR 1.07, 95% CI 1.02–1.15), bladder compliance (P < 0.01, OR 2.37, 95% CI 1.20–4.67), detrusor function (P < 0.01, OR 5.92, 95% CI 2.10–16.6), and the severity of BOO (P < 0.01, OR 2.21, 95% CI 1.07–4.54).
Furthermore, the collinearity diagnostic analysis demonstrated that the VIFs of those risk factors were less than 4 (Supplementary Table 1), indicating that there is no strong indication of multicollinearity among variables. Thus, there were four variables included in the final multivariable prediction model as predictors.
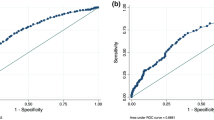
The nomogram was established by assigning a graphic preliminary score to each of the 4 significant predictors with a point ranging from 0 to 100, which was then summed to generate a total point, and finally converted into an individual probability of incomplete recovery of urination function after transurethral surgery (Fig. 2). For example, a patient with age at 65 years, bladder compliance decompensation, detrusor contractility decreased, and severe bladder outlet obstruction would have a total of 71 points (40 points for age, 31 points for bladder compliance, 0 for detrusor, 0 for bladder outlet obstruction). The predicted possibility of unsatisfactory rehabilitation was less than 15% for this patient. We calculated the AUC to investigate the discrimination of the nomogram, which was 0.83 (95% CI 0.77–0.88) in the training group, which indicated a good predictive power (Fig. 3A). For each patient, higher total points indicated a higher risk of unsuccessful surgical outcome. Additionally, the risk score of 125.50 was determined as the optimal cutoff value with the maximum Youden index. The sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio were 0.67 (95% CI, 0.55–0.77), 0.89 (95% CI 0.84–0.94), 6.41 (95% CI 4.03–10.22), and 0.367 (95% CI 0.264–0.51) when this cutoff was applied. Figure 4A shows the comparison of the calibration between the nomogram prediction and actual observation by using a calibration plot. The calibration plot revealed good predictive accuracy of this nomogram. An additional 181 patients were prospectively enrolled as the validation group to validate the new nomogram. The baseline characteristics of the validation group are demonstrated in Table 1. The AUC of the nomogram in the validation group was 0.785 (95% CI 0.713–0.858) (Fig. 3B), and the sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio were 0.67 (95% CI 0.53–0.79), 0.80 (95% CI 0.72–0.86), 3.34 (95% CI 2.26–4.94), and 0.41 (95% CI 0.28–0.61) when the cutoff value of 125.50 was utilized. The good calibration of the nomogram was also confirmed by the validation group (Fig. 4B).
The nomogram model for prediction of efficacy in benign prostatic hyperplasia patients after transurethral surgery. For “compliance,” 1 means better compliance and 2 means lower compliance. As to “detrusor,” 1 means stronger contractility and 2 means weaker contractility. With regard to “BOO,” 1 means obvious BOO and 2 means unclear or non-existent BOO
Discussion
Early in 1993, Kuo et al. revealed that after BPH surgery, part of the patients (19%) cannot achieve a successful result and in 4.5% of patients, the symptoms even worsened [3]. They figured out 9 favorable factors to predict satisfactory surgical outcomes such as the history of acute urinary retention and urodynamically obstructive BPH. However, the history of chronic urinary retention and irritative bladder symptoms alone were identified as unfavorable factors. In recent years, with the development of urodynamics, an increasing number of studies focused on postoperative unsatisfactory urination rehabilitation in BPH patients were reported. Kim et al. revealed that preoperative detrusor underactivity correlated with poorer IPSS and Qmax improvement [4]. However, in a study reported by Myeong et al., 56 patients with BPH and detrusor underactivity were enrolled. After holmium laser enucleation (HoLEP) (24 patients) and transurethral resection of the prostate (TURP) (32 patients), both groups showed significant improvement in the total IPSS and maximal flow rate compared to preoperative characteristics. Based on the result, Myeong inferred that detrusor underactivity may not be a contraindication for HoLEP and TURP [17]. The results of these two studies seemed to be inconsistent. The main reason for such a problem may be that both studies predicted the efficacy of urination function after surgery with only one or two predictors. Nevertheless, there are many other influencing factors such as age, bladder compliance, and the history of AUR. Therefore, the prediction was not ideal. In 2015, De Nunzio et al. developed a nomogram for the diagnosis of BPH (the Young Academic Urologist nomogram, YAU nomogram), which have two prediction factors: Qmax and transitional zone volume [18]. Then YAU nomogram was applied to the prediction of clinical outcome of Italian patients treated with TURP and this nomogram achieve good results with an area under the curve of 0.77 [19]. However, only part of urodynamic factors were included in their study which means the bladder function was not fully considered. Young et al. have analyzed the data from UPSTREAM trail and pointed out that transurethral surgery was more beneficial in those with bladder outlet obstruction index > 47.6, and bladder contractility index > 123.0, which is consistent with our study [20, 21]. Our study aims to develop and validate a model for predicting the probability of postoperative urination unsatisfactory rehabilitation. And our data showed that age, bladder compliance, detrusor function, and the severity of bladder outlet obstruction were significant and independent predictors for postoperative urination unsatisfactory rehabilitation which is consistent with previous studies.
Choi et al. studied 116 men with symptomatic BPH requiring surgery, they found that patients in the persistent storage symptom-positive group were older than those in the storage symptom-negative group [22]. This finding was also confirmed by the nomogram reported by De Nunzio et al [15]. Both of them conclude that age is an independent predictor for poor TURP outcome. Previous studies have revealed that age may lead to functional changes in bladder compliance and detrusor. The multicollinearity diagnosis in our study indicated that there is no multicollinearity between age, bladder compliance, detrusor function, and BOO. Based on the results of our multicollinearity diagnosis and previous studies, we considered age as an independent predictor for poor TURP outcome.
Bladder compliance decompensation is a common function change secondary to BPH, leading to reduced capacity or increased post-void residual. Clinical studies revealed that bladder compliance significantly correlates with LUTS in the elderly population. It was shown that decreased blood flow and the changed ratio of collagens in the human bladder significantly correlate with reduced bladder compliance [23, 24]. The predictive value of bladder compliance was also validated in our study.
Detrusor underactivity is widely perceived as contributing to poor surgical treatment outcomes [4, 25]. Cho et al. pointed out that deterioration of voiding symptoms at long-term follow-up visits after HoLEP is more significant in LUTS/BPH patients with DU [26]. Currently, the possible mechanism of low detrusor contractility may be that the detrusor muscle fibers are disordered or even broken after long-term BPH which leads to a lower detrusor muscle-to-collagen ratio, and changes in collagen and muscle quantity [27]. Our data also confirmed that better detrusor contractility was associated with better surgical outcomes of TURP.
BOO is one of the most important components to assess in patients with LUTS/BPH. Currently, it is widely acknowledged that preoperative identification of BOO is the prerequisite and key point for successful postoperative surgical outcomes. Schneider et al. concluded in a meta-analysis that a significant association between urodynamic BOO and better improvements in all treatment outcome parameters such as IPSSs, QoL scores, Qmax, and PVR [28]. However, Masumori et al. reported that although the IPSS in patients without BOO deteriorated faster than in those with it, two-thirds of patients with DUA but not BOO were satisfied with their urinary condition at 12 years [29]. In a word, BOO was able to be used as a valuable predictor, but surgery was also reasonable for patients with insignificant BOO, which was consistent with our results.
Limitation
Our study has several limitations that should be noted. First, patients who underwent TURP and PVP were included, while patients treated with HoLEP were not included, which may weaken the universality of the model. Second, although we have collected as many predictors as possible, some potential predictors associated with successful surgical outcomes were not available, such as prostatic urethral length and bladder wall thickness [30]. Third, the history of medication for LUTS/BPH was not meticulously classified, which may weaken the predictive value of this predictor. Finally, more patients with varied clinical characteristics especially larger prostate volume should be included in our training group in order to improve our prediction model.
Conclusion
In conclusion, our nomogram composed of age, bladder compliance, detrusor contractility, and BOO may predict the efficacy of TURP and PVP. The AUC of this nomogram indicates a superior discriminative ability. The discrimination and calibration of the nomogram were confirmed in internal and external validation.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
Devlin CM, Simms MS, Maitland NJ (2021) Benign prostatic hyperplasia—what do we know? BJU Int 127:389–399
Miernik A, Gratzke C (2020) Current treatment for benign prostatic hyperplasia. Dtsch Arztebl Int 117:843–854
Kuo HC, Chang SC, Hsu T (1993) Predictive factors for successful surgical outcome of benign prostatic hypertrophy. Eur Urol 24:12–19
Kim M, Jeong CW, Oh SJ (2018) Effect of preoperative urodynamic detrusor underactivity on transurethral surgery for benign prostatic hyperplasia: a systematic review and meta-analysis. J Urol 199:237–244
Wu SY, Kuo HC (2020) Predictive factors for recovery of voiding function after transurethral prostate surgery in men with small prostate volume and very low detrusor contractility. Low Urin Tract Symptoms 12:41–46
Plata M, Santander J, Trujillo CG et al (2021) Impact of detrusor underactivity on the postoperative outcomes after benign prostatic enlargement surgery. Neurourol Urodyn 40:868–875
Zhu Y, Zhao Y, Zhong P et al (2021) Detrusor underactivity influences the efficacy of TURP in patients with BPO. Int Urol Nephrol 53:835–841
Hiremath A, Shiradkar R, Fu P et al (2021) An integrated nomogram combining deep learning, Prostate Imaging-Reporting and Data System (PI-RADS) scoring, and clinical variables for identification of clinically significant prostate cancer on biparametric MRI: a retrospective multicentre study. Lancet Digit Health 3:e445–e454
Wu S, Zheng J, Li Y et al (2017) A radiomics nomogram for the preoperative prediction of lymph node metastasis in bladder cancer. Clin Cancer Res 23:6904–6911
Zelic R, Garmo H, Zugna D et al (2020) Predicting prostate cancer death with different pretreatment risk stratification tools: a head-to-head comparison in a nationwide cohort study. Eur Urol 77:180–188
Drake MJ, Doumouchtsis SK, Hashim H et al (2018) Fundamentals of urodynamic practice, based on International Continence Society good urodynamic practices recommendations. Neurourol Urodyn 37:S50-s60
Rosier P, Schaefer W, Lose G et al (2017) International Continence Society Good Urodynamic Practices and Terms 2016: urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol Urodyn 36:1243–1260
Abrams P, Cardozo L, Fall M et al (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol 187:116–126
van Dort W, Rosier P, Geurts BJ et al (2023) Quantifying bladder outflow obstruction in men: a comparison of four approximation methods exploiting large data samples. Neurourol Urodyn 42:1628–1638
De Nunzio C, Lombardo R, Cicione A et al (2020) The role of bladder wall thickness in the evaluation of detrusor underactivity: development of a clinical nomogram. Neurourol Urodyn 39:1115–1123
Osman NI, Chapple CR, Abrams P et al (2014) Detrusor underactivity and the underactive bladder: a new clinical entity? A review of current terminology, definitions, epidemiology, aetiology, and diagnosis. Eur Urol 65:389–398
Woo MJ, Ha YS, Lee JN et al (2017) Comparison of surgical outcomes between holmium laser enucleation and transurethral resection of the prostate in patients with detrusor underactivity. Int Neurourol J 21:46–52
De Nunzio C, Lombardo R, Gacci M et al (2015) The diagnosis of benign prostatic obstruction: validation of the young academic urologist clinical nomogram. Urology 86:1032–1036
CDEN, Lombardo R, Nacchia A et al (2018) Young Academic Urologists’ benign prostatic obstruction nomogram predicts clinical outcome in patients treated with transurethral resection of prostate: an Italian cohort study. Minerva urologica e nefrologica Ital J Urol Nephrol 70:211–217
Lewis AL, Young GJ, Abrams P et al (2019) Clinical and patient-reported outcome measures in men referred for consideration of surgery to treat lower urinary tract symptoms: baseline results and diagnostic findings of the Urodynamics for Prostate Surgery Trial; Randomised Evaluation of Assessment Methods (UPSTREAM). Eur Urol Focus 5:340–350
Young GJ, Metcalfe C, Lane JA et al (2022) Prostate surgery for men with lower urinary tract symptoms: do we need urodynamics to find the right candidates? Exploratory findings from the UPSTREAM trial. Eur Urol Focus 8:1331–1339
Choi H, Kim JH, Shim JS et al (2014) Prediction of persistent storage symptoms after transurethral resection of the prostate in patients with benign prostatic enlargement. Urol Int 93:425–430
Sharma S, Rajani S, Hui J et al (2022) Development of enzymatic-resistant and compliant decellularized extracellular matrixes via aliphatic chain modification for bladder tissue engineering. ACS Appl Mater Interfaces 14:37301–37315
Zwaans BMM, Grobbel M, Carabulea AL et al (2022) Increased extracellular matrix stiffness accompanies compromised bladder function in a murine model of radiation cystitis. Acta Biomater 144:221–229
Kiba K, Akashi Y, Yamamoto Y et al (2022) Clinical features of detrusor underactivity in elderly men without neurological disorders. Low Urin Tract Symptoms 14:193–198
Cho MC, Yoo S, Park J et al (2019) Effect of preoperative detrusor underactivity on long-term surgical outcomes of photovaporization and holmium laser enucleation in men with benign prostatic hyperplasia: a lesson from 5-year serial follow-up data. BJU Int 123:E34-e42
Namitome R, Takei M, Takahashi R et al (2020) A prediction model of detrusor underactivity based on symptoms and noninvasive test parameters in men with lower urinary tract symptoms: an analysis of a large group of patients undergoing pressure-flow studies. J Urol 203:779–785
Schneider AJ, Grimes M, Lyon W et al (2021) Cluster analysis of men undergoing surgery for BPH/LUTS reveals prominent roles of both bladder outlet obstruction and diminished bladder contractility. PLoS One 16:e0251721
Masumori N, Furuya R, Tanaka Y et al (2010) The 12-year symptomatic outcome of transurethral resection of the prostate for patients with lower urinary tract symptoms suggestive of benign prostatic obstruction compared to the urodynamic findings before surgery. BJU Int 105:1429–1433
Kim BS, Ko YH, Song PH et al (2019) Prostatic urethral length as a predictive factor for surgical treatment of benign prostatic hyperplasia: a prospective, multiinstitutional study. Prostate Int 7:30–34
Funding
This study is funded by Sichuan Province Regional Innovation Cooperation Project (2023YFQ0015) and the 1.3.5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (23HXFH028).
Author information
Authors and Affiliations
Contributions
Zhu-Feng Peng, Liang-Ren Liu, and Qiang Dong contributed to conception and design. Kai Ma, Lin-Chun Wang, Yun-Fei Yu, and Jun-Hao Chen extracted data. Jing Zhou, Pan Song, Lu-Cheng Yang, Zheng-Huan Liu, and Sheng-Zhuo Liu analyzed and interpreted data. Jing Zhou, Lu-Chen Yang and Zhu-Feng Peng drafted the manuscript. Zhu-Feng Peng, Liang-Ren Liu, and Qiang Dong performed supervision. All authors read and agree to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Informed consent
After full communication, informed consent was obtained from each patient and patients who disagreed were excluded.
Statement of human and animal rights
This study was conducted following the principles of the Declaration of Helsinki and was approved by the Ethics Committee on Biomedical Research, West China Hospital of Sichuan University (Approval No. 2022-356).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhou, J., Peng, ZF., Yang, LC. et al. Nomogram predicting the efficacy of transurethral surgery in benign prostatic hyperplasia patients. Aging Clin Exp Res 36, 71 (2024). https://doi.org/10.1007/s40520-024-02708-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40520-024-02708-8