Abstract
Background
Osteoporotic-related fractures represent an increasing burden to patients, health care systems and society.
Aims
This study estimated cost-effectiveness of sequential treatment with abaloparatide (ABL) followed by alendronate (ALN) compared to relevant alternative strategies in US men and women aged 50 to 80 years at very high fracture risk (bone mineral density T-score ≤ − 2.5 and a recent fracture).
Methods
A lifetime Markov-based microsimulation model was used to estimate healthcare costs and quality-adjusted life years (QALYs). Comparators were sequential treatment with unbranded teriparatide (TPTD)/ALN, generic ALN monotherapy, and no treatment. Analyses were conducted based on initial fracture site (hip, vertebral, or any fracture) and treatment efficacy data (derived from clinical trials or a recent network meta-analysis).
Results
From all analyses completed, sequential ABL/ALN demonstrated more QALYs for lower healthcare costs versus unbranded TPTD/ALN. No treatment was dominated (higher costs for less QALYs) versus ALN monotherapy. Sequential ABL/ALN resulted in favorable cost-effectiveness (at US threshold of $150,000/QALY) versus generic ALN monotherapy in men aged ≥ 50 years with any fracture type, women aged ≥ 65 years with any fracture type, and women aged ≥ 55 years having a hip or vertebral fracture.
Discussion
Similar cost-effectiveness of sequential ABL/ALN versus unbranded TPTD/ALN, ALN monotherapy, and no treatment was observed in both US men and women at very high fracture risk, with a moderate improvement in cost-effectiveness in men versus women and in patients with a hip or vertebral fracture.
Conclusions
Sequential therapy with ABL/ALN was cost-effective in US men and women at very high risk of fractures.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Osteoporotic-related fractures represent a massive and increasing burden on patients, healthcare systems, policymakers, and society. It is estimated that one out of four men and one out of two women aged 50 years will have an osteoporotic fracture during their remaining lifetime [1, 2]. Fractures, especially at the hip or spine, are associated with increased morbidity, mortality excess, and have a significant impact on quality of life. In 2016, 2.1 million osteoporotic fractures occurred among US Medicare patients: 25% at the spine and 17% at the hip [3]. In the 27 countries of the European Union as well as the United Kingdom and Switzerland, the number of fragility fractures in 2019 was estimated at 4.3 million in people aged ≥ 50 years, of which about 30% occurred in men [4]. The total economic burden of these fractures was estimated at €57 billion. With increasing life expectancy, the number of fractures is anticipated to increase by 25% in the next 15 years, and even more so in men [4]. The substantial and increasing burden of osteoporosis in men has revealed the critical need to identify and manage what was thought to be a disease primarily of women.
It is further recognized that the risk of subsequent fractures increases significantly after an initial fracture [5]. Patients with at least one previous fragility fracture with a diagnosis of osteoporosis are considered at very high risk of subsequent fractures [6,7,8]. Despite this population being most likely to sustain a new fracture, a vast majority is not receiving an osteoporosis medication [4, 9]. Recently, an expert working group [8] has recommended the use of sequential treatment for patients found to be at very high risk, beginning with an anabolic and followed by maintenance therapy using an antiresorptive agent, in line with clinical studies showing a better risk reduction with sequential treatment compared to an antiresorptive agent alone [10, 11]. Sequential therapies, however, are more expensive, and economic evaluations are therefore increasingly important to inform decision makers about the potential economic value of this strategy [12]. A recent systematic review of cost-effectiveness analyses of sequential therapies published with data to June 2022 [13] identified a few studies that suggested the cost-effectiveness of sequential treatment with either abaloparatide (ABL) or romosozumab in populations at very high risk. All the studies included in this review were, however, conducted in postmenopausal women with osteoporosis. Another recent systematic review of cost-effectiveness studies conducted in men with osteoporosis [14] found that economic evaluations in men are lacking compared to studies in women and that there is limited information on the comparability of the cost-effectiveness of drugs between men and women.
Recently, we showed the cost-effectiveness of sequential therapy with ABL followed by alendronate (ALN) in US men at high risk of fracture [12]. Although results were rather similar to what was observed in postmenopausal women with osteoporosis [15, 16], it is difficult to make a direct comparison of studies between men and women, as several model parameters are different, including various populations, fracture risk, fracture costs and different model assumptions such as adherence scenarios, time-dependent risk of subsequent fractures, or drug prices. A direct comparison using a systematic approach would reveal whether the cost-effectiveness of sequential ABL/ALN is similar in both men and women at very high risk of fractures. Integrating gender into cost-effectiveness analyses is necessary to build rigorous evidence to capture a more accurate picture of the economic impact of sequential therapy, with potential implications on healthcare decision-making and health inequalities between genders in particular. This study was therefore designed to assess and compare the cost-effectiveness of sequential treatment with ABL followed by ALN to alternative strategies in US men and women at very high fracture risk.
Methods
Interventions
This study compared lifetime healthcare costs and health outcomes expressed as quality-adjusted life years (QALYs) of sequential ABL/ALN compared to sequential unbranded teriparatide (TPTD)/ALN, generic ALN monotherapy, and no treatment. No treatment is included as a comparator as many patients at very high risk of fracture are not receiving a medication for osteoporosis. In line with clinical practices [6], patients received 18 months of ABL or unbranded TPTD followed by an additional 5 years of ALN. A treatment duration of 5 years was also used for ALN monotherapy. As medication adherence is an important driver of the cost-effectiveness of osteoporosis medications [17], it was included in the model.
Model structure
A Markov-based microsimulation model was implemented using TreeAge Pro 2023 R1.0 (TreeAge Pro Inc., Williamston, MA, USA), and was similar to the model used recently in Hiligsmann et al. [12]. All costs were adjusted for inflation by the US consumer price index for medical care to 2022 US dollars, and were discounted, as QALYs, annually by 3% [14]. The model consisted of the following health states: “high risk,” “hip fracture,” “vertebral fracture,” “nonhip nonvertebral fractures (NHNV)” and “death” (Online Resource 1). All patients begin in the “high risk” health state where the patient was a 70-year-old man or woman with a bone mineral density (BMD) T-score ≤ − 2.5 and a recent fracture, in line with definitions of very high risk in the US [6, 7]. Patients moved between health states in the model according to transition probabilities, and costs and health outcomes (life years and health utility) were captured for all individuals during all cycles. A total of 1,000,000 individual patients were simulated for every analysis to guarantee the stability of the results. Each cycle was set to 6 months and patients could have multiple fractures during their lifetime at different fracture sites. Analyses were conducted from the US healthcare decision maker perspective [18]. A similar structure of the model was used for both men and women, while gender-specific data (derived preferably from the same references) were used whenever possible. Key model inputs and assumptions are described below (and in Table 1), while additional information on the model is available in Hiligsmann et al. [12].
Transition probabilities
The baseline age- and gender-specific risk of fractures used in the model combined the general population fracture risk and increased risks associated with osteoporosis (BMD T-score ≤ − 2.5) and with a recent fracture. The fracture incidences in the US general population were extracted from Ettinger et al. [19], in line with the current US FRAX® Tool and recent published economic studies [12, 20]. A commonly used method [21] was applied to derive the increased risk associated with osteoporosis, using the US Caucasian female BMD reference database to derive T-scores in both men and women [22]. Time-dependent (6-month intervals) relative risks of subsequent fractures were used for patients with at least one fracture [5] and were higher for men than women [23].
During simulation, fracture risk was updated when the patient age changed and after a new fracture occurred. In case of multiple previous fractures, only one (the highest) increased risk was used in the model. A relative fracture risk reduction was further applied during the treatment period and during a posttreatment period (called offset time) where the treatment effect was declining. Treatment persistence was modeled according to the methodology of Liu et al. [24] and using persistence levels from the US study of Cheng et al. [25].
Two scenarios for the treatment effects were investigated: (1) efficacy data from randomized controlled trials (RCTs) and (2) efficacy data from a network meta-analysis (NMA). The first scenario used similar data and assumptions as Hiligsmann et al. [12]. Therefore, fracture risk reduction for ABL and unbranded TPTD were derived from the 43-month ACTIVE/ACTIVExtend Trial [10] conducted in postmenopausal women with osteoporosis, and the effect of ALN on fracture risk, used in both sequential and monotherapy strategies, was derived from the National Institute for Health and Care Excellence (NICE) appraisal (TA464) [26]. The second scenario was based on the recent study of Willems et al. [27] that conducted an NMA of all RCTs of osteoporosis medications for postmenopausal women with osteoporosis up to September 2020. The fracture risk reductions of TPTD and ABL at 24 months were used in our model, while fracture risk reduction at 36 months was used for ALN. Due to similar gains of osteoporosis medications on BMD in men and women [28, 29] and the lack of fracture efficacy data in men, similar treatment efficacy (derived from studies with postmenopausal women with osteoporosis) was used for both men and women.
Age- and gender-specific mortality rates (in 2019) were derived from US national statistics. Mortality after hip and vertebral fractures was incorporated in the model, consistent with prior economic studies [12]. Mortality after NHNV fractures was included for women but not for men due to the lack of significant effect [30]. In line with the International Osteoporosis Foundation–European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (IOF-ESCEO) guideline for economic evaluations in osteoporosis [31], 25% of the fracture excess death was considered to be attributable to fractures.
Costs
As the model was developed from the US payer decision maker perspective, only the direct medical care costs, including drug acquisition, monitoring, management of adverse events, fracture hospitalization, or rehabilitation were considered. Yearly incremental medical costs of hip, vertebral, and NHNV fractures for Medicare- and commercially insured women were derived from Tran et al. [32] and were adjusted to reflect higher costs of a second fracture [33]. Costs in subsequent years up to five years after an initial fracture from the same study [32] were also included in the model. As hip fractures are associated with long-term admission to nursing home and high associated costs [31], the incremental cost of hip fractures in year 5 was maintained for lifetime. In cases of multiple fractures, only one (the highest) fracture cost was considered. As men experienced higher fracture costs than women, all fracture costs were increased by 11% in men, as suggested by Williams et al. [34].
Drug prices were derived from the wholesale acquisition cost (WAC) price from the online Red Book in 2022. Yearly cost of ABL, unbranded TPTD, and generic ALN were thus US$27,468, US$33,774, and US$390, respectively. Total drug costs were adjusted by number of drugs taken during the ACTIVE trial [29] to allow for the fact that patients did not receive all drugs. Monitoring costs included one physician visit of (US$118) every six months and one BMD measurement at a cost of US$47.50 every two years in line with Medicare insurance reimbursement. We also considered the costs associated with managing treatment adverse events, as done previously [12].
Health utility
Health benefits were expressed in QALYs measuring the impact of treatments on quantity and quality of life. To generate QALY, health utility summarizing quality of life between 0 (corresponding to death) and 1 (corresponding to perfect health) is needed. Baseline age- and gender-specific utility was derived from the report of nationally representative values for the noninstitutionalized US adult population (2006 data using EQ-5D) [35] and were reduced by 13% to reflect the lower utility of US patients with fracture compared to the general population [36]. The effects of new fractures on utility were derived from the large international ICUROS study [37] and from Kanis et al. [38] for NHNV fractures. Similar fracture effect on utility was assumed for men and women, in line with a recent study suggesting that men and women had a similar quality of life one year after fracture [39].
Base-case and sensitivity analyses
Four base-case analyses were conducted in patients aged 70 years according to gender (men and women) and the two treatment efficacy data scenarios (RCT efficacy data, NMA efficacy data). An intervention is dominated if it provides less QALYs for more costs than another intervention. Incremental cost-effectiveness ratios (ICERs), defined as the difference between two strategies in terms of total healthcare costs divided by their difference in QALYs, were estimated. If the ICER is below the cost-effectiveness threshold representing decision makers’ willingness to pay, the intervention is considered cost-effective. In the US, a threshold of US$150,000 per QALY gained has been recommended for interventions that offer considerable other benefits [40].
To evaluate the robustness of base-case results and determine key drivers of cost-effectiveness, one-way sensitivity analyses were conducted on age (from 50 to 80 years), fracture incidence (± 25%), fracture costs (± 25%), fracture effects on utilities (± 25%), discount rates (0%, 5%), no fracture excess mortality, ABL drug price (± 20% and 50%), and the offset time of treatment effect (a linear decrease up to three years following discontinuation and a maintenance of the effects two years following discontinuation followed by a linear decline in the following three years). Finally, complete medication adherence was also assessed. One-way sensitivity analyses were presented as tornado diagrams for the four base-case analyses.
To better understand the joint uncertainty of our analyses, probabilistic sensitivity analyses were also done, varying key parameters from specified distributions (see Online Resource 2). Two hundred second-order simulations of 50,000 individual patients were performed and were presented as cost-effectiveness acceptability curves that show the probability of each intervention being cost-effective according to decision makers’ willingness to pay per QALY gained.
The ESCEO-IOF guideline for economic evaluation in the field of osteoporosis [31] and the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) 2022 statement [41] were followed to make sure all relevant components of this economic study were adequately designed and reported appropriately. The completed checklists of items of these guidelines are included in Online Resource 3. The model has been extensively validated and used in the past. For the purpose of this study, US clinical experts were involved in the design of the health economic plan and approved the final version with all data and assumptions. Validation efforts included running the model with other parameters and assumptions and comparison of predicted outcomes (fractures, life expectancies) with other published studies.
Results
Base-case analyses
In the four base-case analyses (Table 2), sequential ABL/ALN was associated with an incremental gain of QALY relative to no treatment (ranging from 0.123 to 0.169), to sequential unbranded TPTD/ALN (0.020–0.030), and to ALN monotherapy (0.099–0.121). However, total healthcare costs were higher for sequential ABL/ALN compared to no treatment (US$3944-US$9577) and to ALN monotherapy (US$7389-US$11,226), resulting in ICERs of US$20,378 to US$77,547 per QALY gained of sequential ABL/ALN compared to no treatment, and of US$60,810 to US$113,244 compared to ALN monotherapy. As such, the base-case analyses concluded that sequential ABL/ALN is cost-effective compared to no treatment and to generic ALN monotherapy. Furthermore, sequential ABL/ALN dominated sequential unbranded TPTD/ALN with more QALYs for less costs (US$ − 9211 to US$ − 7621). No treatment was also dominated (higher costs for less QALYs) compared to ALN monotherapy. The ICERs of sequential ABL/ALN were lower in men compared to women and when using NMA efficacy data.
Between the two non-dominated interventions, in patients with any recent fracture, sequential ABL/ALN was cost-effective (at the US cost-effectiveness threshold) compared to generic ALN monotherapy in men aged ≥ 50 years and in women aged ≥ 65 years (Table 3). The costs per QALY gained decreased with increasing age and were lower in patients with a hip or a vertebral fracture, leading to the cost-effectiveness of sequential ABL/ALN in women aged ≥ 55 years with a hip or vertebral fracture. Moreover, sequential ABL/ALN was even dominant (more QALYs for less costs) compared to ALN monotherapy in men aged ≥ 75 years with a vertebral fracture and those aged ≥ 70 years with hip fractures using NMA efficacy data. Online Resource 4 Tables S1–6 present the ICERs of sequential ABL/ALN compared to all strategies according to fracture site and treatment efficacy data.
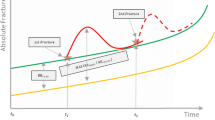
One-way sensitivity analyses
Base-case analyses were robust over one-way sensitivity analyses that are summarized as tornado diagrams in Fig. 1. Cost of ABL, fracture incidence, offset time, and the site of previous fracture were key model drivers. Assuming complete medication adherence also led to a higher ICER of sequential ABL/ALN compared to ALN monotherapy. In men, sequential ABL/ALN was cost-effective compared to ALN monotherapy in all sensitivity analyses except when assuming a 50% higher drug cost in the RCT’s efficacy data scenario. In women, there were some sensitivity analyses, especially using RCT’s efficacy data, that led to ICERs (slightly) higher than $150,000, in particular when assuming lower drug costs, shorter offset time, or complete medication adherence. As shown in Online Resource 4 Table S7, sequential ABL/ALN remained dominant (more QALYs for less costs) compared to sequential unbranded TPTD/ALN in all sensitivity analyses, except when assuming a 50% higher drug cost of ABL. In that simulation, ABL/ALN led to more costs and QALYs, resulting in ICERs between US$36,082 and US$175,441 per QALY gained. All sensitivity analyses on the cost-effectiveness of sequential ABL/ALN compared to no treatment were below the US cost-effectiveness threshold, except again when ABL price was 50% higher. No treatment was further dominated (less QALY, more costs) compared to ALN monotherapy in all sensitivity analyses.
One-way sensitivity analyses on the cost per QALY gained of ABL/ALN compared to ALN monotherapy in a men using clinical trials efficacy data, b men using NMA efficacy data, c women using clinical trials efficacy data and d women using NMA efficacy data. ABL abaloparatide, ALN alendronate, NMA network meta-analysis, QALY quality-adjusted life year
Probabilistic sensitivity analyses
The probabilistic sensitivity analyses confirmed that sequential ABL/ALN was the most cost-effective intervention at the US cost-effectiveness threshold of US$150,000 per QALY gained with probabilities to be cost-effective of 86% (in men using RCT efficacy data), 57% (in men using NMA efficacy data), 73% (in women using RCT efficacy data), and 61% (in women using NMA efficacy data) (see Fig. 2). Online Resource 4 Figures S1–2 show the cost-effectiveness acceptability curves in patients with a recent hip or vertebral fracture, respectively. Online Resource 4 Figure S3 shows the probabilities of a cost-effective outcome for sequential ABL/ALN compared to ALN monotherapy and revealed higher uncertainty when using the NMA efficacy data scenario (resulting from the large confidence interval of the effect of ABL on hip fractures).
Cost-effectiveness acceptability curves in patients aged 70 years with a recent fracture and BMD T-score ≤ − 2.5, in a men using clinical trials efficacy data, b men using NMA efficacy data, c women using clinical trials efficacy data and d women using NMA efficacy data. ABL abaloparatide, ALN alendronate, BMD bone mineral density, NMA network meta-analysis, QALY quality-adjusted life year, TPTD teriparatide
Discussion
Sequential therapy with ABL/ALN was overall cost-effective in US men and postmenopausal women at very high risk of fractures. In all analyses completed, sequential ABL/ALN was associated with more QALYs for less costs compared with sequential unbranded TPTD/ALN, while no treatment was dominated (less QALYs for more costs) by ALN monotherapy. Among the two nondominated interventions, sequential ABL/ALN was cost-effective compared to ALN monotherapy (at the US cost-effectiveness threshold) in men aged ≥ 50 years, in women aged ≥ 65 years with any fracture, and women aged ≥ 55 years with a hip or vertebral fracture.
Generally, for similar age and initial fracture site, men were associated with slightly lower ICERs than women. This result is in contrast with the review of Li et al. [14] that suggested higher ICERs in men in 75% of studies. This finding could however be explained by the very high risk of our population. Indeed, the increased risks due to osteoporosis and to recent fracture were both higher for men compared to women, leading to a greater absolute fracture risk for men at very high fracture risk. Furthermore, consequences of fractures (such as excess mortality or fracture costs) were higher in men. Improved cost-effectiveness was also observed in patients with a hip or vertebral fracture, resulting from the higher risk of subsequent fractures in these patients. In women, the minimum age at which sequential treatment ABL/ALN was cost-effective compared to ALN monotherapy decreased from 65 to 55 years with these fracture types. Furthermore, the ICERs were generally lower when using the NMA efficacy data, due to higher treatment fracture risk reduction in this scenario. However, the age at which sequential ABL/ALN was cost-effective remained similar, suggesting that our conclusions are robust over treatment efficacy scenarios. The limited impact of gender on the cost-effectiveness of sequential therapy therefore does not support different osteoporosis treatment and management strategies in men and women at very high risk of fractures.
This study confirms the economic benefits of treating patients at very high risk of fractures with sequential treatment [8]. Currently, many patients at high fracture risk do not receive an osteoporosis medication [9], and adherence to osteoporosis medication remains suboptimal [42]. As patients with a recent fracture are the most likely to sustain further fractures, it is important to optimize secondary fracture prevention. In particular, fracture liaison services are essential and have been shown to be effective in reducing subsequent fractures [43] and to be cost-effective in combination with oral bisphosphates [44]. Potentially higher economic benefits of fracture liaison services could even be reached when combined with sequential therapy with ABL.
There are potential limitations of this study, of which some were already reported in previous studies [12, 15, 16]. First, a direct comparison of the cost-effectiveness between men and women could be limited by the lack of fracture risk studies in men. In line with regulators accepting a bridging study with a placebo for approval in men, similar treatment efficacy is commonly assumed between men and women with osteoporosis [14, 45]. Second, certain relevant detailed data (such as fracture costs or increased risks of subsequent fracture after fractures) were only available for women, and adjustments needed to be done to consider expected differences between men and women. Another example is the use of similar medication adherence for men and women, while other studies have suggested that men are generally less adherent to osteoporosis medications than women [46]. More gender-specific data on real-world persistence to sequential ABL/ALN would thus be of interest to confirm our findings. Similarly, real-world effectiveness data [47] could be used in future economic evaluations and improve the robustness of our conclusions. Third, the study was conducted using populations considered white or Caucasian men and women. It is nowadays recognized that there are racial and ethnic differences in fracture risk [48] and fracture outcomes [49]. More economic studies are needed to investigate the transferability of our findings to “non-white” US men and women. Finally, this study was limited to QALY as health outcome. Although QALY is the academic standard for measuring health outcomes in economic evaluations, the Institute for Clinical and Economic Review (ICER) introduced in 2018, to supplement, QALY the equal value of life years gained (evLYG) metric which evenly measures any gains in length of life, regardless of the treatment’s ability to improve patients’ quality of life [50]. As fracture prevention, especially in the oldest patients, leads to life extension, high expected benefits are also anticipated with evLYG.
In conclusion, this study suggests similar cost-effectiveness of sequential ABL/ALN compared to unbranded TPTD/ALN, ALN monotherapy, and no treatment in both US men and women at very high fracture risk, with a moderate improvement in cost-effectiveness in men compared to women and in patients with a hip or vertebral fracture.
Data availability
Data that underlie the results reported in a published article may be requested for further research 6 months after completion of FDA or EMA regulatory review of a marketing application (if applicable) or 18 months after trial completion (whichever is latest). Radius will review requests individually to determine whether (i) the requests are legitimate and relevant and meet sound scientific research principles, and (ii) are within the scope of the participants’ informed consent. Prior to making data available, requestors will be required to agree in writing to certain obligations, including without limitation, compliance with applicable privacy and other laws and regulations. Proposals should be directed to info@radiuspharm.com.
References
National Osteoporosis Foundation (2011) The man’s guide to osteoporosis. Bone Health and Osteoporosis Foundation. https://www.bonehealthandosteoporosis.org/wp-content/uploads/2016/02/Mans-Guide-to-Osteoporosis.pdf. Accessed 5 Oct 2023.
Office of the Surgeon General (US) (2004) Bone health and osteoporosis: a report of the surgeon general. Office of the Surgeon General (US), Rockville (MD). http://www.ncbi.nlm.nih.gov/books/NBK45513/. Accessed 16 Aug 2023.
Hansen D, Pelizzari PM, Pyenson BS (2021) Medicare cost of osteoporotic fractures: 2021 updated report. https://www.milliman.com/en/insight/medicare-cost-of-osteoporotic-fractures-2021-updated-report. Accessed 1 Oct 2023.
Kanis JA, Norton N, Harvey NC et al (2021) SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos 16:82. https://doi.org/10.1007/s11657-020-00871-9
Soreskog E, Strom O, Spangeus A et al (2020) Risk of major osteoporotic fracture after first, second and third fracture in Swedish women aged 50 years and older. Bone 134:115286. https://doi.org/10.1016/j.bone.2020.115286
Camacho PM, Petak SM, Binkley N et al (2020) American association of clinical endocrinologists/American college of endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 update. Endocr Pract 26:1–46. https://doi.org/10.4158/gl-2020-0524suppl
Eastell R, Rosen CJ, Black DM et al (2019) Pharmacological management of osteoporosis in postmenopausal women: an endocrine society* clinical practice guideline. J Clin Endocrinol Metab 104:1595–1622. https://doi.org/10.1210/jc.2019-00221
Curtis EM, Reginster J-Y, Al-Daghri N et al (2022) Management of patients at very high risk of osteoporotic fractures through sequential treatments. Aging Clin Exp Res 34:695–714. https://doi.org/10.1007/s40520-022-02100-4
Kim SC, Kim MS, Sanfelix-Gimeno G et al (2015) Use of osteoporosis medications after hospitalization for hip fracture: a cross-national study. Am J Med 128:519–26 e1. https://doi.org/10.1016/j.amjmed.2015.01.014
Bone HG, Cosman F, Miller PD et al (2018) ACTIVExtend: 24 months of alendronate after 18 months of abaloparatide or placebo for postmenopausal osteoporosis. J Clin Endocrinol Metab 103:2949–2957. https://doi.org/10.1210/jc.2018-00163
Yang D, Tan J, Long Y et al (2023) Sequential treatment of teriparatide and alendronate versus alendronate alone for elevation of bone mineral density and prevention of refracture after percutaneous vertebroplasty in osteoporosis: a prospective study. Aging Clin Exp Res 35:531–539. https://doi.org/10.1007/s40520-023-02342-w
Hiligsmann M, Silverman SS, Singer AJ et al (2023) Cost-effectiveness of sequential abaloparatide/alendronate in men at high risk of fractures in the United States. Pharmacoeconomics 41:819–830. https://doi.org/10.1007/s40273-023-01270-x
Yu G, Tong S, Liu J et al (2023) A systematic review of cost-effectiveness analyses of sequential treatment for osteoporosis. Osteoporos Int 34:641–658. https://doi.org/10.1007/s00198-022-06626-1
Li N, Beaudart C, Cauley JA et al (2023) Cost effectiveness analyses of interventions for osteoporosis in men: a systematic literature review. Pharmacoeconomics 41:363–391. https://doi.org/10.1007/s40273-022-01239-2
Hiligsmann M, Williams SA, Fitzpatrick LA et al (2019) Cost-effectiveness of sequential treatment with abaloparatide vs. teriparatide for United States women at increased risk of fracture. Semin Arthritis Rheum 49:184–196. https://doi.org/10.1016/j.semarthrit.2019.01.006
Hiligsmann M, Williams SA, Fitzpatrick LA et al (2020) Cost-effectiveness of sequential treatment with abaloparatide followed by alendronate vs. alendronate monotherapy in women at increased risk of fracture: a US payer perspective. Semin Arthritis Rheum 50:394–400. https://doi.org/10.1016/j.semarthrit.2020.02.004
Hiligsmann M, Boonen A, Rabenda V et al (2012) The importance of integrating medication adherence into pharmacoeconomic analyses: the example of osteoporosis. Expert Rev Pharmacoecon Outcomes Res 12:159–166. https://doi.org/10.1586/erp.12.8
AMCP (2023) AMCP Format for formulary submissions—guidance on submission of pre-approval and post-approval clinical and economic information and evidence, version 4.1. AMCP. https://www.amcp.org/Resource-Center/format-formulary-submissions/AMCP-Format-for-Formulary-Submissions-4.1. Accessed 16 Aug 2023.
Ettinger B, Black DM, Dawson-Hughes B et al (2010) Updated fracture incidence rates for the US version of FRAX. Osteoporos Int 21:25–33. https://doi.org/10.1007/s00198-009-1032-9
Luo C, Qin SX, Wang QY et al (2023) Cost-effectiveness analysis of five drugs for treating postmenopausal women in the United States with osteoporosis and a very high fracture risk. J Endocrinol Invest 46:367–379. https://doi.org/10.1007/s40618-022-01910-7
Kanis JA, Johnell O, Oden A et al (2000) Risk of hip fracture according to the World Health Organization criteria for osteopenia and osteoporosis. Bone 27:585–590. https://doi.org/10.1016/s8756-3282(00)00381-1
Looker AC, Wahner HW, Dunn WL et al (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8:468–489. https://doi.org/10.1007/s001980050093
Center JR, Bliuc D, Nguyen TV et al (2007) Risk of subsequent fracture after low-trauma fracture in men and women. JAMA 297:387–394. https://doi.org/10.1001/jama.297.4.387
Liu H, Michaud K, Nayak S et al (2006) The cost-effectiveness of therapy with teriparatide and alendronate in women with severe osteoporosis. Arch Intern Med 166:1209–1217. https://doi.org/10.1001/archinte.166.11.1209
Cheng LI, Durden E, Limone B et al (2015) Persistance and compliance with osteroporosis therapies among women in a commercially insured population in the United States. J Manag Care Spec Pharm 21:824–833. https://doi.org/10.18553/jmcp.2015.21.9.824
NICE (2017) Bisphosphonates for treating osteoporosis: technology appraisal guidance [TA464]. https://www.nice.org.uk/guidance/ta464. Accessed 16 Aug 2023.
Willems D, Javaid MK, Pinedo-Villanueva R et al (2022) Importance of time point-specific indirect treatment comparisons of osteoporosis treatments: a systematic literature review and network meta-analyses. Clin Ther 44:81–97. https://doi.org/10.1016/j.clinthera.2021.11.015
Czerwinski E, Cardona J, Plebanski R et al (2022) The efficacy and safety of abaloparatide-SC in men with osteoporosis: a randomized clinical trial. J Bone Miner Res 37:2435–2442. https://doi.org/10.1002/jbmr.4719
Miller PD, Hattersley G, Riis BJ et al (2016) Effect of abaloparatide vs placebo on new vertebral fractures in postmenopausal women with osteoporosis: a randomized clinical trial. JAMA 316:722–733. https://doi.org/10.1001/jama.2016.11136
Tran T, Bliuc D, van Geel T et al (2017) Population-wide impact of non-hip non-vertebral fractures on mortality. J Bone Miner Res 32:1802–1810. https://doi.org/10.1002/jbmr.3118
Hiligsmann M, Reginster J-Y, Tosteson ANA et al (2019) Recommendations for the conduct of economic evaluations in osteoporosis: outcomes of an experts’ consensus meeting organized by the European society for clinical and economic aspects of osteoporosis, osteoarthritis and musculoskeletal diseases (ESCEO) and the US branch of the International Osteoporosis Foundation. Osteoporos Int 30:45–57. https://doi.org/10.1007/s00198-018-4744-x
Tran O, Silverman S, Xu X et al (2021) Long-term direct and indirect economic burden associated with osteoporotic fracture in US postmenopausal women. Osteoporos Int 32:1195–1205. https://doi.org/10.1007/s00198-020-05769-3
Weaver J, Sajjan S, Lewiecki EM et al (2017) Prevalence and cost of subsequent fractures among US patients with an incident fracture. J Manag Care Spec Pharm 23:461–471. https://doi.org/10.18553/jmcp.2017.23.4.461
Williams SA, Chastek B, Sundquist K et al (2020) Economic burden of osteoporotic fractures in US managed care enrollees. Am J Manag Care 26:e142–e149. https://doi.org/10.37765/ajmc.2020.43156
Hanmer J, Lawrence WF, Anderson JP et al (2006) Report of nationally representative values for the noninstitutionalized US adult population for 7 health-related quality-of-life scores. Med Decis Making 26:391–400. https://doi.org/10.1177/0272989x06290497
Gold T, Williams SA, Weiss RJ et al (2019) Impact of fractures on quality of life in patients with osteoporosis: a US cross-sectional survey. J Drug Assess 8:175–183. https://doi.org/10.1080/21556660.2019.1677674
Svedbom A, Borgstöm F, Hernlund E et al (2018) Quality of life for up to 18 months after low-energy hip, vertebral, and distal forearm fractures-results from the ICUROS. Osteoporos Int 29:557–566. https://doi.org/10.1007/s00198-017-4317-4
Kanis JA, Johansson H, Odén A et al (2018) Characteristics of recurrent fractures. Osteoporos Int 29:1747–1757. https://doi.org/10.1007/s00198-018-4502-0
Talevski J, Sanders KM, Watts JJ et al (2022) Sex differences in recovery of quality of life 12 months post-fracture in community-dwelling older adults: analyses of the Australian arm of the International Costs and Utilities Related to Osteoporotic Fractures Study (AusICUROS). Osteoporos Int 33:67–75. https://doi.org/10.1007/s00198-021-06058-3
Dubois RW (2016) Cost-effectiveness thresholds in the USA: are they coming? Are they already here? J Comp Eff Res 5:9–11. https://doi.org/10.2217/cer.15.50
Husereau D, Drummond M, Augustovski F et al (2022) Consolidated health economic evaluation reporting standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Pharmacoeconomics 40:601–609. https://doi.org/10.1016/j.jval.2021.11.1351
Hiligsmann M, Cornelissen D, Vrijens B et al (2019) Determinants, consequences and potential solutions to poor adherence to anti-osteoporosis treatment: results of an expert group meeting organized by the European society for clinical and economic aspects of osteoporosis, osteoarthritis and musculoskeletal diseases (ESCEO) and the International Osteoporosis Foundation (IOF). Osteoporos Int 30:2155–2165. https://doi.org/10.1007/s00198-019-05104-5
Li N, Hiligsmann M, Boonen A et al (2021) The impact of fracture liaison services on subsequent fractures and mortality: a systematic literature review and meta-analysis. Osteoporos Int 32:1517–1530. https://doi.org/10.1007/s00198-021-05911-9
Wu C-H, Kao I-J, Hung W-C et al (2018) Economic impact and cost-effectiveness of fracture liaison services: a systematic review of the literature. Osteoporos Int 29:1227–1242. https://doi.org/10.1007/s00198-018-4411-2
Beaudart C, Demonceau S, Sabico S et al (2023) Efficacy of osteoporosis pharmacological treatments in men: a systematic review and meta-analysis. Aging Clin Exp Res 35:1789–1806. https://doi.org/10.1007/s40520-023-02478-9
Yeam CT, Chia S, Tan HCC et al (2018) A systematic review of factors affecting medication adherence among patients with osteoporosis. Osteoporos Int 29:2623–2637. https://doi.org/10.1007/s00198-018-4759-3
Cosman F, Cooper C, Wang Y et al (2022) Comparative effectiveness and cardiovascular safety of abaloparatide and teriparatide in postmenopausal women new to anabolic therapy: a US administrative claims database study. Osteoporos Int 33:1703–1714. https://doi.org/10.1007/s00198-022-06413-y
Bao Y, Xu Y, Li Z et al (2023) Racial and ethnic difference in the risk of fractures in the United States: a systematic review and meta-analysis. Sci Rep 13:9481. https://doi.org/10.1038/s41598-023-32776-1
Noel SE, Santos MP, Wright NC (2021) Racial and ethnic disparities in bone health and outcomes in the United States. J Bone Miner Res 36:1881–1905. https://doi.org/10.1002/jbmr.4417
Institute for Clinical and Economic Review. The QALY: rewarding the care that most improves patients’ lives. December 2018. https://icer.org/wp-content/uploads/2020/12/QALY_evLYG_FINAL.pdf. Accessed 25 Aug 2023.
Haentjens P, Magaziner J, Colon-Emeric CS et al (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152:380–390. https://doi.org/10.7326/0003-4819-152-6-201003160-00008
Acknowledgements
All listed authors meet the criteria for authorship set forth by the International Committee for Medical Journal Editors. The sponsor, Radius Health, Inc., was involved in the design of the study, review of the protocol, and review and author approval of the manuscript. The sponsor had no role in the final selection of data and assumptions, execution and analysis of the model, and the interpretation of the results. Medical editorial support and graphic services were provided by AOIC, LLC and were funded by Radius. Artificial intelligence (AI) technologies such as Language Learning Models, chatbots, and image creators were not used in the production of this work.
Funding
This study was funded by Radius Health, Inc.
Author information
Authors and Affiliations
Contributions
MH and JYR contributed to the study design. MH, YW, and JYR contributed to the acquisition of data. MH and JYR conducted the analysis. MH, SLS, AJS, LP, YW, JC, and JYR contributed to the data interpretation. MH wrote the first draft and SLS, AJS, LP, YW, JC, and JYR reviewed all drafts critically. All authors provide final approval of this manuscript for submission and agree to be accountable for the work.
Corresponding author
Ethics declarations
Conflict of interest
MH has received research grants through his institution from Amgen, Radius Health, Inc. (Radius), ViiV, and Angelini Pharma, consulting fees from UCB and Pfizer (paid to institution), lecture fees from IBSA (paid to institution) and Mylan Pharmaceuticals. SLS has received grants from Amgen and Radius and consulting fees from Amgen and Radius. AJS has received research grants paid to her institution from Radius and UCB, consulting fees from Agnovos, Amgen, Radius, and UCB, and speaking fees from Amgen and Radius. LP and YW are employees of Radius. JC was an employee at Radius at the time of the analyses. JYR has received consulting fees or paid advisory boards from IBSA-Genevrier, Mylan, Radius, Pierre Fabre, and Teva, lecture fees when speaking at the invitation of sponsors IBSA-Genevrier, Mylan, CNIEL, Dairy Research Council, and Teva, and grant support from industry (all through institution) from IBSA-Genevrier, Mylan, CNIEL, and Radius.
Ethical approval
No ethics approval was required as no primary data were collected.
Statement of human and animal rights
As no primary data was collected, nor human or animal patients used, no ethical approval was required for this paper.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hiligsmann, M., Silverman, S.L., Singer, A.J. et al. Comparison of the cost-effectiveness of sequential treatment with abaloparatide in US men and women at very high risk of fractures. Aging Clin Exp Res 36, 14 (2024). https://doi.org/10.1007/s40520-023-02682-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40520-023-02682-7