Abstract
Background
Insulin plays a crucial and multifactorial role in cognitive activity, with insulin resistance appearing in neurodegenerative and metabolic diseases. Insulin resistance contributes to the pathobiology of postoperative cognitive dysfunction (POCD) in experimental models, which can be rescued by intranasal insulin administration.
Aims
To test the effect of intranasal insulin on the incidence of POCD in elderly patients with metabolic syndrome.
Methods
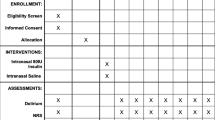
The study was designed as a randomized, double-blind, placebo-controlled clinical trial. 116 elderly participants were randomly assigned to receive either 40 IU insulin (n = 58) or placebo (n = 58) for 7 days. The primary outcome was the incidence of POCD at 7 days and 3 months after surgery. Secondary outcomes included the degree of peripheral insulin resistance postoperatively, changes in peripheral inflammation levels and the safety of interventions.
Results
The results showed that POCD occurred in the insulin group on the 7th postoperative day in 11 (20.8%) patients, which was fewer than the 23 (45.1%) patients in the placebo group (P = 0.008). The insulin group indicated better cognitive functional performance on language and memory test than the placebo group (P < 0.05). Mean peripheral plasma concentration of TNF-α (P < 0.05) and CRP (P < 0.001) in the insulin group was significantly declined compared with the placebo group on D3 and D7.
Conclusions
Intranasal insulin administration reduced the incidence of POCD and alleviated peripheral inflammatory levels in elderly patients with metabolic syndrome.
Trial registry
Chinese Clinical Trial Registry (ChiCTR1800015502).





Similar content being viewed by others
Data availability
The originale contributions presented in the study are included in the article, further inquiries can be directed to the corresponding authors.
References
Evered LA, Silbert BS (2018) Postoperative cognitive dysfunction and noncardiac surgery. Anesth Analg 127:496–505
Feinkohl I, Winterer G, Pischon T (2017) Hypertension and risk of post-operative cognitive dysfunction (POCD): a systematic review and meta-analysis. Clin Pract Epidemiol Ment Health 13:27–42
Feinkohl I, Winterer G, Pischon T (2017) Diabetes is associated with risk of postoperative cognitive dysfunction: a meta-analysis. Diabetes Metab Res Rev. https://doi.org/10.1002/dmrr.2884
Feinkohl I, Winterer G, Pischon T (2016) Obesity and post-operative cognitive dysfunction: a systematic review and meta-analysis. Diabetes Metab Res Rev 32:643–651
Kotfis K, Szylińska A, Listewnik M et al (2019) Diabetes and elevated preoperative HbA1c level as risk factors for postoperative delirium after cardiac surgery: an observational cohort study. Neuropsychiatr Dis Treat 15:511–521
Kadoi Y, Saito S, Fujita N et al (2005) Risk factors for cognitive dysfunction after coronary artery bypass graft surgery in patients with type 2 diabetes. J Thorac Cardiovasc Surg 129:576–583
Denver P, McClean PL (2018) Distinguishing normal brain aging from the development of Alzheimer’s disease: inflammation, insulin signaling and cognition. Neural Regen Res 13:1719–1730
Kullmann S, Heni M, Hallschmid M et al (2016) Brain insulin resistance at the crossroads of metabolic and cognitive disorders in humans. Physiol Rev 96:1169–1209
Kellar D, Craft S (2020) Brain insulin resistance in Alzheimer’s disease and related disorders: mechanisms and therapeutic approaches. Lancet Neurol 19:758–766
Hölscher C (2020) Brain insulin resistance: role in neurodegenerative disease and potential for targeting. Expert Opin Investig Drugs 29:333–348
He X, Long G, Quan C et al (2019) Insulin resistance predicts postoperative cognitive dysfunction in elderly gastrointestinal patients. Front Aging Neurosci 11:197
Tang N, Jiang R, Wang X et al (2017) Insulin resistance plays a potential role in postoperative cognitive dysfunction in patients following cardiac valve surgery. Brain Res 1657:377–382
Badenes R, Qeva E, Giordano G et al (2021) Intranasal insulin administration to prevent delayed neurocognitive recovery and postoperative neurocognitive disorder: a narrative review. Int J Environ Res Public Health 18:2681
Chen Y, Dai CL, Wu Z et al (2017) Intranasal insulin prevents anesthesia-induced cognitive impairment and chronic neurobehavioral changes. Front Aging Neurosci 9:136
Du Y, Cui H, Xiao Y et al (2019) The mechanism of lipopolysaccharide administration-induced cognitive function impairment caused by glucose metabolism disorder in adult rats. Saudi J Biol Sci 26:1268–1277
Kawano T, Iwata H, Aoyama B et al (2016) The role of hippocampal insulin signaling on postoperative cognitive dysfunction in an aged rat model of abdominal surgery. Life Sci 162:87–94
Ott V, Benedict C, Schultes B et al (2012) Intranasal administration of insulin to the brain impacts cognitive function and peripheral metabolism. Diabetes Obes Metab 14:214–221
Avgerinos KI, Kalaitzidis G, Malli A et al (2018) Intranasal insulin in Alzheimer’s dementia or mild cognitive impairment: a systematic review. J Neurol 265:1497–1510
Rajasekar N, Nath C, Hanif K et al (2017) Intranasal insulin administration ameliorates streptozotocin (ICV)-induced insulin receptor dysfunction, neuroinflammation, amyloidogenesis, and memory impairment in rats. Mol Neurobiol 54:6507–6522
Simon KU, Neto EW, Tramontin NDS et al (2020) Intranasal insulin treatment modulates the neurotropic, inflammatory, and oxidant mechanisms in the cortex and hippocampus in a low-grade inflammation model. Peptides 123:170175
Creavin ST, Wisniewski S, Noel-Storr AH et al (2016) Mini-Mental State Examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Cochrane Database Syst Rev 2016:011145
Grundy SM, Brewer HB Jr, Cleeman JI et al (2004) Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 109:433–438
Borchers F, Spies CD, Feinkohl I et al (2021) Methodology of measuring postoperative cognitive dysfunction: a systematic review. Br J Anaesth 126:1119–1127
Matthews DR, Hosker JP, Rudenski AS et al (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Wei P, Yang F, Zheng Q et al (2019) The potential role of the NLRP3 inflammasome activation as a link between mitochondria ros generation and neuroinflammation in postoperative cognitive dysfunction. Front Cell Neurosci 13:73
Brünner YF, Kofoet A, Benedict C et al (2015) Central insulin administration improves odor-cued reactivation of spatial memory in young men. J Clin Endocrinol Metab 100:212–219
Benedict C, Hallschmid M, Schmitz K et al (2007) Intranasal insulin improves memory in humans: superiority of insulin aspart. Neuropsychopharmacology 32:239–243
Feld GB, Wilhem I, Benedict C et al (2016) Central nervous insulin signaling in sleep-associated memory formation and neuroendocrine regulation. Neuropsychopharmacology 41:1540–1550
Novak V, Milberg W, Hao Y et al (2014) Enhancement of vasoreactivity and cognition by intranasal insulin in type 2 diabetes. Diabetes Care 37:751–759
Craft S, Raman R, Chow TW et al (2020) Safety, efficacy, and feasibility of intranasal insulin for the treatment of mild cognitive impairment and alzheimer disease dementia: a randomized clinical trial. JAMA Neurol 77:1099–1109
Alam A, Hana Z, Jin Z et al (2018) Surgery, neuroinflammation and cognitive impairment. EBioMedicine 37:547–556
Shoelson SE, Lee J, Goldfine AB (2006) Inflammation and insulin resistance. J Clin Invest 116:1793–1801
Hotamisligil GS (2006) Inflammation and metabolic disorders. Nature 444:860–867
Kellar D, Register T, Lockhart SN et al (2022) Intranasal insulin modulates cerebrospinal fluid markers of neuroinflammation in mild cognitive impairment and Alzheimer’s disease: a randomized trial. Sci Rep 12:1346
O’Bryan LJ, Atkins KJ, Lipszyc A et al (2022) Inflammatory biomarker levels after propofol or sevoflurane anesthesia: a meta-analysis. Anesth Analg 134:69–81
Deiner S, Baxter MG, Mincer JS et al (2020) Human plasma biomarker responses to inhalational general anaesthesia without surgery. Br J Anaesth 125:282–290
de la Monte SM (2013) Intranasal insulin therapy for cognitive impairment and neurodegeneration: current state of the art. Expert Opin Drug Deliv 10:1699–1709
Hallschmid M (2021) Intranasal Insulin for Alzheimer’s disease. CNS Drugs 35:21–37
Willette AA, Bendlin BB, Starks EJ et al (2015) Association of insulin resistance with cerebral glucose uptake in late middle-aged adults at risk for Alzheimer disease. JAMA Neurol 72:1013–1020
Heni M, Kullmann S, Ketterer C et al (2012) Nasal insulin changes peripheral insulin sensitivity simultaneously with altered activity in homeostatic and reward-related human brain regions. Diabetologia 55:1773–1782
Evered L, Silbert B, Knopman DS et al (2018) Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018. Anesthesiology 129:872–879
Acknowledgements
Assistance with the article: we thank all included patients, all physicians, paramedics and nurses from the participating hospitals, who supported the protocol development, implementation and compliance adherence of this clinical trial. We thank all departments of the Third Xiangya Hospital of Central South University involved in the project: Departments of General Surgery, Thoracic Surgery, Urological Surgery, Orthopedic Surgery and Central Lab.
Funding
The trial was funded by the National Natural Science Foundation of China 81901842, China Primary Health Care Foundation YLGX-WS-2020003 and Natural Science Foundation of Hunan Province 2021JJ40936.
Author information
Authors and Affiliations
Contributions
HX, YM, LG and OW: designed the study. Material preparation and data collection were performed by LG and TY. LX and TJ: was responsible for the statistical design of the study and for carrying out the statistical analysis. The first draft of the manuscript was written by YM and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that there is no conflict of interest.
Ethical approval
Ethical approval for this study (ethical code: K18193) was provided by the Ethical Committee of the Third Xiangya Hospital of Central South University.
Informed consent
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mi, Y., Wen, O., Ge, L. et al. Protective effect of intranasal insulin on postoperative cognitive dysfunction in elderly patients with metabolic syndrome undergoing noncardiac surgery: a randomized clinical trial. Aging Clin Exp Res 35, 3167–3178 (2023). https://doi.org/10.1007/s40520-023-02593-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02593-7