Abstract
Purpose
The prevalence of frailty in individuals with cardiometabolic disease (CMD) has become a growing concern in public health. The purpose of this study was to investigate the association between estimated pulse wave velocity (ePWV) and frailty in middle-aged and older adults with CMD.
Methods
We analyzed data from 23,313 non-institutionalized adults with CMD from the National Health and Nutrition Examination Survey 2003–2018. Frailty status was determined using the frailty index, and logistic regression models were used to assess the association of ePWV with frailty risk. Multivariable logistic regression and propensity-score matching (PSM) were used to adjust for potential confounders. The restricted cubic spline regression model was used to evaluate the non-linear association between ePWV and frailty risk.
Results
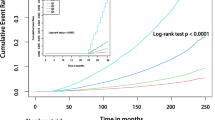
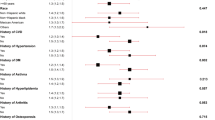
After adjusting for potential confounding factors, we found that each one m/s increase in ePWV was associated with a 15% higher risk of frailty (odds ratio [OR] = 1.15, 95% confidence interval [CI] 1.12 to 1.18, P < 0.001). After PSM, the association remained significant (OR = 1.05, 95% CI 1.03 to 1.08, P < 0.001). The logistic models with restricted cubic splines showed a non-linear dose–response association, with the risk of frailty increasing more rapidly when ePWV exceeded 9.5 m/s.
Conclusions
The findings of this study suggest that a higher level of ePWV is associated with an increased risk of frailty in middle-aged and older adults with CMD, and may serve as a viable alternative to directly measured cfPWV.




Similar content being viewed by others
Data availability
The NHANES datasets are publicly available in “www.cdc.gov/nchs/nhanes/”.
References
GBD (2019) Risk Factors Collaborators (2020) Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396:1223–1249. https://doi.org/10.1016/S0140-6736(20)30752-2
Roth GA, Mensah GA, Johnson CO et al (2020) Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol 76:2982–3021. https://doi.org/10.1016/j.jacc.2020.11.010
Miranda JJ, Barrientos-Gutiérrez T, Corvalan C et al (2019) Understanding the rise of cardiometabolic diseases in low- and middle-income countries. Nat Med 25:1667–1679. https://doi.org/10.1038/s41591-019-0644-7
Chang AY, Skirbekk VF, Tyrovolas S et al (2019) Measuring population ageing: an analysis of the Global Burden of Disease Study 2017. Lancet Public Health 4:e159–e167. https://doi.org/10.1016/S2468-2667(19)30019-2
Richter D, Guasti L, Walker D et al (2022) Frailty in cardiology: definition, assessment and clinical implications for general cardiology. A consensus document of the Council for Cardiology Practice (CCP), Association for Acute Cardio Vascular Care (ACVC), Association of Cardiovascular Nursing and Allied Professions (ACNAP), European Association of Preventive Cardiology (EAPC), European Heart Rhythm Association (EHRA), Council on Valvular Heart Diseases (VHD), Council on Hypertension (CHT), Council of Cardio-Oncology (CCO), Working Group (WG) Aorta and Peripheral Vascular Diseases, WG e-Cardiology, WG Thrombosis, of the European Society of Cardiology, European Primary Care Cardiology Society (EPCCS). Eur J Prev Cardiol 29:216–227. https://doi.org/10.1093/eurjpc/zwaa167
Wilkinson C, Rockwood K (2022) Frailty assessment in the management of cardiovascular disease. Heart 108:1991–1995. https://doi.org/10.1136/heartjnl-2022-321265
Brunner EJ, Shipley MJ, Ahmadi-Abhari S et al (2018) Midlife contributors to socioeconomic differences in frailty during later life: a prospective cohort study. Lancet Public Health 3:e313–e322. https://doi.org/10.1016/S2468-2667(18)30079-3
Hoogendijk EO, Afilalo J, Ensrud KE et al (2019) Frailty: implications for clinical practice and public health. Lancet 394:1365–1375. https://doi.org/10.1016/S0140-6736(19)31786-6
Monin J, Doyle M, Levy B et al (2016) Spousal associations between frailty and depressive symptoms: longitudinal findings from the cardiovascular health study. J Am Geriatr Soc 64:824–830. https://doi.org/10.1111/jgs.14023
Li G, Prior JC, Leslie WD et al (2019) Frailty and risk of fractures in patients with type 2 diabetes. Diabetes Care 42:507–513. https://doi.org/10.2337/dc18-1965
Ida S, Kaneko R, Imataka K et al (2019) Relationship between frailty and mortality, hospitalization, and cardiovascular diseases in diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol 18:81. https://doi.org/10.1186/s12933-019-0885-2
Damluji AA, Chung S-E, Xue Q-L et al (2021) Frailty and cardiovascular outcomes in the National Health and Aging Trends Study. Eur Heart J 42:3856–3865. https://doi.org/10.1093/eurheartj/ehab468
Qayyum S, Rossington JA, Chelliah R et al (2020) Prospective cohort study of elderly patients with coronary artery disease: impact of frailty on quality of life and outcome. Open Heart 7:e001314. https://doi.org/10.1136/openhrt-2020-001314
Fan J, Yu C, Guo Y et al (2020) Frailty index and all-cause and cause-specific mortality in Chinese adults: a prospective cohort study. Lancet Public Health 5:e650–e660. https://doi.org/10.1016/S2468-2667(20)30113-4
Kojima G, Iliffe S, Walters K (2018) Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing 47:193–200. https://doi.org/10.1093/ageing/afx162
Chode S, Malmstrom TK, Miller DK et al (2016) Frailty, diabetes, and mortality in middle-aged African Americans. J Nutr Health Aging 20:854–859. https://doi.org/10.1007/s12603-016-0801-3
Dent E, Kowal P, Hoogendijk EO (2016) Frailty measurement in research and clinical practice: a review. Eur J Intern Med 31:3–10. https://doi.org/10.1016/j.ejim.2016.03.007
Blodgett J, Theou O, Kirkland S et al (2015) Frailty in NHANES: comparing the frailty index and phenotype. Arch Gerontol Geriatr 60:464–470. https://doi.org/10.1016/j.archger.2015.01.016
Rockwood K, Andrew M, Mitnitski A (2007) A comparison of two approaches to measuring frailty in elderly people. J Gerontol A Biol Sci Med Sci 62:738–743. https://doi.org/10.1093/gerona/62.7.738
Kulminski AM, Ukraintseva SV, Kulminskaya IV et al (2008) Cumulative deficits better characterize susceptibility to death in elderly people than phenotypic frailty: lessons from the Cardiovascular Health Study. J Am Geriatr Soc 56:898–903. https://doi.org/10.1111/j.1532-5415.2008.01656.x
Piotrowicz K, Gąsowski J (2020) Risk factors for frailty and cardiovascular diseases: are they the same? In: Veronese N (ed) Frailty and cardiovascular diseases: research into an elderly population. Springer International Publishing, Cham, pp 39–50
Orkaby AR, Lunetta KL, Sun FJ et al (2019) Cross-sectional association of frailty and arterial stiffness in community-dwelling older adults: the Framingham heart study. J Gerontol A Biol Sci Med Sci 74:373–379. https://doi.org/10.1093/gerona/gly134
Nadruz W, Kitzman D, Windham BG et al (2017) Cardiovascular dysfunction and frailty among older adults in the community: the ARIC study. J Gerontol A Biol Sci Med Sci 72:958–964. https://doi.org/10.1093/gerona/glw199
Laurent S, Cockcroft J, Van Bortel L et al (2006) Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 27:2588–2605. https://doi.org/10.1093/eurheartj/ehl254
The Reference Values for Arterial Stiffness' Collaboration (2010) Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. Eur Heart J 31:2338–2350. https://doi.org/10.1093/eurheartj/ehq165
Greve SV, Blicher MK, Kruger R et al (2016) Estimated carotid-femoral pulse wave velocity has similar predictive value as measured carotid-femoral pulse wave velocity. J Hypertens 34:1279–1289. https://doi.org/10.1097/HJH.0000000000000935
Jae SY, Heffernan KS, Park JB et al (2021) Association between estimated pulse wave velocity and the risk of cardiovascular outcomes in men. Eur J Prev Cardiol 28:e25–e27. https://doi.org/10.1177/2047487320920767
Heffernan KS, Wilmoth JM, London AS (2022) Estimated pulse wave velocity and all-cause mortality: findings from the health and retirement study. Innov Aging 6:igac056. https://doi.org/10.1093/geroni/igac056
Heffernan KS, Jae SY, Loprinzi PD (2020) Association between estimated pulse wave velocity and mortality in U.S. Adults J Am Coll Cardiol 75:1862–1864. https://doi.org/10.1016/j.jacc.2020.02.035
Vlachopoulos C, Terentes-Printzios D, Laurent S et al (2019) Association of estimated pulse wave velocity with survival: a secondary analysis of SPRINT. JAMA Netw Open 2:e1912831. https://doi.org/10.1001/jamanetworkopen.2019.12831
National Center for Health Statistics (2020) NHANES—about the National Health and Nutrition Examination Survey. https://www.cdc.gov/nchs/nhanes/about_nhanes.htm. Accessed 7 Apr 2022
Centers for Disease Control and Prevention (2022) NCHS Research Ethics Review Board (ERB) Approval. https://www.cdc.gov/nchs/nhanes/irba98.htm. Accessed 9 Nov 2022
Guo F, Moellering DR, Garvey WT (2014) The progression of cardiometabolic disease: validation of a new cardiometabolic disease staging system applicable to obesity. Obesity (Silver Spring) 22:110–118. https://doi.org/10.1002/oby.20585
Searle SD, Mitnitski A, Gahbauer EA et al (2008) A standard procedure for creating a frailty index. BMC Geriatr 8:24. https://doi.org/10.1186/1471-2318-8-24
Rockwood K, Mitnitski AB, MacKnight C (2002) Some mathematical models of frailty and their clinical implications. Rev Clin Gerontol 12:109–117. https://doi.org/10.1017/S0959259802012236
Möller S, Bliddal M, Rubin KH (2021) Methodical considerations on adjusting for Charlson Comorbidity Index in epidemiological studies. Eur J Epidemiol 36:1123–1128. https://doi.org/10.1007/s10654-021-00802-z
Charlson ME, Carrozzino D, Guidi J et al (2022) Charlson comorbidity index: a critical review of clinimetric properties. Psychother Psychosom 91:8–35. https://doi.org/10.1159/000521288
Stekhoven DJ, Bühlmann P (2012) MissForest–non-parametric missing value imputation for mixed-type data. Bioinformatics 28:112–118. https://doi.org/10.1093/bioinformatics/btr597
Heffernan KS, Stoner L, London AS et al (2023) Estimated pulse wave velocity as a measure of vascular aging. PLoS One 18:e0280896. https://doi.org/10.1371/journal.pone.0280896
Lu Y, Pechlaner R, Cai J et al (2020) Trajectories of age-related arterial stiffness in Chinese men and women. J Am Coll Cardiol 75:870–880. https://doi.org/10.1016/j.jacc.2019.12.039
Lyle AN, Raaz U (2017) Killing me un-softly: causes and mechanisms of arterial stiffness recent highlights of ATVB: early career committee contribution. Arterioscler Thromb Vasc Biol 37:e1–e11. https://doi.org/10.1161/ATVBAHA.116.308563
Lacolley P, Regnault V, Segers P et al (2017) Vascular smooth muscle cells and arterial stiffening: relevance in development, aging, and disease. Physiol Rev 97:1555–1617. https://doi.org/10.1152/physrev.00003.2017
Donato AJ, Machin DR, Lesniewski LA (2018) Mechanisms of dysfunction in the aging vasculature and role in age-related disease. Circ Res 123:825–848. https://doi.org/10.1161/CIRCRESAHA.118.312563
Chirinos JA, Segers P, Hughes T et al (2019) Large artery stiffness in health and disease: JACC state-of-the-art review. J Am Coll Cardiol 74:1237–1263. https://doi.org/10.1016/j.jacc.2019.07.012
Yang T, Sun Y, Lu Z et al (2017) The impact of cerebrovascular aging on vascular cognitive impairment and dementia. Ageing Res Rev 34:15–29. https://doi.org/10.1016/j.arr.2016.09.007
Kim ED, Tanaka H, Ballew SH et al (2018) Associations between kidney disease measures and regional pulse wave velocity in a large community-based cohort: the atherosclerosis risk in communities (ARIC) study. Am J Kidney Dis 72:682–690. https://doi.org/10.1053/j.ajkd.2018.04.018
Landers-Ramos RQ, Prior SJ (2018) The microvasculature and skeletal muscle health in aging. Exerc Sport Sci Rev 46:172–179. https://doi.org/10.1249/JES.0000000000000151
Kim ED, Ballew SH, Tanaka H et al (2019) Short-term prognostic impact of arterial stiffness in older adults without prevalent cardiovascular disease. Hypertension 74:1373–1382. https://doi.org/10.1161/HYPERTENSIONAHA.119.13496
Nilsson ED, Elmståhl S, Minthon L et al (2014) Nonlinear association between pulse wave velocity and cognitive function: a population-based study. J Hypertens 32:2152. https://doi.org/10.1097/HJH.0000000000000329
Chen Y, Shen F, Liu J et al (2017) Arterial stiffness and stroke: de-stiffening strategy, a therapeutic target for stroke. Stroke Vasc Neurol 2:65–72. https://doi.org/10.1136/svn-2016-000045
Cobos-Palacios L, Ruiz-Moreno MI, Muñoz-Ubeda M et al (2022) A healthy lifestyle is associated with lower arterial stiffness in a metabolically healthy elderly population with overweight or obesity. J Hypertens 40:1808–1814. https://doi.org/10.1097/HJH.0000000000003227
Jayanama K, Theou O, Godin J et al (2021) Relationship between diet quality scores and the risk of frailty and mortality in adults across a wide age spectrum. BMC Med 19:64. https://doi.org/10.1186/s12916-021-01918-5
Ward RE, Orkaby AR, Chen J et al (2020) Association between diet quality and frailty prevalence in the physicians’ health study. J Am Geriatr Soc 68:770–776. https://doi.org/10.1111/jgs.16286
Maddock J, Ziauddeen N, Ambrosini GL et al (2018) Adherence to a Dietary Approaches to Stop Hypertension (DASH)-type diet over the life course and associated vascular function: a study based on the MRC 1946 British birth cohort. Br J Nutr 119:581–589. https://doi.org/10.1017/S0007114517003877
Nordstrand N, Gjevestad E, Hertel JK et al (2013) Arterial stiffness, lifestyle intervention and a low-calorie diet in morbidly obese patients—a nonrandomized clinical trial. Obesity (Silver Spring) 21:690–697. https://doi.org/10.1002/oby.20099
Liu P, Li Y, Ma L (2021) Caloric restriction may help delay the onset of frailty and support frailty management. Front Nutr 8:731356. https://doi.org/10.3389/fnut.2021.731356
Millar CL, Dufour AB, Hebert JR et al (2022) Association of pro-inflammatory diet with frailty onset among adults with and without depressive symptoms: results from the Framingham Offspring Study. J Gerontol A Biol Sci Med Sci. https://doi.org/10.1093/gerona/glac140
Camargo-Ramos CM, Correa-Bautista JE, Correa-Rodríguez M et al (2017) Dietary inflammatory index and cardiometabolic risk parameters in overweight and sedentary subjects. Int J Environ Res Public Health 14:1104. https://doi.org/10.3390/ijerph14101104
Acknowledgements
The authors thank all contributors and participants of NAHNES.
Funding
This work was supported by the National Natural Science Foundation of China (Grant no. 81974566) and the Jinan “University 20” Project (Grant no. 2020GXRC017).
Author information
Authors and Affiliations
Contributions
YLH conducted analyses and wrote the article. XJW, JMH, LZ, LL, and YL collected and assembled the data. YLH and YLL conceived the study design. All authors have contributed to the interpretation of the results and have critically revised the content of the manuscript. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the National Center for Health Statistics (NCHS) Research Ethics Review Board (Protocols #98-12, #2005-06, #2011-17, and #2018-01).
Statement of human and animal rights
This study does not include any animal studies conducted by the authors and adheres to the guidelines for conducting research involving human participants.
Consent to participate
NHANES is a public dataset and all participants provided a written informed consent.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hu, Y., Huan, J., Wang, X. et al. Association of estimated carotid-femoral pulse wave velocity with frailty in middle-aged and older adults with cardiometabolic disease. Aging Clin Exp Res 35, 2425–2436 (2023). https://doi.org/10.1007/s40520-023-02556-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02556-y