Abstract
Aim
The impact of frailty, a physiological state characterized by reduced reserve for stressors and related to worse outcomes, on older adults during the pandemic is unclear. Our aim was to identify the effects of frailty among older adults during the COVID-19 pandemic.
Methods
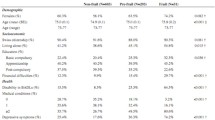
A total of 197 older adults who were not exposed to COVID-19 were assessed with an online survey one year after the pandemic began in Turkey. Frailty, quality of life, and fear of COVID-19 were assessed with the Tilburg Frailty Indicator, the Nottingham Health Profile, and the Fear of COVID-19 Scale, respectively. Since March 2020, changes in pain severity and localization, fatigue, and fear of falling were assessed. Multiple linear regression analyses were conducted.
Results
In this study, 62.5% of the participants were frail. The prevalence of pain was significantly increased during the COVID-19 pandemic, but only among the frail. The increases in pain severity, fear of falling, and fatigue were significantly higher for the frail than the non-frail. The model including physical and psychological components of frailty and pain severity explained 49% of the variation in quality of life (R = 0.696; R2 = 0.485; p < 0.001). The physical component of frailty had the highest impact on quality of life (B = 20.591; β = 0.334).
Conclusion
This study focused on negative outcomes that were experienced more by frail older adults compared to non-frail older adults when they were locked down at home for an extended period of time during the COVID-19 pandemic. It is necessary to quickly improve and maintain the health of these affected individuals.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Sepúlveda-Loyola W, Rodríguez-Sánchez I, Pérez-Rodríguez P et al (2020) Impact of social isolation due to COVID-19 on health in older people: mental and physical effects and recommendations. Nutr Health Aging 24:938–947. https://doi.org/10.1007/s12603-020-1500-7
Martínez-de-Quel Ó, Suárez-Iglesias D, López-Flores M et al (2021) Physical activity, dietary habits and sleep quality before and during COVID-19 lockdown: a longitudinal study. Appetite 158:105019. https://doi.org/10.1016/j.appet.2020.105019
Roggio F, Trovato B, Ravalli S et al (2021) One year of COVID-19 pandemic in Italy: effect of sedentary behavior on physical activity levels and musculoskeletal pain among university students. Int J Environ Res Public Health 18:680. https://doi.org/10.3390/ijerph18168680
Damiot A, Pinto AJ, Turner JE et al (2020) Immunological implications of physical inactivity among older adults during the COVID-19 pandemic. Gerontol 66:431–438. https://doi.org/10.1159/000509216
Karayannis NV, Baumann I, Sturgeon JA et al (2019) The impact of social isolation on pain interference: a longitudinal study. Ann Behav Med 53:65–74. https://doi.org/10.1093/abm/kay017
Saraiva M, Apolinario D, Avelino-Silva T et al (2021) The impact of frailty on the relationship between life-space mobility and quality of life in older adults during the COVID-19 pandemic. J Nutr Health Aging 25:440–447. https://doi.org/10.1007/s12603-020-1532-z
Pérez LM, Castellano-Tejedor C, Cesari M et al (2021) Depressive symptoms, fatigue and social relationships influenced physical activity in frail older community-dwellers during the Spanish lockdown due to the COVID-19 pandemic. Int J Environ Res Public Health 18:808. https://doi.org/10.3390/ijerph18020808
Cesari M, Calvani R, Marzetti E (2017) Frailty in older persons. Clin Geriatr Med 33:293–303. https://doi.org/10.1016/j.cger.2017.02.002
Ruiz M, Cefalu C, Reske T (2012) Frailty syndrome in geriatric medicine. Am J Med Sci 344:395–398. https://doi.org/10.1097/MAJ.0b013e318256c6aa
Soysal P, Stubbs B, Lucato P et al (2016) Inflammation and frailty in the elderly: a systematic review and meta-analysis. Ageing Res Rev 31:1–8. https://doi.org/10.1016/j.arr.2016.08.006
Smith KJ, Gavey S, RIddell NE et al (2020) The association between loneliness, social isolation and inflammation: a systematic review and meta-analysis. Neurosci Biobehav Rev 112:519–541. https://doi.org/10.1016/j.neubiorev.2020.02.002
Koop MA, Lutke Schipholt IJ, Scholten-Peeters GG et al (2021) Identifying the most important confounders when assessing the association between low-grade systemic inflammation and musculoskeletal pain: a modified Delphi study. Pain Med 22:2661–2669. https://doi.org/10.1093/pm/pnab243
Rockwood K (2005) What would make a definition of frailty successful? Age ageing 34:432–434. https://doi.org/10.1093/ageing/afi146
Bijur PE, Silver W, Gallagher EJ (2001) Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med 8:1153–1157. https://doi.org/10.1111/j.1553-2712.2001.tb01132.x
Hoffman GJ, Malani PN, Solway E et al (2022) Changes in activity levels, physical functioning, and fall risk during the COVID-19 pandemic. J Am Geriatr Soc 70:49–59. https://doi.org/10.1111/jgs.17477
Arslan M, Koç EM, Sözmen MK (2018) The Turkish adaptation of the tilburg frailty indicator: a validity and reliability study. Turk Geriatri Derg 21:173–183. https://doi.org/10.31086/tjgeri.2018240418
Gobbens RJ, Uchmanowicz I (2021) Assessing frailty with the Tilburg Frailty Indicator (TFI): a review of reliability and validity. Clin Interv Aging 16:863–875. https://doi.org/10.2147/CIA.S298191
Kücükdeveci A, McKenna S, Kutlay S et al (2000) The development and psychometric assessment of the Turkish version of the Nottingham Health Profile. Int J Rehabil Res 23:31–38. https://doi.org/10.1097/00004356-200023010-00004
Ahorsu DK, Lin C-Y, Imani V et al (2022) The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict 20:1537–1545. https://doi.org/10.1007/s11469-020-00270-8
Satici B, Gocet-Tekin E, Deniz M et al (2021) Adaptation of the Fear of COVID-19 Scale: Its association with psychological distress and life satisfaction in Turkey. Int J Ment Health Addict 19:1980–1988. https://doi.org/10.1007/s11469-020-00294-0
Schober P, Boer C, Schwarte LA (2018) Correlation coefficients: appropriate use and interpretation. Anaesth Analg 126:1763–1768. https://doi.org/10.1213/ANE.0000000000002864
Demirdel E, Demirdel S, Karahan S et al (2021) The cons of COVID-19 restrictions on physical activity in the elderly; results of an online survey. Turk Geriatri Derg. https://doi.org/10.31086/tjgeri.2021.197
Machón Sobrado M, Mateo-Abad M, Vrotsou K et al (2021) Health status and lifestyle habits of vulnerable, community-dwelling older people during the COVID-19 lockdown. J Frailty Aging 10:286–289. https://doi.org/10.14283/jfa.2021.12
İlhan B, Bahat G, Erdoğan T et al (2019) Chronic pain: prevalent and independently associated with frailty and female gender in geriatric outpatients. Eur Geriatr Med 10:931–937. https://doi.org/10.1007/s41999-019-00235-8
Wilkie R, Peat G, Thomas E et al (2007) Factors associated with restricted mobility outside the home in community-dwelling adults ages fifty years and older with knee pain: an example of use of the international classification of functioning to investigate participation restriction. Arthritis Care Res 57:1381–1389. https://doi.org/10.1002/art.23083
De Souza IMB, Sakaguchi TF, Yuan SLK et al (2019) Prevalence of low back pain in the elderly population: a systematic review. Clinics 74:e789. https://doi.org/10.6061/clinics/2019/e789
Korhonen N, Kannus P, Niemi S et al (2013) Fall-induced deaths among older adults: nationwide statistics in Finland between 1971 and 2009 and prediction for the future. Injury 44:867–871. https://doi.org/10.1016/j.injury.2013.03.004
Theou O, Jones GR, Overend TJ et al (2008) An exploration of the association between frailty and muscle fatigue. Appl Physiol Nutr Metab 33:651–665. https://doi.org/10.1139/H08-058
Lang P-O, Michel J-P, Zekry D (2009) Frailty syndrome: a transitional state in a dynamic process. Gerontol 55:539–549. https://doi.org/10.1159/000211949
CDC COVID-19 Response Team (2020) Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19). MMWR Morb Mortal Wkly Rep 69:343–346
Mistry SK, Ali A, Akther F et al (2021) Exploring fear of COVID-19 and its correlates among older adults in Bangladesh. Glob Health 17:1–9. https://doi.org/10.1186/s12992-021-00698-0
Espinoza SE, Jung I, Hazuda H (2012) Frailty transitions in the San Antonio longitudinal study of aging. J Am Geriatr Soc 60:652–660. https://doi.org/10.1111/j.1532-5415.2011.03882.x
Belloni G, Büla C, Santos-Eggimann B et al (2020) A single question as a screening tool to assess fear of falling in young-old community-dwelling persons. J Am Med Dir Assoc 21:1295-1301.e1292. https://doi.org/10.1016/j.jamda.2020.01.101
Funding
This study did not receive financial support.
Author information
Authors and Affiliations
Contributions
UKS: conceptualization, methodology, data collection, statistical analysis, writing, investigation. HD: data collection, writing, statistical analysis. NK: data collection, writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Ethical approval
The study design and all procedures in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Ethics Committee of Trabzon Kanuni Training and Research Hospital—2021/47), as well as the 1964 Helsinki Declaration and its subsequent amendments or comparable ethical standards.
Human and animal rights disclosure
This article does not involve any studies with animals performed by any of the authors.
Informed consent
All individual participants in the research gave their informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sahin, U.K., Durdu, H. & Korkmaz, N. The role of frailty on quality of life in older adults during the COVID-19 pandemic. Aging Clin Exp Res 35, 1779–1787 (2023). https://doi.org/10.1007/s40520-023-02469-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02469-w