Abstract
Background
Gustatory stimulus interventions have been shown to improve swallowing function in older adults with dysphagia. However, the optimal intervention strategies as well as their effects and safety remain unclear.
Aims
To explore current evidence regarding gustatory stimulus interventions for dysphagia in older adults.
Methods
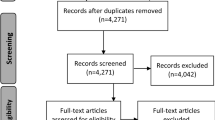
Nine electronic databases (PubMed, Web of Science, Embase, CINAHL, Cochrane Library, China National Knowledge Infrastructure, Wanfang Database, China Science and Technology Journal Database, and Sinomed) were searched from their inception to August 2022.
Results
This review identified 263 articles, and 15 met the inclusion criteria. The types of gustatory stimulus interventions included spicy (n = 10), sour (n = 3), and mixed (sour–sweet) stimuli (n = 2), with most studies focusing on spicy stimuli. The most frequently reported spicy stimulus was capsaicin. Further, the most commonly reported intervention frequency was thrice a day before meals for 1–4 weeks. The stimuli concentrations and dosages could not be standardized due to the among-study heterogeneity. These studies reported 16 assessment tools and 42 outcomes, which mainly included videofluoroscopy and swallowing response time respectively. More than half of the included studies reported no adverse effects of gustatory stimulus interventions.
Conclusion and discussions
Gustatory stimulus interventions improved swallowing function in older adults with dysphagia. However, assessment tools and outcomes for dysphagia should be standardized in the future, and explore personalized interventions based on different diseases and their stages, to determine the most cost-effective interventions, and to prevent its complications.

Similar content being viewed by others
Data availability
All data supporting the findings of this study are available within the paper and its supplementary information files.
References
McCarty EB, Chao TN (2021) Dysphagia and swallowing disorders. Med Clin North Am 105:939–954. https://doi.org/10.1016/j.mcna.2021.05.013
Braun T, Doerr JM, Peters L et al (2022) Age-related changes in oral sensitivity, taste and smell. Sci Rep 12:1533. https://doi.org/10.1038/s41598-022-05201-2
Herrera C, Quilez R, Castro ME et al (2014) Dysphagia in the elderly. Rev Esp Geriatr Gerontol 49:243–244. https://doi.org/10.1016/j.regg.2014.02.001
Wirth R, Dziewas R, Beck AM et al (2016) Oropharyngeal dysphagia in older persons—from pathophysiology to adequate intervention: a review and summary of an international expert meeting. Clin Interv Aging 11:189–208. https://doi.org/10.2147/cia.S97481
Jardine M, Miles A, Allen J (2020) A systematic review of physiological changes in swallowing in the oldest old. Dysphagia 35:509–532. https://doi.org/10.1007/s00455-019-10056-3
Austbø Holteng LB, Frøiland CT, Corbett A et al (2017) Care staff perspective on use of texture modified food in care home residents with dysphagia and dementia. Ann Palliat Med 6:310–318. https://doi.org/10.21037/apm.2017.06.24
Partridge L, Deelen J, Slagboom PE (2018) Facing up to the global challenges of ageing. Nature 561:45–56. https://doi.org/10.1038/s41586-018-0457-8
Hashimoto H, Hirata M, Takahashi K et al (2018) Non-invasive quantification of human swallowing using a simple motion tracking system. Sci Rep 8:5095. https://doi.org/10.1038/s41598-018-23486-0
Benjapornlert P, Kagaya H, Shibata S et al (2020) The prevalence and findings of fibre-optic endoscopic evaluation of swallowing in hospitalised patients with dysphagia. J Oral Rehabil 47:983–988. https://doi.org/10.1111/joor.13026
Rogus-Pulia N, Wirth R, Sloane PD (2018) Dysphagia in frail older persons: making the most of current knowledge. J Am Med Dir Assoc 19:736–740. https://doi.org/10.1016/j.jamda.2018.07.018
Mandell LA, Niederman MS (2019) Aspiration pneumonia. N Engl J Med 380:651–663. https://doi.org/10.1056/NEJMra1714562
Ortega O, Martin A, Clave P (2017) Diagnosis and management of oropharyngeal dysphagia among older persons, state of the art. J Am Med Dir Assoc 18:576–582. https://doi.org/10.1016/j.jamda.2017.02.015
Estupiñán Artiles C, Regan J, Donnellan C (2021) Dysphagia screening in residential care settings: A scoping review. Int J Nurs Stud 114:103813. https://doi.org/10.1016/j.ijnurstu.2020.103813
Marin S, Serra-Prat M, Ortega O et al (2021) Healthcare costs of post-stroke oropharyngeal dysphagia and its complications: malnutrition and respiratory infections. Eur J Neurol 28:3670–3681. https://doi.org/10.1111/ene.14998
Rommel N, Hamdy S (2016) Oropharyngeal dysphagia: manifestations and diagnosis. Nat Rev Gastroenterol Hepatol 13:49–59. https://doi.org/10.1038/nrgastro.2015.199
Thiyagalingam S, Kulinski AE, Thorsteinsdottir B et al (2021) Dysphagia in older adults. Mayo Clin Proc 96:488–497. https://doi.org/10.1016/j.mayocp.2020.08.001
Di Pede C, Mantovani ME, Del Felice A et al (2016) Dysphagia in the elderly: focus on rehabilitation strategies. Aging Clin Exp Res 28:607–617. https://doi.org/10.1007/s40520-015-0481-6
Molina L, Santos-Ruiz S, Clavé P et al (2018) Nursing interventions in adult patients with oropharyngeal dysphagia: a systematic review. Eur Geriatr Med 9:5–21. https://doi.org/10.1007/s41999-017-0009-z
Li C, Qiu C, Shi Y et al (2022) Experiences and perceptions of stroke patients living with dysphagia: a qualitative meta-synthesis. J Clin Nurs 31:820–831. https://doi.org/10.1111/jocn.15995
Baba M, Saitoh E, Okada S (2008) Dysphagia rehabilitation in Japan. Phys Med Rehabil Clin N Am 19:x. https://doi.org/10.1016/j.pmr.2008.07.002
Hossain MZ, Ando H, Unno S et al (2020) Targeting chemosensory ion channels in peripheral swallowing-related regions for the management of oropharyngeal dysphagia. Int J Mol Sci 21:42. https://doi.org/10.3390/ijms21176214
Christmas C, Rogus-Pulia N (2019) Swallowing disorders in the older population. J Am Geriatr Soc 67:2643–2649. https://doi.org/10.1111/jgs.16137
Ebihara S, Naito T (2022) A systematic review of reported methods of stimulating swallowing function and their classification. Tohoku J Exp Med 256:1–17. https://doi.org/10.1620/tjem.256.1
Wu XS, Miles A, Braakhuis AJ (2021) Texture-modified diets, nutritional status and mealtime satisfaction: a systematic review. healthcare (Basel) 9. https://doi.org/10.3390/healthcare9060624
Cohen DL, Roffe C, Beavan J et al (2016) Post-stroke dysphagia: a review and design considerations for future trials. Int J Stroke 11:399–411. https://doi.org/10.1177/1747493016639057
Dou Z (2017) Evaluation and Treatment of Dysphagia Second Edition. BeiJing.
Kaindlstorfer A, Pointner R (2016) An appraisal of current dysphagia diagnosis and treatment strategies. Expert Rev Gastroenterol Hepatol 10:929–942. https://doi.org/10.1586/17474124.2016.1158098
Battel I, Calvo I, Walshe M (2021) Interventions involving biofeedback to improve swallowing in people with parkinson disease and dysphagia: a systematic review. Arch Phys Med Rehabil 102:314–322. https://doi.org/10.1016/j.apmr.2020.06.033
van de Wetering-van Dongen VA, Kalf JG, van der Wees PJ et al (2020) The effects of respiratory training in parkinson’s disease: a systematic review. J Parkinsons Dis 10:1315–1333. https://doi.org/10.3233/jpd-202223
Mancopes R, Smaoui S, Steele CM (2020) Effects of expiratory muscle strength training on videofluoroscopic measures of swallowing: a systematic review. Am J Speech Lang Pathol 29:335–356. https://doi.org/10.1044/2019_ajslp-19-00107
Cheng I, Hamdy S (2022) Metaplasticity in the human swallowing system: clinical implications for dysphagia rehabilitation. Neurol Sci 43:199–209. https://doi.org/10.1007/s10072-021-05654-9
Rofes L, Arreola V, Martin A et al (2014) Effect of oral piperine on the swallow response of patients with oropharyngeal dysphagia. J Gastroenterol 49:1517–1523. https://doi.org/10.1007/s00535-013-0920-0
Mores S, Vandenberghe LPS, Magalhães Júnior AI et al (2021) Citric acid bioproduction and downstream processing: Status, opportunities, and challenges. Bioresour Technol 320:124426. https://doi.org/10.1016/j.biortech.2020.124426
French SA (2003) Pricing effects on food choices. J Nutr 133:841s–843s. https://doi.org/10.1093/jn/133.3.841S
Cabib C, Nascimento W, Rofes L et al (2020) Short-term neurophysiological effects of sensory pathway neurorehabilitation strategies on chronic poststroke oropharyngeal dysphagia. Neurogastroenterol Motil 32:14. https://doi.org/10.1111/nmo.13887
Peña-Chávez RE, Schaen-Heacock NE, Hitchcock ME et al (2022) Effects of food and liquid properties on swallowing physiology and function in adults. Dysphagia. https://doi.org/10.1007/s00455-022-10525-2
Mulheren R, Westemeyer RM, Dietsch AM (2022) The effect of taste on swallowing: A scoping and systematic review. Crit Rev Food Sci Nutr:1–27. https://doi.org/10.1080/10408398.2022.2115003
Colquhoun HL, Levac D, O’Brien KK et al (2014) Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol 67:1291–1294. https://doi.org/10.1016/j.jclinepi.2014.03.013
Tricco AC, Lillie E, Zarin W et al (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169:467–473. https://doi.org/10.7326/m18-0850
Z. AEM (2020) JBI Manual for Evidence Synthesis. JBI. https://jbi-global-wiki.refined.site/space/MANUAL. Accessed 29 April 2022.
Lockwood C, dos Santos KB, Pap R (2019) Practical guidance for knowledge synthesis: scoping review methods. Asian Nurs Res (Korean Soc Nurs Sci) 13:287–294. https://doi.org/10.1016/j.anr.2019.11.002
Wang Z, Wu L, Fang Q et al (2019) Effects of capsaicin on swallowing function in stroke patients with dysphagia: a randomized controlled trial. J Stroke Cerebrovasc Dis 28:1744–1751. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.02.008
Tomsen N, Ortega O, Rofes L et al (2019) Acute and subacute effects of oropharyngeal sensory stimulation with TRPV1 agonists in older patients with oropharyngeal dysphagia: a biomechanical and neurophysiological randomized pilot study. Therap Adv Gastroenterol 12:1756284819842043. https://doi.org/10.1177/1756284819842043
Alvarez-Berdugo D, Rofes L, Arreola V et al (2018) A comparative study on the therapeutic effect of TRPV1, TRPA1, and TRPM8 agonists on swallowing dysfunction associated with aging and neurological diseases. Neurogastroenterol Motil 30. https://doi.org/10.1111/nmo.13185
Nakato R, Manabe N, Shimizu S et al (2017) Effects of capsaicin on older patients with oropharyngeal dysphagia: a double-blind, placebo-controlled, crossover study. Digestion 95:210–220. https://doi.org/10.1159/000463382
Ortega O, Rofes L, Martin A et al (2016) A comparative study between two sensory stimulation strategies after two weeks treatment on older patients with oropharyngeal dysphagia. Dysphagia 31:706–716. https://doi.org/10.1007/s00455-016-9736-4
Ebihara T, Takahashi H, Ebihara S et al (2005) Capsaicin troche for swallowing dysfunction in older people. J Am Geriatr Soc 53:824–828. https://doi.org/10.1111/j.1532-5415.2005.53261.x
Rofes L, Arreola V, Martin A et al (2013) Natural capsaicinoids improve swallow response in older patients with oropharyngeal dysphagia. Gut 62:1280–1287. https://doi.org/10.1136/gutjnl-2011-300753
Hamdy S, Jilani S, Price V et al (2003) Modulation of human swallowing behaviour by thermal and chemical stimulation in health and after brain injury. Neurogastroenterol Motil 15:69–77. https://doi.org/10.1046/j.1365-2982.2003.00390.x
Pauloski BR, Nasir SM (2016) Orosensory contributions to dysphagia: a link between perception of sweet and sour taste and pharyngeal delay time. Physiol Rep 4. https://doi.org/10.14814/phy2.12752
Gatto AR, Cola PC, Silva RG et al (2013) Sour taste and cold temperature in the oral phase of swallowing in patients after stroke. Codas 25:164–168. https://doi.org/10.1590/s2317-17822013000200012
Pelletier CA, Lawless HT (2003) Effect of citric acid and citric acid-sucrose mixtures on swallowing in neurogenic oropharyngeal dysphagia. Dysphagia 18:231–241. https://doi.org/10.1007/s00455-003-0013-y
Regan J (2020) Impact of sensory stimulation on pharyngo-esophageal swallowing biomechanics in adults with dysphagia: a high-resolution manometry study. Dysphagia 35:825–833. https://doi.org/10.1007/s00455-019-10088-9
Nascimento W, Tomsen N, Acedo S et al (2021) Effect of Aging, Gender and Sensory Stimulation of TRPV1 Receptors with Capsaicin on Spontaneous Swallowing Frequency in Patients with Oropharyngeal Dysphagia: A Proof-of-Concept Study. Diagnostics (Basel) 11. https://doi.org/10.3390/diagnostics11030461
Sporns PB, Muhle P, Hanning U et al (2017) Atrophy of swallowing muscles is associated with severity of dysphagia and age in patients with acute stroke. J Am Med Dir Assoc 18:635.e631-635.e637. https://doi.org/10.1016/j.jamda.2017.02.002
Azzolino D, Damanti S, Bertagnoli L et al (2019) Sarcopenia and swallowing disorders in older people. Aging Clin Exp Res 31:799–805. https://doi.org/10.1007/s40520-019-01128-3
Teismann IK, Steinstraeter O, Stoeckigt K et al (2007) Functional oropharyngeal sensory disruption interferes with the cortical control of swallowing. BMC Neurosci 8:62. https://doi.org/10.1186/1471-2202-8-62
He L, Yadgarov A, Sharif S et al (2012) Aging profoundly delays functional recovery from gustatory nerve injury. Neuroscience 209:208–218. https://doi.org/10.1016/j.neuroscience.2012.02.012
Barritt AW, Smithard DG (2009) Role of cerebral cortex plasticity in the recovery of swallowing function following dysphagic stroke. Dysphagia 24:83–90. https://doi.org/10.1007/s00455-008-9162-3
Singh S, Hamdy S (2006) Dysphagia in stroke patients. Postgrad Med J 82:383–391. https://doi.org/10.1136/pgmj.2005.043281
Panebianco M, Marchese-Ragona R, Masiero S et al (2020) Dysphagia in neurological diseases: a literature review. Neurol Sci 41:3067–3073. https://doi.org/10.1007/s10072-020-04495-2
Martin C, Neyraud E (2021) Impact of Very Hot Drink Consumption Habits, Age, and Sex, on Taste Sensitivity. Foods 10. https://doi.org/10.3390/foods10051139
Chamoun E, Carroll NA, Duizer LM et al (2018) The Relationship between Single Nucleotide Polymorphisms in Taste Receptor Genes, Taste Function and Dietary Intake in Preschool-Aged Children and Adults in the Guelph Family Health Study. Nutrients 10. https://doi.org/10.3390/nu10080990
Zhu Z, Mei J, Sun S et al (2021) Nutrigenomics reveals potential genetic underpinning of diverse taste preference of Chinese men. Genes Genomics 43:689–699. https://doi.org/10.1007/s13258-021-01079-y
Nagy A, Steele CM, Pelletier CA (2014) Barium versus nonbarium stimuli: differences in taste intensity, chemesthesis, and swallowing behavior in healthy adult women. J Speech Lang Hear Res 57:758–767. https://doi.org/10.1044/2013_jslhr-s-13-0136
Nagy A, Steele CM, Pelletier CA (2014) Differences in swallowing between high and low concentration taste stimuli. Biomed Res Int 2014:813084. https://doi.org/10.1155/2014/813084
Qu X, Na X, Yang J et al (2022) Reaching and maintaining higher dietary diversity is associated with decreased risk of all-cause mortality: A longitudinal study from the China Health and Nutrition Survey. Front Nutr 9:947290. https://doi.org/10.3389/fnut.2022.947290
Colvin JL, Pullicin AJ, Lim J (2018) Regional differences in taste responsiveness: effect of stimulus and tasting mode. Chem Senses 43:645–653. https://doi.org/10.1093/chemse/bjy055
Doty RL (2012) Gustation. Wiley Interdiscip Rev. Cogn Sci 3:29–46. https://doi.org/10.1002/wcs.156
Fernández-Rosati J, Lera L, Fuentes-López E et al (2018) Validation of the eat-10 score to detect dysphagia in older people. Rev Med Chil 146:1008–1015. https://doi.org/10.4067/s0034-98872018000901008
Speyer R, Cordier R, Farneti D et al (2022) White paper by the european society for swallowing disorders: screening and non-instrumental assessment for dysphagia in adults. Dysphagia 37:333–349. https://doi.org/10.1007/s00455-021-10283-7
Birchall O, Bennett M, Lawson N et al (2021) Instrumental swallowing assessment in adults in residential aged care homes: a scoping review. J Am Med Dir Assoc 22:372-379.e376. https://doi.org/10.1016/j.jamda.2020.08.028
Aroke EN, Powell-Roach KL, Jaime-Lara RB et al (2020) Taste the Pain: The Role of TRP Channels in Pain and Taste Perception. Int J Mol Sci 21. https://doi.org/10.3390/ijms21165929
Tomsen N, Alvarez-Berdugo D, Rofes L et al (2020) A randomized clinical trial on the acute therapeutic effect of TRPA1 and TRPM8 agonists in patients with oropharyngeal dysphagia. Neurogastroenterol Motil 32:e13821. https://doi.org/10.1111/nmo.13821
Roper SD (2014) TRPs in taste and chemesthesis. Handb Exp Pharmacol 223:827–871. https://doi.org/10.1007/978-3-319-05161-1_5
Viana F (2011) Chemosensory properties of the trigeminal system. ACS Chem Neurosci 2:38–50. https://doi.org/10.1021/cn100102c
Kittipanya-ngam P, Benjapornlert P, Rattanakanokchai S et al (2021) Effect of TRP-stimulating compounds to reduce swallowing response time in the elderly: a systematic review. Dysphagia 36:614–622. https://doi.org/10.1007/s00455-020-10175-2
Funding
This work was supported by the National Natural Science Foundation of China (No. 71871147); the Science and Technology Department of Sichuan Province (No. 2021YJ0013); and West China Nursing Discipline Development Special Fund Project, Sichuan University (No. HXHL20023).
Author information
Authors and Affiliations
Contributions
Conceptualization: WJ, YZ, and FZ; Analysis: WJ, YZ, and LH; Writing—Original draft: WJ and YZ; Visualization: WJ, YZ, and LH; Methodology: WJ, YZ, YZ, LDX, and FZ; Writing—review & editing: YZ, LDX, QC, and FZ; Supervision: FZ; Funding acquisition: FZ.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there was no conflict of interest.
Ethical approval
This is a scoping review, and ethical approval was not required.
Informed consent
Due to the type of this article, informed consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, W., Zou, Y., Huang, L. et al. Gustatory stimulus interventions for older adults with dysphagia: a scoping review. Aging Clin Exp Res 35, 1429–1442 (2023). https://doi.org/10.1007/s40520-023-02437-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02437-4