Abstract
Background
Cerebrospinal fluid (CSF) growth-associated protein 43 (GAP-43) is prominently elevated in Alzheimer’s disease (AD) dementia patients in comparison to normal controls. CSF GAP-43 levels in mild cognitive impairment (MCI) individuals who have different clinical trajectories need to be studied.
Methods
We examined 137 cognitively normal (CN) controls, 218 stable MCI patients (sMCI), 99 progressive MCI (pMCI) patients, and 120 AD dementia patients. Associations between the CSF GAP-43 levels and the four diagnosis groups were evaluated with multiple-variable linear regression. The relationships between CSF GAP-43 and core CSF biomarkers were assessed by Spearman correlations. Cox regression analysis was performed to assess the values of GAP-43 in predicting MCI conversion. We examined associations between baseline CSF GAP-43 levels and longitudinal cognitive function, hippocampal volumes, and brain glucose metabolism using linear mixed-effects models.
Results
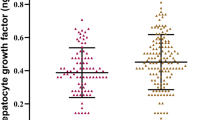
CSF GAP-43 was elevated in the pMCI and AD groups in comparison to the CN group and in the pMCI and AD groups in comparison to the sMCI group. CSF GAP-43 significantly predicted conversion from MCI to AD. CSF GAP-43 was a significant predictor of cognitive decline, hippocampal atrophy, and brain hypometabolism over time. Furthermore, elevated CSF GAP-43 levels were associated with accelerated deterioration in cognition and neurodegeneration.
Conclusions
CSF GAP-43 is increased in the predementia stage of AD, and it may enhance the neurodegenerative process. Future efforts on pharmacological interventions targeting synaptic dysfunction could be promising in AD treatment.




Similar content being viewed by others
Data availability
The data sets analyzed during the current study are available upon request with no restriction.
References
Winblad B, Amouyel P, Andrieu S et al (2016) Defeating Alzheimer’s disease and other dementias: a priority for European science and society. Lancet Neurol 15:455–532
Deture MA, Dickson DW (2019) The neuropathological diagnosis of Alzheimer’s disease. Mol Neurodegener 14:32
Jack CR Jr, Bennett DA, Blennow K et al (2018) NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement 14:535–562
Gauthier S, Reisberg B, Zaudig M et al (2006) International psychogeriatric association expert conference on. Mild cognitive impairment Mild cognitive impairment. Lancet 36:1262–1270
Mitchell AJ, Shiri-Feshki M (2009) Rate of progression of mild cognitive impairment to dementia–meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand 119:252–265
John A, Reddy PH (2021) Synaptic basis of Alzheimer’s disease: focus on synaptic amyloid beta P-tau and mitochondria. Ageing Res Rev 65:101208
Chen Y, Fu AKY, Ip NY (2019) Synaptic dysfunction in Alzheimer’s disease: mechanisms and therapeutic strategies. Pharmacol Ther 195:186–198
Sjögren M, Minthon L, Davidsson P et al (2000) CSF levels of tau, β-amyloid 1–42 and GAP-43 in frontotemporal dementia, other types of dementia and normal aging. J Neural Transm 107:563–579
Skene JH, Jacobson RD, Snipes GJ et al (1986) A protein induced during nerve growth (GAP-43) is a major component of growth-cone membranes. Science 233:783–786
Allegra Mascaro AL, Cesare P, Sacconi L et al (2013) In vivo single branch axotomy induces GAP-43-dependent sprouting and synaptic remodeling in cerebellar cortex. Proc Natl Acad Sci USA 110:10824–10829
Camporesi E, Nilsson J, Brinkmalm A et al (2020) Fluid biomarkers for synaptic dysfunction and loss. Biomark Insights 15:1177271920950319
Denny JB (2006) Molecular mechanisms, biological actions, and neuropharmacology of the growth-associated protein GAP-43. Curr Neuropharmacol 4:293–304
Morita S, Miyata S (2013) Synaptic localization of growth-associated protein 43 in cultured hippocampal neurons during synaptogenesis. Cell Biochem Funct 31:400–411
Holahan MR, Honegger KS, Tabatadze N et al (2007) GAP-43 gene expression regulates information storage. Learning Mem (Cold Spring Harbor, N.Y.) 14:407–415
Bloniecki V, Zetterberg H, Aarsland D et al (2020) Are neuropsychiatric symptoms in dementia linked to CSF biomarkers of synaptic and axonal degeneration? Alz Res Therapy. https://doi.org/10.1111/j.1600-0447.2008.01326.x
Milà-Alomà M, Brinkmalm A, Ashton NJ et al (2021) CSF Synaptic biomarkers in the preclinical stage of Alzheimer disease and their association with MRI and PET: a cross-sectional study. Neurology 97:e2065–e2078
Sandelius Å, Portelius E, Källén Å et al (2019) Elevated CSF GAP 43 is Alzheimer’s disease specific and associated with tau and amyloid pathology. Alzheimers Dement 15:55–64
Sjögren M, Davidsson P, Gottfries J et al (2001) The cerebrospinal fluid levels of tau, growth-associated protein-43 and soluble amyloid precursor protein correlate in Alzheimer’s disease, reflecting a common pathophysiological process. Dement Geriatr Cogn Disord 12:257–264
Zhang H, Lyu D, Jia J (2022) Alzheimer’s disease neuroimaging initiative. the trajectory of cerebrospinal fluid growth-associated protein 43 in the Alzheimer’s disease continuum: a longitudinal study. J Alzheimers Dis 85:1441–1452
Petersen RC, Aisen PS, Beckett LA et al (2010) Alzheimer’s disease neuroimaging initiative (ADNI): clinical characterization. Neurology 74:201–209
Berg L (1988) Clinical dementia rating (CDR). Psychopharmacol Bull 24:637–639
Aisen PS, Petersen RC, Donohue MC et al (2010) Clinical core of the Alzheimer’s disease neuroimaging initiative: progress and plans. Alzheimers Dement 6:239–246
McKhann G, Drachman D, Folstein M et al (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA work group under the auspices of department of health and human services task force on Alzheimer’s disease. Neurology 34:939–944
Tierney MC, Fisher RH, Lewis AJ et al (1988) The NINCDS-ADRDA work group criteria for the clinical diagnosis of probable Alzheimer’s disease: a clinicopathologic study of 57 cases. Neurology 38:359–364
Portelius E, Zetterberg H, Skillback T et al (2015) Cerebrospinal fluid neurogranin: relation to cognition and neurodegeneration in Alzheimer’s disease. Brain 138:3373–3385
Zhang H, Joseph T, Kang MS et al (2018) Cerebrospinal fluid synaptosomal-associated protein 25 is a key player in synaptic degeneration in mild cognitive impairment and Alzheimer’s disease. Alzheimers Res Ther 10:80
Jack CR Jr, Bernstein MA, Fox NC et al (2008) The Alzheimer’s disease neuroimaging initiative (ADNI): MRI methods. J Magn Reson Imaging 27:685–691
Landau SM, Harvey D, Madiso CM et al (2010) Comparing predictors of conversion and decline in mild cognitive impairment. Neurology 75:230–238
Masliah E, Mallory M, Alford M et al (2001) Altered expression of synaptic proteins occurs early during progression of Alzheimer’s disease. Neurology 56:127–129
Remnestål J, Just D, Mitsios N et al (2016) CSF profiling of the human brain enriched proteome reveals associations of neuromodulin and neurogranin to Alzheimer’s disease. Proteomics Clin Appl 10:1242–1253
Butt OH, Long JM, Henson RL et al (2021) Cognitively normal APOE ε4 carriers have specific elevation of CSF SNAP-25. Neurobiol Aging 102:64–72
Colom-Cadena M, Spires-Jones T, Zetterberg H et al (2020) The clinical promise of biomarkers of synapse damage or loss in Alzheimer’s disease. Alzheimers Res Ther 12:21
Öhrfelt A, Brinkmalm A, Dumurgier J et al (2019) A novel ELISA for the measurement of cerebrospinal fluid SNAP-25 in patients with Alzheimer’s disease. Neuroscience 420:136–144
Casaletto KB, Zetterberg H, Blennow K et al (2021) Tripartite relationship among synaptic, amyloid, and tau proteins: an in vivo and postmortem study. Neurology 97:e284–e297
Blennow K, Zetterberg H (2018) Biomarkers for Alzheimer’s disease: current status and prospects for the future. J Intern Med 284:643–663
Scheltens P, Blennow K, Breteler MM et al (2016) Alzheimer’s disease. Lancet 388:505–517
Pooler AM, Noble W, Hanger DP (2014) A role for tau at the synapse in Alzheimer’s disease pathogenesis. Neuropharmacology 76:1–8
Zhou L, McInnes J, Wierda K et al (2017) Tau association with synaptic vesicles causes presynaptic dysfunction. Nat Commun 8:15295
Arendt T (2009) Synaptic degeneration in Alzheimer’s disease. Acta Neuropathol 118:167–179
Heister D, Brewer JB, Magda S et al (2011) Predicting MCI outcome with clinically available MRI and CSF biomarkers. Neurology 77:1619–1628
Llano DA, Devanarayan P, Devanarayan V (2019) Alzheimer’s disease neuroimaging initiative (ADNI). VGF in cerebrospinal fluid combined with conventional biomarkers enhances prediction of conversion from MCI to AD. Alzheimer Dis Assoc Disord 33:307–314
Chung D, Shum A, Caraveo G (2020) GAP-43 and BASP1 in axon regeneration: implications for the treatment of neurodegenerative diseases. Front Cell Dev Biol 8:567537
Acknowledgements
Data collection and sharing for this project were sponsored by the Alzheimer’s Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012).
Funding
We do not have any financial support for this study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
Since the data in this paper were obtained from the ADNI, it does not include any research involving human or animal subjects.
Informed consent
For this type of study, formal consent is not required.
Consent for publication
All authors approved the final manuscript for submission and gave consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Data used to prepare this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in the analysis or writing of this report. A complete listing of ADNI investigators can be found at: http://adni.loni.usc.edu/wpcontent/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lu, Y., for the Alzheimer’s Disease Neuroimaging Initiative. Cerebrospinal fluid growth-associated protein 43 levels in patients with progressive and stable mild cognitive impairment. Aging Clin Exp Res 34, 2399–2406 (2022). https://doi.org/10.1007/s40520-022-02202-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02202-z