Abstract
Background
The positive effect of cardiac rehabilitation (CR) on outcomes after acute coronary syndromes (ACS) is established. Nevertheless, enrollment rates into CR programs remain low, although ACS carry a high risk of functional decline particularly in the elderly.
Aim
We aimed to determine if a multidisciplinary CR improves exercise capacity in an older population discharged after ACS systematically treated with PCI.
Methods
CR-AGE ACS is a prospective, single-center, cohort study. All patients aged 75+ years consecutively referred to Cardiac Rehabilitation outpatient Unit at Careggi University Hospital, were screened for eligibility. Moderate/severe cognitive impairment, disability in 2+ basic activities of daily living, musculoskeletal diseases, contraindication to Cardiopulmonary Exercise Test, and diseases with an expected survival < 6 months, were exclusion criteria. Participants attended a CR program, based on 5-day-per-week aerobic training sessions for 4 weeks.
Results
We enrolled 253 post-ACS patients with a mean age 80.6 ± 4.4 years. After CR, 136 (56.2%) 77 (31.3%) patients obtained, respectively, at least a moderate (∆+5%) or an optimal (∆+15%) increase in VO2peak. Baseline VO2peak (− 1 ml/kg/min: OR 1.18; 95% CI 1.09–1.28), the number of training sessions (+1 session: OR 1.07; 95% CI 1.01–1.15), and mild-to-moderate baseline disability (yes vs. no: OR 0.22; 95% CI 0.01–0.57) were the predictors of VO2peak changes.
Conclusions
A CR program started early after discharge from ACS produces a significant increase in exercise capacity in very old patients with mild-to-moderate post-acute physical impairment. Baseline VO2peak, the number of training sessions, and the level of baseline disability are the independent predictors of improvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The positive effects of cardiac rehabilitation (CR) on cardiovascular mortality, re-hospitalizations, and quality of life have been established [1] and current guidelines strongly suggest an early planning of interventional secondary prevention after acute coronary syndromes (ACS) [2, 3]. Few studies that enrolled elderly patients demonstrated a significant improvement in exercise capacity with CR also in this age cohort [4]. Despite proven benefits, CR enrollment rates remain remarkably low in the elderly in general, and in older women in particular [5]. Indeed, referral to CR at hospital discharge is even lower in patients treated with percutaneous coronary intervention (PCI) for ACS than after cardiac surgery [6], probably reflecting physicians’ perception that functional recovery is less stringently needed after ACS than after cardiac surgery [7]. Conversely, discharge from hospital where PCI has been performed [8] and where facilities for CR program are present [9], are strong positive predictors of referral to CR. The physician perception of less functional impact of ACS than cardiac surgery in the elderly [10] is contradicted by observations of about 30% of older patients having a remarkable functional decline six months after ACS, with an increased risk of long-term adverse events [10]. The need for multidisciplinary therapeutic interventions aimed at improving exercise capacity and reducing the risk of physical and also cognitive disability is becoming a priority in older cardiovascular patients [11]. Among different indexes of functional capacity, the maximal oxygen consumption (VO2peak, ml/kg/min) measured at cardiopulmonary exercise test (CPET) remains a gold standard [11, 12].
With the aim of investigating the effect of CR in older patients [13], we have conducted the Cardiac Rehabilitation in Advanced aGE (CR-AGE) single-center, prospective study, which recently identified the subset of patients benefiting the most from CR in terms of improved exercise capacity [14].
Based on these premises, the present study was aimed at identifying the independent predictors of improvement in VO2peak at the end of a multidisciplinary CR program in an older population discharged after ACS systematically treated with PCI.
Methods
Over the last 10 years, 1580 patients older than 75 years have been discharged from our hospital after an ACS treated with PCI. In the absence of standardized procedure to refer eligible patients to CR, the referral decision was made by acute-care physicians and, therefore, was based only on physician’s clinical judgment and acknowledgement of potential CR benefits.
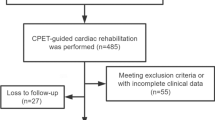
The CR-AGE protocol, including the description of the methods and data collected, has been detailed elsewhere [14] and can be summarized as follows. The program consists of 5-day-per-week sessions of aerobic exercise for 4 weeks, at an intensity corresponding to 60–70% of VO2peak measured in a baseline with a symptom-limited cardiopulmonary stress test as a measure of maximal functional capacity at the entry. This program duration reflects the length of CR usually provided by the Italian national healthcare system. Each session consists of 30 minutes of either biking or calisthenics on alternate days, with an expert physiotherapist supervising activities through telemetric ECG and non-invasive arterial blood pressure monitoring [14]. Based on the same protocol, in the present study we screened for eligibility for CR all patients aged 75+ years consecutively referred to our CR Unit (Fig. 1). Accordingly to the CRAGE protocol, moderate-to-severe cognitive impairment (Mini-Mental State Examination score < 18) [15], disability in 2+ basic activities of daily living (BADL) [16], ejection fraction equal or less 35%, musculoskeletal diseases or other absolute contraindication to CPET, and diseases with an expected survival < 6 months, were taken as exclusion criteria [14, 17].
All patients were evaluated through a comprehensive geriatric assessment process, which included the definition of chronic comorbidity burden [18], independence in activities of daily living, and psycho-emotional [19] and socio-economic profile. Loss of only one BADL and/or one or more instrumental ADL (IADL, 20) was taken to indicate mild-to moderate disability, but did not cause patient’s exclusion.
Functional evaluation
Changes in aerobic capacity at the end of the 4-week physical training (see below) was the main study outcome measure. Aerobic capacity was expressed as the VO2peak resulting from breath-to-breath analysis (CPX Medical Graphics system) during a symptom-limited CPET on cycle ergometer (Esaote Biomedica Formula). All participants screened for participation in study were prescribed the above described [14], 4-week training program.
CR program
The CR program was individually customized and the work load of exercise sessions, consisting of 30-minute biking or calisthenics on alternate days, was changed weekly according to the Borg rating of perceived exertion scale [21]. The calisthenics program consisted of a warm-up period followed by eight 2-minute exercises, each followed by 1-minute rest, and of stretching of the trunk muscles aimed at improving strength and flexibility and, hence, autonomy in common daily activities. A progressive increase in muscle resistance was reached by applying ankle or wristbands of increasing weight (0.5-1 kg), again based on the Borg rating of perceived exertion scale, which was re-evaluated weekly. As already reported, sessions were supervised by an expert physiotherapist, with telemetric ECG and non-invasive arterial pressure monitoring [22]. The study has been approved by the local ethics committee and has been conducted in accordance with the Declaration of Helsinki.
Statistical analysis
Data were analyzed using the SPSS 25.0 statistical package (SPSS, Inc., Chicago, IL). Continuous and categorical variables are reported respectively as mean ± standard error, or as N and percent. The univariable associations of demographic, clinical, and echocardiographic variables with indexes of exercise performance derived from CPET at the end of CR, were tested using Student’s t test and chi-square tests, as appropriate. For this analysis, according to the results of previous studies [14], thresholds indicating at least a moderate or an optimal increase in VO2peak from baseline to the end of CR program, were set respectively at > +5% and ≥ +15%. Variables significantly associated with either a moderate or an optimal final increase in VO2peak at univariable analysis, were entered into multivariable logistic models (with stepwise backward deletion), to identify the independent predictors of the two thresholds of exercise capacity increase. A p value < 0.05 was considered statistically significant.
Results
We consecutively enrolled 253 patients (Fig. 1) aged ≥ 75 years (mean age 80.6±4.4 years, range 75–94; 116 males, 65.6%) who had been treated with PCI during an ACS (156 STEMI, 61.7%; 96 NSTEMI/unstable angina, 37.9 %) (Table 1). Of these, 93 (36.8%) had a single-, 84 (33.2%) a two-, and 71 (31.1%) a three-vessel disease; 151 (59.3%) had had a complete coronary revascularization, and 177 (70.0%) had received at least one drug-eluting stent. The average intervals from ACS and from hospital discharge to enrollment were 19 ± 11 and 11 ± 10 days, respectively.
In accordance with the exclusion criteria, 80.5% of patients were independent in 6/6 BADL and only 23.8% had limitations in two or more IADL, while the average cognitive and psycho-emotional profiles were good, as indicated by a MMSE score of 27.6 ± 3.2 and a 15-item GDS score of 3.5 ± 3.0. A Charlson comorbidity index of 5.7 ± 1.6 indicated a moderate average burden of non-cardiovascular chronic comorbidity. Overall, the prescription rate of guidelines-recommended therapies after ACS at CR entry was very satisfying (Table 1), particularly if we consider the high mean age of the study population. Patients participated in 13±4 physical exercise sessions as previously described, under physiotherapist’s supervision.
Of 253 patients enrolled, 242 (94.2%) completed the whole CR program and underwent a final CPET before discharge (Fig. 1), whereas 11 patients initially enrolled could not attend the CR program due to lacking familial support or logistic difficulties. VO2peak and exercise duration remarkably and significantly improved from baseline to final evaluation (Fig. 2). When changes in VO2peak from baseline to the end of CR program were analyzed according to the two pre-defined thresholds, 136 (56.2%) and 77 (31.3%) resulted to have reached an increase in VO2peak > 5% or ≥ 15%, respectively. At univariable analysis, attainment of the lower threshold was significantly associated with number of IADL lost, presence of mild-to-moderate disability, baseline VO2peak, and the number of training sessions attended, while attainment of the upper threshold was associated with MMSE score, baseline VO2peak and the number of training sessions (Table 2).
At multivariable analysis, baseline VO2peak and the number of training sessions were the strongest independent predictors of both thresholds of VO2peak increase at the end of CR program, whereas the number of IADL preserved and the presence of mild-to-moderate disability were retained in the model as predictors of the lower threshold only, and the MMSE score was marginally associated with the upper threshold only (Table 3).
Discussion
The first finding of our study to be highlighted is the advanced mean age (greater than 80 years) of enrolled patients, who had all been treated with an early invasive strategy during an ACS. Such an aggressive strategy, together with the adopted exclusion criteria, likely resulted in a well preserved average clinical and functional profile that was associated with a high rate (94.2%) of patients completing the multidisciplinary 4-week outpatient CR program. Moreover, we confirmed the effectiveness of CR in improving the global exercise capacity also in such a geriatric cohort.
As known, physical-function maintenance is a crucial target for clinical interventions in the elderly, and exercise training is a key tool to improve and promote secondary prevention in coronary artery disease [22]. Nevertheless, an increase in physical exercise performance is of crucial importance for maintaining the independence in activities of daily living, and is associated with an improvement in health related quality of life [11]. In the elderly, this positive effect should be obtained soon [23] after ACS, to prevent the negative effects related to hospital stay, associated with deconditioning caused by muscle mass and strength loss that occurs even after a short length of stay [24]. In addition, an early CR program can contribute to rebuild patient’s confidence with physical activities [11] . Our structured CR programs are run by trained physiotherapists, who are in charge of coordinating tailored on-site exercise programs and, at the same time, of educating patients to continue the same programs at home. [14].
Despite all aforementioned positive results and derived clinical practice guidelines recommendations [5, 17], enrollment in CR still remains poor [7, 9] with physicians’ decision still resulting as the main barrier to enrollment [7]: in fact, many potentially eligible patients, particularly older adults, are not referred as a consequence of multiple factors such as health conditions, hospital policies, but also physicians’ unjustified perception of limited usefulness [8, 23]. Hopefully, in this perspective, our findings may contribute to contrast this phenomenon so difficult to explain in the light of the above described solid evidence in favor of CR referral, particularly in elderly patients.
Indeed, in a large US population [25], age resulted to be per se a significant barrier to patients referral to a CR program after PCI: in fact, every 5 years of increasing age caused a 2% reduction in the probability of being referred to CR, even after adjusting for cardiovascular risk profile, comorbidities, hospital facilities, type of insurance and ethnicity. In our study, only 17% of older patients discharged from hospital over 10 years have been referred to CR. These data are consistent with the literature, which reports that older adults are 1.5–2 times less likely to participate in CR, with a referral rate dropping to only 13% in those aged 80 + years [26, 27].
A further valuable finding of the present study is the achievement of a significant increase in VO2peak with multidisciplinary CR program in a large proportion of our study population. Moreover, we have confirmed in a large and more clinically uniform population of older patients with ischemic heart disease, the findings of our previous CR-AGE study [14], that greatest gains in exercise capacity occur in those who have the lowest baseline physical performance. In fact, we observed that for each ml/kg/min lower baseline VO2peak, there was an independent 18% increased probability to obtain a functionally remarkable increase in exercise tolerance. This finding reinforces the positive impact of an early referral of older patients to a CR program that can largely and rapidly improve the aerobic capacity particularly in those patients with the most impaired physical performance at hospital discharge [14]. Recently, it has been demonstrated, in older post-MI patients, that frailty (defined as a slow gait speed) and non‐participation to CR, were independent predictors of 1-year mortality and incident disability, and we know to what extent impairment in physical performance is a central domain of frailty and, hence, of further loss of physical function and incident disability [28, 29].
Indeed, it is well known that a decreased VO2peak, together with comorbidities and sedentariness, contribute to feed a vicious circle made of worsening cardiac disease and progressive loss of physical functioning, with a consequent high risk of incident BADL/IADL disability [12]. Therefore, it is not surprising that, in functionally frail individuals, an even small increase in VO2peak can produce a substantial reduction in all-cause and cardiovascular mortality [30]. However, though the individual response to CR is largely variable, exercise programs proved to be safe and to improve the functional capacity and reduce myocardial work to a similar extent in older and younger coronary patients [31]. The variability in CR beneficial effects has been highlighted by authors of the SAINTEX-CAD study, who demonstrated that as many as one-third of patients did not obtain a significant improvement in exercise capacity [32], despite high participation in the CR program. In that study, older age, elective PCI, higher baseline VO2peak, and oxygen uptake efficiency slope, as well as lower training intensity and baseline energy expenditure, but not the number of training sessions, were the predictors of non-response to training. In our study, the number of training sessions turned out to be a significant positive predictor of response to CR expressed in terms of a moderate or an optimal VO2peak increase from baseline to the end of CR. We hypothesize that this difference might be related to a remarkable age difference between the two study populations (middle-age patients in SAINTEX-CAD vs. very old participants in our study) and, most importantly, to a different duration of the CR program (12 vs. 4 weeks). Therefore, because of the high number (N=36) of training sessions in both physical exercise groups, a ceiling effect, above which a further increase in VO2peak cannot be obtained, might have occurred in SAINTEX study. Whether increasing the duration of training sessions of the CR program can improve the cardiopulmonary exercise capacity, as well as the optimal modalities to supervise the exercise capacity of patients after an ACS in the follow-up period, remains to be further assessed in older patients.
It is interesting to note that, in the present CR-AGE ACS study, neither the extension of coronary disease, nor the type of myocardial infarction (NSTEMI vs. STEMI), nor the completeness of myocardial revascularization, were predictors of aerobic capacity improvement. As a side note, in our population we observed a higher prevalence of STEMI, whereas NSTEMI/UA are usually more prevalent in older patients, probably because we selected patients treated in any case with PCI.
We must underline how we cannot debate about the predictive role of reduced ejection fraction and/or overt heart failure in our study population. The importance of physical activity or structured cardiac rehabilitation in the field of heart failure caused by ischemic or no ischemic diseases is clearly established in term of its effect on outcomes (33 REF-Cacciatore). The reasons of this lack is related to different reasons: first, in the CRAGE protocol [14] ejection fraction equal or less 35% was an exclusion criteria; consequently those patients with HFrEF could not be enrolled. Second, as reported in the method section we enrolled patients early from discharge after acute coronary syndrome. This fact limited greatly to refer us patients with history of heart failure or incident acute heart failure soon after an acute coronary syndrome treated with PCI, unless to enroll patients clinically unstable but, of course, not eligible at this time for cardiac rehabilitation program (34 JAMA. 2009;301:1439-1450).
Finally, an interesting finding regards the influence of baseline functional independency on the improvement of the exercise capacity at the end of CR. We found that even a mild-to-moderate decline in functional independency (defined as a loss of 1+ BADL or 2+ IADL) can negatively affect the probability to reach an increase ≥ 5% in VO2peak from baseline. Older patients often become sedentary after acute cardiac events, due to physical deconditioning after an even short hospitalization [35] and because of reactive depressive symptoms that negatively impact on functional recovery [36]. Such a sedentariness may lead to further global functional decline in the early post-acute clinical course [37]. In this scenario, a baseline comprehensive geriatric assessment may play a crucial role in precisely planning an individually tailored CR program in the elderly. This view is further supported by our finding that even a modest decrease of a substantially normal cognitive profile can negatively impact the maximally attainable cardiopulmonary fitness. Although this finding is slightly below the threshold of statistical significance, we believe that it is consistent with the general evidence of a close association of cognitive function with cardiorespiratory fitness [38].
Study limitations can be summarized as follows: The first study limitation is its observational nature. Second limitation is the absence of a control group even if the aim of the present study was not to compare the effect of CR vs usual care, but it was to identify the independent predictors of changes in physical performance in this real world and homogenous population of older patients recovering from an ACS; all treated with early invasive strategy and PCI. A third limitation is the relatively short duration of CR, as 4 weeks may be regarded as insufficient to maximize the increase in VO2peak, especially in older adults. However, this duration reflects the routine length of rehabilitation provided by the Italian national healthcare system and, therefore, our study provides information that are relevant in the perspective of real-world rehabilitation practice in Italy. Furthermore, the availability of only two measurements (at baseline and 4 weeks later) cannot exclude the influence of a regression to the mean effect, but the average improvement observed in VO2peak is close to that obtained in similarly old population enrolled in other studies [14]. Finally, a selection bias represented by the exclusion of individuals with more marked cognitive decline or disability and patients affected by any clinical phenotype of heart failure, might limit, together with the fact that CR-AGE ACS study represents a single-center experience, the generalizability of these findings to the broader spectrum of older adults routinely hospitalized for ACS with or without overt HF, also because the presence of some of these conditions generally produces a more conservative approach to ACS treatment strategy or induces toward a later referral to CR program.
Conclusions
Despite the aforementioned limitations, the CR-AGE ACS study demonstrated that a multidisciplinary, structured CR program started early after discharge in very old patients who underwent PCI for ACS, produces remarkable and clinically valuable improvements in exercise capacity in the majority of them. These results confirm that older adults with mild-to-moderate post-acute physical impairment are ideal candidates for CR program to promote their rapid functional recovery although in our study population were not included severe frail or comorbid older patients that obviously limits the widespread generalization of the finding. Our next aim will be to verify if the improvement in exercise capacity obtained during CR program is maintained in the follow-up period; because this confirmation undoubtedly will reinforce greatly the clinical message.
Change history
28 July 2022
Missing Open Access funding information has been added in the Funding Note.
References
Anderson L, Thompson DR, Oldridge N et al (2016) Exercise-based cardiac rehabilitation for coronary artery disease: cochrane systematic review and meta-analysis. J Am Coll Cardiol 67:1–12
Roffi M, Patrono C, Collet JP et al (2016) 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the european society of cardiology. Eur Heart J 37:267–315
Ibanez B, James S, Agewall S et al (2018) 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 39:119–177
Vilela EM, Ladeiras Lopes R et al (2020) Differential impact of a cardiac rehabilitation program on functional parameters in elderly versus non-elderly myocardial infarction survivors. Cardiology 145:98–105
Piepoli MF, Corra U, Benzer W et al (2010) Secondary prevention through cardiac rehabilitation: from knowledge to implementation. A position paper from the cardiac rehabilitation section of the European association of cardiovascular prevention and rehabilitation. Eur J Cardiovasc Prev Rehabil 17:1–17
Beatty AL, Bradley SM, Maynard C et al (2017) Referral to cardiac rehabilitation after percutaneous coronary intervention, coronary artery bypass surgery, and valve surgery: data from the clinical outcomes assessment program. Circ Cardiovasc Qual Outcomes 10:e003364
Grace SL, Gravely-Witte S, Brual J et al (2008) Contribution of patient and physician factors to cardiac rehabilitation referral: a prospective multilevel study. Nat Clin Pract Cardiovasc Med 5:653–662
Beatty AL, Li S, Thomas L et al (2014) Trends in referral to cardiac rehabilitation after myocardial infarction: data from the National cardiovascular data registry 2007 to 2012. J Am Coll Cardiol 63:2582–2583
Aragam KG, Dai D, Neely ML et al (2015) Gaps in referral to cardiac rehabilitation of patients undergoing percutaneous coronary intervention in the United States. J Am Coll Cardiol 65:2079–2088
Decourcelle V, Maréchaux S, Pinçon C et al (2013) Impact of functional decline on outcome in elderly patients with acute coronary syndromes. Am J Crit Care 22:e1–e11
Forman DE, Arena R, Boxer R et al (2017) prioritizing functional capacity as a principal end point for therapies oriented to older adults with cardiovascular disease: a scientific statement for healthcare professionals from the American heart association. Circulation 135:e894–e918
Arena R, Myers J, Williams MA et al (2007) Assessment of functional capacity in clinical and research settings: a scientific statement from the American heart association committee on exercise, rehabilitation, and prevention of the council on clinical cardiology and the council on cardiovascular nursing. Circulation 116:329–343
Pratesi A, Baldasseroni S, Burgisser C et al (2019) Long-term functional outcomes after cardiac rehabilitation in older patients. Data from the cardiac rehabilitation in advanced aGE: exercise training and active follow-up (CR-AGE EXTRA) randomized study. Eur J Prev Cardiol 26:1470–1478
Baldasseroni S, Pratesi A, Francini S et al (2016) Cardiac rehabilitation in very old adults: effect of baseline functional capacity on treatment effectiveness. J Am Geriatr Soc 64:1640–1645
Folstein MF, Folstein SE, McHugh PR (1975) ‘Mini-Mental State’. A practical method for grading the cognitive state of patients for the clinicians. J Psychiatr Res 12:189–198
Katz S, Ford AB, Moskowitz RW et al (1963) Studies of illness in the aged: the Index of ADL: a standardized measure of biological and psychosocial function. JAMA 185:914–919
Fletcher GF, Ades PA, Kligfield P et al (2013) Exercise standards for testing and training: a scientific statement from the American heart association. Circulation 128:873–934
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Sheikh JI, Yesavage JA (1986) Geriatric depression scale (GDS): recent evidence and development of a shorter version. Clin Gerontol 5:165–173
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Borg G (1998) Borg’s perceived exertion and pain scales. Human kinetics, Champaign
Busch JC, Lillou D, Wittig G et al (2012) Resistance and balance training improves functional capacity in very old participants attending cardiac rehabilitation after coronary bypass surgery. J Am Geriatr Soc 60:2270–2276
Pack QR, Mansour M, Barboza JS et al (2013) An early appointment to outpatient cardiac rehabilitation at hospital discharge improves attendance at orientation: a randomized, single-blind, controlled trial. Circulation 127:349–355
Bloomfield SA (1997) Changes in musculoskeletal structure and function with prolonged bed rest. Med Sci Sports Exerc 29:197–206
Aragam KG, Moscucci M, Smith DE et al (2011) Trends and disparities in referral to cardiac rehabilitation after percutaneous coronary intervention. Am Heart J 161:544.e2-551.e2
O’Neill D, Forman DE (2019) Never too old for cardiac rehabilitation. Clin Geriatr Med 35:407–421
Ritchey MD, Maresh S, McNeely J et al (2020) Tracking cardiac rehabilitation participation and completion among medicare beneficiaries to inform the efforts of a national initiative. Circ Cardiovasc Qual Outcomes 13:e005902
Flint K, Kennedy K, Arnold SV et al (2018) Slow gait speed and cardiac rehabilitation participation in older adults after acute myocardial infarction. J Am Heart Assoc 7:e008296
Afilalo J, Joshi A, Mancini R (2019) If you cannot measure frailty, you cannot improve it. JACC Heart Fail 7:303–305
Kodama S, Saito K, Tanaka S et al (2009) Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA 301:2024–2035
Ferrara N, Corbi G, Bosimini E et al (2006) Cardiac rehabilitation in the elderly: patient selection and outcomes. Am J Geriatr Cardiol 15:22–27
Witvrouwen I, Pattyn N, Gevaert AB et al (2019) Predictors of response to exercise training in patients with coronary artery disease—a subanalysis of the SAINTEX-CAD study. Eur J Prev Cardiol 26:1158–1163
Cacciatore F, Amarelli C, Ferrara N et al (2019) Protective effect of physical activity on mortality in older adults with advanced chronic heart failure: a prospective observational study. Eur J Prev Cardiol 26:481–488
O’Connor CM, Whellan DJ, Lee KL et al (2009) HF-ACTION investigators Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 301:1439–1450
Kortebein P, Ferrando A, Lombeida J et al (2007) Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA 297:1772–1774
Lichtman JH, Bigger JT Jr, Blumenthal JA et al (2008) Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American heart association prevention committee of the council on cardiovascular nursing, council on clinical cardiology, council on epidemiology and prevention, and interdisciplinary council on quality of care and outcomes research. Circulation 118:1768–1775
Afilalo J (2019) Evaluating and treating frailty in cardiac rehabilitation. Clin Geriatr Med 35:445–457
Farrell SW, Abramowitz AR, Willis BL et al (2018) The relationship between cardiorespiratory fitness and montreal cognitive assessment scores in older adults. Gerontology 64:440–445
Acknowledgements
The authors greatly appreciate and thank all cardiac rehabilitation staff for invaluable patient care: Weruska Mannelli (Physioterapist); Federica Santagiuliana (Dietitian); Adriana Bambi, Silvia Burchi, Maddalena Ciompi, Marzia Conforti, Damasco Donati, Rita Peruzzi, Francesca Valeri, Katia Zini (Nurses).
Funding
Open access funding provided by Università degli Studi di Firenze within the CRUI-CARE Agreement. The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
This statement is to certify that all authors have seen and approved the manuscript being submitted, have contributed significantly to the work, attest to the validity and legitimacy of the data and its interpretation, and agree to its submission to the Aging Clinical and Experimental Research. We attest that the article is the Authors’ original work, has not received prior publication and is not under consideration for publication elsewhere. On behalf of all Co-Authors, the corresponding Author shall bear full responsibility for the submission.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no competing interests to declare that are relevant to the content of this article. All authors declare no potential conflict of interest including any financial, personal or other relationships or be perceived to influence, their work. None of the authors have any commercial relationship with industries.
Ethical approval
The CR-AGE protocol has been approved by Local Ethic Committee and it complies with the rules of the declaration of Helsinki. The CR-AGE study is also registered at ClinicalTrial.gov with n°NCT00641134.
Informed consent
Written informed consent was given by each patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Baldasseroni, S., Silverii, M.V., Pratesi, A. et al. Cardiac Rehabilitation in Advanced aGE after PCI for acute coronary syndromes: predictors of exercise capacity improvement in the CR-AGE ACS study. Aging Clin Exp Res 34, 2195–2203 (2022). https://doi.org/10.1007/s40520-022-02130-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02130-y