Abstract
Background
Comorbidities have major implications for the care of people with dementia.
Aim
To investigate the patterns of comorbidities in dementia in the last five years of life and how these patterns differed between three cohorts.
Methods
The study included people who died at age 70 and above in 2001 (n = 13,717), 2007 (n = 34,750) and 2013 (n = 38,087) in Finland. ICD-10 morbidity data for a five-year period prior to death were extracted from national registers. Principal component analysis was employed to identify patterns for several morbidities. The associations of principal component scores with dementia were analysed using binary logistic regression. Linear regression was used to examine changes in the number of morbidities in patterns over time.
Results
The morbidity patterns identified in the last years of life were (1) cardiometabolic disorders, (2) neurological, (3) cerebrovascular diseases and (4) musculoskeletal, thyroid and psychiatric disorders. Among the patterns, neurological and musculoskeletal, thyroid and psychiatric disorders were associated with dementia. The number of diagnoses in the cerebrovascular pattern increased and those in the musculoskeletal, thyroid and psychiatric pattern decreased over time.
Discussion
Comorbidity patterns identified in this nationwide register study are largely in line with previous evidence. Time difference in these patterns provide crucial information for service planning.
Conclusions
Comorbidities in dementia in the last years of life occur in patterns and change over time. More systematic monitoring and updated clinical guidelines are needed for the care of comorbidities with dementia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Comorbidities among people with dementia is a rising concern for health care systems worldwide as the number of older adults continues to increase [1]. Research findings are contradictory: some studies report that people with dementia have a higher number of coexisting diseases [2, 3], some suggest that they are healthier [4], and some report similar levels of morbidity [5] as in people without dementia. The inconsistencies are likely to reflect the differences in studied populations and methods [5,6,7,8]. There is also a lack of evidence on how comorbidities in dementia change over time [9].
Other medical conditions in dementia might accelerate the decline of functional and cognitive abilities [10, 11]. Dementia is found to complicate the management of other illnesses [1, 12] and conversely, treatment of comorbid conditions may generate an opposite effect on the treatment of dementia due to improper drug combinations [4]. Furthermore, especially people living with advanced dementia may have difficulty communicating their health problems, resulting in hidden comorbidities, lack of treatment and poor health outcomes [7]. Therefore, dementia with coexisting diseases requires different treatment strategies. Multidisciplinary coordinated care has been recommended instead of a single disease approach [1].
A recent study reported that the incidence of dementia has declined by 13% in Europe [13] potentially explained by factors like improved living conditions, education, and more effective prevention and management of risk factors [14]. According to Alzheimer Europe report 2020, the prevalence of dementia has declined over the last decade (2008–2018), but the proportion of population having dementia is expected to double (1.57% in 2018 to 3% in 2050), because of the increase in ageing population, especially those above 85 years [15]. In Finland, the number of deaths from dementia has almost doubled in the last decade, and the country now has the highest age-adjusted dementia-related death rate in Europe [16]. Furthermore, as more people live in to very advanced age, the number of individuals with dementia is likely to grow [17, 18]. Increasing dementia is posing new requirements for care.
This study aims to identify the most common comorbidities and patterns of comorbidities in people with dementia in the last five years of life. Furthermore, it examines the differences between these patterns in 2001, 2007 and 2013. This information will help professionals redefine the necessary clinical guidelines [9] and develop nursing care on the continuum of services for better health outcomes and quality of life.
Methods
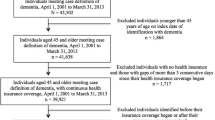
The study population included three cohorts of people in Finland who died at age 70 and above in 2001 (n = 13,717), 2007 (n = 34,750) and 2013 (n = 38,087). The first dataset included a random sample of 40% of the 2001 cohort and the two other datasets comprised all decedents aged 70 or over in the respective years. The data included information on date and age of death and gender.
ICD-10 morbidity data for a five-year period prior to death were extracted from national registers as described below. A person was considered to have the diagnosis if it was indicated in any of the three source registers, namely The Causes of Death Register (Statistics Finland), The Care Register for Health Care and The Care Register for Social Welfare (Finnish Institute for Health and Welfare). These exhaustive registers cover every individual living in Finland and their use of health care, and the principle of registers have remained the same across study cohorts. Information on direct, immediate and underlying causes and other morbidities leading to death were extracted from the death register. The dementia group was identified using ICD-10 codes F00 (dementia in Alzheimer’s disease), F01 (vascular dementia), F02 (dementia in other diseases), F03 (unspecified dementia) or G30 (Alzheimer’s disease). In addition to dementia, the other diagnoses included in our analyses were hypertension (I10–I16), coronary artery disease (CAD) (I20–I25), diabetes (E10–E14), stroke (I60–I69), Parkinson’s disease or other neurological diseases (G00–G99 excluding G30), atherosclerosis or peripheral arterial occlusive disease (I65, I66, I67.2, I70, I73.9), cardiac insufficiency (I50), asthma or chronic obstructive pulmonary disease (COPD) (J40–J47), cancer (C00–C97), hip fracture (S72), thyroid disorders (E01–E07), diseases of lipoprotein metabolism and other lipidemias (E78), psychotic or neurotic disorders (F20–F29, F40–F48), depression (F32, F33), insomnia (F51, G47), joint arthrosis (M15–M19), osteoporosis (M80–M82) and renal insufficiency or failure (N17–N19). The list of morbidities was based on conditions found to be the most prevalent in the older population [7] and conditions associated with dementia in the previous literature [2, 12].
This study is part of the ongoing project: the longevity revolution: implications for the need and cost of health and social care (COCTEL) [19].
Statistical analysis
The study participants’ characteristics were described as frequencies and percentages or means and standard deviations (SD). To determine the impact of dementia and time, differences between people with and without dementia and between the three cohorts were tested by independent samples t test for continuous variables and by Pearson’s Chi-squared test for categorical variables. A Mantel–Haenszel test was performed to investigate the trend in the proportion of people with and without dementia across the cohorts. We calculated the proportions of morbidities in the three cohorts of people with dementia, and then estimated odds ratios for each morbidity with cohort as the independent variable from binary logistic regression. Finally, we tested the linear trend of odds ratios for morbidities using the contrast command in Stata.
Principal component analysis (PCA) was used to identify morbidity patterns. PCA is a dimensionality reduction technique that was used to reduce the large number of diseases into a smaller number of components while retaining most of the relevant information in the large dataset. The number of components extracted depended on the eigenvalue (variances of the principal components) ≥ 1, scree plot (graphical plot of eigenvalues against component numbers) and clinically meaningful interpretable components. We proceeded with PCA as Bartlett’s test showed a significance of < 0.001. Component loadings > 0.3 were considered significant [20,21,22,23]. Chronic respiratory diseases had loadings > 0.3 in two components and negative loading in one component, and cancer was negatively loaded on two components and hence were excluded from PCA. Next, the associations of the principal component scores with dementia were examined by binary logistic regression analysis adjusted for age at death and gender. Finally, a linear regression model (adjusted for age at death and gender) with an interaction term between dementia and cohort was used to examine changes in the number of diseases in the morbidity patterns over time. As the number of diseases may have been affected by increasing age at death across the cohorts, we also run the analyses without age adjustment. Statistical analyses were performed using Stata 15 (College Station, TX, USA) and SPSS 25 (Armonk, NY, USA). We considered statistical significance at p < 0.05.
Results
Almost one-third (31.7%) of the study population (n = 86,554) had dementia at the time of death. The figures for 2001, 2007 and 2013 were 24.5%, 30.2% and 35.6%, respectively. In each cohort, the share of women and mean age at death were significantly higher in people with dementia than in people without dementia. In people with dementia, the age and gender standardised mean number of morbidities increased significantly between the first two cohorts and then decreased slightly in the most recent cohort, still remaining at a higher level than in the first cohort (3.52, 3.77 and 3.74), while in people without dementia that number increased steadily (2.84, 3.08 and 3.20) (Table 1).
Table 2 reports the comorbidities for people with dementia over time. In the most recent year, the most prevalent comorbidities were coronary artery disease (37.3%), hypertension (36.0%), cardiac insufficiency (24.3%), and stroke (22.5%). Stroke, hip fracture, atherosclerosis, psychotic or neurotic disorders and depression decreased significantly across time while hypertension, cardiac insufficiency, diabetes, cancer, lipoprotein disorders, renal insufficiency, osteoporosis, insomnia and thyroid disorders increased. No significant cohort differences were found for coronary artery disease, Parkinson’s disease, or joint arthrosis.
PCA revealed four morbidity patterns in the whole sample (Table 3). The first component, cardiometabolic disorders, had heavy loadings (factor loading > 0.4) on cardiac insufficiency, coronary artery disease, renal insufficiency, diabetes and atherosclerosis or peripheral arterial occlusive disease. The second component was named as neurological diseases, with heavy loadings on insomnia and Parkinson’s disease or other neurological diseases. The third component was cerebrovascular diseases due to heavy loadings on hypertension, diseases of lipoprotein metabolism and stroke. The last component, musculoskeletal, thyroid and psychiatric disorders, included osteoporosis, hip fracture, joint arthrosis, thyroid disorders, depression and psychotic or neurotic disorders.
Table 4 demonstrates the association between the principal component scores of the patterns identified and dementia (adjusted for age, gender and cohort). The odds of having dementia was higher for those whose principal scores for neurological diseases (ORadj 1.79, 95% confidence interval (CI) 1.65–1.93) and musculoskeletal, thyroid and psychiatric disorders (ORadj 1.78, 95% CI 1.64–1.92) were higher. Meanwhile, the odds of having dementia was lower for those whose principal scores for cardiometabolic disorders (ORadj 0.34, 95% CI 0.32–0.35) and cerebrovascular diseases (ORadj 0.71, 95% CI 0.67–0.74) were higher.
Figure 1 shows the observed means in the three cohorts and fitted trajectories for changes in the number of diseases in the morbidity patterns over time in people with dementia from the linear regression model. There was a significant increase in cerebrovascular diseases (p < 0.001) and a decrease in musculoskeletal, thyroid and psychiatric disorders (p < 0.001). The decreases in cardiometabolic disorders (p = 0.11) and neurological and lung-related diseases (p = 0.32) were not statistically significant. Cardiometabolic disorders was the only disease pattern that showed a different time trend depending on whether the changing age structure was taken into account. Without age adjustment, there was a slight increase in cardiometabolic diagnoses but that turned to decline when adjusted for age.
Discussion
We found mixed time trends for comorbidities in the last years of life of people with dementia: some increased, a few decreased and some were stable between the cohorts. The most frequent conditions in people with dementia were coronary artery disease followed by hypertension, cardiac insufficiency and stroke. Our findings are supported by previous research which has reported that hypertension [1, 2], cardiovascular diseases, stroke and diabetes are the most common diseases among people with dementia [12].
Changes in comorbid conditions over time
Trends in the chronic disease burden in the older population have been quite extensively explored [24, 25], but to our knowledge, there are no previous studies on how comorbidities in people with dementia change over time. Of the diagnoses, hypertension, cancer, renal insufficiency, osteoporosis, insomnia and lipoprotein disorders became more frequent in people with dementia. The increasing prevalence of hypertension may be due to lowered blood pressure cut-offs for diagnosis [26]. Diabetes has increased over time, which may explain the increasing occurrence of renal insufficiency in the sample. Among cardiovascular diseases, cardiac insufficiency increased while coronary artery diseases showed no change in people with dementia. An earlier Finnish study reported a decrease in cardiovascular diseases in working-age people due to a reduction in risk factors and a shift to older age due to better treatment and survival [27]. An increasing trend in the prevalence of comorbidities may partly be due to increasing life expectancy, changing diagnostic criteria, more active diagnosing of dementia and some of the comorbidities, and the availability of more effective drugs [25]. The prevalence of comorbidities varies with the type of dementia and increases with severity of cognitive impairment [2, 8].
Comorbidity patterns and their associations with dementia
A better understanding of conditions that coexist with dementia in specific patterns is crucial for care planning [11]. Using PCA, a novel way to summarise complex conditions, we were able to identify four morbidity patterns, two of which were associated with dementia. The coexistence of neurological pattern with dementia represents a clinically interpretable pattern and is supported by previous studies [28,29,30]. Insomnia is found to be associated with increased risk of dementia and is one of the most common symptoms in Parkinson’s disease [29], thus explaining the pattern.
Despite differences in methodological and statistical approaches, earlier studies have consistently identified cardiometabolic, mental health, musculoskeletal, and neuropsychiatric patterns in adults [6, 23]. Such patterns might stem from similar risk factors or common pathophysiological mechanisms [9]. The diseases in the fourth pattern we identified—musculoskeletal, thyroid and psychiatric disorders—are interrelated: it has been reported that people on medications for depression or psychosis, with adverse effects such as sedation and hypotension, are at greater risk for falls and fractures [31]. There are several reports of a significant association between depression and osteoporosis [32] and hypothyroidism and depression [33], lending support to the convergence thesis. The evidence suggests associations between dementia and depression [7], hip fracture [31], higher thyroid function [34] and osteoporosis [35]. These associations underline the need for early diagnosis and management of depression and osteoporosis as well as the importance of identifying the type of thyroid disorders associated with dementia. Our results are in line with existing reports on disease patterns coexisting with dementia in older adults, including anxiety, depression, somatoform disorders and pain, and neuropsychiatric disorders [2, 28]. The morbidity pattern showing the greatest increase over time was that of cerebrovascular diseases, a group not specifically associated with dementia. Among the patterns that were more frequent in dementia patients than in those without dementia, musculoskeletal, thyroid and psychiatric disorders showed a significant decline between the cohorts. The decrease in this pattern is attributable to the decrease in several diagnoses associated with this pattern, namely hip fracture, psychotic or neurotic disorders and depression, while osteoporosis and thyroid disorders increased.
This first nationwide study in Finland provides information on changes over time in comorbidity in dementia and introduces a novel approach to comorbidity research by employing PCA to detect concurrent diagnoses in dementia. It overcomes many limitations of earlier comorbidity studies, drawing its data from multiple national registers and using a comprehensive list of morbidities and disease patterns instead of any single disease [9]. The exhaustive registers contain information on every individual in Finland. Diagnosis of dementia (ICD10) is entered in the Care Register for Health Care or the Care Register for Social Welfare when a person with dementia is admitted to care, i.e., uses the service. In addition, the Causes of Death Register includes information on dementia diagnosis. These practices have not changed from 2001 to 2013, and we have no reason to suspect differences between the study years in this respect. It is important to note, however, that we can draw no inferences about causality between dementia and comorbidities and that the trends observed must be interpreted with caution as they largely depend on the population, clinical criteria used, hospital reporting, death registry data and health seeking patterns [5, 7]. People in the advanced stages of dementia may not be able to communicate their symptoms, which may lead to underestimation of several medical conditions. Furthermore, there may be differences in the associations of different subtypes of dementia, but our main concern here is with population health needs and care organisation rather than etiology. As the age structure and chronic conditions among old are approximately similar, we believe that largely our findings are applicable to Europe, especially Northern countries [36].
Our findings warrant the development of improved models of dementia care, both clinical and social, that anticipate the future scale of dementia and its comorbidities. New clinical guidelines are needed for coexisting diseases as most current guidelines are disease-specific [22], often leading to polypharmacy, drug interactions and iatrogenic events [3]. Coordination and communication between specialists and primary care providers may help to attain the best possible outcomes.
In conclusion, our study highlights the medical complexity associated with dementia, underscoring the importance of regular monitoring and an integrated treatment protocol with a multiple disease approach. This will help to improve the quality of life of people with dementia. Further research should focus on the mechanisms in the relationship between comorbidity patterns and dementia and its subtypes.
Data availability
The research group has received permission to use the register data from Statistics Finland and the National Institute for Health and Welfare. The register data are not owned by the research group. The data are confidential and not freely available.
References
Nelis SM, Wu Y-T, Matthews FE et al (2018) The impact of comorbidity on the quality of life of people with dementia: findings from the IDEAL study. Age Ageing. https://doi.org/10.1093/ageing/afy155
Poblador-Plou B, Calderón-Larrañaga A, Marta-Moreno J et al (2014) Comorbidity of dementia:a cross-sectional study of primary care older patients. BMC Psychiatry 14:84. https://doi.org/10.1186/1471-244X-14-84
Clague F, Mercer SW, McLean G, Reynish E, Guthrie B (2017) Comorbidity and polypharmacy in people with dementia: insights from a large, population-based cross-sectional analysis of primary care data. Age Ageing 46:33–39. https://doi.org/10.1093/ageing/afw176
Schubert CC, Boustani M, Callahan CM et al (2006) Comorbidity profile of dementia patients in primary care: are they sicker? J Am Geriatr Soc 54:104–109. https://doi.org/10.1111/j.1532-5415.2005.00543.x
Zekry D, Herrmann FR, Grandjean R et al (2008) Demented versus non-demented very old inpatients: the same comorbidities but poorer functional and nutritional status. Age Ageing 37:83–89. https://doi.org/10.1093/ageing/afm132
Prados-Torres A, Calderón-Larrañaga A, Hancco-Saavedra J, Poblador-Plou B, Van Den Akker M (2014) Multimorbidity patterns: a systematic review. J Clin Epidemiol 67:254–266. https://doi.org/10.1016/j.jclinepi.2013.09.021
Bauer K, Schwarzkopf L, Graessel E, Holle R (2014) A claims data-based comparison of comorbidity in individuals with and without dementia. BMC Geriatr 14:10. https://doi.org/10.1186/1471-2318-14-10
Doraiswamy PM, Leon J, CummingsJ L, Marin D, Neumann PJ (2002) Prevalence and impact of medical comorbidity in Alzheimer’s disease. J Gerontol Ser A 57:M173–M177. https://doi.org/10.1093/gerona/57.3.M173
Calderón-Larrañaga A, Vetrano DL, Onder G et al (2017) Assessing and measuring chronic multimorbidity in the older population: a proposal for its operationalization. J Gerontol A Biol Sci Med Sci 72:1417–1423. https://doi.org/10.1093/gerona/glw233
Callahan CM, Schubert CC (2014) The complexities of comorbidity in dementia. Nat Rev Neurol 10:184–186. https://doi.org/10.1038/nrneurol.2014.46
Subramaniam H (2019) Co-morbidities in dementia: time to focus more on assessing and managing co-morbidities. Age Ageing 48:314–315. https://doi.org/10.1093/ageing/afz007
Vogelgsang J, Wolff-Menzler C, Kis B, Abdel-Hamid M, Wiltfang J, Hessmann P (2018) Cardiovascular and metabolic comorbidities in patients with Alzheimer’s disease and vascular dementia compared to a psychiatric control cohort. Psychogeriatrics 18:393–401. https://doi.org/10.1111/psyg.12338
Wolters FJ, Chibnik LB, Waziry R, Anderson R, Berr C, Beiser A et al (2020) Twenty-seven-year time trends in dementia incidence in Europe and the United States: the Alzheimer Cohorts Consortium. Neurology 95:e519–e531. https://doi.org/10.1212/WNL.0000000000010022
Wu Y-T, Fratiglioni L, Matthews FE et al (2016) Dementia in western Europe: epidemiological evidence and implications for policy making. Lancet Neurol 15:116–124. https://doi.org/10.1016/S1474-4422(15)00092-7
Alzheimer Europe (2020) Publications: Alzheimer Europe Reports. Dementia as a European Priority—a policy overview. https://www.alzheimer-europe.org/Publications/Alzheimer-Europe-Reports. Accessed 06 Feb 2021
Official Statistics of Finland (OSF) (2017) Causes of death [e-publication]. ISSN=1799–5078. Every fifth person aged over 65 died of dementia and Alzheimer’s disease. Statistics Finland, Helsinki [referred: 6.5.2019]. http://www.stat.fi/til/ksyyt/2017/ksyyt_2017_2018-12-17_kat_003_en.html. Accessed 05 Feb 2020
Pierce AL, Kawas CH (2017) Dementia in the oldest old: beyond Alzheimer disease. PLoS Med. https://doi.org/10.1371/journal.pmed.1002263
Bullain SS, Corrada MM (2013) Dementia in the oldest old. Continuum (Minneap Minn) 19:457–469. https://doi.org/10.1212/01.CON.0000429172.27815.3f
Aaltonen MS, Forma LP, Pulkki JM, Raitanen JA, Rissanen P, Jylhä MK (2019) The joint impact of age at death and dementia on long-term care use in the last years of life: changes from 1996 to 2013 in Finland. Gerontol Geriatr Med 5:2333721419870629. https://doi.org/10.1177/2333721419870629
Islam MM, Valderas JM, Yen L, Dawda P, Jowsey T, McRae IS (2014) Multimorbidity and comorbidity of chronic diseases among the senior Australians: prevalence and patterns. PLoS One 9:e83783. https://doi.org/10.1371/journal.pone.0083783
Mjørud M, Kirkevold M, Røsvik J, Engedal K (2014) Principal component analysis of the Norwegian version of the quality of life in late-stage dementia scale. Dement Geriatr Cogn Disord 37:265–275. https://doi.org/10.1159/000356497
Wang YP, Nunes BP, Coêlho BM et al (2019) Multilevel analysis of the patterns of physical-mental multimorbidity in general population of São Paulo metropolitan area, Brazil. Sci Rep 9:2390. https://doi.org/10.1038/s41598-019-39326-8
Mino-León D, Reyes-Morales H, Doubova SV, Pérez-Cuevas R, Giraldo-Rodríguez L, Agudelo-Botero M (2017) Multimorbidity patterns in older adults: an approach to the complex interrelationships among chronic diseases. Arch Med Res 48:121–127. https://doi.org/10.1016/j.arcmed.2017.03.001
Karppinen H, Pitkälä KH, Kautiainen H et al (2017) Changes in disability, self-rated health, comorbidities and psychological wellbeing in community-dwelling 75–95-year-old cohorts over two decades in Helsinki. Scand J Prim Health Care 35:279–285. https://doi.org/10.1080/02813432.2017.1358855
Meinow B, Kåreholt I, Thorslund M, Parker MG (2015) Complex health problems among the oldest old in Sweden: increased prevalence rates between 1992 and 2002 and stable rates thereafter. Eur J Ageing 12:285–297. https://doi.org/10.1007/s10433-015-0351-2
James PA, Oparil S, Carter BL et al (2014) Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth Joint National Committee (JNC 8). JAMA 311:507–520. https://doi.org/10.1001/jama.2013.284427
Kattainen A, Salomaa V, Härkänen T et al (2006) Coronary heart disease: from a disease of middle-aged men in the late 1970s to a disease of elderly women in the 2000s. Eur Heart J 27:296–301. https://doi.org/10.1093/eurheartj/ehi630
Schäfer I, von Leitner E-C, Schön G et al (2010) Multimorbidity patterns in the elderly: a new approach of disease clustering identifies complex interrelations between chronic conditions. PLoS One. https://doi.org/10.1371/journal.pone.0015941
de Almondes KM, Costa MV, Malloy-Diniz LF, Diniz BS (2016) Insomnia and risk of dementia in older adults: systematic review and meta-analysis. J Psychiatr Res 77:109–115. https://doi.org/10.1016/j.jpsychires.2016.02.021
Aarsland D, Brønnick K, Larsen JP, Tysnes OB, Alves G, Norwegian ParkWest Study Group (2009) Cognitive impairment in incident, untreated Parkinson disease: the Norwegian Park West study. Neurology 72:1121–1126. https://doi.org/10.1212/01.wnl.0000338632.00552.cb
Wang H-K, Hung C-M, Lin S-H et al (2014) Increased risk of hip fractures in patients with dementia: a nationwide population-based study. BMC Neurol 14:175. https://doi.org/10.1186/s12883-014-0175-2
Robbins J, Hirsch C, Whitmer R, Cauley J, Harris T (2001) The association of bone mineral density and depression in an older population. J Am Geriatr Soc 49:732–736
Fugger G, Dold M, Bartova L et al (2018) Comorbid thyroid disease in patients with major depressive disorder—results from the European Group for the Study of Resistant Depression (GSRD). Eur Neuropsychopharmacol 28:752–760. https://doi.org/10.1016/j.euroneuro.2018.03.011
Chaker L, Cappola AR, Mooijaart SP, Peeters RP (2018) Clinical aspects of thyroid function during ageing. Lancet Diabetes Endocrinol 6:733–742. https://doi.org/10.1016/S2213-8587(18)30028-7
Kostev K, Hadji P, Jacob L (2018) Impact of osteoporosis on the risk of dementia in almost 60,000 patients followed in general practices in Germany. J Alzheimer’s Dis 65:401–407. https://doi.org/10.3233/JAD-180569
European Commission (2020) Statistical office of the European Union. Ageing Europe: looking at the lives of older people in the EU : 2020 edition. Publications office. https://data.europa.eu/doi/https://doi.org/10.2785/628105. Accessed 23 Mar 2021
Acknowledgements
This work was conducted as part of a research project on “The longevity revolution: Implications for the need and cost of health and social care” (COCTEL). COCTEL is one of the research projects underway at the Center of Excellence in Research on Ageing and Care.
Funding
The work was supported by The Academy of Finland [project no 287372] and funding to the Academy of Finland Centre of Excellence in Research on Ageing and Care [Grant Number 312311] to MJ.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethics approval
Approval obtained from The Ethics Committee of Pirkanmaa Hospital District (R09089).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vargese, S.S., Halonen, P., Raitanen, J. et al. Comorbidities in dementia during the last years of life: a register study of patterns and time differences in Finland. Aging Clin Exp Res 33, 3285–3292 (2021). https://doi.org/10.1007/s40520-021-01867-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-021-01867-2