Abstract
Background
At least one-third of hip fracture patients have some degree of impaired cognitive status, which may complicate their postoperative rehabilitation.
Aim
We aimed to describe the outcome for elderly patients with cognitive dysfunction operated with hemiarthroplasty (HA) for a femoral neck fracture and to study the impact postoperative geriatric rehabilitation has on functional outcome up to 1 year after surgery.
Methods
98 patients with a displaced femoral neck fracture with a mean age of 86 years were included and followed up to 1 year. The outcomes were hip-related complications and reoperations, the capacity to return to previous walking ability, health-related quality of life, hip function and mortality.
Results
The prevalence of hip complications leading to a major reoperation was 6% and the 1-year mortality rate was 31%. The lack of geriatric rehabilitation was correlated with poorer outcomes overall and those who receive geriatric rehabilitation were less likely to be confined to a wheelchair or bedridden at the 1-year follow-up.
Conclusions
Hemiarthroplasty is an acceptable option for elderly patients with a displaced femoral neck fracture and cognitive dysfunction. A lack of structured rehabilitation is associated with a significant deterioration in walking ability despite a well-functioning hip. However, the causality of this could be due to selection bias of healthier patients being sent to geriatric rehabilitation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In lucid, elderly patients, with a displaced femoral neck fracture (FNF), primary hip arthroplasty provides better hip function and significantly fewer reoperations compared to internal fixation [1,2,3]. However, the optimal surgical procedure for FNF in elderly patients with cognitive dysfunction remain controversial [2, 4, 5].
The prevalence of cognitive impairment among hip-fracture patients has been reported to be as high as 55% [6, 7]. Patients with cognitive dysfunction have a high mortality rate as well as a high rate of both general and fracture-related complications [8,9,10,11]. This subgroup of patients is often excluded from participation in clinical trials, and therefore, there is little knowledge concerning the risk factors and prognosis in this group of patients [12]. In randomized controlled trials (RCTs) comparing surgical treatment options for patients with cognitive dysfunction, the inability for this patient group to give informed consent, and thereby the practical inclusion rate, have severely limited both the number of included patients and the external validity of these trials. Previous studies comparing hemiarthroplasty (HA) and internal fixation, [13] for patients with cognitive dysfunction have thus shown contradictory results [2, 4, 5] with high reoperation rates regardless of surgical treatment. There is also a lack of evidence regarding the effect of postoperative rehabilitation in patients with cognitive dysfunction.
In this study, we aimed to describe the outcome for elderly patients with cognitive dysfunction operated with HA for a displaced (garden 3 and 4) [14, 15] FNF and to study the impact postoperative rehabilitation has on functional outcome.
Methods
Study design and setting
This single-centre, prospective, observational cohort study was conducted between September 2009 and March 2016 at the Orthopaedic Department at Danderyd Hospital in Stockholm, Sweden. The study adhered to the STROBE (Strengthening The Reporting of Observational Studies in Epidemiology) guidelines [16].
Ethical statement
The study was approved by the ethics committee of the Karolinska Intitutet and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. All persons gave their informed consent prior to their inclusion in the study. For Patients with severe cognitive dysfunction their relative gave informed consent as approved by the ethical committee.
Study subjects and eligibility criteria
All patients with a displaced FNF who were admitted to the hospital during the inclusion period were screened for participation in the study. The inclusion criteria were patients ≥ 65 years old with an acute displaced FNF who were independent walkers, with or without walking aids, with cognitive dysfunction, defined as a known diagnosis of dementia and/or defined by a Short Portable Mental Status Questionnaire (SPMSQ) score of 0–7 indicating cognitive dysfunction. Exclusion criteria were pathological fractures, osteoarthritis, rheumatoid arthritis, previous hip disorders and patients deemed unsuitable for participation. Informed consent was given by the patients or relatives.
Surgery and postoperative rehabilitation
The same surgical teams at our hospital were used for the surgeries and the patients were operated by orthopaedic general trauma surgeons. A direct lateral approach was used. A tapered, cemented stem with a unipolar head (CPT stem, Zimmer, Warsaw, Indiana, USA) was used. The patients were encouraged to immediate weight bearing and there were no restrictions applied for range of motion.
The patients were discharged for rehabilitation at a specialized geriatric ward or returned to their home or nursing home. The allocation to the type of rehabilitation was not formally randomized but was rather dependent on the present occupancy at the geriatric unit, i.e., if there currently were beds available. The rehabilitation in the geriatric ward was individually adapted to the degree of cognitive dysfunction with the goal of restoring walking ability before discharge. The usual stay at the geriatric ward was 10 days before discharge to their nursing home. For those patients who were discharged after surgery directly to their nursing home, the rehabilitation varied depending on the availability of physiotherapy and whether the staff had sufficient time to help the patient implement the training programme. All nursing homes did not have a defined rehabilitation programme for patients with displaced femoral neck fractures.
Variables
Outcomes
Main outcomes were the prevalence of all hip-related complications and reoperations. Other outcomes included the ability to return to previous walking status, mortality, health-related quality of life (HRQoL), hip function, pain numeric rating scale (PNRS) and adverse events during the study period. The unique Swedish civic registration number for all patients was used to verify complications in the Swedish Hip Arthroplasty Register (SHAR) and mortality in the Swedish Death Register. HRQoL was assessed with a generic instrument, the health section of the EuroQol (European Quality of life) 5 dimensions (EQ-5D) score. Hip function and walking ability were evaluated with the modified Harris hip score (HHS) [17,18,19,20]. To assess the status of the activities of daily living, the ADL index according to Katz [21] was used. Pain in the involved hip was measured using the PNRS. We recorded all general adverse events.
Exposure and confounders
The cohort was divided into two groups, those who were allocated to geriatric rehabilitation after surgery, and those who were not (control group). Allocation was performed on availability, i.e., a formal randomization was not done. The availability was determined by the number of beds currently available at the geriatric ward.
Follow-up and data collection
Data were collected at the time of study inclusion, at the end of hospital stay and by visits to research nurses at 3 and 12 months after surgery. If the patient was unable to attend a follow-up visit, the family, caregiver or patients themselves were interviewed by telephone. All study data were collected and managed in Research Electronic Data Capture (REDCap) at Karolinska Institutet.
Statistical analysis
Fisher’s exact tests were used to analyse correlations between ordinal data, and Student’s t tests were used to analyse scale variables. A binary logistic regression was used for evaluating the risk of being unable to walk at the 1-year follow-up. The factors used in the model were the exposure variable (geriatric rehabilitation after surgery [yes/no]), age, sex and pre-fracture walking ability and living condition. The data are presented as mean differences and odds ratios (ORs) and the uncertainty estimation with 95% confidence intervals (CIs). A p value < 0.05 was considered statistically significant. Statistical analysis was performed using SPSS Statistics software version 22.0.
Source of funding
The study was funded by grants from the regional agreement on medical training and clinical research (ALF) and from Sven Noréns foundation.
Results
Patient flow and descriptive data
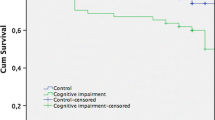
A total of 214 patients were screened during the inclusion period, and of these patients, 98 were recruited to participate in the study, 60 in the control group and 38 in the geriatric rehabilitation group (Fig. 1). The baseline demographics of the groups were similar but a higher proportion of the control group were admitted from nursing homes (Table 1). The overall mortality rate was 31% (30/98) with the control group having a slightly higher mortality rate at 1 years (36% versus 21%) but this difference did not reach statistical significance (p = 0.102, Fisher’s exact test).
Outcome data
Hip complications and reoperations
During the study period, eight patients (8%) suffered at least one hip-related complication, 5 (8%) in the control group and 3 (8%) in the geriatric rehabilitation group (Table 2). Two patients in the control group with recurrent dislocations were treated twice with closed reduction before revision surgery to a total hip arthroplasty with a dual-mobility cup.
Three periprosthetic fractures occurred in patients who had received a tapered CPT stem, two in the control group and one in the geriatric rehabilitation group. All were treated with open reduction and internal fixation. One patient in the geriatric rehabilitation group suffered a periprosthetic joint infection that healed after debridement and antibiotics for 3 months.
Walking ability
One year after surgery, 19% (19/61) of the surviving patients were either bedridden or wheelchair bound. The capacity to return to preoperative walking ability was diminished over the study duration; only 51% of the patients in both groups returned to their previous walking ability. The geriatric rehabilitation group had a statistically significant lower risk of being confined to a wheelchair or bedridden at the 1-year follow-up (odds ratio: 0.25; 95% CI 0.08–0.82; Table 3).
Functional outcome
The functional outcome scores were similar in both groups at baseline (Table 4). The mean HRQoL declined from baseline in the control group but increased slightly in the geriatric rehabilitation group with a clinically and statistically significant difference between the groups at 1 year (mean difference 0.30, 95% CI 0.07–0.15) (Fig. 2). Hip function as measured with HHS declined in the control group and remained unchanged in the geriatric rehabilitation group compared to baseline at 1 year (mean difference 13, 95% CI 4–21(Fig. 2). The pain scores were relatively unchanged during the study period and we found no statistically significant difference between the groups at any of the follow-ups (Table 4). The initial radiological classification of the fracture (garden 3 or 4) did not affect outcome.
Line graph illustrating the mean values (and 95% confidence intervals) of health-related quality of life (HRQoL), hip function and pain scores during the study. Solid lines represent the control group and dotted lines represent the geriatric rehabilitation group. EQ-5D European Quality of life five dimensions, HHS Harris hip score
Discussion
In this prospective observational study of elderly patients with cognitive dysfunction treated with cemented HA for a displaced FNF, we found an 8% prevalence of hip-related complications up to 1 year after surgery. We also found that patients who received geriatric rehabilitation despite their cognitive dysfunction were less likely to be confined to a wheelchair or to be bedridden than those who did not. Geriatric rehabilitation was also correlated with a better hip function and health-related quality of life up to 1 year after surgery.
There is a persistent controversy regarding the use of HA in elderly patients with dementia or cognitive dysfunction [2, 4, 5, 22]. In the hip-fracture population, mortality is high [23], and patients with hip fractures and a SPMSQ score below seven points have a twofold increased mortality rate during the first 2 years after surgery compared to that of those with a hip fracture and a SPMSQ score of 7 or higher [7]. The 1-year mortality in our study was 31% and that is similar to that which was reported by others [2, 4, 22].
The prevalence of hip-related complications and major reoperations was doubled in comparison to the prevalence reported by Hedbeck et al. [5] and less than that reported by Blomfeldt et al. [2]. The differences could be explained by the limited number of patients included in Hedbeck's study and the use of an outdated implant in Blomfeldt’s study. In our study, the main reason for reoperation was the occurrence of periprosthetic fractures.
The mean HRQoL and hip function in our study was better at 1 year in the geriatric rehabilitation group compared to controls. The overall hip scores and EQ-5D scores are similar to those reported from other cohorts [22, 24,25,26].
In the present study, we found a high prevalence (19%) of being unable to walk which is in line with the findings by Mukka et al. [22]. In addition, despite the fact that all participants in the study were walkers prior to surgery, only 51% of the patients were able to return to their previous walking ability. These results conform with the study by Rogmark et al. [6]. The high incidence of deterioration in walking ability among patients with cognitive dysfunction reflects the natural process of dementia and cognitive impairment and the difficulty for these patients to understand and follow rehabilitation regimes. Another explanation could also be the lack of rehabilitation resources for this patient group. Most patients with dementia or cognitive dysfunction live in nursing homes and are often discharged early from the hospital without receiving adequate rehabilitation.
The ultimate goal of rehabilitation is to return the patient to pre-fracture mobility and to avoid wheelchair dependence [27]. However, due to the inherent characteristics of the elderly hip-fracture population with often pre-existing comorbid conditions, rehabilitation can be difficult. The presence of cognitive impairment can alter their understanding of the need for rehabilitation, especially when it is painful [28]. Dementia can also increase the risk of falling by negatively impacting the individual’s ability to recognize and negotiate hazards, contributing to impaired body awareness and judgement [29].
Patients with dementia are at risk of being excluded from rehabilitation because of their perceived limited capacity for adherence and mobility. In contradiction to these assumptions, this study has shown that patients with cognitive dysfunction can benefit from participation in rehabilitation programmes and can regain their pre-fracture function after rehabilitation, which is in accordance with the findings from other studies [30,31,32,33].
Strengths and limitations
One of the main strengths of our study is its uniqueness, as it focuses on the patient outcome in cognitively impaired patients who have a displaced femoral neck fracture. Another strength is the large number of patients included in the study compared to that in previous studies. Additionally, all patients were monitored according to a strict protocol with regular follow-ups and validated outcome scores.
The short follow-up time could be seen as a limitation, but in this patient group, the short-term mortality rate is high, and therefore, it is important to present the 1-year results. The use of a proxy, i.e., relatives or significant others, to report a patient’s condition is a limitation, but it is the only possible method that can be used, and the method is well documented [34, 35]. Our allocation to geriatric rehabilitation can have, although unintentionally, introduced a selection bias where healthier/more fit patients were selected to geriatric rehabilitation. Although this is not reflected in the two groups baseline data and that we have adjusted for this in our statistically model, we still advise caution when interpreting our results as these can be the results of selection bias. In addition, we had no data on the type of rehabilitation, if any, that the nursing homes providing.
Conclusion
Cemented hemiarthroplasty with a direct lateral approach is a good option for elderly patients with a displaced (garden 3 and 4) femoral neck fracture and cognitive dysfunction. The lack of structured rehabilitation after surgery is associated with a significant deterioration in walking ability, regardless of a well-functioning prosthetic joint. However, the causality of this could be due to selection bias of healthier patients being sent to geriatric rehabilitation.
References
Chammout GK, Mukka SS, Carlsson T et al (2012) Total hip replacement versus open reduction and internal fixation of displaced femoral neck fractures: a randomized long-term follow-up study. J Bone Jt Surg. https://doi.org/10.2106/JBJS.K.01615
Blomfeldt R, Tornkvist H, Ponzer S et al (2005) Comparison of internal fixation with total hip replacement for displaced femoral neck fractures. Randomized, controlled trial performed at four years. J Bone Jt Surg Am 87:1680–1688
Gjertsen JE, Vinje T, Engesaeter LB et al (2010) Internal screw fixation compared with bipolar hemiarthroplasty for treatment of displaced femoral neck fractures in elderly patients. J Bone Jt Surg Am 92:619–628. https://doi.org/10.2106/JBJS.H.01750
van Dortmont LM, Douw CM, van Breukelen AM et al (2000) Cannulated screws versus hemiarthroplasty for displaced intracapsular femoral neck fractures in demented patients. Ann Chir Gynaecol 89:132–137
Hedbeck CJ, Inngul C, Blomfeldt R et al (2013) Internal fixation versus cemented hemiarthroplasty for displaced femoral neck fractures in patients with severe cognitive dysfunction: a randomized controlled trial. J Orthop Trauma 27:690–695. https://doi.org/10.1097/BOT.0b013e318291f544
Rogmark C, Carlsson A, Johnell O et al (2002) Primary hemiarthroplasty in old patients with displaced femoral neck fracture: a 1-year follow-up of 103 patients aged 80 years or more. Acta Orthop Scand 73:605–610. https://doi.org/10.1080/000164702321039534
Holmes J, House A (2000) Psychiatric illness predicts poor outcome after surgery for hip fracture: a prospective cohort study. Psychol Med 30:921–929
Samuelsson B, Hedstrom MI, Ponzer S et al (2009) Gender differences and cognitive aspects on functional outcome after hip fracture—a 2 years' follow-up of 2134 patients. Age Ageing 38:686–692. https://doi.org/10.1093/ageing/afp169
Stromberg L, Lindgren U, Nordin C et al (1997) The appearance and disappearance of cognitive impairment in elderly patients during treatment for hip fracture. Scand J Caring Sci 11:167–175
Johansson T, Jacobsson SA, Ivarsson I et al (2000) Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures: a prospective randomized study of 100 hips. Acta Orthop Scand 71:597–602
Marottoli RA, Berkman LF, Leo-Summers L et al (1994) Predictors of mortality and institutionalization after hip fracture: the New Haven EPESE cohort. Established populations for epidemiologic studies of the elderly. Am J Public Health 84:1807–1812
Soderqvist A, Ekstrom W, Ponzer S et al (2009) Prediction of mortality in elderly patients with hip fractures: a two-year prospective study of 1944 patients. Gerontology 55:496–504. https://doi.org/10.1159/000230587
Mundi S, Chaudhry H, Bhandari M (2014) Systematic review on the inclusion of patients with cognitive impairment in hip fracture trials: a missed opportunity? Can J Surg 57:E141–145
Biz C, Tagliapietra J, Zonta F et al (2020) Predictors of early failure of the cannulated screw system in patients, 65 years and older, with non-displaced femoral neck fractures. Aging Clin Exp Res 32:505–513. https://doi.org/10.1007/s40520-019-01394-1
Garden R (1961) Low-angle fixation in fractures of the femoral neck. J Bone Jt Surg Br 43:647–663
von Elm E, Altman DG, Egger M et al (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg (London, England) 12:1495–1499. https://doi.org/10.1016/j.ijsu.2014.07.013
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Jt Surg Am 51:737–755
Frihagen F, Grotle M, Madsen JE et al (2008) Outcome after femoral neck fractures: a comparison of Harris Hip Score, Eq-5d and Barthel Index. Injury 39:1147–1156. https://doi.org/10.1016/j.injury.2008.03.027
Soderman P, Malchau H (2001) Is the Harris hip score system useful to study the outcome of total hip replacement? Clin Orthop Relat Res 384:189–197
Mahomed NN, Arndt DC, McGrory BJ et al (2001) The Harris hip score: comparison of patient self-report with surgeon assessment. J Arthroplasty 16:575–580
Katz S, Ford AB, Moskowitz RW et al (1963) Studies of illness in the aged. The index of Adl: a standardized measure of biological and psychosocial function. JAMA 185:914–919
Mukka S, Knutsson B, Krupic F et al (2017) The influence of cognitive status on outcome and walking ability after hemiarthroplasty for femoral neck fracture: a prospective cohort study. Eur J Orthop Surg Traumatol 27:653–658. https://doi.org/10.1007/s00590-016-1873-9
Valizadeh M, Mazloomzadeh S, Golmohammadi S et al (2012) Mortality after low trauma hip fracture: a prospective cohort study. BMC Musculoskelet Disord 13:143. https://doi.org/10.1186/1471-2474-13-143
Parsons N, Griffin XL, Achten J et al (2014) Outcome assessment after hip fracture: is EQ-5D the answer? Bone Jt Res 3:69–75. https://doi.org/10.1302/2046-3758.33.2000250
Griffin XL, Parsons N, Achten J et al (2015) Recovery of health-related quality of life in a United Kingdom hip fracture population. The Warwick Hip Trauma Evaluation—a prospective cohort study. Bone Jt J 97:372–382. https://doi.org/10.1302/0301-620X.97B3.35738
Soderqvist A, Miedel R, Ponzer S et al (2006) The influence of cognitive function on outcome after a hip fracture. J Bone Jt Surg Am 88:2115–2123
Mitchell R, Harvey L, Brodaty H et al (2016) Hip fracture and the influence of dementia on health outcomes and access to hospital-based rehabilitation for older individuals. Disabil Rehabil 38:2286–2295. https://doi.org/10.3109/09638288.2015.1123306
Gill N, Hammond S, Cross J et al (2017) Optimising care for patients with cognitive impairment and dementia following hip fracture. Z Gerontol Geriatr 50:39–43. https://doi.org/10.1007/s00391-017-1224-4
McGilton K, Wells J, Davis A et al (2007) Rehabilitating patients with dementia who have had a hip fracture. Top Geriatr Rehabil 23:174–182. https://doi.org/10.1097/01.tgr.0000270186.36521.85
Huusko TM, Karppi P, Avikainen V et al (2000) Randomised, clinically controlled trial of intensive geriatric rehabilitation in patients with hip fracture: subgroup analysis of patients with dementia. BMJ 321:1107–1111
Beloosesky Y, Grinblat J, Epelboym B et al (2002) Functional gain of hip fracture patients in different cognitive and functional groups. Clin Rehabil 16:321–328. https://doi.org/10.1191/0269215502cr497oa
Rolland Y, Pillard F, Lauwers-Cances V et al (2004) Rehabilitation outcome of elderly patients with hip fracture and cognitive impairment. Disabil Rehabil 26:425–431. https://doi.org/10.1080/09638280410001663148
Al-Ani AN, Flodin L, Soderqvist A et al (2010) Does rehabilitation matter in patients with femoral neck fracture and cognitive impairment? A prospective study of 246 patients. Arch Phys Med Rehabil 91:51–57. https://doi.org/10.1016/j.apmr.2009.09.005
Coucill W, Bryan S, Bentham P et al (2001) EQ-5D in patients with dementia: an investigation of inter-rater agreement. Med Care 39:760–771
Selai C (2001) Assessing quality of life in dementia. Med Care 39:753–755
Acknowledgements
Open access funding provided by Karolinska Institute. We gratefully acknowledge the support from the staff at Danderyd hospital.
Funding
The study was funded by grants from the regional agreement on medical training and clinical research (ALF) and from Sven Noréns foundation.
Author information
Authors and Affiliations
Contributions
GC and OS initiated the study, designed the study, followed-up patients and wrote the manuscript. PKP followed-up patients and wrote the manuscript. CJH, HB, AS and SM initiated the study, designed the study and wrote the manuscript. All authors have given final approval of the version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
All authors report no conflict of interest.
Ethical approval
The study was approved by the ethics committee of the Karolinska Intitutet and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Informed consent
All persons gave their informed consent prior to their inclusion in the study. For Patients with severe cognitive dysfunction their relatives gave informed consent as approved by the ethical committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chammout, G., Kelly-Pettersson, P., Hedbeck, CJ. et al. Primary hemiarthroplasty for the elderly patient with cognitive dysfunction and a displaced femoral neck fracture: a prospective, observational cohort study. Aging Clin Exp Res 33, 1275–1283 (2021). https://doi.org/10.1007/s40520-020-01651-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01651-8