Abstract
Background
Aging is associated with declines in muscle mass, strength and quality, leading to physical impairments. An even protein distribution in daily meals has recently been proposed along with adequate total protein intake as important modulators of muscle mass. In addition, due to its short duration, high-intensity interval training (HIIT) has been highlighted as a promising intervention to prevent physical deterioration. However, the interaction between daily protein intake distribution and HIIT intervention in elderlies remain unknown.
Objective
To investigate muscle adaptation following HIIT in older adults according to daily protein intake distribution.
Methods
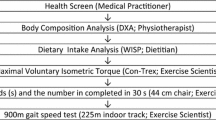
Thirty sedentary obese subjects who completed a 12-week elliptical HIIT program were matched [criteria: age (± 2 years), sex, BMI (± 2 kg/m2)] and divided a posteriori into 2 groups according to the amount of protein ingested at each meal: < 20 g in at least one meal (P20−, n = 15, 66.8 ± 3.7 years) and ≥ 20 g in each meal (P20+, n = 15, 68.1 ± 4.1 years). Body composition, functional capacity, muscle strength, muscle power, physical activity level, and nutritional intakes were measured pre- and post-intervention. A two way repeated ANOVA was used to determine the effect of the intervention (HIIT) and protein distribution (P20− vs P20+, p < 0.05).
Results
No difference was observed at baseline between groups. Following the HIIT intervention, we observed a significant decrease in waist and hip circumferences and improvements in functional capacities in both P20− and P20 + group (p < 0.05). However, no protein distribution effect was observed.
Conclusion
A 12-week HIIT program is achievable and efficient to improve functional capacities as well as body composition in obese older adults. However, consuming at least 20 g of proteins in every meal does not further enhance muscle performance in response to a 12-week HIIT intervention.

Similar content being viewed by others
References
Phillips SM, Chevalier S, Leidy HJ (2016) Protein “requirements” beyond the RDA: implications for optimizing health. Appl Physiol Nutr Metab 41:565–572. https://doi.org/10.1139/apnm-2015-0550
Janssen I (2010) Evolution of sarcopenia research. Appl Physiol Nutr Metab 35:707–712. https://doi.org/10.1139/h10-067
Stuck AE, Walthert JM, Nikolaus T, Bula CJ, Hohmann C, Beck JC (1999) Risk factors for functional status decline in community-living elderly people: a systematic literature review. Social Sci Med 48:445–469
Janssen I (2006) Influence of sarcopenia on the development of physical disability: the Cardiovascular Health Study. J Am Geriatr Soc 54:56–62. https://doi.org/10.1111/j.1532-5415.2005.00540.x
Kim JS, Wilson JM, Lee SR (2010) Dietary implications on mechanisms of sarcopenia: roles of protein, amino acids and antioxidants. J Nutr Biochem 21:1–13. https://doi.org/10.1016/j.jnutbio.2009.06.014
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinkova E, Vandewoude M, Zamboni M (2010) Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age ageing 39:412–423. https://doi.org/10.1093/ageing/afq034
Gingrich A, Spiegel A, Kob R, Schoene D, Skurk T, Hauner H, Sieber CC, Volkert D, Kiesswetter E (2017) Amount, distribution, and quality of protein intake are not associated with muscle mass, strength, and Power in healthy older adults without functional limitations—an enable study. Nutrients 9. https://doi.org/10.3390/nu9121358
Phillips SM (2016) The impact of protein quality on the promotion of resistance exercise-induced changes in muscle mass. Nutr Metab 13:64. https://doi.org/10.1186/s12986-016-0124-8
Hoffman JR, Falvo MJ (2004) Protein - Which is Best? J Sports Sci Med 3:118–130
Katsanos CS, Kobayashi H, Sheffield-Moore M, Aarsland A, Wolfe RR (2006) A high proportion of leucine is required for optimal stimulation of the rate of muscle protein synthesis by essential amino acids in the elderly. Am J Physiol Endocrinol Metab 291:E381–E387. https://doi.org/10.1152/ajpendo.00488.2005
Bauer J, Biolo G, Cederholm T, Cesari M, Cruz-Jentoft AJ, Morley JE, Phillips S, Sieber C, Stehle P, Teta D, Visvanathan R, Volpi E, Boirie Y (2013) Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc 14:542–559. https://doi.org/10.1016/j.jamda.2013.05.021
Gingrich A, Spiegel A, Gradl JE, Skurk T, Hauner H, Sieber CC, Volkert D, Kiesswetter E (2018) Daily and per-meal animal and plant protein intake in relation to muscle mass in healthy older adults without functional limitations: an enable study. Aging Clin Exp Res. https://doi.org/10.1007/s40520-018-1081-z
Volpi E, Campbell WW, Dwyer JT, Johnson MA, Jensen GL, Morley JE, Wolfe RR (2013) Is the optimal level of protein intake for older adults greater than the recommended dietary allowance? J Gerontol Series A, Biol Sci Med Sci 68:677–681. https://doi.org/10.1093/gerona/gls229
Trumbo P, Schlicker S, Yates AA, Poos M (2002) Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J Am Diet Assoc 102:1621–1630
Houston DK, Nicklas BJ, Ding J, Harris TB, Tylavsky FA, Newman AB, Lee JS, Sahyoun NR, Visser M, Kritchevsky SB (2008) Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the Health, Aging, and Body Composition (Health ABC) Study. Am J Clin Nutr 87:150–155. https://doi.org/10.1093/ajcn/87.1.150
Buckinx F, Allepaerts S, Paquot N, Reginster JY, de Cock C, Petermans J, Bruyere O (2017) Energy and nutrient content of food served and consumed by nursing home residents. J Nutr Health Aging 21:727–732. https://doi.org/10.1007/s12603-016-0782-2
Gregorio L, Brindisi J, Kleppinger A, Sullivan R, Mangano KM, Bihuniak JD, Kenny AM, Kerstetter JE, Insogna KL (2014) Adequate dietary protein is associated with better physical performance among post-menopausal women 60–90 years. J Nutr Health Aging 18:155–160. https://doi.org/10.1007/s12603-013-0391-2
Farsijani S, Payette H, Morais JA, Shatenstein B, Gaudreau P, Chevalier S (2017) Even mealtime distribution of protein intake is associated with greater muscle strength, but not with 3-y physical function decline, in free-living older adults: the Quebec longitudinal study on Nutrition as a Determinant of Successful Aging (NuAge study). Am J Clin Nutr 106:113–124. https://doi.org/10.3945/ajcn.116.146555
Moore DR, Robinson MJ, Fry JL, Tang JE, Glover EI, Wilkinson SB, Prior T, Tarnopolsky MA, Phillips SM (2009) Ingested protein dose response of muscle and albumin protein synthesis after resistance exercise in young men. Am J Clin Nutr 89:161–168. https://doi.org/10.3945/ajcn.2008.26401
Farsijani S, Morais JA, Payette H, Gaudreau P, Shatenstein B, Gray-Donald K, Chevalier S (2016) Relation between mealtime distribution of protein intake and lean mass loss in free-living older adults of the NuAge study. Am J Clin Nutr 104:694–703. https://doi.org/10.3945/ajcn.116.130716
Bollwein J, Diekmann R, Kaiser MJ, Bauer JM, Uter W, Sieber CC, Volkert D (2013) Distribution but not amount of protein intake is associated with frailty: a cross-sectional investigation in the region of Nurnberg. Nutr J 12:109. https://doi.org/10.1186/1475-2891-12-109
Bouillanne O, Curis E, Hamon-Vilcot B, Nicolis I, Chretien P, Schauer N, Vincent JP, Cynober L, Aussel C (2013) Impact of protein pulse feeding on lean mass in malnourished and at-risk hospitalized elderly patients: a randomized controlled trial. Clin Nutr (Edinburgh Scotland) 32:186–192. https://doi.org/10.1016/j.clnu.2012.08.015
Mamerow MM, Mettler JA, English KL, Casperson SL, Arentson-Lantz E, Sheffield-Moore M, Layman DK, Paddon-Jones D (2014) Dietary protein distribution positively influences 24-h muscle protein synthesis in healthy adults. J Nutr 144:876–880. https://doi.org/10.3945/jn.113.185280
Gray M, Powers M, Boyd L, Garver K (2018) Longitudinal comparison of low- and high-velocity resistance training in relation to body composition and functional fitness of older adults. Aging Clin Exper Res 30:1465–1473. https://doi.org/10.1007/s40520-018-0929-6
Barbat-Artigas S, Dupontgand S, Pion CH, Feiter-Murphy Y, Aubertin-Leheudre M (2014) Identifying recreational physical activities associated with muscle quality in men and women aged 50 years and over. J Cachexia Sarcopenia Muscle 5:221–228. https://doi.org/10.1007/s13539-014-0143-0
Gibala MJ (2007) High-intensity interval training: a time-efficient strategy for health promotion? Curr Sports Med Rep 6:211–213
Coetsee C, Terblanche E (2017) The effect of three different exercise training modalities on cognitive and physical function in a healthy older population. Eur Rev Aging Phys Activity 14:13. https://doi.org/10.1186/s11556-017-0183-5
Fex A, Leduc-Gaudet JP, Filion ME, Karelis AD, Aubertin-Leheudre M (2015) Effect of elliptical high intensity interval training on metabolic risk factor in pre- and type 2 diabetes patients: a pilot study. J Phys Act Health 12:942–946. https://doi.org/10.1123/jpah.2014-0123
Batacan RB Jr, Duncan MJ, Dalbo VJ, Tucker PS, Fenning AS (2017) Effects of high-intensity interval training on cardiometabolic health: a systematic review and meta-analysis of intervention studies. Br J Sports Med 51:494–503. https://doi.org/10.1136/bjsports-2015-095841
Sculthorpe NF, Herbert P, Grace F (2017) One session of high-intensity interval training (HIIT) every 5 days, improves muscle power but not static balance in lifelong sedentary ageing men: a randomized controlled trial. Medicine 96:e6040. https://doi.org/10.1097/md.0000000000006040
Karlsen T, Aamot IL, Haykowsky M, Rognmo O (2017) High intensity interval training for maximizing health outcomes. Prog Cardiovasc Dis 60:67–77. https://doi.org/10.1016/j.pcad.2017.03.006
Gillen JB, Gibala MJ (2014) Is high-intensity interval training a time-efficient exercise strategy to improve health and fitness? Appl Physiol Nutr Metab 39:409–412. https://doi.org/10.1139/apnm-2013-0187
Garcia-Pinillos F, Camara-Perez JC, Soto-Hermoso VM, Latorre-Roman PA (2017) A high intensity interval training (HIIT)-based running plan improves athletic performance by improving muscle power. J Strength Cond Res 31:146–153. https://doi.org/10.1519/jsc.0000000000001473
Thum JS, Parsons G, Whittle T, Astorino TA (2017) High-intensity interval training elicits higher enjoyment than moderate intensity continuous exercise. PloS One 12:e0166299. https://doi.org/10.1371/journal.pone.0166299
Vella CA, Taylor K, Drummer D (2017) High-intensity interval and moderate-intensity continuous training elicit similar enjoyment and adherence levels in overweight and obese adults. Eur J Sport Sci 17:1203–1211. https://doi.org/10.1080/17461391.2017.1359679
Mitchell CJ, Milan AM, Mitchell SM, Zeng N, Ramzan F, Sharma P, Knowles SO, Roy NC, Sjodin A, Wagner KH, Cameron-Smith D (2017) The effects of dietary protein intake on appendicular lean mass and muscle function in elderly men: a 10-wk randomized controlled trial. Am J Clin Nutr 106:1375–1383. https://doi.org/10.3945/ajcn.117.160325
Dulac MC, Pion CH, Lemieux F, Boutros El Hajj G, Belanger M, Gaudreau P, Chevalier S, Morais JA, Gouspillou G, Aubertin-Leheudre M (2018) Differences in muscle adaptation to a 12-week mixed power training in elderly men, depending on usual protein intake. Exp Gerontol 104:78–85. https://doi.org/10.1016/j.exger.2018.02.001
Hudson JL, Kim JE, Paddon-Jones D, Campbell WW (2017) Within-day protein distribution does not influence body composition responses during weight loss in resistance-training adults who are overweight. Am J Clin Nutr 106:1190–1196. https://doi.org/10.3945/ajcn.117.158246
Kim IY, Schutzler S, Schrader AM, Spencer HJ, Azhar G, Wolfe RR, Ferrando AA (2018) Protein intake distribution pattern does not affect anabolic response, lean body mass, muscle strength or function over 8 weeks in older adults: A randomized-controlled trial. Clin Nutr (Edinburgh Scotland) 37:488–493. https://doi.org/10.1016/j.clnu.2017.02.020
Baumgartner RN, Wayne SJ, Waters DL, Janssen I, Gallagher D, Morley JE (2004) Sarcopenic obesity predicts instrumental activities of daily living disability in the elderly. Obes Res 12:1995–2004. https://doi.org/10.1038/oby.2004.250
Chen MJ, Fan X, Moe ST (2002) Criterion-related validity of the Borg ratings of perceived exertion scale in healthy individuals: a meta-analysis. J Sports Sci 20:873–899. https://doi.org/10.1080/026404102320761787
Karvonen J, Vuorimaa T (1988) Heart rate and exercise intensity during sports activities. Practical application. Sports Med 5:303–311
Williams JE, Wells JC, Wilson CM, Haroun D, Lucas A, Fewtrell MS (2006) Evaluation of Lunar Prodigy dual-energy X-ray absorptiometry for assessing body composition in healthy persons and patients by comparison with the criterion 4-component model. Am J Clin Nutr 83:1047–1054
Kiebzak GM, Leamy LJ, Pierson LM, Nord RH, Zhang ZY (2000) Measurement precision of body composition variables using the lunar DPX-L densitometer. J Clin Densitom 3:35–41
ATS statement: guidelines for the six-minute walk test (2002) Am J Respir Crit Care Med 166:111–117. https://doi.org/10.1164/ajrccm.166.1.at1102
Burr JF, Bredin SS, Faktor MD, Warburton DE (2011) The 6-minute walk test as a predictor of objectively measured aerobic fitness in healthy working-aged adults. Phys Sports Med 39:133–139. https://doi.org/10.3810/psm.2011.05.1904
Munoz-Mendoza CL, Cabanero-Martinez MJ, Millan-Calenti JC, Cabrero-Garcia J, Lopez-Sanchez R, Maseda-Rodriguez A (2011) Reliability of 4-m and 6-m walking speed tests in elderly people with cognitive impairment. Arch Gerontol Geriatr 52:e67–e70. https://doi.org/10.1016/j.archger.2010.06.020
Unver B, Baris RH, Yuksel E, Cekmece S, Kalkan S, Karatosun V (2017) Reliability of 4-meter and 10-meter walk tests after lower extremity surgery. Disabil Rehabil 39:2572–2576. https://doi.org/10.1080/09638288.2016.1236153
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39:142–148
Mathias S, Nayak US, Isaacs B (1986) Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil 67:387–389
Yanagawa N, Shimomitsu T, Kawanishi M, Fukunaga T, Kanehisa H (2016) Relationship between performances of 10-time-repeated sit-to-stand and maximal walking tests in non-disabled older women. J Physiol Anthropol 36:2. https://doi.org/10.1186/s40101-016-0100-z
Chung MM, Chan RW, Fung YK, Fong SS, Lam SS, Lai CW, Ng SS (2014) Reliability and validity of Alternate Step Test times in subjects with chronic stroke. J Rehabil Med 46:969–974. https://doi.org/10.2340/16501977-1877
Berg KO, Wood-Dauphinee SL, Williams JI, Maki B (1992) Measuring balance in the elderly: validation of an instrument. Can J Publ health 83(Suppl 2):S7–S11
Springer BA, Marin R, Cyhan T, Roberts H, Gill NW (2007) Normative values for the unipedal stance test with eyes open and closed. J Geriat Phys Ther 30:8–15
Mathiowetz V, Weber K, Volland G, Kashman N (1984) Reliability and validity of grip and pinch strength evaluations. J Hand Surg 9:222–226
Dulac M, Boutros GE, Pion C, Barbat-Artigas S, Gouspillou G, Aubertin-Leheudre M (2016) Is handgrip strength normalized to body weight a useful tool to identify dynapenia and functional incapacity in post-menopausal women? Braz J Phys Ther 20:510–516. https://doi.org/10.1590/bjpt-rbf.2014.0184
Houtz SJ, Lebow MJ, Beyer FR (1957) Effect of posture on strength of the knee flexor and extensor muscles. J Appl Physiol 11:475–480
Williams M, Stutzman L (1959) Strength variation through the range of joint motion. Phys Ther Rev 39:145–152
Riggs BL, Wahner HW, Dunn WL, Mazess RB, Offord KP, Melton LJ 3rd (1981) Differential changes in bone mineral density of the appendicular and axial skeleton with aging: relationship to spinal osteoporosis. J Clin Investig 67:328–335. https://doi.org/10.1172/JCI110039
Barbat-Artigas S, Rolland Y, Cesari M, Abellan van Kan G, Vellas B, Aubertin-Leheudre M (2013) Clinical relevance of different muscle strength indexes and functional impairment in women aged 75 years and older. J Gerontol Ser A, Biol Sci Med Sci 68:811–819. https://doi.org/10.1093/gerona/gls254
Verdijk LB, van Loon L, Meijer K, Savelberg HH (2009) One-repetition maximum strength test represents a valid means to assess leg strength in vivo in humans. J Sports Sci 27:59–68. https://doi.org/10.1080/02640410802428089
Newman AB, Kupelian V, Visser M, Simonsick EM, Goodpaster BH, Kritchevsky SB, Tylavsky FA, Rubin SM, Harris TB (2006) Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J Gerontol Series A, Biol Sci Med Sci 61:72–77
Bassey EJ, Short AH (1990) A new method for measuring power output in a single leg extension: feasibility, reliability and validity. Eur J Appl Physiol 60:385–390
Skelton DA, Kennedy J, Rutherford OM (2002) Explosive power and asymmetry in leg muscle function in frequent fallers and non-fallers aged over 65. Age Ageing 31:119–125
Blew RM, Lee VR, Farr JN, Schiferl DJ, Going SB (2014) Standardizing evaluation of pQCT image quality in the presence of subject movement: qualitative versus quantitative assessment. Calcif Tissue Int 94:202–211
Doube M, Kłosowski MM, Arganda-Carreras I, Cordelières FP, Dougherty RP, Jackson JS, Schmid B, Hutchinson JR, Shefelbine SJ (2010) BoneJ: free and extensible bone image analysis in ImageJ. Bone 47:1076–1079
Frank-Wilson AW, Johnston JD, Olszynski WP, Kontulainen SA (2015) Measurement of muscle and fat in postmenopausal women: precision of previously reported pQCT imaging methods. Bone 75:49–54
Brazeau AS, Beaudoin N, Belisle V, Messier V, Karelis AD, Rabasa-Lhoret R (2016) Validation and reliability of two activity monitors for energy expenditure assessment. J Sci Med Sport 19:46–50. https://doi.org/10.1016/j.jsams.2014.11.001
Colbert LH, Matthews CE, Havighurst TC, Kim K, Schoeller DA (2011) Comparative validity of physical activity measures in older adults. Med Sci Sports Exerc 43:867–876. https://doi.org/10.1249/MSS.0b013e3181fc7162
Buckley S, Knapp K, Lackie A, Lewry C, Horvey K, Benko C, Trinh J, Butcher S (2015) Multimodal high-intensity interval training increases muscle function and metabolic performance in females. Appl Physiol Nutr Metab 40:1157–1162. https://doi.org/10.1139/apnm-2015-0238
Dawson BM, Axford S (2014) Nutrition as a part of healthy aging and reducing cardiovascular risk: improving functionality in later life using quality protein, with optimized timing and distribution. Semin Thromb Hemost 40:695–703. https://doi.org/10.1055/s-0034-1389081
Moore DR, Churchward-Venne TA, Witard O, Breen L, Burd NA, Tipton KD, Phillips SM (2015) Protein ingestion to stimulate myofibrillar protein synthesis requires greater relative protein intakes in healthy older versus younger men. J Gerontol Series A, Biol Sci Med Sci 70:57–62. https://doi.org/10.1093/gerona/glu103
Burd NA, Gorissen SH, van Loon LJ (2013) Anabolic resistance of muscle protein synthesis with aging. Exerc Sport Sci Rev 41:169–173. https://doi.org/10.1097/JES.0b013e318292f3d5
Maltais M, Du Bois-Dit-Bonclaude M, Amamou T, Riesco E, Dionne IJ (2018) The impact of post-resistance exercise protein consumption on subsequent appetite and daily energy intake of sarcopenic older men: a pilot study. Aging Clin Exp Res 30:1087–1092. https://doi.org/10.1007/s40520-017-0880-y
Acknowledgements
This study was supported by the Fonds de Recherche du Québec en Santé (FRQS) - Université du Québec à Montréal fund and by the Quebec Network for Research on Aging, a thematic network supported by the FRQS (QNRA-FRQS) and the Canada Foundation for Innovation. MAL is recipient of Chercheur Boursier Junior 2 salary awards from the FRQS. DM is recipient of PhD scholarship from the FRQS. The authors are grateful to all the volunteers for their participation in this study and to Carole Roy for her technical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures were approved by the Ethics Committee of the Université du Québec à Montréal (UQAM).
Informed consent
All participants provided informed written consent after having received information on nature, goal, procedures and risks associated with the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Buckinx, F., Gaudreau, P., Marcangeli, V. et al. Muscle adaptation in response to a high-intensity interval training in obese older adults: effect of daily protein intake distribution. Aging Clin Exp Res 31, 863–874 (2019). https://doi.org/10.1007/s40520-019-01149-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01149-y