Abstract
Background
Given the progressive demographic ageing of the population and the National Health System reforms affecting care at the bedside, a periodic re-evaluation of in-hospital mortality rates and associated factors is recommended.
Aims
To describe the occurrence of in-hospital mortality among patients admitted to acute medical units and associated factors. Two hypotheses (H) were set as the basis of the study: patients have an increased likelihood to die H1: at the weekend when less nursing care is offered; H2: when they receive nursing care with a skill-mix in favour of Nursing Aides instead of Registered Nurses.
Methods
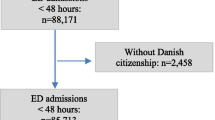
Secondary analysis of a prospective study of patients >65 years consecutively admitted in 12 Italian medical units. Data on individual and nursing care variables were collected and its association with in-hospital mortality was analysed by stepwise logistic regression analysis.
Results
In-hospital mortality occurrence was 6.8 %, and 37 % of the patients died during the weekend. The logistic regression model explained 34.3 % (R 2) of the variance of in-hospital mortality: patients were six times (95 % CI = 3.632–10.794) more likely at risk of dying at weekends; those with one or more AEDs admissions in the last 3 months were also at increased risk of dying (RR 1.360, 95 % CI = 1.024–1.806) as well as those receiving more care from family carers (RR = 1.017, 95 % CI = 1.009–1.025). At the nursing care level, those patient receiving less care by RNs at weekends were at increased risk of dying (RR = 2.236, 95 % CI = 1.270–3.937) while those receiving a higher skill-mix, thus indicating that more nursing care was offered by RNs instead of NAs were at less risk of dying (RR = 0.940, 95 % CI = 0.912–0.969).
Conclusions
Within the limitations of this secondary analysis, in addition to the role of some clinical factors, findings suggest redesigning acute care at weekends ensuring consistent care both at the hospital and at the nursing care levels.
Similar content being viewed by others
References
Toscani F, Di Giulio P, Brunelli C et al (2005) How people die in hospital general wards: a descriptive study. J Pain Symptom Manag 30:33–40
Campbell MJ, Jacques RM, Fotheringham J et al (2012) Developing a summary hospital mortality index: retrospective analysis in English hospitals over five years. BMJ 344:e1001. doi:10.1136/bmj.e1001
Viana A, Carballo F, Beato I et al (1990) An analysis of 14,000 patients admitted to an internal medicine service during 1982–1988. An Med Interna 7:459–462
Escolar Castellón F, Sampériz Legarre AL, Pérez Poza A et al (1993) Morbidity, mortality and other indicators of health care activities, at a General Internal Medicine Service. An Med Interna 10:327–332
Del Río Fernández MC, Fernández Renedo A, de Frutos Arribas JF et al (1998) Mortality in an internal medicine department within a third-level hospital; twenty years experience. An Med Interna 15:197–201
Delgado Morales JL, Alonso del Busto R, Pascual Calleja I et al (2004) Observational study of patients admitted to an Internal Medicine service. An med Interna 21:3–6
Barba R, Losa JE, Velasco M et al (2006) Mortality among adult patients admitted to the hospital on weekends. Eur J Intern Med 17:322–324
Rayego Rodríguez J, Rodríguez-Vidigal FF, Mayoral Martín L et al (2006) Hospital Mortality in the Internal Medicine Services of a first level center. An Med Interna 23:406–410
Barba Martín R, Marco Martínez J, Emilio Losa J et al (2009) Two-year analysis of internal medicine activity in the National Health Care System hospitals. Rev Clin Esp 209:459–466
Marco J, Barba R, Plaza S et al (2010) Analysis of the mortality of patients admitted to internal medicine wards over the weekend. Am J Med Qual 25:312–318. doi:10.1177/1062860610366031
Leshem-Rubinow E, Vaknin A, Sherman S et al (2013) Norton scale, hospitalization length, complications, and mortality in elderly patients admitted to internal medicine departments. Gerontology 59:507–513. doi:10.1159/000353710
Nobili A, Licata G, Salerno F et al (2011) Polypharmacy, length of hospital stay, and in-hospital mortality among elderly patients in internal medicine wards. The REPOSI study. Eur J Clin Pharmacol 67:507–519. doi:10.1007/s00228-010-0977-0
Marengoni A, Nobili A, Romano V et al (2013) Adverse clinical events and mortality during hospitalization and 3 months after discharge in cognitively impaired elderly patients. J Gerontol A Biol Sci Med Sci 68:419–425. doi:10.1093/gerona/gls181
Aiken LH, Sloane DM, Bruyneel L et al (2014) Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet 383:1824–1830. doi:10.1016/S0140-6736(13)62631-8
Tourangeau AE, Cranley LA, Jeffs L (2006) Impact of nursing on hospital patient mortality: a focused review and related policy implications. Qual Saf Health Care 15:4–8
Meschi T, Ticinesi A, Prati B et al (2016) A novel organizational model to face the challenge of multimorbid elderly patients in an internal medicine setting: a case study from Parma Hospital, Italy. Intern Emerg Med (in press)
La Regina M, Orlandini F, Ligurian Internal Medicine Group (2014) Internal medicine wards and the chronic diseases epidemic: it is time to change the standards. Intern Emerg Med 9:483–485. doi:10.1007/s11739-013-1029-4
Huang C-C, Huang Y-T, Hsu N-C et al (2016) Effect of weekend admissions on the treatment process and outcomes of internal medicine patients a nationwide cross-sectional study. Medicine (Baltimore) 95:e2643. doi:10.1097/MD.0000000000002643
Organization for Economic Co-operation and Development (OECD) (2015). http://stats.oecd.org/. Accessed 29 Dec 2015
Palese A, Bevilacqua MG, Dante A et al (2010) Do randomized controlled nursing trials have a pragmatic or explanatory attitude? Findings from the Pragmatic-Explanatory Continuum Indicator Summary (PRECIS) tool exercise. J Nurs Res 22:216–220. doi:10.1097/jnr.0000000000000045
Palese A, Ambrosi E, Prosperi L et al (2015) Missed nursing care and predicting factors in the Italian medical care setting. Intern Emerg Med 10:693–702. doi:10.1007/s11739-015-1232-6
Palese A, Cuel M, Zambiasi P et al (2013) Nursing care received by older patients in Italian medical units: findings from an explorative study. Aging Clin Exp Res 25:707–710
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel Index. Md State Med J 14:61–65
Bergstrom N, Braden BJ, Laguzza A et al (1987) The Braden Scale for predicting pressure sore risk. Nurs Res 36:205–210
Blaylock A, Cason CL (1992) Discharge planning predicting patients’ needs. J Gerontol Nurs 18:5–10
Saiani L, Zanolin ME, Dalponte A et al (2008) Sensibility and specificity of a screening instrument for patients at risk of difficult discharge. Assist Inferm Ric 27:184–193
Registered Nurses Association of Ontario (RNAO) (2003) Screening for delirium,dementia and depression in older adults. Registered Nurses Association of Ontario (RNAO), Toronto
Socorro García A, de la Puente M, Perdomo B et al (2015) Functional status and mortality at month and year in nonagenarians hospitalized due to acute medical illness. Eur J Intern Med 26:705–708. doi:10.1016/j.ejim.2015.08.007
Kalisch BJ, Williams RA (2009) Development and psychometric testing of a tool to measure missed nursing care. J Nurs Adm 39:211–219. doi:10.1097/NNA.0b013e3181a23cf5
Sist L, Cortini C, Bandini A et al (2012) Il concetto di missed nursing care: una revisione narrativa della letteratura. Assist Inferm Ric 31:234–239. doi:10.1702/1211.13414
Callaly E, Mikulich O, Silke B (2013) Increased winter mortality: the effect of season, temperature and deprivation in the acutely ill medical patient. Eur J Intern Med 24:546–551. doi:10.1016/j.ejim.2013.02.004
Barba R, Martínez JM, Zapatero A et al (2011) Mortality and complications in very old patients (90+) admitted to departments of internal medicine in Spain. Eur J Intern Med 22:49–52. doi:10.1016/j.ejim.2010.11.001
Teno JM, Gozalo PL, Bynum JP et al (2013) Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA 309:470–477. doi:10.1001/jama.2012.207624
Smith S, Allan A, Greenlaw N et al (2013) Emergency medical admissions, deaths at weekends and the public holiday effect. Cohort study. Emerg Med J 31:30–34. doi:10.1136/emermed-2012-201881
Barba R, Losa JE, Canora J et al (2009) The influence of nursing homes in the functioning of internal medicine services. Eur J Intern Med 20:85–88. doi:10.1016/j.ejim.2008.04.001
Sharp AL, Choi H, Hayward RA (2013) Don’t get sick on the weekend: an evaluation of the weekend effect on mortality for patients visiting US EDs. Am J Emerg Med 31:835–837. doi:10.1016/j.ajem.2013.01.006
Handel AE, Patel SV, Skingsley A et al (2012) Weekend admissions as an independent predictor of mortality: an analysis of Scottish hospital admissions. BMJ Open 2:e001789. doi:10.1136/bmjopen-2012-001789
Aylin P, Yunus A, Bottle A et al (2010) Weekend mortality for emergency admissions. A large, multicentre study. Qual Saf Health Care 19:213–217. doi:10.1136/qshc.2008.028639
Palese A, Beltrame ER, Bin A et al (2008) Esiti sensibili alle cure infermieristiche: analisi critica della letteratura. Assist Inferm Ric 27:33–42
Steinhauser KE, Christakis NA, Clipp EC et al (2000) Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 284:2476–2482
Tourangeau AE, Giovannetti P, Tu JV et al (2002) Nursing-related determinants of 30-day mortality for hospitalized patients. Can J Nurs Res 33:71–88
Goldstein SD, Papandria DJ, Aboagye J et al (2014) The “weekend effect” in pediatric surgery—increased mortality for children undergoing urgent surgery during the weekend. J Pediatr Surg 49:1087–1091. doi:10.1016/j.jpedsurg.2014.01.001
Suissa S, Dell’Aniello S, Suissa D et al (2014) Friday and weekend hospital stays: effects on mortality. Eur Respir J 44:627–633. doi:10.1183/09031936.00007714
Ambrosi E, Biavati C, Guarnier A et al (2015) Factors affecting in-hospital informal caregiving as decided by families: findings from a longitudinal study conducted in acute medical units. Scand J Caring Sci. doi:10.1111/scs.12321 (in press)
Acknowledgments
The researchers would like to thank both the patients and the clinical teams of the involved hospitals for their participation in the research process.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors confirm that there are no conflicts of interest.
Ethical approval
Ethical approval was granted by the Clinical Research Ethics Committee of Verona University Hospital.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Rights and permissions
About this article
Cite this article
Ambrosi, E., De Togni, S., Guarnier, A. et al. In-hospital elderly mortality and associated factors in 12 Italian acute medical units: findings from an exploratory longitudinal study. Aging Clin Exp Res 29, 517–527 (2017). https://doi.org/10.1007/s40520-016-0576-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-016-0576-8