Abstract
Aim
To investigate the prevalence and clinical correlates of overprescribing and underprescribing of low molecular weight heparins (LMWHs) for thromboprophylaxis among older medical inpatients.
Methods
Eight hundred seventy six patients (mean age 81.5 ± 7.6 years, female gender 57.2 %) enrolled in a multicenter observational study of seven acute care wards of geriatric medicine in Italy. The risk of venous thromboembolism was ascertained by calculating the Padua score for each patient. Patients receiving appropriate prescription of LMHW during stay were compared to those receiving LMHW with a Padua score <4 (overprescribing group). Similarly, patients with a high thromboembolic risk (Padua score ≥4) but not receiving LMHW (underprescribing group) were compared to patients appropriately not receiving LMHW during stay. Independent correlates of overprescribing and underprescribing were investigated by logistic regression analysis.
Results
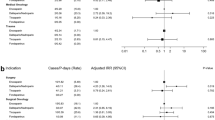
Overall, 42.8 % of patients had a Padua score ≥4. LMWHs were overprescribed in 7.3 % and underprescribed in 25.2 % of patients. The number of lost basic activities of daily living (BADL) (OR = 0.25; 95 % CI 0.15–0.41) and the number of diagnoses (OR = 0.76; 95 % CI 0.61–0.95) were inversely associated with LMWH overprescription. Conversely, older age (75–84 years: OR = 2.39; 95 % CI 1.10–5.19—85 years or more: OR = 3.25, 95 % CI 1.40–7.61), anemia (OR = 1.80, 95 % CI 1.05–3.16), pressure sores (OR = 4.15, 95 % CI 1.20–14.3), number of lost BADL at the admission (OR = 3.92, 95 % CI 2.86–5.37) and number of diagnoses (OR = 1.29, 95 % CI 1.15–1.44) qualified as significant correlates of LMWH underprescription.
Discussion
Underprescription and, to a lesser extent, overprescription still represent an issue among older medical inpatients.
Conclusion
Implementing risk-stratifying scores into clinical practice may improve appropriateness of LMWHs prescribing during hospitalization.

Similar content being viewed by others
References
Mahe I, Gouin-Thibault I, Drouet L, Simoneau G, Di Castillo H, Siguret V, Bergmann JF, Pautas E (2007) Elderly medical patients treated with prophylactic dosages of enoxaparin: influence of renal function on anti-Xa activity level. Drugs Aging 24:63–71
Trc T, Kvasnicka J, Kudrnova Z (2007) Prevention of venous thromboembolism: the seventh conference American College of Chest Physician (ACCP). Acta Chir Orthop Traumatol Cech 74:126–131
Wiseman DN, Harrison J (2010) A retrospective review of the use of thromboprophylaxis in patients who subsequently developed a venous thromboembolism after discharge from hospital. N Z Med J 123:37–49
Mahan CE, Fisher MD, Mills RM, Fields LE, Stephenson JJ, Fu AC, Spyropoulos AC (2013) Thromboprophylaxis patterns, risk factors, and outcomes of care in the medically ill patient population. Thromb Res 132:520–526
Kahn SR, Lim W, Dunn AS, Cushman M, Dentali F, Akl EA, Cook DJ, Balekian AA, Klein RC, Le H, Schulman S, Murad MH (2012) Prevention of VTE in nonsurgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:e195S–e226S
Barbar S, Noventa F, Rossetto V, Ferrari A, Brandolin B, Perlati M, De Bon E, Tormene D, Pagnan A, Prandoni P (2010) A risk assessment model for the identification of hospitalized medical patients at risk for venous thromboembolism: the Padua Prediction Score. J Thromb Haemost 8:2450–2457
Greig MF, Rochow SB, Crilly MA, Mangoni AA (2013) Routine pharmacological venous thromboembolism prophylaxis in frail older hospitalised patients: where is the evidence? Age Ageing 42:428–434
Fitzmaurice DA, Blann AD, Lip GY (2002) Bleeding risks of antithrombotic therapy. BMJ 325:828–831
Navarro Puerto MA, Medrano Ortega FJ, Izquierdo Guerrero R, Calderon Sandubete E, Buzon-Barrera ML, Marin-Leon I (2015) Assessment of thromboprophylaxis in medical patients hospitalized in Andalusia. A multicenter study. Rev Clin Esp 215:141–147
Tosato M, Settanni S, Antocicco M, Battaglia M, Corsonello A, Ruggiero C, Volpato S, Fabbietti P, Lattanzio F, Bernabei R, Onder G (2013) Pattern of medication use among older inpatients in seven hospitals in Italy: results from the Criteria to assess appropriate medication use among Elderly complex patients (CRIME) project. Curr Drug Saf 8:98–103
Pahor M, Chrischilles EA, Guralnik JM, Brown SL, Wallace RB, Carbonin P (1994) Drug data coding and analysis in epidemiologic studies. Eur J Epidemiol 10:405–411
Di Minno A, Spadarella G, Prisco D, Scalera A, Ricciardi E, Di Minno G (2015) Antithrombotic drugs, patient characteristics, and gastrointestinal bleeding: clinical translation and areas of research. Blood Rev 29(5):335–343
Rodeghiero F, Michel M, Gernsheimer T, Ruggeri M, Blanchette V, Bussel JB, Cines DB, Cooper N, Godeau B, Greinacher A, Imbach P, Khellaf M, Klaassen RJ, Kuhne T, Liebman H, Mazzucconi MG, Newland A, Pabinger I, Tosetto A, Stasi R (2013) Standardization of bleeding assessment in immune thrombocytopenia: report from the International Working Group. Blood 121:2596–2606
Mucino-Bermejo J, Carrillo-Esper R, Uribe M, Mendez-Sanchez N (2013) Coagulation abnormalities in the cirrhotic patient. Ann Hepatol 12:713–724
Kooiman J, den Exter PL, Cannegieter SC, le Cessie S, del Toro J, Sahuquillo JC, Pedrajas JM, Huisman MV (2013) Impact of chronic kidney disease on the risk of clinical outcomes in patients with cancer-associated venous thromboembolism during anticoagulant treatment. J Thromb Haemost 11:1968–1976
Matta F, Singala R, Yaekoub AY, Najjar R, Stein PD (2009) Risk of venous thromboembolism with rheumatoid arthritis. Thromb Haemost 101:134–138
Lee AY, Levine MN (2003) Venous thromboembolism and cancer: risks and outcomes. Circulation 107:I17–I21
Huang W, Anderson FA, Rushton-Smith SK, Cohen AT (2015) Impact of thromboprophylaxis across the US acute care setting. PLoS One 10:e0121429
Goldhaber SZ, Dunn K, MacDougall RC (2000) New onset of venous thromboembolism among hospitalized patients at Brigham and Women’s Hospital is caused more often by prophylaxis failure than by withholding treatment. Chest 118:1680–1684
Kahn SR, Panju A, Geerts W, Pineo GF, Desjardins L, Turpie AG, Glezer S, Thabane L, Sebaldt RJ (2007) Multicenter evaluation of the use of venous thromboembolism prophylaxis in acutely ill medical patients in Canada. Thromb Res 119:145–155
Montero Ruiz E, Baldominos Utrilla G, Lopez Alvarez J, Santolaya Perrin R (2011) Effectiveness and safety of thromboprophylaxis with enoxaparin in medical inpatients. Thromb Res 128:440–445
Sganga F, Landi F, Vetrano DL, Corsonello A, Lattanzio F, Bernabei R, Onder G (2015) Impact of hospitalization on modification of drug regimens: results of the criteria to assess appropriate medication use among elderly complex patients study. Geriatr Gerontol Int. doi:10.1111/ggi.12517
Decousus H, Tapson VF, Bergmann JF, Chong BH, Froehlich JB, Kakkar AK, Merli GJ, Monreal M, Nakamura M, Pavanello R, Pini M, Piovella F, Spencer FA, Spyropoulos AC, Turpie AG, Zotz RB, Fitzgerald G, Anderson FA (2011) Factors at admission associated with bleeding risk in medical patients: findings from the IMPROVE investigators. Chest 139:69–79
Yusen RD, Hull RD, Schellong SM, Tapson VF, Monreal M, Samama MM, Chen M, Deslandes B, Turpie AG (2013) Impact of age on the efficacy and safety of extended-duration thromboprophylaxis in medical patients. Subgroup analysis from the EXCLAIM randomised trial. Thromb Haemost 110:1152–1163
Palareti G, Cosmi B (2009) Bleeding with anticoagulation therapy—who is at risk, and how best to identify such patients. Thromb Haemost 102:268–278
Lip GY (2011) Chronic renal disease and stroke in atrial fibrillation: balancing the prevention of thromboembolism and bleeding risk. Europace 13:145–148
Poli M, Girelli D, Campostrini N, Maccarinelli F, Finazzi D, Luscieti S, Nai A, Arosio P (2011) Heparin: a potent inhibitor of hepcidin expression in vitro and in vivo. Blood 117:997–1004
Holbrook A, Schulman S, Witt DM, Vandvik PO, Fish J, Kovacs MJ, Svensson PJ, Veenstra DL, Crowther M, Guyatt GH (2012) Evidence-based management of anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:e152S–e184S
de Lissovoy G, Subedi P (2002) Economic evaluation of enoxaparin as prophylaxis against venous thromboembolism in seriously ill medical patients: a US perspective. Am J Manag Care 8:1082–1088
Khorana AA, Carrier M, Garcia DA, Lee AY (2016) Guidance for the prevention and treatment of cancer-associated venous thromboembolism. J Thromb Thrombolysis 41:81–91
Shirvanian S, Tapson VF (2015) Venous thromboembolism: identifying patients at risk and establishing prophylaxis. Curr Med Res Opin 31:2297–2311
Acknowledgments
The study group CRIME: (Gemelli Hospital, Center of Aging Medicine, Catholic University of the Sacred Heart, Rome, Italy; University of Perugia, University of Ferrara, Italian National Research Center on Aging—INRCA situated in Ancona, Cosenza, Fermo, and Rome).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. No animal experiments are included in this study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Funding
The study was supported by the Italian Ministry of Health (Grants No. GR-2007-685638).
Rights and permissions
About this article
Cite this article
Garasto, S., Fusco, S., Onder, G. et al. Inappropriate prescription of low molecular weight heparins for thromboprophylaxis among older hospitalized patients. Aging Clin Exp Res 29, 483–490 (2017). https://doi.org/10.1007/s40520-016-0571-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-016-0571-0