Abstract
Objectives
The purpose of this study is to investigate whether the relationship between weight stigma experiences and disordered eating behaviors during the COVID-19 pandemic is mediated by weight gain concern and psychological distress among university students with and without overweight.
Methods
A cross-sectional study was conducted with university students from five regions of Brazil who participated in the baseline assessment of the Online Cohort on Eating Behavior and Health (July/August 2020). Information on the frequency of binge eating episodes, food restriction, and purging, as well as experienced weight stigma, weight gain concern, and psychological distress, were recorded in an online questionnaire. Stratified structural equation modeling (SEM) analyses were performed to address the research questions of interest.
Results
Out of the total sample (n = 2511), 33.5% of participants reported experiencing weight stigma. The prevalence of binge eating episodes, food restriction, and purging was 43.7%, 24.1%, and 5.4%, respectively. These behaviors were more prevalent in individuals with overweight than in those without this condition. Furthermore, it was observed that weight gain concern and psychological distress mediated the relationship between weight stigma and disordered eating behaviors regardless of body weight status.
Conclusions
Experiences of weight stigma and disordered eating behaviors were prevalent among Brazilian university students, especially among those with overweight. Weight gain concern and psychological distress appear to be important factors underlying the relationship between these constructs during the pandemic, and they can contribute to the development of targeted strategies for the prevention and management of disordered eating.
Level of evidence
Level V, cross-sectional study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the beginning of the COVID-19 pandemic, body weight has been the focus of media and scientific coverage, with news highlighting obesity as a comorbidity that worsens viral infection and social isolation as a contributing factor to weight gain [1, 2]. Although this discussion has been grounded in health care considerations, it is inferred that this scenario may have contributed to the manifestation of weight stigma [1], predominantly directed toward individuals with higher body weight [3, 4].
Weight stigma is a multidimensional phenomenon that encompasses structural and individual forms of devaluation and derogation due to excess weight [5]. From this perspective, experiences of weight stigma, or experienced weight stigma, are situated at the individual level and focus on the perception of the individual who has undergone stigmatization-related experiences [6]. This construct is a well-known risk factor for the development of various disordered eating behaviors (DEB), or disordered eating (DE), in the pre-pandemic context [7,8,9,10,11].
Furthermore, it is worth considering that DEB encompasses various behaviors [12], ranging from binge eating to restrictive dieting for weight loss, which are prevalent among young adults and associated with higher body weight and body image dissatisfaction [13,14,15]. Although theoretical frameworks suggest that similar models can explain the effect of weight stigma on binge eating, restrictive eating, and purging behaviors [16, 17], understanding the associations between weight stigma and DEB during the pandemic is particularly relevant, because this context has been shown to be conducive to increased experiences of weight stigma [3, 18] and the development of DEB [19,20,21].
Beyond weight stigma, the literature highlights a multitude of variables that can directly or indirectly influence disordered eating behaviors (DEB). These variables encompass concerns related to appearance, body dissatisfaction, and the internalization of beauty ideals [22,23,24,25]. While classic theoretical models, such as the tripartite model, are commonly used to explain sociocultural factors in the development of DEB, the incorporation of weight stigma into models that encompass aspects like weight and appearance concerns is a relatively nascent endeavor [16, 17, 26]. Hence, the incorporation of sociocultural and psychological variables can aid in comprehending the intricate connections associated with the development of DEB, thereby expanding the existing literature.
In this regard, Rodgers et al. [27] propose that due to the disruption in routine during the pandemic, variables such as psychological distress and increased concern about weight and body shape may be associated with an increase in disordered eating behaviors. However, despite the inclusion of body dissatisfaction and mental health in previous models seeking to explain the relationship between weight stigma and DE [16, 17], specific weight gain concerns have not been considered thus far. In addition, understanding these relationships among university students is important given the high prevalence of DEB in this group [15, 23] and their increased vulnerability to poorer mental health outcomes [28].
Finally, the recognition of the implications of weight stigma on disordered eating behaviors is significant in both pre-pandemic and pandemic settings across various populations [29,30,31,32], but its assessment remains limited in Brazil. Thus far, two isolated studies have investigated the association between these constructs among Brazilian adolescents in the pre-pandemic period [33, 34], and one study was conducted with adults during the pandemic [35].
Therefore, considering that experiences of weight stigma are prevalent in Western countries [36], the fact that the pandemic intensifies these experiences [3, 4] and that this phenomenon may be associated with episodes of disordered eating behaviors in individuals with and without overweight [16, 17, 38], a broader understanding of these issues is important. Such clarifications are essential for planning prevention and intervention strategies for eating disorders.
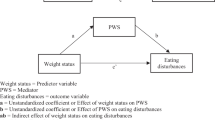
The aim of this study is to test an adapted theoretical model based on O'Brien et al. (2016) [16] and Romano et al. (2020) [17]—incorporating the variable of weight gain concern—to clarify the relationship between experiences of weight stigma and disordered eating behaviors among Brazilian students, both those with and without overweight, during the COVID-19 pandemic. The underlying hypothesis is that this relationship is mediated by weight gain concern and psychological distress (see Fig. 1) in both weight groups during this period after controlling for confounding variables, such as sex, race/ethnicity, income, and age.
Methodology
Study design
This is a cross-sectional study using data from the Online Cohort on Eating Behavior and Health (COCASa: Cohort Online on Eating Behavior and Health). COCASa is a national longitudinal research project that aims to study the influence of the COVID-19 pandemic on eating behavior and mental health among students and faculty members from Brazilian universities. This cohort started in July 2020, and data collection was completed in October 2022. At the baseline of the study, a total of 3178 students and 1919 faculty members from public and private undergraduate institutions across the five regions of the country were included and responded to all questionnaires. This research was approved by the ethics committee of the School of Nutrition at the Federal University of Bahia (approval number 4,125,928) in accordance with national health regulations for research involving human subjects and the recommendations for conducting research during the pandemic. More detailed information about other methodological aspects and additional cross-sectional analyses of the COCASa study have been described in separate manuscripts with different objectives [35, 40].
Participants and procedure
Participants included undergraduate students over the age of 18, of both sexes, enrolled in courses that had face-to-face activities suspended during the pandemic. Women who were pregnant or lactating and individuals over the age of 60 were not eligible to participate in this study. Out of the 3178 university students at baseline, the following exclusions were made: (1) 57 participants were excluded due to pregnancy/lactation (1.7%), (2) 14 participants were excluded due to being older adults (0.4%), and (3) after reviewing the questionnaires, 370 participants were excluded due to missing data (11.6%), and 226 participants were excluded because they selected the response option “prefer not to answer” for sociodemographic variables (7.1%). Thus, the final sample consisted of 2511 university students (1909 women and 602 men) (Fig. 2).
Sample power
In this study, the sample power was calculated using power analysis techniques. For the mediation analysis, the method proposed by Sobel [41] was employed to estimate the confidence intervals for indirect effects in structural equation models. In addition, the pwrss package in R [42] was utilized to calculate the statistical power and minimum required sample size. This package provides a comprehensive set of tools for power analysis and sample size calculations across various statistical tests, including testing an indirect effect in mediation analysis. The calculations revealed a sample power of 90% considering the sample of 2511 university students, allowing for a robust examination of the relationships between experienced weight stigma, psychological distress, weight gain concern, and disordered eating behaviors.
Measures
Disordered eating behaviors
Disordered eating behaviors were identified through five self-reported questions regarding weekly frequency in the past 3 months of binge eating, food restriction (eating little or fasting), and purging behaviors characterized by the use of diuretics, laxatives, and self-induced vomiting for weight loss. Participants responded to the questions using a 4-point Likert scale ranging from 1 = never per week to 4 = 2 or more times per week. These questions were proposed by Hay [43], adapted from the EDE-Q [40], validated for Brazilian adolescents [45], and previously used in studies with Brazilian university students [15, 25, 46, 47]. For each question, the response options were dichotomously scored (0 = No, 1 = Yes) according to the cutoff determined by Hay [43] for the presence of disordered eating behaviors (at least once a week). The variables for the use of diuretics, laxatives, or vomiting for weight loss were recategorized into a single dichotomous variable called purging behaviors, where positivity of the variable (Yes = 1) was considered for the occurrence of one or more of these symptoms weekly in the past 3 months (Supplementary Table S1). It is important to note that disordered eating behaviors were not assessed as a single construct but rather as three separate variables: binge eating, food restriction, and purging behaviors, following the approach adopted by other researchers [15, 25, 46, 47].
Experienced weight stigma
Experienced weight stigma was assessed through the question, “Have you ever been discriminated against or harassed because of your weight?’ (No; Yes, due to excess weight; Yes, due to low weight). Single-item measures have been used to track weight discrimination trends before [48, 49] and during the COVID-19 pandemic [32, 38, 50]. This measure reflects subjective experiences of weight stigma rather than objective experiences [51]. As the construct of interest in this study was discrimination due to excess weight, the data were regrouped into No (= 0; those who answered “no” or “yes, due to low weight”) and Yes (= 1; if the participant responded “yes, due to excess weight”) (Supplementary Table S1).
Weight gain concern during the pandemic
Weight gain concern was assessed using the question, “Has concern about weight gain become prominent in your life since the start of the COVID-19 pandemic?” The question was in a forced-choice format of “yes” or “no”.
Psychological distress
Psychological distress was evaluated using the 21 items of the Depression, Anxiety, and Stress Scale (DASS-21; [52]), which has demonstrated adequate validity and reliability, including in samples of Brazilian university students [53]. The DASS-21 consists of three subscales of 7 items each (depression, anxiety, and stress), scored on a Likert scale ranging from 0 (never) to 3 (almost always). Item scores within their respective subscales are summed, resulting in scores ranging from 0 to 21. In addition, a composite score of depression, anxiety, and stress, representing overall psychological distress (DASS-total), can be calculated (range: 0–63). In the current study, only the DASS-total score was examined. Higher scores indicate greater psychological distress (Cronbach’s alpha for this sample = 0.95).
Sociodemographic and anthropometric status variables
Participants self-reported their date of birth, gender, race/skin color, monthly income, weight (kg), and height (cm). Age was calculated by subtracting the date of questionnaire response from the date of birth. All sociodemographic variables were dichotomized (see Supplementary Table S1).
Body mass index (BMI) was calculated based on weight and height data using the formula BMI = kg/m2. Anthropometric status was determined using cutoff points for underweight (< 18.5 kg/m2), normal weight (between 18.5 kg/m2 and < 25 kg/m2), overweight (between 25 kg/m2 and < 30 kg/m2), and obesity (≥ 30 kg/m2) for adults and BMI-for-age percentiles: underweight (< 3rd percentile), normal weight (≥ 3rd percentile and < 85th percentile), overweight (≥ 85th percentile and < 97th percentile), and obesity (≥ 97th percentile) for 18–19-year-old university students [51]. For analysis purposes, participants were divided into two categories: without overweight (underweight and normal weight) and with overweight (overweight and obesity).
Statistical analysis
Descriptive analyses were performed on all variables of interest, checking for normal distribution using the Kolmogorov‒Smirnov test and assessing homogeneity of variances using Levene’s test. Differences between participants without and with overweight in continuous variables were assessed using the Mann‒Whitney U test, given the nonnormality of the data, while the chi-square test was applied to categorical variables. A significant interaction was observed between anthropometric status and weight stigma regarding binge eating and purging, leading to stratified analyses for the two anthropometric status (without overweight and with overweight).
The relationship between experienced weight stigma, psychological distress, and disordered eating behaviors was investigated using structural equation modeling (SEM), with model fit assessed based on established criteria: root mean square error of approximation (RMSEA) ≤ 0.08, comparative fit index (CFI) > 0.95, Tucker‒Lewis index (TLI) > 0.90, and standardized root mean square residual (SRMR) < 0.08 [55, 56]. The robust method with the DWLS (diagonally weighted least squares) estimator was chosen to compute the standard errors of indirect effects. This method is particularly suitable for handling nonnormal variables and categorical or ordinal data. Complete case exclusion was adopted to handle missing data. The software packages R (version 3.6.3, 2020, Vienna, Austria: The R Foundation) and JASP (version 0.17.1, JASP Team University of Amsterdam, Amsterdam, The Netherlands) were used for the analyses.
Results
Sociodemographic variables of interest for the study according to anthropometric status
Out of the 2511 participants, 35.4% were classified as overweight. As described in Table 1, individuals with overweight had a higher median age (24.1; IQR = 8.7). The median BMI was 21.4 (IQR = 3.4) in the nonoverweight group and 28.2 (IQR = 4.7) in the group with overweight. Female gender, self-reported white race/ethnicity, and lower monthly family income were frequent in both studied groups. In the total sample, 33.5% of participants reported experiencing weight stigma, a frequency that was three times higher in individuals with overweight than in those without excess weight (Table 1).
Regarding the prevalence of disordered eating behaviors (DEB) between the groups, individuals with overweight had higher frequencies of binge eating (55.9% vs. 37%, p < 0.001), food restriction (32.8% vs. 19.4%, p < 0.001), and purging behaviors (9.5% vs. 3.1%, p < 0.001) than those without overweight. The frequency of weight gain concern and levels of psychological distress were also higher in individuals with overweight. Furthermore, among individuals with overweight, the prevalence of binge eating, food restriction, and purging behaviors was significantly higher among those who reported experiencing weight stigma (respectively, 40%, 23.4%, 7.4%) compared to those who did not report such experiences (respectively, 15.9%, 9.3%, 2%). Conversely, in the group without overweight, the opposite pattern of these behaviors emerged, with lower prevalence rates among individuals who reported weight stigma experiences (respectively, 8.6%, 6.9%, 1.2%) compared to those who did not report such experiences (respectively, 28.4%, 12.5%, 2%).
Structural model
The initial structural model showed a poor fit with the data. To improve the model fit, we made adjustments by removing direct paths from experienced weight stigma to food restriction and purging, as these paths were found to be nonsignificant. After the modifications, the model showed an acceptable fit with a CFI value of 0.96, TLI of 0.96, SRMR of 0.005, and RMSEA of 0.097 (90% CI: 0.086, 0.010).
In the analysis of the final model, controlling for age, sex, race/ethnicity, and income, it was observed that experienced weight stigma was directly associated with weight gain concern and higher levels of psychological distress in both individuals with and without overweight. In turn, these two constructs were directly associated with the three disordered eating behaviors: binge eating, food restriction, and purging. Figure 3 illustrates how weight gain concern and higher levels of psychological distress mediated the relationship between experienced weight stigma and disordered eating behaviors in both groups. Experienced weight stigma had a significant direct effect on binge eating only in individuals with overweight (B = 0.09, p < 0.01).
As demonstrated in Table 2, nearly all indirect effects connecting experiences of weight stigma to subsequent outcomes, including weight gain concern, psychological distress, and heightened levels of respective DEB, were found to be statistically significant. The exceptions were the pathways from weight stigma to psychological distress to food restriction and purging among individuals without overweight, as well as the pathway involving weight stigma, psychological distress, and purging in individuals with overweight. Importantly, regardless of anthropometric status, the path from weight stigma to weight gain concern, and subsequently to all three DEB, exhibited statistically significant effects.
Discussion
Based on a previous literature review, the present study is the first to investigate the prevalence of weight stigma and its relationship with disordered eating behavior in a national sample of Brazilian university students using a structural equation model. In the present study, the prevalence of experienced weight stigma was 33.5%, and the prevalence of binge eating, food restriction, and purging behaviors was 43.7%, 24.1%, and 5.4%, respectively, all of which were significantly higher (p < 0.001) in individuals with overweight compared to those without this condition. Furthermore, weight gain concern and psychological distress mediated the relationship between experienced weight stigma and disordered eating behaviors in both groups.
Although studies on the prevalence of weight stigma in Brazil are limited [33, 34], the results of this research demonstrate that a notable percentage of university students have experienced weight discrimination in the country. Compared to the international scenario, the present research corroborates previous studies conducted with adults during the same period using a similar instrument, whether in the total sample [50] or when stratified by weight status [38]. Given the sociocultural model of weight stigma [57], it is worth considering that the high frequency of weight stigma may be related to the significant concern with the appearance characteristics of Brazil [58]. It is valid to note that it is not possible to attribute these results solely to the pandemic due to the absence of published data on weight stigma with this population before the COVID-19 outbreak.
Regarding the prevalence of disordered eating behaviors stratified by weight status, the percentages identified in this study were twice as high as those found in previous research using the same instrument among university students in national [15] and international [43] settings and similar to those found for food restriction and binge eating in nonclinical samples during the pandemic [19]. Evidence suggests that the high prevalence and susceptibility to disordered eating behaviors during the pandemic may be related to a set of psychological, social, and individual factors, such as difficulty in emotion regulation [19], high BMI, and exposure to previous experiences of weight stigma [59].
The results of this study provide initial evidence supporting the model that relates weight stigma to disordered eating behaviors during the first wave of the COVID-19 pandemic. It was found that experiences of weight stigma were associated with binge eating, food restriction, and purging behaviors, and these relationships were mediated by weight gain concern and psychological distress. These findings expand and reinforce the importance of body image and psychological factors in understanding disordered eating behaviors demonstrated in previous research [16, 17], highlighting the importance of including weight gain concern in theoretical models that explain the association between weight stigma and disordered eating.
Moreover, our findings carry practical implications that extend beyond the research realm. By integrating ‘weight gain concern’ and ‘psychological distress’ into theoretical frameworks, we deepen our comprehension of the complex interplay among weight stigma, mental well-being, and eating behaviors. In practical terms, these results hold several key implications. Firstly, they reinforced the importance of interventions aimed at mitigating ‘weight gain concern’ as potentially effective in the prevention and treatment of disordered eating behaviors, such interventions that increase body acceptance and develop healthy eating skills [60], for example. In addition, they underscore the need for systematic assessments of 'weight gain concern' and 'psychological distress' in both clinical and research settings. Such assessments can identify individuals at risk and enable the tailoring of therapeutic approaches to their unique needs. Our discussion emphasizes how these findings not only expand our theoretical knowledge but also offer the potential to inform more effective and nuanced practices when addressing the intricate dynamics between weight stigma, mental health, and disordered eating behaviors.
In addition, although the explanatory models are similar in both weight groups, weight stigma had a significant direct relationship with disordered eating behaviors only in individuals with higher body weight. In this regard, the data presented in this study may support the weight-based stigma/excess weight cyclical model (COBWEBS), which proposes that the impact of weight stigma on overeating, particularly in individuals with overweight, occurs as a response to the stress resulting from weight-related stigmatizing experiences [61].
There are important theoretical and methodological considerations to interpret the results. First, individuals with higher body weight are considered marginalized identities, and the effects of weight stigma on disordered eating behaviors are compounded by other consequences in their lives. In this sense, during the pandemic, in addition to dealing with the inherent changes in the context, individuals with obesity faced additional concerns such as the lack of adequate equipment and structures to assist them in case of illness [62].
Furthermore, since the experienced weight stigma in this study corresponded to retrospective data, the reported stigma experiences among individuals without overweight/obesity may be retrospective self-reports of previous overweight or obesity [36]. In addition, the relationship between weight stigma and disordered eating behaviors in individuals with overweight may have been underestimated due to the low variability of weight stigma experiences among the participants [63]. It is also important to acknowledge that while the RMSEA value did not meet the predefined criteria for adequacy, it is well-established in the literature that model adequacy should be assessed by considering a combination of fit indices [64]. This underscores the importance of evaluating the overall fit of the structural model, recognizing that the RMSEA, being sensitive to deviations from normality in the data [65], may indicate less favorable fit outcomes in such cases. Therefore, caution should be exercised in interpreting the results.
Finally, stratifying the sample by weight status contributed to demonstrating that the frequencies of the outcomes according to weight stigma experiences differed between individuals with and without overweight, which may suggest that while the relationships between variables can be explained by similar models, the distributions manifest themselves differently among the groups and need to be understood in their singularities.
Strengths and limitations
The strengths of the study include the use of a large sample of university students, which allowed for robust statistical analysis controlled for sociodemographic variables. The use of a population sample, rather than clinical samples, enables the evaluation of factors associated with disordered eating behaviors in a broader group of healthy individuals. Furthermore, students are a population susceptible to poorer mental health indicators, especially during the pandemic, which reinforces the importance of understanding the implications of psychological and sociocultural factors on disordered eating behaviors in this pandemic scenario. The relationship between constructs in the field of nutrition and mental health contributes to supporting the importance of multidisciplinary healthcare teams in the care of this population, considering the challenge of implementing strategies that synergistically address obesity and disordered eating behaviors in low-income countries [66].
Despite important contributions to the field of disordered eating, our study has some limitations. First, all stages of the study were conducted online due to pandemic restrictions, which may introduce information bias. Second, experiences of weight stigma were assessed retrospectively, which increases the possibility of recall bias. Third, weight stigma was assessed using dichotomous (yes/no) questions. Although brief tools are commonly used in epidemiological studies in the field, this type of item can lead to measurement errors. Finally, the cross-sectional nature of the study limits the inference of causal relationships between variables.
This study has several implications for future research. The high prevalence of experiences of weight stigma and its association with disordered eating behaviors in Brazil signals the need to pay attention to this indicator as a factor associated with such outcomes. In this regard, further research is needed to examine the pathways through which weight discrimination impacts disordered eating behaviors, as the assessment of mediators in this process can help identify individuals who are more vulnerable to the effects of weight stigma on eating behavior. In addition, conducting longitudinal studies can provide evidence about the direction of the association and assist in the development of programs aimed at the prevention and management of disordered eating behaviors in individuals with or without weigh excess.
What is already known about this subject?
High frequencies of experienced weight stigma and disordered eating behaviors have been observed among university students, as well as the association between these variables. During the pandemic, few studies have assessed the relationship between weight stigma and disordered eating behaviors, and no studies on this topic in the Brazilian context have been conducted.
What does this study add?
This is the only epidemiological study that provided the prevalence of experienced weight stigma according to weight status in a national sample of Brazilian university students during the COVID-19 pandemic. The study found a high prevalence of experiences of weight stigma, and all investigated disordered eating behaviors during the pandemic (binge eating, food restriction, and purging behaviors), which were notably higher in individuals with overweight. The relationship between the variables was mediated by weight gain concern and psychological distress, highlighting the importance of considering these constructs in the targeted development of prevention and control strategies for disordered eating behaviors in the future.
Conclusion
The present study identified a high prevalence of experienced weight stigma and disordered eating behaviors in the early stages of the pandemic, particularly in individuals with overweight. As hypothesized, weight gain concern and psychological distress mediated the relationship between experiences of weight stigma and disordered eating behaviors during the first wave of the COVID-19 pandemic. The identification of these issues can be useful for the development of targeted strategies for the prevention and management of disordered eating behaviors.
Data availability
The datasets generated and/or analyzed during the current study are available upon request from the corresponding author.
References
Flint SW (2020) Stigmatizing media portrayal of obesity during the coronavirus (COVID-19) pandemic. Front Psychol 11:10–12
Pearl RL, Schulte EM (2021) Weight bias during the COVID-19 pandemic. Curr Obes Rep 10:181–190
Brown A, Flint SW, Kalea AZ, O’Kane M, Williams S, Batterham RL (2021) Negative impact of the first COVID-19 lockdown upon health-related behaviours and psychological wellbeing in people living with severe and complex obesity in the UK. EClinicalMedicine 34:100796–100796
Lessard LM, Puhl RM (2021) Adolescents’ exposure to and experiences of weight stigma during the COVID-19 pandemic. J Pediatric Psychol 46:950
Emmer C, Bosnjak M, Mata J (2020) The association between weight stigma and mental health: a meta-analysis. Obes Rev 21:1–13
Depierre JA, Puhl RM (2012) Experiences of weight stigmatization: a review of self-report assessment measures. Obes Facts 5:897–918
Mason TB, Mozdzierz P, Wang S, Smith KE (2021) Discrimination and eating disorder psychopathology: a meta-analysis. Behav Ther 52:406–417
Menzel JE, Schaefer LM, Burke NL, Mayhew LL, Brannick MT, Thompson JK (2010) Appearance-related teasing, body dissatisfaction, and disordered eating: a meta-analysis. Body Image 7:261–270
Papadopoulos S, Brennan L (2015) Correlates of weight stigma in adults with overweight and obesity: a systematic literature review. Obesity 23:1743–1760
Vartanian LR, Porter AM (2016) Weight stigma and eating behavior: a review of the literature. Appetite 102:3–14
Wu YK, Berry DC (2018) Impact of weight stigma on physiological and psychological health outcomes for overweight and obese adults: a systematic review. J Adv Nurs 74:1030–1042
American DA (2006) Position of the American Dietetic Association: nutrition intervention in the treatment of anorexia nervosa, bulimia nervosa, and other eating disorders. J Am Diet Assoc 106:2073–2082
Vijayalakshmi P, Thimmaiah R, Gandhi S, BadaMath S (2018) Eating attitudes, weight control behaviors, body image satisfaction and depression level among indian medical and nursing undergraduate students. Community Ment Health J 54:1266–1273
Barrack MT, West J, Christopher M, Pham-Vera A-M (2019) Disordered eating among a diverse sample of first-year college students. J Am Coll Nutr 38:141–148
de Matos AP, Rodrigues PRM, Fonseca LB, Ferreira MG, Muraro AP (2021) Prevalence of disordered eating behaviors and associated factors in Brazilian university students. Nutr Health 27(2):231–241
O’Brien KS, Latner JD, Puhl RM, Vartanian LR, Giles C, Griva K, Carter A (2016) The relationship between weight stigma and eating behavior is explained by weight bias internalization and psychological distress. Appetite 102:70–76
Romano KA, Heron KE, Henson JM (2021) Examining associations among weight stigma, weight bias internalization, body dissatisfaction, and eating disorder symptoms: does weight status matter? Body Image 37:38–49
de Macêdo PFC, Nepomuceno CMM, dos Santos NS, Queiroz VAO, Pereira EM, Leal LC, Santos LAS, Nascimento LF, Martins PC, de Santana MLP (2022) Weight stigma in the COVID-19 pandemic: a scoping review. J Eat Disord 10:44–44
Linardon J, Messer M, Rodgers RF, Fuller-Tyszkiewicz M (2022) A systematic scoping review of research on COVID-19 impacts on eating disorders: A critical appraisal of the evidence and recommendations for the field. Int J Eat Disord 55(1):3–38. https://doi.org/10.1002/eat.23640
Monteleone AM, Cascino G, Barone E, Carfagno M, Monteleone P (2021) COVID-19 pandemic and eating disorders: what can we learn about psychopathology and treatment? A systematic review. Curr Psychiatry Reports 23:83–83
Sideli L, Lo CG, Bonfanti RC, Borsarini B, Fortunato L, Sechi C, Micali N (2021) Effects of COVID-19 lockdown on eating disorders and obesity: a systematic review and meta-analysis. Eur Eat Disord Rev 29:826–841
Thompson JK, Heinberg LJ, Altabe M, Tantleff-Dunn S (1999) Exacting beauty: theory, assessment, and treatment of body image disturbance. American Psychological Association, Washington
Alvarenga MDS, Lourenço BH, Philippi ST, Scagliusi FB (2013) Disordered eating among Brazilian female college students. Cad Saude Publica 29:879–888
Ferreira JE, de Souza PR, da Costa RS, Sichieri R, da Veiga GV (2013) Disordered eating behaviors in adolescents and adults living in the same household in metropolitan area of Rio de Janeiro, Brazil. Psychiatry Res 210(2):612–617
Carvalho PHB, Alvarenga MDS, Ferreira MEC (2017) An etiological model of disordered eating behaviors among Brazilian women. Appetite 116:164–172
Obeid N, Flament MF, Buchholz A, Henderson KA, Schubert N, Tasca G, Thai H, Goldfield G (2022) Examining shared pathways for eating disorders and obesity in a community sample of adolescents: the REAL study. Front Psychol 13:805596
Rodgers RF, Lombardo C, Cerolini S, Franko DL, Omori M, Fuller-Tyszkiewicz M, Linardon J, Courtet P, Guillaume S (2020) The impact of the COVID-19 pandemic on eating disorder risk and symptoms. Int J Eat Disord 53:1166–1170
Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, Demyttenaere K, Ebert DD, Green JG, Hasking P, Murray E, Nock MK, Pinder-Amaker S, Sampson NA, Stein DJ, Vilagut G, Zaslavsky AM, Kessler RC (2018) WHO World Mental Health Surveys International College Student Project: prevalence and distribution of mental disorders. J Abnorm Psychol 127:623–638
Hooper L, Puhl R, Eisenberg ME, Crow S, Neumark-Sztainer D (2021) Weight teasing experienced during adolescence and young adulthood: cross-sectional and longitudinal associations with disordered eating behaviors in an ethnically/racially and socioeconomically diverse sample. Int J Eat Disord 54:1449–1462
Lessard LM, Puhl RM, Himmelstein MS, Pearl RL, Foster GD (2021) Eating and exercise-related correlates of weight stigma: a multinational investigation. Obesity 29:966–970
Pearl RL, Puhl RM, Lessard LM, Himmelstein MS, Foster GD (2021) Prevalence and correlates of weight bias internalization in weight management: a multinational study. SSM Popul Health 13:100755
Sutin AR, Stephan Y, Luchetti M, Aschwanden D, Strickhouser JE, Lee JH, Sesker AA, Terracciano A (2021) BMI, weight discrimination, and the trajectory of distress and well-being across the coronavirus pandemic. Obesity 29:38–45
Leme ACB, Philippi ST (2013) Teasing and weight-control behaviors in adolescent girls. Revista Paulista de Pediatria 31:431–436
Philippi ST, Leme ACB (2018) Weight-teasing: does body dissatisfaction mediate weight-control behaviors of Brazilian adolescent girls from low-income communities? Cadernos de saude publica 34
Cunha CdM, Pereira EM, Souto MCR, de Sá LB, da Silva HBM, de Brito E, de Santana MLP (2023) Factors associated with body image dissatisfaction in a Brazilian university sample during the COVID-19 pandemic. Front Educ 8:1044727. https://doi.org/10.3389/feduc.2023.1044727
Spahlholz J, Baer N, König HH, Riedel-Heller SG, Luck-Sikorski C (2016) Obesity and discrimination—a systematic review and meta-analysis of observational studies. Obes Rev 17:43–55
Pearl RL (2020) Weight Stigma and the “Quarantine-15.” Obesity 28:1180–1181
Sutin AR, Robinson E, Daly M, Gerend MA, Stephan Y, Luchetti M, Aschwanden D, Strickhouser JE, Lee JH, Sesker AA, Terracciano A (2020) BMI, weight discrimination, and psychological, behavioral, and interpersonal responses to the coronavirus pandemic. Obesity 28:1590–1594
Brasil. Ministério da Saúde. Secretaria Executiva do Conselho Nacional de Saúde. Comissão Nacional de Ética em Pesquisa. (2020). Orientações para condução de pesquisas e atividade dos CEP durante a pandemia provocada pelo Coronavírus SARS-COV-2 (COVID-19). Brasília. URL: http://conselho.saude.gov.br/normativasconep?view=default
Santana MLP, Oliveira AM, Cunha CM, Araújo MPN, Queiroz VAO, Martins PC, Costa PRF, Nepomuceno CM, Barroso RRF, Fonseca NSS, Oliveira LPM, Machado MEP, Machado ML, Santos SMC, Silva KBB, Silva HBM, Macêdo PFC, Carvalho MV, Pereira JM (2021) Aspectos metodológicos e desafios da Coorte On-line Comportamento Alimentar e Saúde Mental (COCASa) de docentes e discentes universitários durante a pandemia da COVID-19. Res Soc Dev 10:e148101724258–e148101724258
Sobel ME (1982) Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol 13:290–312
Bulus M, Polat S (2023) pwrss: Statistical Power and Sample Size Calculation Tools (Version 0.3.1) [Software]. Retrieved from Comprehensive R Archive Network (CRAN) https://CRAN.R-project.org/package=pwrss
Hay P (1998) The epidemiology of eating disorder behaviors: an Australian community-based survey. Int J Eat Disord 23:371–382
Fairburn CG, Cooper Z, O’Connor M (1993) The eating disorder examination. Int J Eat Disord 6:1–8
Ferreira JEDS, Da Veiga GV (2008) Test-retest reliability of a simplified questionnaire for screening adolescents with risk behaviors for eating disorders in epidemiologic studies. Rev Bras Epidemiol 11:393–401
Carvalho PHB, Ferreira MEC (2020) Disordered eating and body change behaviours: support for the Tripartite Influence Model among Brazilian male university students Comportamentos de risco para transtornos alimentares e de mudança corporal: suporte ao Modelo dos Três Fatores para adultos. Ciencia & Saúde Coletiva 25:4485–4496
Ferreira C, Pinto-Gouveia J, Duarte C (2013) Physical appearance as a measure of social ranking: the role of a new scale to understand the relationship between weight and dieting. Clin Psychol Psychother 20:55–66
Andreyeva T, Puhl RM, Brownell KD (2008) Changes in perceived weight discrimination among Americans, 1995–1996 through 2004–2006. Obesity 16:1129–1134
Sutin AR, Stephan Y, Luchetti M, Terracciano A (2014) Perceived weight discrimination and C-reactive protein. Obesity 22:1959–1961
Puhl RM, Lessard LM, Larson N, Eisenberg ME, Neumark-Stzainer D (2020) Weight stigma as a predictor of distress and maladaptive eating behaviors during covid-19: longitudinal findings from the eat study. Ann Behav Med 54:738–746
Himmelstein MS, Puhl RM, Quinn DM (2018) Weight stigma in men: what, when, and by whom? Obesity 26:968–976
Lovibond PF, Lovibond SH (1995) The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 33:335–343
Martins BG, Da Silva WR, Maroco J, Campos JADB (2019) Depression, anxiety, and stress scale: psychometric properties and affectivity prevalence. J Bras Psiquiatr 68:32–41
World Health O (2000) Obesity: preventing and managing the global epidemic. Report of a World Health Organization Consultation. Geneva: WHO; 2000. WHO Obesity Technical Report Series
Hu L-t, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidisciplinary J 6(1):1–55
Schumacker RE, Lomax RG (2004) A beginner’s guide to structural equation modeling. Psychology press
Nutter S, Russell-Mayhew S, Saunders JF (2021) Towards a sociocultural model of weight stigma. Eat Weight Disord-Studies on Anorexia, Bulimia and Obesity 26:999–1005
Goldenberg M (2010) The Body as Capital. Understanding Brazilian Culture. VIBRANT-Vibrant Virtual Braz Anthropol 7:220–238
Schneider J, Pegram G, Gibson B, Talamonti D, Tinoco A, Craddock N, Matheson E, Forshaw M (2023) A mixed-studies systematic review of the experiences of body image, disordered eating, and eating disorders during the COVID-19 pandemic. Int J Eat Disord 56:26–67
Wilson RE, Marshall RD, Murakami JM, Latner JD (2020) Brief non-dieting intervention increases intuitive eating and reduces dieting intention, body image dissatisfaction, and anti-fat attitudes: a randomized controlled trial. Appetite 148:104556
Tomiyama AJ (2014) Weight stigma is stressful. A review of evidence for the Cyclic Obesity/Weight-Based Stigma model. Appetite 82:8–15
Pausé C, Parker G, Gray L (2021) Resisting the problematisation of fatness in COVID-19: in pursuit of health justice. Int J Disaster Risk Reduction 54:102021
Goldschmidt AB, Wall MM, Loth KA, Neumark-Sztainer D (2015) Risk factors for disordered eating in overweight adolescents and young adults. J Pediatr Psychol 40:1048–1055
Schermelleh-Engel K, Moosbrugger H, Müller H (2003) Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res Online 8(2):23–74
Xia Y, Yang Y (2019) RMSEA, CFI, and TLI in structural equation modeling with ordered categorical data: the story they tell depends on the estimation methods. Behav Res Methods 51:409–428
Leme ACB, Philippi ST, Thompson D, Nicklas T, Baranowski T (2019) “Healthy Habits, Healthy Girls—Brazil”: an obesity prevention program with added focus on eating disorders. Eat Weight Disord-Studies on Anorexia, Bulimia and Obesity 24:107–119
Funding
This study was conducted with the support of the Coordination for the Improvement of Higher Education Personnel—Brazil (CAPES)—Funding Code 001.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. Data collection and material preparation were performed by all authors. The analysis was conducted by PFCdM and EB. The initial draft of the manuscript was written by PFCdM, and all authors provided comments on earlier versions of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is an observational study. The Research Ethics Committee of the Federal University of Bahia approved all protocols used by the COCASA cohort. Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Macêdo, P.F.C., Brito, E., de Magalhães Cunha, C. et al. Weight stigma and disordered eating behaviors during the COVID-19 pandemic: the mediating role of weight gain concern and psychological distress. Eat Weight Disord 28, 78 (2023). https://doi.org/10.1007/s40519-023-01608-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40519-023-01608-6