Abstract
Purpose
As a maladaptive disordered eating behavior, binge eating (BE) onset has been reported in children as young as eight years old and is linked with a range of negative psychological consequences. However, previous neuroimaging research of BE has mainly focused on adults in clinical conditions, and little is known about the potential neurostructural and neurofunctional bases of BE in healthy children.
Methods
In this study, we examined these issues in 76 primary school students (mean age = 9.86 years) using voxel-based morphometry and resting-state functional connectivity (rsFC) approaches.
Results
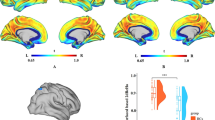
After controlling for age, sex, and total intracranial volume/head motion, we observed that higher levels of BE were correlated with greater gray matter volumes (GMV) in the left fusiform and right insula and weaker rsFC between the right insula and following three regions: right orbital frontal cortex, left cingulate gyrus, and left superior frontal gyrus. No significant associations were observed between BE and regional white matter volume. Significant sex differences were found only in the relationship between BE and GMV in the left fusiform. Furthermore, the GMV- and rsFC-based predictive models (a machine-learning method) achieved significant correlations between the actual and predicted BE values, demonstrating the robustness of our findings.
Conclusion
The present study provides novel evidence for the brain structural and functional substrates of children’s BE, and further reveals that the weakened communication between core regions associated with negative affectivity, reward responsivity, and executive function is strongly related to dysregulated eating.
Level of evidence
Level V, descriptive study.


Similar content being viewed by others
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Publishing, Washington, DC
Davis HA, Ortiz AML, Smith GT (2018) The occurrence and covariation of binge eating and compensatory behaviors across early to mid-adolescence. J Pediatr Psychol 43(4):402–412. https://doi.org/10.1093/jpepsy/jsx113
Tanofsky-Kraff M (2008) Binge eating among children and adolescents. Handbook of childhood and adolescent obesity. Springer, Boston, MA, pp 43–59
He J, Cai Z, Fan X (2017) Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: an exploratory meta-analysis. Int J Eat Disord 50(2):91–103. https://doi.org/10.1002/eat.22661
Wellman JD, Araiza AM, Solano C, Berru E (2019) Sex differences in the relationships among weight stigma, depression, and binge eating. Appetite 133:166–173. https://doi.org/10.1016/j.appet.2018.10.029
Bentley C, Gratwick-Sarll K, Harrison C, Mond J (2015) Sex differences in psychosocial impairment associated with eating disorder features in adolescents: a school based study. Int J Eat Disord 48(6):633–640. https://doi.org/10.1002/eat.22396
Tanofsky-Kraff M, Faden D, Yanovski SZ, Wilfley DE, Yanovski JA (2005) The perceived onset of dieting and loss of control eating behaviors in overweight children. Int J Eat Disord 38(2):112–122. https://doi.org/10.1002/eat.20158
Kotler LA, Cohen P, Davies M, Pine DS, Walsh BT (2001) Longitudinal relationships between childhood, adolescent, and adult eating disorders. J Am Acad Child Adolesc Psychiatry 40(12):1434–1440. https://doi.org/10.1097/00004583-200112000-00014
Smith KE, Luo S, Mason TB (2021) A systematic review of neural correlates of dysregulated eating associated with obesity risk in youth. Neurosci Biobehav Rev 124:245–266. https://doi.org/10.1016/j.neubiorev.2021.02.013
Estella NM, Sanches LG, Maranhão MF, Hoexter MQ, Schmidt U, Campbell IC, Claudino AM (2020) Brain white matter microstructure in obese women with binge eating disorder. Eur Eat Disord Rev 28(5):525–535. https://doi.org/10.1002/erv.2758
Kessler RM, Hutson PH, Herman BK, Potenza MN (2016) The neurobiological basis of binge-eating disorder. Neurosci Biobehav Rev 63:223–238. https://doi.org/10.1016/j.neubiorev.2016.01.013
Mele G, Alfano V, Cotugno A, Longarzo M (2020) A broad-spectrum review on multimodal neuroimaging in bulimia nervosa and binge eating disorder. Appetite 151:104712. https://doi.org/10.1016/j.appet.2020.104712
Kober H, Boswell RG (2018) Potential psychological & neural mechanisms in binge eating disorder: implications for treatment. Clin Psychol Rev 60:32–44. https://doi.org/10.1016/j.cpr.2017.12.004
Cuthbert BN (2015) Research domain criteria: toward future psychiatric nosologies. Dialogues Clin Neurosci 17(1):89–97. https://doi.org/10.31887/DCNS.2015.17.1/bcuthbert
Abdo N, Boyd E, Baboumian S, Pantazatos SP, Geliebter A (2020) Relationship between binge eating and associated eating behaviors with subcortical brain volumes and cortical thickness. J Affect Disord 274:1201–1205. https://doi.org/10.1016/j.jad.2019.10.032
Hagan KE, Bohon C (2021) Subcortical brain volume and cortical thickness in adolescent girls and women with binge eating. Int J Eat Disord 54(8):1527–1536. https://doi.org/10.1002/eat.23563
Oliva R, Morys F, Horstmann A, Castiello U, Begliomini C (2020) Characterizing impulsivity and resting-state functional connectivity in normal-weight binge eaters. Int J Eat Disord 53(3):478–488. https://doi.org/10.1002/eat.23212
Oliva R, Morys F, Horstmann A, Castiello U, Begliomini C (2019) The impulsive brain: neural underpinnings of binge eating behavior in normal-weight adults. Appetite 136:33–49. https://doi.org/10.1016/j.appet.2018.12.043
Zhang Z, Robinson L, Jia T, Quinlan EB, Tay N, Chu C, Desrivières S (2021) Development of disordered eating behaviors and comorbid depressive symptoms in adolescence: neural and psychopathological predictors. Biol Psychiat 90(12):853–862. https://doi.org/10.1016/j.biopsych.2020.06.003
Vannucci A, Tanofsky-Kraff M, Ranzenhofer LM, Kelly NR, Hannallah LM, Pickworth CK, Yanovski JA (2014) Puberty and the manifestations of loss of control eating in children and adolescents. Int J Eat Disord 47(7):738–747. https://doi.org/10.1002/eat.22305
Spear HJ, Kulbok P (2004) Autonomy and adolescence: a concept analysis. Public Health Nurs 21(2):144–152. https://doi.org/10.1111/j.0737-1209.2004.021208.x
Shapiro A, Johnson SL, Sutton B, Legget KT, Dabelea D, Tregellas JR (2019) Eating in the absence of hunger in young children is related to brain reward network hyperactivity and reduced functional connectivity in executive control networks. Pediatr Obes 14(6):e12502. https://doi.org/10.1111/ijpo.12502
Maayan L, Hoogendoorn C, Sweat V, Convit A (2011) Disinhibited eating in obese adolescents is associated with orbitofrontal volume reductions and executive dysfunction. Obesity 19(7):1382–1387. https://doi.org/10.1038/oby.2011.15
Boos HB, Aleman A, Cahn W, Hulshoff Pol H, Kahn RS (2007) Brain volumes in relatives of patients with schizophrenia: a meta-analysis. Arch Gen Psychiatry 64(3):297–304. https://doi.org/10.1001/archpsyc.64.3.297
Wagner G, Koch K, Schachtzabel C, Schultz CC, Sauer H, Schlösser RG (2011) Structural brain alterations in patients with major depressive disorder and high risk for suicide: evidence for a distinct neurobiological entity? Neuroimage 54(2):1607–1614. https://doi.org/10.1016/j.neuroimage.2010.08.082
Suñol M, Contreras-Rodríguez O, Macià D, Martínez-Vilavella G, Martínez-Zalacaín I, Subirà M, Soriano-Mas C (2018) Brain structural correlates of subclinical obsessive-compulsive symptoms in healthy children. J Am Acad Child Adolesc Psychiatry 57(1):41–47. https://doi.org/10.1016/j.jaac.2017.10.016
Eklund K, Paavonen EJ, Almqvist F (2005) Factor structure of the eating disorder inventory-C. Int J Eat Disord 37(4):330–341. https://doi.org/10.1002/eat.20097
Wiklund CA, Kuja-Halkola R, Thornton LM, Hübel C, Leppä V, Bulik CM (2019) Prolonged constipation and diarrhea in childhood and disordered eating in adolescence. J Psychosom Res 126:109797. https://doi.org/10.1016/j.jpsychores.2019.109797
Veldsman M, Zamboni G, Butler C, Ahmed S (2019) Attention network dysfunction underlies memory impairment in posterior cortical atrophy. Neuroimage 22:101773. https://doi.org/10.1016/j.nicl.2019.101773
Hahm S, Lotze M, Domin M, Schmidt S (2019) The association of health-related quality of life and cerebral gray matter volume in the context of aging: a voxel-based morphometry study with a general population sample. Neuroimage 191:470–480. https://doi.org/10.1016/j.neuroimage.2019.02.035
Lv Q, Lv Q, Yin D, Zhang C, Sun B, Voon V, Wang Z (2021) Neuroanatomical substrates and predictors of response to capsulotomy in intractable obsessive-compulsive disorder. Biol Psychiatry 6(1):29–38. https://doi.org/10.1016/j.bpsc.2020.05.005
Ashburner J (2007) A fast diffeomorphic image registration algorithm. Neuroimage 38(1):95–113. https://doi.org/10.1016/j.neuroimage.2007.07.007
Friston KJ, Williams S, Howard R, Frackowiak RS, Turner R (1996) Movement-related effects in fMRI time-series. Magn Reson Med 35(3):346–355. https://doi.org/10.1002/mrm.1910350312
Hallquist MN, Hwang K, Luna B (2013) The nuisance of nuisance regression: spectral misspecification in a common approach to resting-state fMRI preprocessing reintroduces noise and obscures functional connectivity. Neuroimage 82:208–225. https://doi.org/10.1016/j.neuroimage.2013.05.116
Ridgway GR, Omar R, Ourselin S, Hill DL, Warren JD, Fox NC (2009) Issues with threshold masking in voxel-based morphometry of atrophied brains. Neuroimage 44(1):99–111. https://doi.org/10.1016/j.neuroimage.2008.08.045
Mao Y, Zuo XN, Ding C, Qiu J (2020) OFC and its connectivity with amygdala as predictors for future social anxiety in adolescents. Dev Cogn Neurosci 44:100804. https://doi.org/10.1016/j.dcn.2020.100804
Supekar K, Swigart AG, Tenison C, Jolles DD, Rosenberg-Lee M, Fuchs L, Menon V (2013) Neural predictors of individual differences in response to math tutoring in primary-grade school children. Proc Natl Acad Sci USA 110(20):8230–8235. https://doi.org/10.1073/pnas.1222154110
Wang Z, Goerlich KS, Ai H, Aleman A, Luo YJ, Xu P (2021) Connectome-based predictive modeling of individual anxiety. Cereb Cortex 31(6):3006–3020. https://doi.org/10.1093/cercor/bhaa407
Marcoulides GA, Hershberger SL (1997) Multivariate statistical methods: a first course. Lawrence Erlbaum Associates, Mahwah, NJ
Wang S, Zhou M, Chen T, Yang X, Chen G, Wang M, Gong Q (2017) Grit and the brain: spontaneous activity of the dorsomedial prefrontal cortex mediates the relationship between the trait grit and academic performance. Soc Cognit Affect Neurosci 12(3):452–460. https://doi.org/10.1093/scan/nsw145
Wang S, Zhao Y, Cheng B, Wang X, Yang X, Chen T, Gong Q (2018) The optimistic brain: trait optimism mediates the influence of resting-state brain activity and connectivity on anxiety in late adolescence. Hum Brain Mapp 39(10):3943–3955. https://doi.org/10.1002/hbm.24222
Steward T, Menchon JM, Jiménez-Murcia S, Soriano-Mas C, Fernandez-Aranda F (2018) Neural network alterations across eating disorders: a narrative review of fMRI studies. Curr Neuropharmacol 16(8):1150–1163. https://doi.org/10.2174/1570159X15666171017111532
Gaudio S, Quattrocchi CC (2012) Neural basis of a multidimensional model of body image distortion in anorexia nervosa. Neurosci Biobehav Rev 36(8):1839–1847. https://doi.org/10.1016/j.neubiorev.2012.05.003
De Coen J, Verbeken S, Goossens L (2021) Media influence components as predictors of children’s body image and eating problems: a longitudinal study of boys and girls during middle childhood. Body Image 37:204–213. https://doi.org/10.1016/j.bodyim.2021.03.001
Gordon KH, Holm-Denoma JM, Troop-Gordon W, Sand E (2012) Rumination and body dissatisfaction interact to predict concurrent binge eating. Body Image 9(3):352–357. https://doi.org/10.1016/j.bodyim.2012.04.001
Craven MP, Fekete EM (2019) Weight-related shame and guilt, intuitive eating, and binge eating in female college students. Eat Behav 33:44–48. https://doi.org/10.1016/j.eatbeh.2019.03.002
Finch JE, Palumbo IM, Tobin KE, Latzman RD (2021) Structural brain correlates of eating pathology symptom dimensions: a systematic review. Psychiatry Res 317:111379. https://doi.org/10.1016/j.pscychresns.2021.111379
Giuliani NR, Drabant EM, Bhatnagar R, Gross JJ (2011) Emotion regulation and brain plasticity: expressive suppression use predicts anterior insula volume. Neuroimage 58(1):10–15. https://doi.org/10.1016/j.neuroimage.2011.06.028
Li W, Yang P, Ngetich RK, Zhang J, Jin Z, Li L (2021) Differential involvement of frontoparietal network and insula cortex in emotion regulation. Neuropsychologia 161:107991. https://doi.org/10.1016/j.neuropsychologia.2021.107991
Laird KT, Siddarth P, Krause-Sorio B, Kilpatrick L, Milillo M, Aguilar Y, Lavretsky H (2019) Anxiety symptoms are associated with smaller insular and orbitofrontal cortex volumes in late-life depression. J Affect Disord 256:282–287. https://doi.org/10.1016/j.jad.2019.05.066
Wu J, Tong H, Liu Z, Tao J, Chen L, Chan C, Lee T (2021) Neurobiological effects of perceived stress are different between adolescents and middle-aged adults. Brain Imaging Behav 15(2):846–854. https://doi.org/10.1007/s11682-020-00294-7
Tanofsky-Kraff M, Schvey NA, Grilo CM (2020) A developmental framework of binge-eating disorder based on pediatric loss of control eating. Am Psychol 75(2):189–203. https://doi.org/10.1037/amp0000592
Murray SB, Duval CJ, Balkchyan AA, Cabeen RP, Nagata JM, Toga AW, Jann K (2022) Regional gray matter abnormalities in pre-adolescent binge eating disorder: a voxel-based morphometry study. Psychiatry Res 310:114473. https://doi.org/10.1016/j.psychres.2022.114473
Monteleone AM, Castellini G, Volpe U, Ricca V, Lelli L, Monteleone P, Maj M (2018) Neuroendocrinology and brain imaging of reward in eating disorders: A possible key to the treatment of anorexia nervosa and bulimia nervosa. Prog Neuropsychopharmacol Biol Psychiatry 80(Pt B):132–142. https://doi.org/10.1016/j.pnpbp.2017.02.020
Farr OM, Li CR, Mantzoros CS (2016) Central nervous system regulation of eating: insights from human brain imaging. Metabolism 65(5):699–713. https://doi.org/10.1016/j.metabol.2016.02.002
Smith DG, Robbins TW (2013) The neurobiological underpinnings of obesity and binge eating: a rationale for adopting the food addiction model. Biol Psychiat 73(9):804–810. https://doi.org/10.1016/j.biopsych.2012.08.026
Adise S, Geier CF, Roberts NJ, White CN, Keller KL (2019) Food or money? Children’s brains respond differently to rewards regardless of weight status. Pediatr Obes 14(2):e12469. https://doi.org/10.1111/ijpo.12469
Chen X, Gao X, Qin J, Wang C, Xiao M, Tian Y, Chen H (2021) Resting-state functional network connectivity underlying eating disorder symptoms in healthy young adults. Neuroimage 30:102671. https://doi.org/10.1016/j.nicl.2021.102671
Goldschmidt AB, Dickstein DP, MacNamara AE, Phan KL, O’Brien S, Le Grange D, Keedy S (2018) A pilot study of neural correlates of loss of control eating in children with overweight/obesity: probing intermittent access to food as a means of eliciting disinhibited eating. J Pediatr Psychol 43:846–855. https://doi.org/10.1093/jpepsy/jsy009
Bright MG, Murphy K (2015) Is fMRI “noise” really noise? Resting state nuisance regressors remove variance with network structure. Neuroimage 114:158–169. https://doi.org/10.1016/j.neuroimage.2015.03.070
Barch DM, Albaugh MD, Avenevoli S, Chang L, Clark DB, Glantz MD, Sher KJ (2018) Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: rationale and description. Dev Cogn Neurosci 32:55–66. https://doi.org/10.1016/j.dcn.2017.10.010
Dieleman N, Koek HL, Hendrikse J (2017) Short-term mechanisms influencing volumetric brain dynamics. Neuroimage 16:507–513. https://doi.org/10.1016/j.nicl.2017.09.002
Liu Y, Gao JH, Liu HL, Fox PT (2000) The temporal response of the brain after eating revealed by functional MRI. Nature 405(6790):1058–1062. https://doi.org/10.1038/35016590
Bullmore E, Sporns O (2009) Complex brain networks: graph theoretical analysis of structural and functional systems. Nat Rev Neurosci 10(3):186–198. https://doi.org/10.1038/nrn2575
Smith R, Sanova A, Alkozei A, Lane RD, Killgore W (2018) Higher levels of trait emotional awareness are associated with more efficient global information integration throughout the brain: a graph-theoretic analysis of resting state functional connectivity. Soc Cognit Affect Neurosci 13(7):665–675. https://doi.org/10.1093/scan/nsy047
Acknowledgements
This study was funded by National Natural Science Foundation of China (No. 31771237; No. 32271087), the Fundamental Research Funds for the Central Universities (No. SWU1709106), and Innovative Research Project for Postgraduate Student of Chongqing (No. CYB21083). The authors would like to express their gratitude to all associated research assistants for their help with participant recruitment and data collection and thank Chaoyang Primary School and Zhongshan Road Primary School for their support of this research.
Funding
This study was funded by National Natural Science Foundation of China (No. 31771237; No. 32271087), the Fundamental Research Funds for the Central Universities (No. SWU1709106), and Innovative Research Project for Postgraduate Student of Chongqing (No. CYB21083).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The research protocol was reviewed for compliance with the standards for the ethical treatment of human participants and approved by the Ethical Committee for Scientific Research at the university with which the authors are affiliated.
Informed consent
All participants and their parents/legal guardians provided written informed consents to participate in the study.
Research involving human participants
All ethical guidelines for human subjects’ research were followed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, X., Li, W., Qin, J. et al. Gray matter volume and functional connectivity underlying binge eating in healthy children. Eat Weight Disord 27, 3469–3478 (2022). https://doi.org/10.1007/s40519-022-01483-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-022-01483-7