Abstract
Purpose of review
Major depressive disorder is a prevalent psychiatric illness associated with significant morbidity, mortality, and economic burden worldwide. Despite the widespread use of antidepressants, remission rates among those treated with antidepressants remain low. Opportunities to personalize medication choices and doses and optimize clinical outcomes using pharmacogenomic testing have been evaluated.
Recent findings
Several prospective clinical trials and a recent meta-analysis have evaluated the impact of PGx-guided prescribing compared to treatment as usual and found no difference in clinical outcomes for patients with MDD.
Summary
We performed a systematic review of all prospective trials evaluating the effect of pharmacogenomic-guided prescribing on clinical outcomes of patients being treated with antidepressants for major depressive disorder. A literature search was performed using PubMed, Scopus, Web of Science, and PsychINFO databases for articles in English published from January 2010 to December 2022. Studies that did not report any patient-level outcomes were excluded. A total of 2489 studies were screened for eligibility. Full-text screening for 315 yielded 293 exclusions; thus, 22 studies were included. Sixteen of the 22 studies were randomized-controlled trials with durations varying from 90 days to 52 weeks. The findings of this systematic review suggest widespread routine pharmacogenomic testing may not yield significant changes in clinical outcomes when compared to treatment as usual. These results may or may not be generalizable to all persons taking antidepressants given guideline recommendations for pharmacogenomic-guided prescribing in patients on specific antidepressants. Future studies are warranted evaluating the utility of such testing in these subpopulations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Major depressive disorder (MDD) is a psychiatric illness associated with high levels of morbidity that increase economic burden. Between the years of 2010–2018, the economic burden of MDD was estimated to be 326.2 billion dollars in the USA, a 37.9% increase from the 2010 estimation [1]. According to the World Health Organization (WHO), an estimated 5% of the world’s adult population suffer from depression [2]. Nonpharmacologic approaches to treating MDD include psychotherapy, transcranial magnetic stimulation (TMS), and electroconvulsive therapy (ECT). While all antidepressants used to treat MDD exhibit similar efficacy, first-line pharmacologic options such as selective serotonin reuptake inhibitors (SSRIs) or selective serotonin and norepinephrine reuptake inhibitors (SNRIs) are often preferred due to their tolerability profile. Other antidepressant subclasses such as atypical antidepressants and tricyclic antidepressants (TCAs) may be prescribed as monotherapy or adjunct to SSRIs or SNRIs to manage MDD.
Antidepressants exhibit modest efficacy when treating MDD. Remission rates of MDD symptomatology after first-time trial are estimated at 30%, with subsequent medication trial failures producing lower remission rates [3, 4]. Because remission rates remain low, alternative treatment approaches are always being explored to improve the quality of patient care. One alternative treatment approach that has gained traction over the past decade is moving towards personalized medicine, also referred to as pharmacogenomic-guided prescribing.
Pharmacogenomic-guided prescribing has the potential to improve outcomes mainly through assistance with identifying genetic variants that alter metabolism. In these scenarios, the identification of polymorphisms can better assist prescribers with dosing these medications to avoid adverse effects and optimize efficacy. Specifically, patients with polymorphisms of CYP2C19, CYP2D6, and CYP2B6 may benefit from pharmacogenomic (PGx) testing prior to antidepressant prescribing [5•]. The Clinical Pharmacogenetics Implementation Consortium (CPIC), Food and Drug Administration (FDA), and the International Society of Psychiatric Genetics (ISPG) recommend pharmacogenomic testing and personalized dosing for antidepressants metabolized by certain CYP enzymes. The dosing recommendations reflect interindividual differences in pharmacokinetic parameters in those with these genetic variants of CYP enzymes such as CYP2C19 and CYP2D6. There is also evidence that certain genes and alleles such as SLC6A4 and HTR2A may influence clinical response to certain antidepressants; existing data does not support their screening for these genes or alleles to inform antidepressant prescribing [5•].
Currently, routine pharmacogenomic testing in psychiatry and specifically for patients initiated on antidepressants is not recommended for several reasons. Access to testing is difficult and expensive, prescribers often report that interpretation can be futile due to clinician unfamiliarity with PGx testing and lack of knowledge about the evidence of PGx use in psychiatry, and incorporation of testing into current workflows is challenging [6]. Additionally, there is little evidence demonstrating improved clinical outcomes in patients receiving PGx-guided prescribing. Several prospective clinical trials have evaluated the impact of PGx-guided prescribing compared to treatment as usual and found no difference in clinical outcomes for patients with MDD. However, in recent years, additional randomized controlled trials have been conducted to add to the body of literature regarding PGx-informed pharmacotherapy in psychiatry. The purpose of this systematic review is to evaluate available prospective literature and determine the impact of PGx-guided prescribing on clinical outcomes such as rating scale changes, response, and remission in patients who received antidepressant treatment for MDD.
Methods
The systematic review protocol was registered with PROSPERO, an international registry of systematic reviews. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement to conduct this review.
Search Strategy
A literature search was performed using PubMed, Scopus, Web of Science, and PsychINFO databases for articles in English published between January 2010 to December 2022. Literature search strategies were developed in collaboration with a research librarian. The following search terms were utilized: pharmacogenomics and depression. MeSH terms, index terms, and subject headings were included where available. The synonyms of the search terms can be found in Table 1. The date of the last search of databases specified above was January 27, 2023.
Eligibility Criteria
Studies included were published in a peer-reviewed journal, were prospective trials assessing the clinical utility of Pgx testing to inform pharmacotherapy treatment decisions for major depressive disorder, and reported clinical outcomes for either efficacy or safety. Included in the study were adults ≥ 18 years of age treated with an antidepressant from drug classes with MDD indications: selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), monoamine oxidase inhibitors, and atypical antidepressants (mirtazapine, trazodone, bupropion, combination olanzapine/fluoxetine). Studies that did not report any patient-level outcomes were excluded. Articles also excluded were pharmacokinetic studies, pediatric studies with patients < 18 years of age, retrospective studies, genome-wide association studies, pharmacoeconomic analyses, reviews, systematic reviews, meta-analyses, letters, book chapters, case studies, case reports, editorials, commentaries, discussion papers, and conference proceedings.
Study Screening
The study team used Covidence, a web-based collaboration software platform that streamlines the production of systematic and other literature reviews, for study screening, data extraction, and quality assessment. Two study team members completed title and abstract screening independently for each article to determine eligibility for inclusion. Each study team member independently designated an inclusion decision for each article as either “yes,” “no,” or “maybe.” Articles with “yes” or “maybe” designations were screened via full-text assessment to determine eligibility for data extraction. The study team discussed and came to a consensus for articles with conflicting designations that needed to be resolved.
Data Extraction and Synthesis
Independent data extraction was performed by four members of the study team using a standardized data extraction form created in Covidence Extraction and checked by one author. The following data were extracted: (1) study information (study design, intervention, follow-up period, primary objectives, statistical methods); (2) population (setting, subject eligibility criteria); (3) patient baseline characteristics; (4) outcomes. For data synthesis, thematic analysis was conducted (refer to supplemental Table 1: sample data extraction template).
Quality Assessment
Two authors independently conducted quality assessments of all included studies using the Cochrane Risk of Bias tool [7] to evaluate for selection bias, reporting bias, performance bias, detection bias, attrition bias, and other biases in the following seven domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective outcome reporting, and other sources of bias. For each domain, the authors assessed the study and assigned a designation of high, low, or unclear risk of bias for that item. For domains with inconsistent ratings, the authors then discussed the studies to come to a consensus.
Results
The systematic review process is summarized in Fig. 1. A total of 2489 studies were screened for eligibility. Full-text screening for 315 yielded 293 exclusions. The most common reason for exclusion was “wrong study design.” Once all screening was completed, 22 studies remained and were included in the analysis. Characteristics of the 22 studies are listed in Table 2. Six of the included studies were prospective cohort trials [8,9,10,11,12,13]; four of these studies did not include a control arm and only evaluated PGx-guided treatment [10,11,12,13]. The rest were randomized-controlled trials. Studies included sample sizes ranging from 44 to 1944; four studies had sample size < 100, 14 studies had sample size 100–999, and four studies had sample size of 1000 or greater. Study durations ranged from 90 days to 52 weeks with greater than half of the studies being conducted over 8 or 12 weeks. The genes tested across studies varied; only two studies exclusively evaluated patients with specific variants (FKBP5 rs1360780) or single gene polymorphisms (CYP2D6) [14, 15]. None of the studies limited patients to prescription antidepressants of specific metabolic pathways.
All studies included patients with a primary diagnosis of MDD excluding two, one of which included any neuropsychiatric disorder [16], and the other included patients on 2 or more mental health medications [13]; two studies included patients with a comorbid diagnosis of bipolar disorder [10, 17]. Rating scales used to evaluate depressive symptoms varied among studies and included the 17-item Hamilton Depression Rating Scale (HAMD-17/HDRS-17), the Quick Inventory of Depressive Symptomatology- Clinician-Rated (QIDS-C16), Quick Inventory of Depressive Symptomatology-Self-Rated (QIDS-SR16), the Beck Depression Inventory (BDI), and the Patient Health Questionnaire (PHQ-9). Most studies utilized the HAMD-17/HDRS-17.
Quality assessment of studies using the Cochrane Risk of Bias tool yielded varying results in risk of bias, with seven studies that had a determination of low risk of bias in every domain or at least 6 of 7 domains. Several of the studies were deemed to have higher risk of bias, mostly due to a lack of rater or participant blinding. A full report of quality assessment judgments for each domain can be seen in supplemental Table 2.
Of the 18 studies that compared PGx-guided dosing to treatment as usual, 9 showed a statistically significant difference in at least one primary or secondary clinical outcome, with a greater degree of efficacy in the PGx group. Two of these were prospective cohort studies [8, 9] comparing HAMD-17 and QIDS-C16 reduction; these studies had a higher risk of bias determined by quality assessment review. Seven were randomized controlled trials with low risk of bias, demonstrating differences in HAMD-17 response and remission [18,19,20], HDRS Remission [21], PHQ9 score reduction [22], PHQ9 response [23•], or adverse effects [16].
Discussion
The findings from this systematic review of 22 prospective studies in patients prescribed antidepressants for MDD suggest that widespread PGx testing does not yield consistently significant changes in clinical outcomes when compared to treatment as usual. Excluding statistically significant changes in depression rating scale scores from a few earlier studies with a weaker trial design, small sample size, and higher levels of bias, more than half of the higher quality and more recent studies do not demonstrate a statistically significant change in depression rating scale scores, response, or remission. Limitations of this systematic review may further impact the generalizability of clinical implications. Prospective studies were not all randomized controlled trials and clinical outcome measures varied across studies, so data were not pooled for additional analyses.
The largest randomized-controlled trial to date conducted by Oslin and colleagues over a 24-week period evaluated remission rates along with the proportion of prescriptions with a predicted drug-gene interaction written in the 30 days after randomization in those receiving PGx-guided prescribing compared to treatment as usual. Though the difference in remission rates between groups were not statistically significant, those in the PGx-guided prescribing group were less likely to receive a prescription with a drug-gene interaction (\(\chi\)2 = 169.2, p < 0.001). Further, the estimated risk of prescribing a medication with a moderate or substantial gene interaction was lower in the PGx-guided prescribing group (− 24.6% [95%CI, − 29.5 to − 19.7%, p < 0.001] and − 9% [95%CI, − 12.7 to − 5.3%, p < 0.001]), respectively. This study did report a significant finding for the secondary outcome of response to treatment, defined as a binary indicator at each time point of at least a 50% decrease from the baseline PHQ-9 score, with PHQ-9 response in 32.1% in the PGx group vs 27.5% in the TAU group (p = 0.03) [23•].
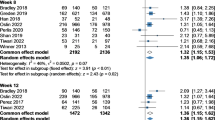
A recent systematic review and meta-analysis of prospective, controlled clinical trials, conducted by Brown and colleagues evaluated depressive symptom remission in guided versus unguided antidepressant prescribing for MDD. The pooled relative risk for all included trials was statistically significant at 1.41 (95% CI, 1.15–1.74, p = 0.001), indicating a higher likelihood of symptom remission in patients receiving PGx-guided antidepressant prescribing. The authors also noted in their meta-regression analysis that the risk ratio favoring PGx-guided treatment increased based on the number of prior antidepressant treatments (Beta = 0.229, p = 0.026) and depressive symptom severity among 12 trials that included this data (Beta = 0.115, p = 0.036) [31•].
While these results may initially seem promising, they must be interpreted with caution. The presence of a drug-gene interaction does not guarantee clinical relevance, as the outcomes can vary depending on the specific assay used and the appropriateness of the clinical interpretation of the reports. In the broader context, the integration of routine PGx testing into antidepressant prescribing may not result in significant changes in clinical outcomes. This highlights a major pitfall in existing studies, as the aggregated results based on pooled data evaluating patients on antidepressants with multiple metabolic pathways and different psychiatric comorbidities may not be generalizable to all patients on antidepressants with MDD. This further underscores the importance of conducting future studies to comprehend the limitations in current PGx research for antidepressant prescribing in MDD and to thoughtfully consider the populations to include, keeping in mind the benefit of including an ethnically diverse sample with varying severities of depressive illness. With the exception of two trials conducted in countries in Asia, most studies were not ethnically diverse, and the majority of the samples were from Caucasian patients. Given the interethnic variability in drug metabolism, this becomes relevant when prescribing antidepressants with CYP-mediated metabolism that could be impacted by CYP polymorphisms. Further, of the studies that reported depressive symptom illness severity, most reported mild-to-moderate depressive symptoms and did not report the number of prior antidepressant trials. In light of the possibility that individuals with a higher number of prior antidepressant trials and more severe depressive symptoms may derive greater advantages from PGx-guided prescribing, and that PGx testing is occasionally pursued in cases of severe or treatment-resistant depressive symptoms following multiple medication trials, it becomes imperative to incorporate these specific patient profiles into clinical trial populations.
The CPIC, FDA, and ISPG all support the use of PGx testing and personalized dosing of antidepressants metabolized by CYP2C19 and CYP2D6 [5•, 32,33,34]. These recommendations include proposed alternative dosing recommendations based on CYP2C19 and CYP2D6 metabolizer status in patients on selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants [5•, 32, 33]. The Food and Drug Administration (FDA) also makes similar recommendations CYP2C19 and CYP2D6 metabolized medications including venlafaxine and escitalopram [33]. The CPIC and ISPG also endorse routine testing and personalized dosing for those prescribed antidepressants by CYP2B6 such as sertraline and bupropion [5•, 34]. Patients prescribed antidepressants metabolized by these enzymes, especially those with genetic polymorphisms, are likely to yield the greatest benefits from PGx testing per available evidence. These benefits would likely have the greatest impact on poor metabolizers and ultrarapid metabolizers as these designations would yield changes in CYP2C19 or CYP2D6-metabolized antidepressant dosing or selection, potentially yielding better efficacy, tolerability, response, and remission rates.
Conclusion
Widespread, routine PGx-guided prescribing of antidepressants for MDD is less likely to significantly improve clinical outcomes such as depression rating scale scores, response, and remission. However, specific patient populations are more likely to benefit from PGx-guided prescribing. Future studies are warranted evaluating the impact of PGx-guided prescribing of antidepressants in certain subpopulations such as patients with treatment-refractory MDD, intolerability to multiple CYP metabolized antidepressants, or those receiving antidepressants metabolized via the CYP2C19, CYP2D6, and CYP2B6 pathways.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
Greenberg PE, Fournier AA, Sisitsky T, et al. The economic burden of adults with major depressive disorder in the United States (2010 and 2018). Pharmacoeconomics. 2021;39(6):653–65. https://doi.org/10.1007/s40273-021-01019-4.
GBD Results. Institute for Health Metrics and Evaluation. Accessed Oct 10 2023.https://vizhub.healthdata.org/gbd-results.
Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163(11):1905–17. https://doi.org/10.1176/ajp.2006.163.11.1905.
Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163(1):28–40. https://doi.org/10.1176/appi.ajp.163.1.28.
• Bousman CA, Stevenson JM, Ramsey LB, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2D6, CYP2C19, CYP2B6, SLC6A4, and HTR2A Genotypes and Serotonin Reuptake Inhibitor Antidepressants. Clin Pharmacol Ther. 2023;114(1):51–68. https://doi.org/10.1002/cpt.2903. Most updated CPIC guidelines on the use of PGx -guided prescribing of antidepressants.
Jameson A, Fylan B, Bristow GC, et al. What are the barriers and enablers to the implementation of pharmacogenetic testing in mental health care settings? Front Genet. 2021;12:740216. https://doi.org/10.3389/fgene.2021.740216.
Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
Hall-Flavin DK, Winner JG, Allen JD, et al. Using a pharmacogenomic algorithm to guide the treatment of depression. Transl Psychiatry. 2012;2(10):e172–e172. https://doi.org/10.1038/tp.2012.99.
Hall-Flavin DK, Winner JG, Allen JD, et al. Utility of integrated pharmacogenomic testing to support the treatment of major depressive disorder in a psychiatric outpatient setting. Pharmacogenet Genomics. 2013;23(10):535. https://doi.org/10.1097/FPC.0b013e3283649b9a.
Brennan FX, Gardner KR, Lombard J, et al. A naturalistic study of the effectiveness of pharmacogenetic testing to guide treatment in psychiatric patients with mood and anxiety disorders. Prim Care Companion CNS Disord. 2015;17(2). https://doi.org/10.4088/PCC.14m01717.
Torrellas C, Carril JC, Cacabelos R. Optimization of antidepressant use with pharmacogenetic strategies. Curr Genomics. 2017;18(5):442–9. https://doi.org/10.2174/1389202918666170426164940.
Tanner JA, Davies PE, Voudouris NC, et al. Combinatorial pharmacogenomics and improved patient outcomes in depression: treatment by primary care physicians or psychiatrists. J Psychiatr Res. 2018;104:157–62. https://doi.org/10.1016/j.jpsychires.2018.07.012.
Wood AE, Agrawal D, Deem AP, et al. Medication optimization using pharmacogenomic testing in a complex mental health population prescribed psychiatric polypharmacy. J Clin Pharmacol. 2022;62(7):898–904. https://doi.org/10.1002/jcph.2032.
Stamm TJ, Rampp C, Wiethoff K, et al. The FKBP5 polymorphism rs1360780 influences the effect of an algorithm-based antidepressant treatment and is associated with remission in patients with major depression. J Psychopharmacol (Oxf). 2016;30(1):40–7. https://doi.org/10.1177/0269881115620459.
Ruaño G, Robinson S, Holford T, et al. Results of the CYP-GUIDES randomized controlled trial: total cohort and primary endpoints. Contemp Clin Trials. 2020;89:105910. https://doi.org/10.1016/j.cct.2019.105910.
Olson MC, Maciel A, Gariepy JF, et al. Clinical impact of pharmacogenetic-guided treatment for patients exhibiting neuropsychiatric disorders: a randomized controlled trial. Prim Care Companion CNS Disord. 2017;19(2). https://doi.org/10.4088/PCC.16m02036.
McCarthy MJ, Chen Y, Demodena A, et al. A prospective study to determine the clinical utility of pharmacogenetic testing of veterans with treatment-resistant depression. J Psychopharmacol (Oxf). 2021;35(8):992–1002. https://doi.org/10.1177/02698811211015224.
Bradley P, Shiekh M, Mehra V, et al. Improved efficacy with targeted pharmacogenetic-guided treatment of patients with depression and anxiety: a randomized clinical trial demonstrating clinical utility. J Psychiatr Res. 2018;96:100–7. https://doi.org/10.1016/j.jpsychires.2017.09.024.
Han C, Wang SM, Bahk WM, et al. A pharmacogenomic-based antidepressant treatment for patients with major depressive disorder: results from an 8-week, randomized, single-blinded clinical trial. Clin Psychopharmacol Neurosci Off Sci J Korean Coll Neuropsychopharmacol. 2018;16(4):469–80. https://doi.org/10.9758/cpn.2018.16.4.469.
Greden JF, Parikh SV, Rothschild AJ, et al. Impact of pharmacogenomics on clinical outcomes in major depressive disorder in the GUIDED trial: a large, patient- and rater-blinded, randomized, controlled study. J Psychiatr Res. 2019;111:59–67. https://doi.org/10.1016/j.jpsychires.2019.01.003.
Singh AB. Improved antidepressant remission in major depression via a pharmacokinetic pathway polygene pharmacogenetic report. Clin Psychopharmacol Neurosci. 2015;13(2):150–6. https://doi.org/10.9758/cpn.2015.13.2.150.
Papastergiou J, Quilty LC, Li W, et al. Pharmacogenomics guided versus standard antidepressant treatment in a community pharmacy setting: a randomized controlled trial. Clin Transl Sci. 2021;14(4):1359–68. https://doi.org/10.1111/cts.12986.
• Oslin DW, Lynch KG, Shih MC, et al. Effect of pharmacogenomic testing for drug-gene interactions on medication selection and remission of symptoms in major depressive disorder: the PRIME Care Randomized Clinical Trial. JAMA. 2022;328(2):151–61. https://doi.org/10.1001/jama.2022.9805. Largest RCT to date evaluating PGx-tesing for patients with MDD on antidepressants.
Winner JG, Carhart JM, Altar CA, Allen JD, Dechairo BM. A prospective, randomized, double-blind study assessing the clinical impact of integrated pharmacogenomic testing for major depressive disorder. Discov Med. 2013;16(89):219–27.
Pérez V, Salavert A, Espadaler J, et al. Efficacy of prospective pharmacogenetic testing in the treatment of major depressive disorder: results of a randomized, double-blind clinical trial. BMC Psychiatry. 2017;17(1):250. https://doi.org/10.1186/s12888-017-1412-1.
Shan X, Zhao W, Qiu Y, et al. Preliminary clinical investigation of combinatorial pharmacogenomic testing for the optimized treatment of depression: a randomized single-blind study. Front Neurosci. 2019;13:960. https://doi.org/10.3389/fnins.2019.00960.
Perlis RH, Dowd D, Fava M, Lencz T, Krause DS. Randomized, controlled, participant- and rater-blind trial of pharmacogenomic test-guided treatment versus treatment as usual for major depressive disorder. Depress Anxiety. 2020;37(9):834–41. https://doi.org/10.1002/da.23029.
Bohlen KN, Kittelsrud JM, Nelson ME, et al. Clinical utility of pharmacogenetics in a psychiatric and primary care population. Pharmacogenomics J. 2023;23(1):21–7. https://doi.org/10.1038/s41397-022-00292-6.
Tiwari AK, Zai CC, Altar CA, et al. Clinical utility of combinatorial pharmacogenomic testing in depression: a Canadian patient- and rater-blinded, randomized, controlled trial. Transl Psychiatry. 2022;12(1):1–10. https://doi.org/10.1038/s41398-022-01847-8.
Pérez V, Salavert A, Espadaler J, Tuson M, Saiz-Ruiz J, Sáez-Navarro C, Bobes J, Baca-García E, Vieta E, Olivares JM, Rodriguez-Jimenez R, Villagrán JM, Gascón J, Cañete-Crespillo J, Solé M, Saiz PA, Ibáñez Á, de Diego-Adeliño J; AB-GEN Collaborative Group; Menchón JM. Efficacy of prospective pharmacogenetic testing in the treatment of major depressive disorder: results of a randomized, double-blind clinical trial. BMC Psychiatry. 2017;17(1):250.
• Brown LC, Stanton JD, Bharthi K, Maruf AA, Müller DJ, Bousman CA. Pharmacogenomic testing and depressive symptom remission: a systematic review and meta-analysis of prospective, controlled clinical trials. Clin Pharmacol Ther. 2022;112(6):1303–17. https://doi.org/10.1002/cpt.2748. Most recent systematic review and meta-analysis indicating a higher likelihood of symptom remission in patients receiving PGx-guided antidepressant prescribing.
Hicks JK, Sangkuhl K, Swen JJ, et al. Clinical pharmacogenetics implementation consortium guideline (CPIC) for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants: 2016 update. Clin Pharmacol Ther. 2017;102(1):37–44. https://doi.org/10.1002/cpt.597.
Health C for D and R. Table of Pharmacogenetic Associations. FDA. Published online October 26, 2022. Accessed Oct 10 2023. https://www.fda.gov/medical-devices/precision-medicine/table-pharmacogenetic-associations.
Bousman CA, Bengesser SA, Aitchison KJ, et al. Review and consensus on pharmacogenomic testing in psychiatry. Pharmacopsychiatry. 2021;54(1):5–17. https://doi.org/10.1055/a-1288-1061.
Acknowledgements
Hector Perez (UCI Research Librarian) for assistance with developing search strategies, Obinna Ekechukwu, Harini Bhat, Jasvir Kaur, for their work on the team with literature screening and data extraction.
The authors wish to thank Dr. Gerard Quinn for reviewing their paper.
Author information
Authors and Affiliations
Contributions
MJ- conceptualization of study, edited manuscript CC- conceptualization of study, screened studies, contributed to manuscript preparation and editing FK- screened studies, summarized trial data, drafted and edited manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Khorassani, F., Jermain, M. & Cadiz, C. Pharmacogenomic Testing to Guide Treatment of Major Depressive Disorder: A Systematic Review. Curr Treat Options Psych 11, 123–140 (2024). https://doi.org/10.1007/s40501-024-00316-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40501-024-00316-x