Abstract
Purpose of Review
This review aims to offer a comprehensive insight and a recent update into the etiology and pathophysiology of ovarian cancer, a recent update on the usage of quercetin for ovarian cancer management.
Recent Findings
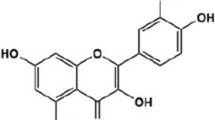
Over the last few decades, an alarming increase in global rates of ovarian cancer has been observed, resulting in increased pressure on the healthcare system. In order to effectively address the situation, there is a need to explore alternatives to currently dominant treatment regimes. The usage of phytoconstituents, such as polyphenols as anti-cancer agents, has emerged as a promising alternative. Quercetin, a widely distributed dietary flavonol, possesses potent antioxidant, anti-inflammatory, and cytoprotective properties, and has been used in the amelioration of a variety of metabolic disorders. In addition to effectively managing various types of cancer, it has been seen to pose lowered side effects and improve the overall quality of life of patients.
Summary
Literature search of quercetin showed remarkable properties like antioxidant, anti-cancer, anti-apoptotic, anti-inflammatory, and bioavailability-enhancing abilities that fit its appropriate use in pathological conditions. However, being a product of natural origin, bioavailability and optimal delivery may prove to be challenging to achieving the desired therapeutic efficacy. This review, in turn, furthers our understanding of the applications of quercetin in cancer management and the identification of challenges and future perspectives, to enable the maximization of therapeutic efficacy.




Similar content being viewed by others
References
Adami HO, Hsieh CC, Lambe M, Trichopoulos D, Leon D, Persson I, Ekbom A, Janson PO. Parity, age at first childbirth, and risk of ovarian cancer. Lancet (London, England). 1994;344(8932):1250–4. https://doi.org/10.1016/s0140-6736(94)90749-8.
Asgharian P, Tazehkand AP, Soofiyani SR, Hosseini K, Martorell M, Tarhriz V, Ahangari H, et al. ‘Quercetin impact in pancreatic cancer: an overview on its therapeutic effects’. Edited by Felipe L. de Oliveira. Oxidative Med Cell Longev. 2021;2021(November):1–13. https://doi.org/10.1155/2021/4393266.
Ashraf AH, Zuberi M, Afroze SH, Yamauchi K, Zawieja DC, Keuhl TJ, Erlandson LW, Uddin MN. Differential mechanism of action of 3,4′,7-O-trimethylquercetin in three types of ovarian cancer cells. Anticancer Res. 2018;38(9):5131–7. https://doi.org/10.21873/anticanres.12835.
Askari G, Ghiasvand R, Feizi A, Ghanadian SM, Karimian J. The effect of quercetin supplementation on selected markers of inflammation and oxidative stress. J Res Med Sci. 2012;17(7):637–41.
Bonifácio VDB. Ovarian cancer biomarkers: moving forward in early detection. Adv Exp Med Biol. 2020;1219:355–63. https://doi.org/10.1007/978-3-030-34025-4_18.
Cao H-H, Cheng C-Y, Tao Su, Xiu-Qiong Fu, Guo H, Li T, Tse A-W, Kwan H-Y, Hua Yu, Zhi-Ling Yu. Quercetin inhibits HGF/c-Met signaling and HGF-stimulated melanoma cell migration and invasion. Mol Cancer. 2015;14(1):103. https://doi.org/10.1186/s12943-015-0367-4.
Chan MM, Fong D, Soprano KJ, Holmes WF, Heverling H. Inhibition of growth and sensitization to cisplatin-mediated killing of ovarian cancer cells by polyphenolic chemopreventive agents. J Cell Physiol. 2003;194(1):63–70. https://doi.org/10.1002/jcp.10186.
Clendenen TV, Lundin E, Zeleniuch-Jacquotte A, Koenig KL, Berrino F, Lukanova A, Lokshin AE, et al. Circulating inflammation markers and risk of epithelial ovarian cancer. Cancer Epidemiol, Biomarkers Prev: Publ Am Assoc Cancer Res, Cosponsored Am Soc Prev Oncol. 2011;20(5):799–810. https://doi.org/10.1158/1055-9965.EPI-10-1180.
Dabeek WM, Marra MV. Dietary quercetin and kaempferol: bioavailability and potential cardiovascular-related bioactivity in humans. Nutrients. 2019;11(10):2288. https://doi.org/10.3390/nu11102288.
D’Andrea G. Quercetin: a flavonol with multifaceted therapeutic applications? Fitoterapia. 2015;106(October):256–71. https://doi.org/10.1016/j.fitote.2015.09.018.
Dhanaraj T, Mohan M, Arunakaran J. Quercetin attenuates metastatic ability of human metastatic ovarian cancer cells via modulating multiple signaling molecules involved in cell survival, proliferation, migration and adhesion. Arch Biochem Biophys. 2021;701(April):108795. https://doi.org/10.1016/j.abb.2021.108795.
Di Meo S, Reed TT, Venditti P, Victor VM. Role of ROS and RNS sources in physiological and pathological conditions. Oxid Med Cell Longev. 2016;2016:1245049. https://doi.org/10.1155/2016/1245049.
Dudley AC, Griffioen AW. Pathological angiogenesis: mechanisms and therapeutic strategies. Angiogenesis. 2023. https://doi.org/10.1007/s10456-023-09876-7.
Eisvand F, Tajbakhsh A, Seidel V, Zirak MR, Tabeshpour J, Shakeri A. Quercetin and its role in modulating endoplasmic reticulum stress: a review. Phytother Res. 2022;36(1):73–84. https://doi.org/10.1002/ptr.7283.
Fares J, Fares MY, Khachfe HH, Salhab HA, Fares Y. Molecular principles of metastasis: a hallmark of cancer revisited. Signal Transduct Target Ther. 2020;5:28. https://doi.org/10.1038/s41392-020-0134-x.
Fatease AA, Shah V, Nguyen DX, Cote B, LeBlanc N, Rao DA, Alani AWG. Chemosensitization and mitigation of adriamycin-induced cardiotoxicity using combinational polymeric micelles for co-delivery of quercetin/resveratrol and resveratrol/curcumin in ovarian cancer. Nanomedicine: Nanotechnol, Biol Med. 2019;19(July):39–48. https://doi.org/10.1016/j.nano.2019.03.011.
Fernandes SG, Gala K, Khattar E. Telomerase inhibitor MST-312 and quercetin synergistically inhibit cancer cell proliferation by promoting DNA damage. Transl Oncol. 2023;27(January):101569. https://doi.org/10.1016/j.tranon.2022.101569.
Ferry DR, Smith A, Malkhandi J, Fyfe DW, deTakats PG, Anderson D, Baker J, Kerr DJ. Phase I clinical trial of the flavonoid quercetin: pharmacokinetics and evidence for in vivo tyrosine kinase inhibition. Clin Cancer Res: Off J Am Assoc Cancer Res. 1996;2(4):659–68.
Gao X, Wang B, Wei X, Men K, Zheng F, Zhou Y, Zheng Y, et al. Anticancer effect and mechanism of polymer micelle-encapsulated quercetin on ovarian cancer. Nanoscale. 2012;4(22):7021. https://doi.org/10.1039/c2nr32181e.
Gates MA, Tworoger SS, Hecht JL, De Vivo I, Rosner B, Hankinson SE. A prospective study of dietary flavonoid intake and incidence of epithelial ovarian cancer. Int J Cancer. 2007;121(10):2225–32. https://doi.org/10.1002/ijc.22790.
Gong C, Yang Z, Zhang L, Wang Y, Gong W, Liu Yi. Quercetin suppresses DNA double-strand break repair and enhances the radiosensitivity of human ovarian cancer cells via P53-dependent endoplasmic reticulum stress pathway. Onco Targets Ther. 2017;11(December):17–27. https://doi.org/10.2147/OTT.S147316.
Hasan AASh, Kalinina EV, Tatarskiy VV, Volodina YuL, Petrova AS, Novichkova MD, Zhdanov DD, Shtil AA. Suppression of the antioxidant system and PI3K/Akt/MTOR signaling pathway in cisplatin-resistant cancer cells by quercetin. Bull Exp Biol Med. 2022;173(6):760–4. https://doi.org/10.1007/s10517-022-05626-9.
Hasan AA, Tatarskiy V, Kalinina E. Synthetic pathways and the therapeutic potential of quercetin and curcumin. Int J Mol Sci. 2022;23(22):14413. https://doi.org/10.3390/ijms232214413.
Hosseini A, Razavi BM, Banach M, Hosseinzadeh H. Quercetin and metabolic syndrome: a review. Phytother Res. 2021;35(10):5352–64. https://doi.org/10.1002/ptr.7144.
Hunn J, Rodriguez GC. Ovarian cancer: etiology, risk factors, and epidemiology. Clin Obstet Gynecol. 2012;55(1):3–23. https://doi.org/10.1097/GRF.0b013e31824b4611.
Haibe Y, Kreidieh M, El Hajj H, Khalifeh I, Mukherji D, Temraz S, Shamseddine A. Resistance mechanisms to anti-angiogenic therapies in cancer. Front Oncol. 2020;10. https://doi.org/10.3389/fonc.2020.00221.
Huang X, He D, Pan Z, Luo G, Deng J. Reactive-oxygen-species-scavenging nanomaterials for resolving inflammation. Mater Today Bio. 2021;11:100124. https://doi.org/10.1016/j.mtbio.2021.100124.
Kashyap D, Mittal S, Sak K, Singhal P, Tuli HS. Molecular mechanisms of action of quercetin in cancer: recent advances. Tumor Biology. 2016;37(10):12927–39. https://doi.org/10.1007/s13277-016-5184-x.
Li Li, Mangali S, Kour N, Dasari D, Ghatage T, Sharma V, Dhar A, Bhat A. Syzygium cumini (jamun) fruit-extracted phytochemicals exert anti-proliferative effect on ovarian cancer cells. J Cancer Res Ther. 2021;17(6):1547–51. https://doi.org/10.4103/jcrt.JCRT_210_20.
Li M, Zhang W, Yang L, Wang H, Wang Y, Huang K, Zhang W. The mechanism of Xiaoyao San in the treatment of ovarian cancer by network pharmacology and the effect of stigmasterol on the PI3K/Akt pathway. Edited by Zhongjie Shi. Dis Markers. 2021;2021(June):1–10. https://doi.org/10.1155/2021/4304507.
Li W, Shen F, Weber G. Ribavirin and quercetin synergistically downregulate signal transduction and are cytotoxic in human ovarian carcinoma cells. Oncol Res. 1999;11(5):243–7.
Li W, Yu Y, Cheng H, Liu S, Gong T, Ma J, Tang Q. ‘Quercetin inhibits KBM7R cell proliferation through Wnt/β-catenin signaling’. Edited by Muhammad Zia-Ul-Haq. Evid-Based Complement Altern Med. 2022;2022(June):1–7. https://doi.org/10.1155/2022/1378976.
Li Y, Kong D, Ying Fu, Sussman MR, Hong Wu. The effect of developmental and environmental factors on secondary metabolites in medicinal plants. Plant Physiol Biochem. 2020;148(March):80–9. https://doi.org/10.1016/j.plaphy.2020.01.006.
Li Y, Yao J, Han C, Yang J, Chaudhry MT, Wang S, Liu H, Yin Y. Quercetin, inflammation and immunity. Nutrients. 2016;8(3):1–14. https://doi.org/10.3390/nu8030167.
Lugano R, Ramachandran M, Dimberg A. Tumor angiogenesis: causes, consequences, challenges and opportunities. Cell Mol Life Sci. 2020;77:1745–70. https://doi.org/10.1007/s00018-019-03351-7.
Lupo G, Cambria MT, Olivieri M, Rocco C, Caporarello N, Longo A, Zanghì G, Salmeri M, Foti MC, Anfuso CD. Anti-angiogenic effect of quercetin and its 8-methyl pentamethyl ether derivative in human microvascular endothelial cells. J Cell Mol Med. 2019;23(10):6565–77. https://doi.org/10.1111/jcmm.14455.
Lupo G, Cambria MT, Olivieri M, Rocco C, Caporarello N, Longo A, Zanghì G, Salmeri M, Foti MC, Anfuso CD. Anti-angiogenic effect of quercetin and its 8-methyl pentamethyl ether derivative in human microvascular endothelial cells. J Cell Mol Med. 2019;23:6565–77. https://doi.org/10.1111/jcmm.14455.
Macciò A, Madeddu C. Inflammation and ovarian cancer. Cytokine. 2012;58(2):133–47. https://doi.org/10.1016/j.cyto.2012.01.015.
Matulonis UA, Sood AK, Fallowfield L, Howitt BE, Sehouli J, Karlan BY. Ovarian cancer. Nat Rev Dis Primers. 2016;2(August):16061. https://doi.org/10.1038/nrdp.2016.61.
Metodiewa D, Jaiswal AK, Cenas N, Dickancaité E, Segura-Aguilar J. Quercetin may act as a cytotoxic prooxidant after its metabolic activation to semiquinone and quinoidal product. Free Radical Biol Med. 1999;26(1–2):107–16. https://doi.org/10.1016/S0891-5849(98)00167-1.
Michalcova K, Roychoudhury S, Halenar M, Tvrda E, Kovacikova E, Vasicek J, Chrenek P, et al. In vitro response of human ovarian cancer cells to dietary bioflavonoid isoquercitrin. J Environ Sci Health B. 2019;54(9):752–7. https://doi.org/10.1080/03601234.2019.1633214.
Mirossay L, Varinská L, Mojžiš J. Antiangiogenic effect of flavonoids and chalcones: an update. Int J Mol Sci. 2017;19(1):E27. https://doi.org/10.3390/ijms19010027.
Moazzami B, Chaichian S, Nikfar B, Bidgoli SA. Modulation of MicroRNAs expression and cellular signaling pathways through curcumin as a potential therapeutical approach against ovarian cancer: a review. Pathol – Res Pract. 2023;247(July):154527. https://doi.org/10.1016/j.prp.2023.154527.
Murakami A, Ashida H, Terao J. Multitargeted cancer prevention by quercetin. Cancer Lett. 2008;269(2):315–25. https://doi.org/10.1016/j.canlet.2008.03.046.
Nabavi SM, Šamec D, Tomczyk M, Milella L, Russo D, Habtemariam S, Suntar I, et al. Flavonoid biosynthetic pathways in plants: versatile targets for metabolic engineering. Biotechnol Adv. 2020;38(January):107316. https://doi.org/10.1016/j.biotechadv.2018.11.005.
Ness RB, Cottreau C. Possible role of ovarian epithelial inflammation in ovarian cancer. J Natl Cancer Inst. 1999;91(17):1459–67. https://doi.org/10.1093/jnci/91.17.1459.
Nessa MU, Beale P, Chan C, Yu JQ, Huq F. Synergism from combinations of cisplatin and oxaliplatin with quercetin and thymoquinone in human ovarian tumour models. Anticancer Res. 2011;31(11):3789–97.
Niedzwiecki A, Roomi MW, Kalinovsky T, Rath M. ‘Anticancer efficacy of polyphenols and their combinations.’ Nutrients. 2016;8(9). https://doi.org/10.3390/nu8090552.
Pani S, Mohapatra S, Sahoo A, Baral B, Debata PR. ‘Shifting of cell cycle arrest from the S‐phase to G2/M phase and downregulation of EGFR expression by phytochemical combinations in HeLa cervical cancer cells’. J Biochem Mol Toxicol 2022;36 (1). https://doi.org/10.1002/jbt.22947.
Penny SM. Ovarian cancer: an overview. Radiol Technol. 2020;91(6):561–75.
Pinheiro RGR, Pinheiro M, Neves AR. Nanotechnology innovations to enhance the therapeutic efficacy of quercetin. Nanomaterials. 2021;11(10):2658. https://doi.org/10.3390/nano11102658.
Perillo B, Di Donato M, Pezone A, Di Zazzo E, Giovannelli P, Galasso G, Castoria G, Migliaccio A. ROS in cancer therapy: the bright side of the moon. Exp Mol Med. 2020;52:192–203. https://doi.org/10.1038/s12276-020-0384-2.
Pratheeshkumar P, Budhraja A, Son Y-O, Wang X, Zhang Z, Ding S, Wang L, Hitron A, Lee J-C, Xu M, Chen G, Luo J, Shi X. Quercetin inhibits angiogenesis mediated human prostate tumor growth by targeting VEGFR-2 regulated AKT/mTOR/P70S6K signaling pathways. PLoS One. 2012;7:e47516. https://doi.org/10.1371/journal.pone.0047516.
Rais J, Jafri A, Siddiqui S, Tripathi M, Arshad M. Phytochemicals in the treatment of ovarian cancer. Front Biosci (Elite Ed). 2017;9(1):67–75. https://doi.org/10.2741/e786.
Ramalingam V, Sathya PM, Srivalli T, Mohan H. Synthesis of quercetin functionalized wurtzite type zinc oxide nanoparticles and their potential to regulate intrinsic apoptosis signaling pathway in human metastatic ovarian cancer. Life Sci. 2022;309(November):121022. https://doi.org/10.1016/j.lfs.2022.121022.
Rashidi Z, Khosravizadeh Z, Talebi A, Khodamoradi K, Ebrahimi R, Amidi F. Overview of biological effects of quercetin on ovary. Phytother Res. 2021;35(1):33–49. https://doi.org/10.1002/ptr.6750.
Rather RA, Bhagat M. Quercetin as an innovative therapeutic tool for cancer chemoprevention: molecular mechanisms and implications in human health. Cancer Med. 2020;9(24):9181–92. https://doi.org/10.1002/cam4.1411.
Ren MX, Deng XH, Ai F, Yuan GY, Song HY. Effect of quercetin on the proliferation of the human ovarian cancer cell line SKOV-3 in vitro. Exp Ther Med. 2015;10(2):579–83. https://doi.org/10.3892/etm.2015.2536.
Sakao K, Fujii M, Hou D-X. Clarification of the role of quercetin hydroxyl groups in superoxide generation and cell apoptosis by chemical modification. Biosci Biotechnol Biochem. 2009;73(9):2048–53. https://doi.org/10.1271/bbb.90253.
Samare-Najaf M, Zal F, Safari S. Primary and secondary markers of doxorubicin-induced female infertility and the alleviative properties of quercetin and vitamin E in a rat model. Reprod Toxicol. 2020;96(September):316–26. https://doi.org/10.1016/j.reprotox.2020.07.015.
Scambia G, Ranelletti FO, Benedetti Panici P, Bonanno G, De Vincenzo R, Piantelli M, Mancuso S. Synergistic antiproliferative activity of quercetin and cisplatin on ovarian cancer cell growth. Anticancer Drugs. 1990;1(1):45–8. https://doi.org/10.1097/00001813-199010000-00008.
Schildkraut JM, Bastos E, Berchuck A. Relationship between lifetime ovulatory cycles and overexpression of mutant P53 in epithelial ovarian cancer. J Natl Cancer Inst. 1997;89(13):932–8. https://doi.org/10.1093/jnci/89.13.932.
Shafabakhsh R, Asemi Z. Quercetin: a natural compound for ovarian cancer treatment. J Ovarian Res. 2019;12(1):1–9. https://doi.org/10.1186/s13048-019-0530-4.
Shen F, Herenyiova M, Weber G. Synergistic down-regulation of signal transduction and cytotoxicity by tiazofurin and quercetin in human ovarian carcinoma cells. Life Sci. 1999;64(21):1869–76. https://doi.org/10.1016/s0024-3205(99)00133-2.
Sinenko SA, Starkova TY, Kuzmin AA, Tomilin AN. Physiological signaling functions of reactive oxygen species in stem cells: from flies to man. Front Cell Dev Biol. 2021;9. https://doi.org/10.3389/fcell.2021.714370.
Shen F, Weber G. Synergistic action of quercetin and genistein in human ovarian carcinoma cells. Oncol Res. 1997;9(11–12):597–602.
Singh P, Arif Y, Bajguz A, Hayat S. The role of quercetin in plants. Plant Physiol Biochem. 2021;166(September):10–9. https://doi.org/10.1016/j.plaphy.2021.05.023.
Teekaraman D, Elayapillai SP, Viswanathan MP, Jagadeesan A. Quercetin inhibits human metastatic ovarian cancer cell growth and modulates components of the intrinsic apoptotic pathway in PA-1 cell line. Chem Biol Interact. 2019;300(January):91–100. https://doi.org/10.1016/j.cbi.2019.01.008.
Tiwari H, Karki N, Pal M, Basak S, Verma RK, Bal R, Kandpal ND, Bisht G, Sahoo NG. Functionalized graphene oxide as a nanocarrier for dual drug delivery applications: the synergistic effect of quercetin and gefitinib against ovarian cancer cells. Colloids Surf B, Biointerfaces. 2019;178(June):452–9. https://doi.org/10.1016/j.colsurfb.2019.03.037.
Uttarawichien T, Kamnerdnond C, Inwisai T, Suwannalert P, Sibmooh N, Payuhakrit W. Quercetin inhibits colorectal cancer cells induced-angiogenesis in both colorectal cancer cell and endothelial cell through downregulation of VEGF-A/VEGFR2. Sc Pharm. 2021;89(2):23. https://doi.org/10.3390/scipharm89020023.
Vafadar A, Shabaninejad Z, Movahedpour A, Fallahi F, Taghavipour M, Ghasemi Y, Akbari M, et al. Quercetin and cancer: new insights into its therapeutic effects on ovarian cancer cells. Cell Biosci. 2020;10:32. https://doi.org/10.1186/s13578-020-00397-0.
Wang RE, Kao JLF, Hilliard CA, Pandita RK, Roti JL, Roti CR, Hunt, and John Stephen Taylor. Inhibition of heat shock induction of heat shock protein 70 and enhancement of heat shock protein 27 phosphorylation by quercetin derivatives. J Med Chem. 2009;52(7):1912–21. https://doi.org/10.1021/jm801445c.
Xu G, Li B, Wang T, Wan J, Zhang Y, Huang J, Shen Y. Enhancing the anti-ovarian cancer activity of quercetin using a self-assembling micelle and thermosensitive hydrogel drug delivery system. RSC Adv. 2018;8(38):21229–42. https://doi.org/10.1039/C8RA03274B.
Xu X, Chen F, Zhang L, Liu L, Zhang C, Zhang Z, Li W. Exploring the mechanisms of anti-ovarian cancer of Hedyotis diffusa Willd and Scutellaria barbata D. Don through focal adhesion pathway. J Ethnopharmacol. 2021;279(October):114343. https://doi.org/10.1016/j.jep.2021.114343.
Yan Y-B, Tian Q, Zhang J-F, Xiang Y. Antitumor effects and molecular mechanisms of action of natural products in ovarian cancer (review). Oncol Lett. 2020;20(5):1–1. https://doi.org/10.3892/ol.2020.12001.
Zarghi A, Arfaei S. Selective COX-2 inhibitors: a review of their structure-activity relationships. Iran J Pharm Res. 2011;10:655–83.
Zimna A, Kurpisz M. Hypoxia-inducible factor-1 in physiological and pathophysiological angiogenesis: applications and therapies. Biomed Res Int. 2015;2015:549412. https://doi.org/10.1155/2015/549412.
Acknowledgements
The authors are thankful to Shobhaben Pratapbhai Patel School of Pharmacy & Technology Management, SVKM’s NMIMS for providing the infrastructural facilities and support.
Author information
Authors and Affiliations
Contributions
GK visualized the presented idea, contributed to manuscript writing and supervised the project. DSG, VG and AK contributed to literature searches and preparing the manuscript draft. AK, MG and HST revised and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gupta, D.S., Gadi, V., Kaur, G. et al. Exploration of the Growing Therapeutic Potentials of Quercetin in Ovarian Cancer Management. Curr. Pharmacol. Rep. 9, 455–467 (2023). https://doi.org/10.1007/s40495-023-00343-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40495-023-00343-x