Abstract
Purpose of Review
In this work, we will describe a scalable and versatile three-dimensional and dynamic (3DD) cell culture system used in our laboratory as an in vitro tool for pharmacokinetic (PK), pharmacodynamic (PD), and toxicodynamic (TD) evaluation of anti-cancer agents in mono and combination therapy.
Recent Findings
Certain attributes of the 3DD cell culture system such as its ability to sustain high-density cell growth, simulation of clinically relevant PK profiles, and sampling of PK, PD, and TD endpoints make it suitable for long-term in vitro studies. Here, we highlight two case examples from our laboratory using this system. First, we have successfully evaluated the PK and PD of a novel combination regimen against human epidermal growth factor receptor type 2 (HER2)–positive breast cancer refractory to HER2 therapy. The resulting PK/PD relationships allowed optimization of drug dosing of the agents in the combination. Second, our laboratory is currently examining the clinical PK determinants controlling doxorubicin (DOX)–induced cardiotoxicity, linking them with TD endpoints and evaluating optimal dosing regimens of DOX for alleviating cardiotoxicity.
Summary
Our promising state-of-the-art in vitro 3DD cell culture system holds several advantages over traditional tissue culture systems. The in vitro simulation of human PK profiles in combination with serial sampling over several weeks allows to more accurately study and predict tumor killing, resistance, and toxicities of anti-cancer agents and combinations for future rationally designed studies in patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The three-dimensional and dynamic (3DD) cell culture system that is employed in our laboratory is a disposable, two-compartment bioreactor designed for use in high-density cell culture and mass production of proteins and/or antibodies secreted by cells [1, 2]. It consists of a cell culture bottle with an upper chamber containing biocompatible fabric carriers and an expandable/contractible bottom, which contains cell culture medium. The bottles are placed on a platform that drives the contraction or expansion of the lower portion of the bottle, hence submerging cells in the media to allow the transfer of nutrients and wastes or exposure to air for oxygenation.
A widely recognized function of this system is its use as an experimental means for cost-effective and scalable production of cells and cellular products such as G protein–coupled receptors [3], recombinant proteins [4], fusion proteins [5], viral vectors, virus-like particles, and viruses [6,7,8,9] (Table 1). It has been used for in vitro pharmacokinetic/pharmacodynamic (PK/PD) studies for optimal dosing regimens [10] and the evaluation of pharmacological activities of anti-viral drugs and combinations [11]. This state-of-the-art in vitro dynamic system offers multiple advantages over the traditional two-dimensional (2D) tissue culture methods, which have several limitations such as they (1) rely on static drug concentrations, (2) do not allow for serial sampling of adherent cells without disruption, and (3) are usually conducted for up to 5 days due to surface area and media constraints of small tissue culture vessels. These limitations make it difficult to translate in vitro findings from a 2D experimental setting to the clinic. Using our 3DD in vitro system, we can overcome these limitations, as it allows us to mimic human PK profiles of any compound. Using this system, we can simulate the drug concentration-time profiles observed in the plasma and/or in any specific organ in patients. Additionally, this 3DD in vitro system allows for serial sampling of adherent cells without disrupting the remaining cells in the vessel. Finally, as fresh media is continuously infused into the bottle, and as a large surface area supports cell growth, PK/PD studies with serial sampling can be conducted over extended periods of time (at least 2 weeks) [10]. These advantages highlight the utility of this system beyond the mass production of cells and/or their products. It also demonstrates that its use can be extended for many PK/PD applications such as dose and dosing regimen optimization to improve drug efficacy and safety profiles.
As a result of the ability of the 3DD cell culture system to accommodate high-density cell culture, flexible dosing regimens, and PK/PD sampling throughout the course of studies, we highlight two case studies from our laboratory using this system: first, by scaling up experiments evaluating the efficacy of a novel chemotherapy regimen against the HER2-positive/trastuzumab-resistant breast cancer cell line JIMT-1 [12], and second, by assessing the impact of treatment schedule modification of the cardiotoxicity associated with DOX in human cardiomyocytes.
Case Studies With the 3DD BelloCell® System
Application of the 3DD BelloCell® System for Evaluation of Efficacy in Oncology
The three-dimensional dynamic (3DD) BelloCell® cell culture system allows for the relatively long-term growth of adherent cells at a high density (~ 109 cells) in an in vitro 3D environment under dynamic conditions. The unique features of this system have potentially powerful applications in oncology, for the purpose of evaluating tumor growth characteristics over long durations and for assessing the efficacy of anti-tumor agents in a time- and concentration-dependent manner in vitro, thus posing several advantages over standard two-dimensional static cell culture approaches. Successful application of the 3DD BelloCell® system in oncology has been previously demonstrated by our group, for the purpose of overcoming anti-HER2 therapy resistance in breast cancer [12, 13]. Following is a brief background, description of the strategy used, and the key outcomes of the study.
Despite advancements in HER2-targeted therapies for the treatment of HER2-positive breast cancer (BC), development of innate and/or acquired resistance to these therapies poses a major clinical challenge [14, 15]. The primary mechanism of resistance to HER2-targeted therapy involves aberrant activation of the phosphatidylinositol 3-kinase/mammalian target of rapamycin/AKT8 virus oncogene cellular homolog (PI3K/Akt/mTOR) signaling pathway [16, 17]. Given this, we proposed the utilization of a triple combination therapy that includes a small molecule agent targeting the mTOR signaling protein, everolimus (EVE), and a Src family kinase inhibitor, dasatinib (DAS), in combination with a standard cytotoxic agent, paclitaxel (PAC), for overcoming resistance in HER2-positive BC. Our rationale was as follows: although EVE directly inhibits mTOR signaling downstream of the PI3K/Akt pathway, existence of feedback activation loops of upstream signaling proteins such as Akt and Src, due to mTOR inhibition, requires the use of another targeted agent such as DAS, in combination with EVE, which can suppress this loop and yield a stronger cell growth inhibition response than either agent alone [18,19,20]. In addition, the inclusion of PAC as a cytotoxic agent can potentiate the overall anti-tumor response in HER2 therapy–resistant BC, through synergism with the two cytostatic agents [21].
With this rationale, we proceeded with a strategy involving a multi-scale 2D-3DD experimental approach used in combination with quantitative systems pharmacology (QSP)-PK/PD as a mathematical tool, for the evaluation of our proposed combination treatment in the HER2 therapy–resistant BC cell line, JIMT-1 [17] (Fig. 1). We first conducted standard static 2D studies by exposing JIMT-1 cells to the three drugs as single agents and combinations and measuring biomarkers of drug efficacy such as, dynamics of key signaling proteins in the PI3K/Akt/mTOR (such as phosphorylated-Src, phosphorylated-Akt, and phosphorylated-mTOR) and caspase-3 activation pathways, as well as JIMT-1 cell viability. This was done at varying concentration levels and time points (0–96 h), and a QSP protein network model was established using observed data. Next, the 2D experiments were scaled up to the 3DD system, wherein dose-response analyses from a preliminary 3DD pilot study, based on 2D-level concentrations, enabled dose selection for subsequent experiments in the 3DD system. PAC was administered to the 3DD system as a 3-h short-term infusion regimen using a syringe pump, and EVE and DAS were sequentially administered as 72-h continuous infusions 24 h after PAC treatment, followed by a washout of all three drugs. PK sampling for PAC was done up to 96 h from the start of treatment, and samples were analyzed by LC-MS/MS assay. For EVE and DAS, pharmacokinetics in the BelloCell® system were determined by simulations based on the known continuous infusion concentrations of both agents and input and output flowrates of media to the system. The PD biomarkers measured were caspase-3 activation and JIMT-1 cell counts over a time course of 1 and 2 weeks respectively, by sampling BioNOC II™ carriers, on which cells adhere and grow in the system. Our 2D QSP models were then scaled up to link PK and PD responses in the 3DD system. A direct translation of the 2D models to the 3DD models was sufficient at characterizing PD responses in the 3DD system. Moreover, the first-order growth rate constants for JIMT-1 cells in the 2D as well as 3DD systems were very close in magnitude, thus indicating similar growth patterns in both systems at least up to 96 h (Table 2).
Schematic of a combined experimental and computational multi-scale strategy for assessment of oncological efficacy and safety of chemotherapeutic agents using the 3DD BelloCell® system (adapted and modified from [13])
The sequential triple combination of PAC followed by DAS + EVE had substantial cell-killing effects in JIMT-1 cells, with an elevation in caspase-3 activity (as a biomarker of apoptosis) of approximately 5-fold from the no-treatment control arm, and an 8.5-fold decrease in JIMT-1 cell numbers compared with the control arm. In addition, sustained cell-killing effects were observed in the 3DD system, even after cessation of therapy and washout of drugs from the system after a period of about 120 h, up to 2 weeks. With the efficacy of the triple combination therapy successfully demonstrated in the 2D and 3DD systems, and qualification of our 2D QSP-PK/PD models, we then utilized our models to predict responses in the 3DD system for various other treatment scenarios such as PAC, DAS, and EVE as single agents, DAS + EVE dual combination, PAC + DAS + EVE simultaneous treatment, and PAC followed by DAS + EVE with different inter-dose intervals between the sequential combination. The sequential triple combination of PAC followed by DAS + EVE with an inter-dose interval of 72 h was determined to have similar cell-killing effects as the PAC + EVE + DAS simultaneous treatment combination, albeit with a longer time to tumor re-growth after cessation of therapy, which was a desired effect. Inter-dose intervals of 24 and 48 h had similar efficacy as well, however, with shorter time to tumor re-growth periods. Moreover, with a decrease in the concentration levels of all three agents to half, substantial efficacy was still retained with the triple combination, compared with any of the single-agent treatment arms, thus corroborating the overall synergistic effects of this combination treatment at overcoming resistance in JIMT-1 cells.
In summary, the efficacy of our proposed triple combination therapy was successfully demonstrated in JIMT-1 cells with the 3DD system. JIMT-1 cell growth could be followed up to a period of about 2 weeks in this system, even after cessation of therapy and drug washout. With the help of our QSP-PK/PD mathematical modeling tool, responses in the 2D setting could be successfully scaled up to the 3DD system. Moreover, JIMT-1 responses could be predicted in the 3DD system for various other combinations and treatment schedules through model simulations, which may enable model-informed dosing regimen optimization for further in vitro and/or in vivo studies. Thus, our combined experimental and computational multi-scale approach could potentially be utilized as a platform for assessing the efficacy and optimizing dosing regimens of investigational drugs in oncology, with the help of the 3DD in vitro BelloCell® system.
Application of the 3DD BelloCell® System for Evaluation of Chemotherapy-Induced Side Effects
Chemotherapeutic agents remain highly potent treatment options for various forms of cancer; however, serious off-target toxicities can result in significant patient morbidity and mortality rates. One such chemotherapeutic agent is doxorubicin (DOX), which belongs to the anthracycline class of compounds. Although efficacious against a wide variety of cancers, its therapeutic utility is severely limited by its associated dose-dependent cardiotoxicity [23, 24]. DOX has been known to cause dose-limiting cardiomyopathy in patients receiving cumulative doses of 450–500 mg/m2 body surface area, which is a major clinical challenge that remains to be addressed [25]. One of the most feasible strategies to alleviate DOX-induced cardiotoxicity (DIC) is treatment schedule modification [26]. Several pre-clinical and early clinical studies have demonstrated that the administration of DOX using a slow continuous infusion regimen or a once-weekly dose-fractionated regimen causes lesser cardiotoxicity compared with large bolus doses of DOX given once every 3 weeks [26,27,28,29,30]. The rationale is that by maintaining lower peak plasma concentrations and hence lower concentrations of DOX in the heart, the intensity of exposure of cardiomyocytes to DOX is attenuated, thus leading to a reduction in the occurrence of DIC. Despite evidence of reduced cardiotoxicity due to DOX dose schedule modification, the practical implementation of this strategy is limited.
To that end, the ongoing work in our lab involves investigating these findings and quantitatively determining pharmacokinetic parameters linked with cardiotoxicity in order to evaluate optimal dosing regimens of DOX for alleviating cardiotoxicity. We aim to achieve this using the 3DD cell culture system to test various dosing regimens of DOX on an immortalized human cardiomyocyte cell line, AC16 [31]. As described previously, the 3DD system has utility in generating PK/PD data in an in vitro setting by mimicking time-varying drug concentrations in humans or animals. Thus, manipulation of the DOX dosing schedule and measurement of toxicity endpoints in cardiomyocytes using our dynamic 3DD system may enable optimization of dosing regimens of DOX through proof-of-principle studies. A 2D-3DD multi-scale approach is being utilized for this purpose [22, 32], similar to that described in case study I. Briefly, AC16 cells are exposed to varying concentrations of DOX over a time course to assess toxicity markers such as dynamics in key signaling proteins of survival and apoptotic pathways (phosphorylated-AKT, phosphorylated-JNK, phosphorylated-Bcl2, caspases 8, 9, and 3) in cardiomyocytes, AC16 cell viability, and release of cardiotoxicity biomarkers such as B-type natriuretic peptide (BNP) [33] in cell culture medium. The activity of signaling proteins and released cardiotoxicity biomarkers such as BNP are measured using relevant immunoassay techniques. AC16 cell viability is measured using a WST-8 tetrazolium salt-based assay that measures the dehydrogenase activity of cells. A quantitative systems toxicology (QST) model is then established based on these data obtained in the 2D system, through the use of simple or pre-cursor pool based indirect response models, and transit compartment models to account for time delays in signaling [34,35,36,37,38]. Essentially, indirect response models assume a zero-order production rate and first-order removal rate of the protein or biomarker of interest, and are characterized using turnover rate constants with the help of ordinary differential equations [34]. Functions of drug concentration are then included in the equations in order to perturb the system and describe the drug effect. Following the establishment of a 2D QST model, experiments are scaled up to the 3DD system, wherein dose-response studies are first conducted by exposing AC16 cells to continuous infusion regimens of DOX at various dose levels and assessing cell death over time using the crystal violet dye (CVD) nuclear staining method. Moreover, cell samples can also be harvested from the system for measurement of other toxicity biomarkers such as signaling proteins in the apoptosis pathways. From preliminary pilot studies, intermediate continuous infusion dose levels are then selected, such that they induce substantial toxicity, and are fractionated into multiple regimens administered as 1-h short-term infusions at every 24, 48, 72, or 96 h, while mimicking human PK based on information such as the terminal half-life and plasma protein binding of DOX. Dose fractionation is performed in order to obtain varying PK profiles of DOX while keeping the total cumulative DOX dose (and area under the concentration curve (AUC)) constant for all regimens. Following the administration of DOX via various dosing schedules, toxicity biomarkers in AC16 cardiomyocytes are then evaluated over a two-week time course and relationships are established between PK parameters such as peak or trough concentrations and AUCs as drivers of toxicity, by utilizing the established 2D QST model as a link between DOX PK and toxicodynamic (TD) responses in the 3DD system. A direct translation of the 2D TD model to the 3DD system is assumed to be applicable in this case because the first-order growth rate constants of the initial growth phase of AC16 cells in both the 2D and 3DD systems are very similar, as assessed in preliminary studies (Table 2), exhibiting similar growth patterns in both systems, at least up to 96 h. Area under the effect (TD response) curves in the 3DD system are then plotted against various PK metrics such as peak or trough concentrations and AUCs, to evaluate correlations between PK parameters and drug toxicity. Preliminary results from our treatment schedule modification studies with AC16 cells in the 3DD system indicated peak concentrations of DOX as drivers of cardiotoxicity, which is in close agreement with the literature [22, 32]. The QST-PK/PD mathematical models established using data from the 2D and 3DD systems can also aid in informing dosing regimen optimization for DOX at alternate dose levels and schedules, through model simulations, which may then enable model-informed design of further in vitro studies in the 3DD system and/or in vivo studies. Additional studies are ongoing to incorporate a range of cumulative dose levels of DOX in order to establish relationships between total cumulative DOX dose and cardiotoxicity for various treatment regimens in the 3DD system. Following the establishment of optimal dosing regimens of DOX for the alleviation of cardiotoxicity, the treatment regimens will then be evaluated in breast cancer cell lines in the 3DD system, in order to evaluate the safety-efficacy balance of DOX with the modified treatment schedules. This will ensure that DOX oncological efficacy is not compromised due to treatment schedule modification. Furthermore, the 3DD system will also be utilized to assess the enhancement of cardioprotection by co-administering a cardioprotective agent, dexrazoxane, an FDA approved cardio-protectant used in breast cancer patients [39, 40] in combination with our optimized dosing regimens of DOX in the 3DD system.
The utility of the 3DD system at assessing optimal dosing regimens for the alleviation of DOX-induced cardiotoxicity has thus been established, as demonstrated in our preliminary studies [22, 32]. Moreover, our 2D scaled up toxicity model predicted cellular response in AC16 cardiomyocytes well, for prolonged durations, in the 3DD system, thus enabling us to utilize a multi-scale 2D-3DD approach for proof-of-principle studies. This may be particularly useful in cases where rich sampling and measurement of biomarkers of toxicity/efficacy might not be logistically or technically feasible in the 3DD system, given a wide range of dose levels and treatment arms to be tested. In that case, 2D-level TD/PD models may be utilized to extrapolate responses in the 3DD system, provided extrapolation has been validated for the cell line and drug of interest. In summary, our combined experimental and computational QST-PK/PD modeling and simulation approach utilizing the 3DD cell culture system may serve as a useful tool for the determination of toxicity and/or efficacy indices of developmental drugs in vitro, thus enabling model-informed design of further studies in an in vivo setting.
Discussion
Some major advantages of the BelloCell® system for the studies described above were that we were able to conduct experiments over longer time spans compared with traditional two-dimensional (2D) static cell culture and administer drugs in a manner where we could simulate different pharmacokinetic profiles. Moreover, the BelloCell® promotes three-dimensional (3D) cell growth, rather than growth as a monolayer, which may be more reflective of in vivo conditions.
Generally, our plate-based cell viability studies last up to 5 days, due to the small surface area available for cells to grow and depletion of nutrients in media beyond this time frame [12]. In contrast, the BelloCell® can adequately support high-density cell growth, as described in publications by Hu et al [6] and Lu et al. [4] where the maximum density of cultured insect cells reached final yields of approximately 3.8–4.6 × 109 cells. Moreover, nutrient supply and waste removal in the BelloCell® are controlled with the help of peristaltic pumps that ensure cells continuously receive fresh nutrients and that wastes do not accumulate, thus supporting the long-term growth of cells contained within the system. The BelloCell® system’s accommodation of studies spanning several weeks was particularly important in our experiments described in case study I, where we aimed to assess the ability of our chosen chemotherapy regimen to control re-growth of JIMT-1 cells up to 2 weeks post-drug administration. As discussed previously, it would not be feasible to conduct these studies with traditional 2D cell culture techniques, as the duration of experiments would be restricted to approximately 5 days, which would not be an adequate time frame where we could draw conclusions regarding the long-term effects on JIMT-1 cell viability following drug exposure. Another important advantage of the BelloCell® was the ability to sample carrier flakes to assess pharmacodynamic endpoints without perturbing the system; this allowed us to monitor day-to-day changes in cell viability, and thus evaluate drug efficacy over time. This study demonstrates the utility of the BelloCell® for oncology studies, as drugs can be dosed for several days and trends in cell growth following treatment can be monitored over extended periods of time.
Simulation of clinically relevant pharmacokinetic profiles in the BelloCell® was first described in a publication by Brown et al. [10], where dose fractionation studies were conducted to optimize dosing regimens and assess the efficacy of the anti-viral compound MK-4519 against hepatitis C virus (HCV). The results of this study confirmed that the BelloCell® was capable of serving as an in vitro method for carrying out PK/PD studies and could successfully identify the relationships between drug dosing/administration schedules and efficacy. In our experiments, we have applied a similar approach to optimize doxorubicin (DOX) dosing to minimize cardiotoxicity. The ability to recreate various clinically relevant pharmacokinetic profiles with the BelloCell® was especially relevant for case study II, where we fractionated DOX doses to obtain varying PK profiles and assessed respective AC16 TD responses. Although the total cumulative DOX dose and AUC were identical for each dose-fractionated DOX treatment arm, the differences in drug administration schedules yielded distinct peak concentrations, which were later identified as the factor driving cardiotoxicity. Case study II presents a clear example supporting the use of the BelloCell® system for toxicology studies. The system can be used as an in vitro technique to identify what PK parameters are responsible for toxicity, and hence possibly modified, in an effort to mitigate drug-induced toxicities before proceeding with in vivo studies.
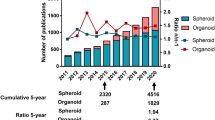
Traditionally, in vitro studies to screen drugs and assess their efficacy have relied on two-dimensional (2D) cell culture techniques, where cells are grown as a monolayer on a flat surface [41]. A drawback of this method, particularly important for oncology research, is that these conditions are not reflective of physiological conditions, as factors such as cell morphology, cell to cell communication, and environmental conditions including oxygen and nutrient gradients differ from those observed in vivo [41, 42]. As a result, drug candidates that have demonstrated efficacy in in vitro pre-clinical studies may fail when moving onto clinical studies [41]. In an effort to improve the physiological relevance of in vitro assays, and thus the translatability of results, three-dimensional (3D) cell culture techniques are being developed. These platforms allow cells to grow in clusters and interact with neighboring cells, creating an environment that better represents in vivo conditions [42, 43]. Moreover, 3D cell cultures are more stable and have longer lifespans compared with 2D cultures, thus allowing long-term studies [41]. In our experiments, we have used BelloCell® as a three-dimensional cell culture technique. This is a result of cell adhesion to BioNOC II™ macro-porous carriers contained within the bottles. The carriers are composed of 20–25 layers of PET fibers, with each layer structured as a grid. Cells grow along the fibers and between the spaces of the grids, thus creating a multi-layer culture that increases cell to cell interactions [44]. Although this cell culture technique may not adequately capture all physiological conditions, we believe that the morphology of cells and increased cellular interactions will be a closer representation of in vivo conditions compared with 2D cell cultures, thus allowing us to evaluate the safety and efficacy of drugs and optimize their dosing in a 3D in vitro setting before starting in vivo studies.
Limitations
Although the BelloCell® is a versatile system, it has few limitations that are worth noting. The first is that as very few BioNOC II™ carriers (3–6 out of a total 865 ± 5%) [1] are sampled to obtain cell counts, there may be some variability depending on cell distribution and attachment to the carriers. In an effort to account for some of this variability, we sample carriers from different parts of the BelloCell® bottle. Moreover, some considerations that may reduce variability due to human error when counting on a hemocytometer include the use of an automatic cell counter or colorimetric assays. Alternatively, cell counts can be estimated by measurement of glucose uptake or consumption and conversion to cell number, as described in the publications by Lu et al. and Hu et al. [4, 6]. In addition, high drug losses may occur due to the length of input tubing or if drugs have an affinity for binding to the plastic of the tubing. In our experiments, we attempted to correct this by priming the tubing to assure that the appropriate volume of the drug would be infused into the system and preparing fresh drug stocks before each scheduled dose to decrease the length of time that drug would have to bind to tubing. Another consideration is that this system may not be the most suitable for the measurement of secreted biomarkers, as these may be diluted due to the large volume of media contained within the BelloCell® bottle (approximately 500 mL) and the influx of fresh media and efflux of wastes from the system. Finally, another limitation of this system is that although cells grow in three dimensions, conditions present in vivo such as the cell microenvironment and interactions with basement membranes and the extracellular matrix may not be adequately captured by the BelloCell®. Nevertheless, we believe that the increased cellular interactions due to multi-layered cell growth on BelloCell® carriers are more reflective of tumor/tissue growth in vivo compared with 2D cell culture. Despite these challenges, we believe that the BelloCell® system is a useful in vitro cell culture technique to assess drug efficacy and safety prior to in vivo studies.
Conclusion
The studies presented above demonstrate the versatility of the BelloCell® system. Although the system was initially designed as a technique for high-density cell culture and mass production of cell products, its ability to accommodate long-term studies and simulate clinically relevant pharmacokinetic profiles makes it useful for in vitro studies to evaluate the efficacy and safety of chemotherapy drugs.
Change history
18 April 2023
A Correction to this paper has been published: https://doi.org/10.1007/s40495-023-00315-1
References
CESCO. BelloCell High-Density, Disposable Cell Culture System. CESCO Bioengineering Co., LTD.; 2008.
Chang K-M. Cell-cultivating device. Taichung (TW): Cesco Bioengineering, Inc; 2006.
Ho L, Greene CL, Schmidt AW, Huang LH. Cultivation of HEK 293 cell line and production of a member of the superfamily of G-protein coupled receptors for drug discovery applications using a highly efficient novel bioreactor. Cytotechnology. 2004;45(3):117–23.
Lu JT, Chung YC, Chan ZR, Hu YC. A novel oscillating bioreactor BelloCell: implications for insect cell culture and recombinant protein production. Biotechnol Lett. 2005;27(15):1059–65.
Wang IK, Hsieh SY, Chang KM, Wang YC, Chu A, Shaw SY, et al. A novel control scheme for inducing angiostatin-human IgG fusion protein production using recombinant CHO cells in a oscillating bioreactor. J Biotechnol. 2006;121(3):418–28.
Hu YC, Lu JT, Chung YC. High-density cultivation of insect cells and production of recombinant baculovirus using a novel oscillating bioreactor. Cytotechnology. 2003;42(3):145–53.
Huang KS, Lo WH, Chung YC, Lai YK, Chen CY, Chou ST, et al. Combination of baculovirus-mediated gene delivery and packed-bed reactor for scalable production of adeno-associated virus. Hum Gene Ther. 2007;18(11):1161–70.
Chen YH, Wu JC, Wang KC, Chiang YW, Lai CW, Chung YC, et al. Baculovirus-mediated production of HDV-like particles in BHK cells using a novel oscillating bioreactor. J Biotechnol. 2005;118(2):135–47.
Toriniwa H, Komiya T. Japanese encephalitis virus production in Vero cells with serum-free medium using a novel oscillating bioreactor. Biologicals. 2007;35(4):221–6.
Brown AN, McSharry JJ, Adams JR, Kulawy R, Barnard RJO, Newhard W, et al. Pharmacodynamic analysis of a serine protease inhibitor, MK-4519, against hepatitis C virus using a novel in vitro pharmacodynamic system. Antimicrob Agents Chemother. 2012;56(3):1170–81.
Brown AN, Liu L, Rodriquez JL, Zhao L, Schuster L, Li E, et al. Sofosbuvir (SOF) suppresses ledipasvir (LDV)-resistant mutants during SOF/LDV combination therapy against genotype 1b hepatitis C virus (HCV). Sci Rep. 2017;7(1):14421.
Ande A, Vaidya TR, Tran BN, Vicchiarelli M, Brown AN, Ait-Oudhia S. Utility of a novel three-dimensional and dynamic (3DD) cell culture system for PK/PD studies: evaluation of a triple combination therapy at overcoming anti-HER2 treatment resistance in breast cancer. Front Pharmacol. 2018;9:403.
Vaidya TR, Ande A, Ait-Oudhia S. Combining multiscale experimental and computational systems pharmacological approaches to overcome resistance to HER2-targeted therapy in breast cancer. J Pharmacol Exp Ther. 2019;369(3):531–45.
Yarden Y. Biology of HER2 and its importance in breast cancer. Oncology. 2001;61(Suppl 2):1–13.
Pohlmann PR, Mayer IA, Mernaugh R. Resistance to trastuzumab in breast cancer. Clin Cancer Res. 2009;15(24):7479–91.
Wilks ST. Potential of overcoming resistance to HER2-targeted therapies through the PI3K/Akt/mTOR pathway. Breast. 2015;24(5):548–55.
Koninki K, et al. Multiple molecular mechanisms underlying trastuzumab and lapatinib resistance in JIMT-1 breast cancer cells. Cancer Lett. 2010;294(2):211–9.
O'Reilly KE, Rojo F, She QB, Solit D, Mills GB, Smith D, et al. mTOR inhibition induces upstream receptor tyrosine kinase signaling and activates Akt. Cancer Res. 2006;66(3):1500–8.
O'Brien NA, McDonald K, Tong L, von Euw E, Kalous O, Conklin D, et al. Targeting PI3K/mTOR overcomes resistance to HER2-targeted therapy independent of feedback activation of AKT. Clin Cancer Res. 2014;20(13):3507–20.
Yori JL, Lozada KL, Seachrist DD, Mosley JD, Abdul-Karim FW, Booth CN, et al. Combined SFK/mTOR inhibition prevents rapamycin-induced feedback activation of AKT and elicits efficient tumor regression. Cancer Res. 2014;74(17):4762–71.
Haltia UM, Andersson N, Yadav B, Färkkilä A, Kulesskiy E, Kankainen M, et al. Systematic drug sensitivity testing reveals synergistic growth inhibition by dasatinib or mTOR inhibitors with paclitaxel in ovarian granulosa cell tumor cells. Gynecol Oncol. 2017;144(3):621–30.
Abstracts for the Ninth American Conference on Pharmacometrics (ACoP9). J Pharmacokinet Pharmacodyn 2018:3–134.
Bonadonna G, Monfardini S, de Lena M, Fossati-Bellani F. Clinical evaluation of adriamycin, a new antitumour antibiotic. Br Med J. 1969;3(5669):503–6.
Von Hoff DD, et al. Risk factors for doxorubicin-induced congestive heart failure. Ann Intern Med. 1979;91(5):710–7.
Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97(11):2869–79.
Lum BL, Svec JM, Torti FM. Doxorubicin: alteration of dose scheduling as a means of reducing cardiotoxicity. Drug Intell Clin Pharm. 1985;19(4):259–64.
Pacciarini MA, Barbieri B, Colombo T, Broggini M, Garattini S, Donelli MG. Distribution and antitumor activity of adriamycin given in a high-dose and a repeated low-dose schedule to mice. Cancer Treat Rep. 1978;62(5):791–800.
Legha SS, Benjamin RS, Mackay B, Ewer M, Wallace S, Valdivieso M, et al. Reduction of doxorubicin cardiotoxicity by prolonged continuous intravenous infusion. Ann Intern Med. 1982;96(2):133–9.
Weiss AJ, et al. Studies on adriamycin using a weekly regimen demonstrating its clinical effectiveness and lack of cardiac toxicity. Cancer Treat Rep. 1976;60(7):813–22.
Chlebowski RT, et al. Adriamycin given as a weekly schedule without a loading course: clinically effective with reduced incidence of cardiotoxicity. Cancer Treat Rep. 1980;64(1):47–51.
Davidson MM, et al. Novel cell lines derived from adult human ventricular cardiomyocytes. J Mol Cell Cardiol. 2005;39(1):133–47.
Vaidya T, et al. Multi-scale and quantitative systems toxicological analysis of doxorubicin action on human cardiomyocytes in clinical pharmacology & therapeutics. Hoboken: Wiley; 2019.
Skovgaard D, Hasbak P, Kjaer A. BNP predicts chemotherapy-related cardiotoxicity and death: comparison with gated equilibrium radionuclide ventriculography. PLoS One. 2014;9(5):e96736.
Dayneka NL, Garg V, Jusko WJ. Comparison of four basic models of indirect pharmacodynamic responses. J Pharmacokinet Biopharm. 1993;21(4):457–78.
Sharma A, Ebling WF, Jusko WJ. Precursor-dependent indirect pharmacodynamic response model for tolerance and rebound phenomena. J Pharm Sci. 1998;87(12):1577–84.
Lobo ED, Balthasar JP. Pharmacodynamic modeling of chemotherapeutic effects: application of a transit compartment model to characterize methotrexate effects in vitro. AAPS PharmSci. 2002;4(4):E42.
Sun YN, Jusko WJ. Transit compartments versus gamma distribution function to model signal transduction processes in pharmacodynamics. J Pharm Sci. 1998;87(6):732–7.
Mager DE, Wyska E, Jusko WJ. Diversity of mechanism-based pharmacodynamic models. Drug Metab Dispos. 2003;31(5):510–8.
Hasinoff BB, et al. Chemical, biological and clinical aspects of dexrazoxane and other bisdioxopiperazines. Curr Med Chem. 1998;5(1):1–28.
Pfizer, Zinecard (dexrazoxane for injection) [package insert]. 2012: U.S. Food and Drug Administration website.
Antoni D, Burckel H, Josset E, Noel G. Three-dimensional cell culture: a breakthrough in vivo. Int J Mol Sci. 2015;16(3):5517–27.
Pampaloni F, Reynaud EG, Stelzer EH. The third dimension bridges the gap between cell culture and live tissue. Nat Rev Mol Cell Biol. 2007;8(10):839–45.
Duval K, et al. Modeling physiological events in 2D vs. 3D cell culture. Physiology (Bethesda). 2017;32(4):266–77.
Vaccixcell, BioNOC II Cell Culture Carriers. Vaccixcell.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pharmacometrics and Quantitative System Pharmacology
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vaidya, T.R., Franco, Y.L. & Ait-Oudhia, S. A Three-dimensional and Dynamic (3DD) Cell Culture System for Evaluation of Pharmacokinetics, Safety and Efficacy of Anti-cancer Drugs. Curr Pharmacol Rep 5, 460–467 (2019). https://doi.org/10.1007/s40495-019-00198-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40495-019-00198-1