Abstract
Gastrointestinal (GI) cancers are a significant global health concern with diverse etiologies and limited treatment options. Ellagic acid (EA), a natural polyphenolic compound, exhibits promising anticancer properties against various GI malignancies. In this article, we have reviewed recent research on the anticancer potential of EA across esophageal, gastric, colorectal, pancreatic, and liver cancers. In esophageal cancer, EA inhibits the formation of O6-methylguanine (O6-meGua) adducts induced by carcinogens like N-nitrosomethylbenzylamine (NMBA), thereby suppressing tumor growth. Additionally, EA inhibits STAT3 signaling and stabilizes tumor suppressor proteins, showing potential as an anti-esophageal cancer agent. In gastric cancer, EA regulates multiple pathways involved in cell proliferation, invasion, and apoptosis, including the p53 and PI3K-Akt signaling pathways. It also demonstrates anti-inflammatory and antioxidant effects, making it a promising therapeutic candidate against gastric cancer. In colorectal cancer (CRC), EA inhibits cell proliferation, induces apoptosis, and modulates the Wnt/β-catenin and PI3K/Akt pathways, suggesting its efficacy in preventing CRC progression. Furthermore, EA has shown promise in pancreatic cancer by inhibiting nuclear factor-kappa B, inducing apoptosis, and suppressing epithelial–mesenchymal transition. In liver cancer, EA exhibits radio-sensitizing effects, inhibits inflammatory pathways, and modulates the tumor microenvironment, offering potential therapeutic benefits against hepatocellular carcinoma. Studies on EA potential in combination therapies and the development of targeted delivery systems are required for enhanced efficacy against gastrointestinal cancers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Ellagic acid (EA) demonstrates promising anticancer properties across various gastrointestinal (GI) malignancies. EA inhibits carcinogen-induced adduct formation and STAT3 signaling in esophageal cancer. |
In gastric cancer, EA regulates the p53 and PI3K-Akt pathways and exhibits anti-inflammatory effects. EA modulates the Wnt/β-catenin and PI3K/Akt pathways in colorectal cancer, preventing progression. |
EA induces apoptosis and suppresses the epithelial–mesenchymal transition in pancreatic cancer. EA shows radio-sensitizing effects and inhibits inflammatory pathways in liver cancer. |
Further research on EA in combination therapies and targeted delivery systems is needed. |
Introduction
Gastrointestinal (GI) cancers are diverse groups of digestive tract cancers that exhibit unique features based on the location of the tumor's origin. Dietary habits, obesity, and lifestyle variables are considered factors driving the rise in the incidence of GI tract cancers worldwide [1]. Globally, GI cancer is the leading cause of cancer-related mortality and the most frequently diagnosed malignancy. The five leading GI tract malignancy types—colorectal, gastric, liver, esophageal, and pancreatic cancers—have a high mortality rate owing to factors like metastasis, delayed detection, and recurrence after surgery [2]. Although anticancer agents remain the mainstay of treatment for cancer, numerous studies have shown that the effectiveness of “standard” therapies is limited [3]. Therefore, there is a pressing need to discover novel and viable treatment strategies for GI cancer. Over the past several years, the use of natural products has garnered significant attention owing to their ability to prevent and effectively treat a variety of human malignancies [4, 5].
One such naturally occurring polyphenolic substance from the family of ellagitannins (ETs) is ellagic acid (EA), which is frequently found in a wide range of plant-based sources, including pomegranate bark, fairy herb, walnut kernel, raspberry, strawberries, myrrh, and loquat leaf [6]. EA is a derivative of chromene-dione (C14H6O8), which can present in diverse forms, including free, glycosylated, and mixed forms of ETs [7,8,9]. Over the past few decades, EA has attracted attention owing to its wide spectrum of biological effects, including anti-inflammatory [10], anti-oxidant [11], anti-allergic [12], and anti-mutagenic [13] properties, as well as potential health advantages like gastroprotective [14], cardioprotective [15], neuroprotective [16, 17], and hepatoprotective [18, 19] effects. Additionally, EA has demonstrated multifaceted mechanisms for treating a range of human malignancies [20]. In GI malignancies, EA is reported to suppress proliferation [21], migration [22], and invasiveness [23] while inducing apoptosis [21, 24] to limit the emergence of therapeutic resistance. Thus, to provide a comprehensive evaluation for prospective future research on the treatment of GI cancers, we discuss here the most recent results from preclinical investigations about the pharmacological mechanisms behind the positive aspects of EA against GI tumors. The objective of this review article is to evaluate the chemopreventive and therapeutic properties of EA against GI cancers and to explore its potential for improved treatment outcomes through synergistic effects with nanotechnology and conventional therapies.
Chemistry and Pharmacokinetics
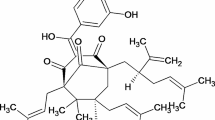
EA (2,3,7,8-tetrahydroxy[1]-benzopyranol[5, 4, 3-cde]benzopyran-5,10-dione) is a naturally occurring polyphenol found in several fruits, nuts, and vegetables. Pomegranates, blackberries, strawberries, raspberries, and walnuts are particularly high in this nutrient [25]. Having a molecular weight of 302.197 g mol−1, it is a very thermostable molecule with a melting point of 350 °C. It is soluble in caustic potash but insoluble in water, alcohol, and ether [17]. It structurally consists of two lactones that represent the hydrophilic domain and form hydrogen bonds with four phenolic groups, which represent the lipophilic domain, and four rings that represent the hydrophilic domain [26].
A significant amount of EA exists in the gastrointestinal tracts of both humans and animals, in addition to the naturally occurring unbound EA present in plant-based diets [6]. Ellagannins, dietary polyphenolic compounds, are broken down either enzymatically or non-enzymatically, resulting in EA synthesis [27]. EA's hydrophobic nature and extremely poor water solubility lead to its limited absorption in the gastrointestinal tract [28]. Furthermore, multiple studies show that EA has qualities that can decrease cell proliferation and potentially inhibit cancer formation [9]. The chemical structure of EA is shown in Fig. 1.
EA functions by modulating a number of pathways, which include activating the antioxidant response via nuclear erythroid 2-related factor 2 (Nrf2) [9, 29] inhibiting proinflammatory agents, such as cyclooxygenase (COX-2) and cytokines, by nuclear factor-kappa B (NF- B) [30], altering the expression of several growth factors, such as platelet-derived growth factor (PDGF), transforming growth factor beta (TGF-β), and hepatic growth factor (HGF), depletion of adhesion molecules, such as vascular cell adhesion molecule-1 (VCAM-1) and intercellular adhesion molecule-1 (ICAM-1), among others [31], and modulating several cell survival/cell-cycle genes, such as cyclin D1 and E, p21, B-cell lymphoma 2 (Bcl-2), and Bcl-2-associated X protein (Bax) [32]. As a potential antioxidant agent, it scavenges reactive oxygen species (ROS), and by upregulating of Nrf2, indirectly protects hepatic cells and downregulation of Kelch-like ECH-associated protein 1 (Keap1) controls the induction of phase I and phase II detoxifying enzymes [33]. Nrf2 is a redox-sensitive transcription factor known as the cell's principal antioxidant response regulator [32]. Moreover, EA increases reduced glutathione (GSH), which is critical for cellular defense against oxidative stress and liver damage, and increases the activity of phase II detoxifying enzymes [18].
Major Gastrointestinal Cancer
Esophageal Cancer
As a chemopreventive agent, EA prevents the development of cancer cells and the bioactivation of carcinogens by binding to DNA [34]. For instance, the development of esophageal tumors in rats is intimately associated with the creation and persistence of O6-methylguanine (O6-meGua) adducts. The identification of these adducts or conjugates in the DNA of patients indicates the role of nitrosamines in esophageal cancer [35].
The carcinogenic impact of N-nitrosomethylbenzylamine (NMBA) is dependent on metabolic activation, making it a procarcinogen. EA inhibits the growth of NMBA tumors in the esophagus of Fischer 344 rats. After 20 and 27 weeks of the bioassay [36, 37], EA can considerably lower (21–55%) the normal number of NMBA-induced esophageal tumors when given in a semi-purified diet at dosages of 0.4 and 4 g/kg. This suppression is associated with decreased esophageal DNA O6-meGua adduct formation generated by NMBA, indicating that the berries affect NMBA metabolism and lessen DNA damage [38]. Since esophageal squamous cell carcinoma (ESCC) has overexpressed and overactivated STAT3, inhibiting STAT3 signaling may be a useful tactic in the development of anti-ESCC medications. STAT3 can also encourage the migration, invasion, and proliferation of ESCC cells [39]. In line with earlier research on HeLa and PC3 cells, EA significantly reduced STAT3 activation in ESCC cells [40]. In the present investigation, it was discovered that EA inhibits STAT3 in ESCC cells to produce its anti-tumor effects. By blocking RNF6 expression, EA may stabilize SHP-1 in ESCC cells through a mechanism [41].
When tested against HM251 and HM233, ellagic acid had the lowest minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) values, at 2.5 and 5 mg/mL, respectively [42]. After 48 h, the polyphenols showed a reduction in cell viability percentage that was concentration-dependent. These polyphenols probably function well as anti-colitic agents [42]. EA suppresses colon cancer growth via the AMPK/mTOR pathway while also inducing apoptosis and protective autophagy [43].
Gastric (Stomach) Cancer
Gastric cancer (GC) is still a major global health issue. Studies conducted recently have demonstrated that EA suppresses the expression of several factors, including COX1, COX2, c-myc, snail, and twist1 to prevent acid-enhanced GC cell migration and invasion [23, 44]. Furthermore, EA has been shown to suppress the migration and proliferation of human GC AGS cells, cause apoptosis, and lower the expression of inflammatory genes [45]. The analysis performed utilizing tissue samples has also demonstrated and established the safety aspects associated with EA use. Furthermore, the human disease Helicobacter pylori and GC are closely associated. Helicobacter pylori has been designated by the World Health Organization (WHO) as a group I carcinogen. Remarkably, several studies have demonstrated that EA has anti-H. pylori action and has tremendous potential for the treatment and prevention of H. pylori [46]. EA anti-GC primarily regulated the p53 signaling pathway, the PI3K-Akt signaling pathway, JUN, CASP3, HSP90AA1, VEGFA, HRAS, CDH1, MAPK3, CDKN1A, SRC, CYCS, BCL2L1, and CDK4 pathways. These pathways are involved in the induction of apoptosis and the inhibition of tumor angiogenesis, cell cycle, proliferation, invasion, and migration. It shows that EA has a lot of potential for both treating and avoiding GC and offers a theoretical framework for more research on EA's anti-GC effects. Additionally, it significantly decreased MMP-2 and MMP-9 expression and activity. Furthermore, it was shown that EA therapy promoted cancer cell death and decreased inflammation due to modulations of gene expressions associated with apoptosis, such as P53 and BAX. Other apoptotic genes, including APAF1 and BCL2, are also modulated during this treatment [47]. EA has proven to have anti-inflammatory [10], antioxidant [11], and anticancer properties. Thirteen major EA targets were found via network pharmacology analysis; these could also be the main targets of EA anti-GC. Among these, tumor protein p53 (TP53), a widely recognized tumor inhibitor gene, is the most commonly mutated gene in gastric cancer, making up roughly 50% of cases [48].
Colorectal Cancer
Colorectal cancer (CRC) is the third most frequent and second most fatal cancer around the globe [2]. Although CRC is primarily associated with industrialized countries, less developed countries are seeing an increase in colorectal cancer cases due to the widespread adoption of Western lifestyles and activities. The advent of drug resistance and frequent recurrence are indicative of the inadequacy of the current treatment regimens. Thus, the disease places a significant burden on the world in terms of complications, death, treatment side effects, use of healthcare resources, and medical expenses [49, 50]. In this regard, several published studies conducted by independent researchers worldwide have demonstrated the significant potential of natural compounds as a source of novel activities for anti-CRC therapeutic leads [51].
EA has demonstrated promising anticancer activity against CRC [52]. Preclinical research has identified multiple pathways by which EA prevents CRC development. In human colon cancer HT-29 and HCT-116 cells, EA was able to successfully decrease cell viability, alter the levels of Wnt/β-catenin pathway proteins, and downregulate CDK8 expression and activity [53]. EA increased the growth of SW480 and SW620 cells [54]. EA has been found to produce a notable delay in CRC advancement in an observation validated by in vivo analysis [55]. On the other hand, in colon adenocarcinoma HCT-15 cells, EA is reported to impede proliferation and encourage apoptosis by inactivating PI3K/Akt signaling [21]. Likewise, it also displayed antiproliferative and proapoptotic activity in Caco-2 (K-Ras+/p53−) and HCT-116 (K-Ras-/p53+) colorectal cell lines. Additionally, EA is identified to decrease K-Ras expression while simultaneously inhibiting the phosphorylation of Akt at both Thr308 and Ser473 positions. Consequently, this suggests that the cellular genetic background (K-Ras−/p53−) was unlikely to place restrictions on the implementation of EA as a CRC therapeutic target [56]. EA has also been demonstrated to promote cell cycle arrest and apoptosis in human colon cancer HCT-116 cells through the TGF-β1/Smad3 pathway [24]. The effect of EA on the inhibition of Drp-1 (a mitochondrial fission protein) is also identified to promote mitochondria-mediated apoptosis in colorectal cancer cell line HCT116 and breast adenocarcinoma cell line MCF7. It culminates with mitochondrial membrane potential loss, a reduction in respiratory efficiency, and cell cycle arrest [57].
In a clinical trial with 35 patients with colorectal cancer, daily supplementation with 900 mg of pomegranate extract significantly modulated the expression of CRC-related genes (CD44, CTNNB1, CDKN1A, EGFR, TYMs) in colon tissues. These effects counterbalanced protocol impacts and were independent of individual urolithin metabotypes and colon tissue levels of urolithins and ellagic acid [58]. By modifying gene expression, EA and urolithin-A and urolithin-B (Uro-A and Uro-B), at amounts attainable in the gastrointestinal lumen from diet, may help prevent colon cancer. Exposure to EAs induced apoptosis, accelerated cell cycle arrest, and elevated the generation of reactive oxygen intermediates [59]. EA may be a new drug that makes colorectal cancer cells more sensitive to 5-fluorouracil [60]. In addition to modulating the cell cycle, translocating Bax to the mitochondrial fraction of cells, activating caspase-8, and lowering proliferating cell nuclear antigen (PCNA) expression, EA also suppressed the proliferation of HCT-116 and CaCo-2 cell lines. The results of the present investigation provide insight on the possible therapeutic application of EA in the development of colon cancer linked to obesity [56]. A study by Ni et al. [43] also revealed the potential of EA in impeding the progression of colon cancer, stimulating apoptosis and protective autophagy through the AMPK/mTOR signaling pathway. Owing to its broad range of effects, research exploring the therapeutic potential (Fig. 2) of EA, either on its own or in conjunction with conventional therapies, is necessary to ascertain its viability in prevention and management of CRC.
Figure shows that EA (C14H6O8) induces apoptosis via both intrinsic and extrinsic pathways. It activates death receptors (TNF, TRAILR, FAS), forming the DISC complex and activating caspase 8. Ellagic acid also impacts the PI3K/Akt/mTOR pathway, causing cytochrome c release from mitochondria, which binds Apaf-1 to form the apoptosome, activating caspase 9 and then caspase 3, leading to apoptosis. It modulates Bcl-2 family proteins, inhibits the STAT3/NF-kβ pathway to reduce VEGF expression, and influences transcription factors FOXO3a and RUNX3, collectively promoting apoptotic cell death
Pancreatic Cancer
EA suppresses the nuclear factor-kappa B and cyclooxygenase 2 (COX-2) in a variety of cell types, including pancreatic cancer cells, and limits the effects of proinflammatory drugs. This is validated in an in vitro study [61]. Inducing apoptosis in pancreatic cancer cells with EA involves the activation of caspase-3 and caspase-9, rather than caspase-8. EA also inhibits pancreatic cancer cells' epithelial mesenchymal transition (EMT), which restricts migration. EA raised the expression of E-cadherin but lowered that of matrix metalloproteinase-9, TGF-β, and matrix metalloproteinase-2 [22]. Pluripotent stem cells (PSCs) and fundamental cell functions are inhibited by EA. It acts as an anti-diabetic agent by influencing β-pancreatic cells [62]. Through the suppression of the Akt, Shh, and Notch pathways, EA can prevent the growth, angiogenesis, and metastasis of pancreatic cancer [63]. T2DM is associated with increased inflammatory markers. Overall tissue reparative and protective characteristics of the EA extract are demonstrated by the increased β-cell population and improved glucose homeostasis. Therefore, EA might be a novel therapeutic strategy for helping people with T2DM maintain normoglycemia. When pancreatic stellate cells were exposed to either platelet-derived growth factor or TGF-β1, EA prevented them from producing reactive oxygen species [64]. EA prevented extracellular signal-regulated kinase and Akt from being activated downstream of the tyrosine phosphorylation of the PDGF beta-receptor caused by PDGF-BB. EA prevented nuclear factor-kappa B from being activated by tumor necrosis factor (TNF)-alpha and interleukin-1 beta (IL-1β), but not mitogen-activated protein kinases or activator protein-1 [65].
Liver Cancer
Liver cancer continues to pose a global health threat; with an increasing incidence rate, it is expected to affect over 1 million individuals yearly by 2025 [66]. Hepatocellular carcinoma (HCC) is one of the most common types of primary liver cancer, accounting for > 90% of the liver cancer-related global health burden [67]. Hepatitis C and B virus infections, and chronic liver illnesses such as cirrhosis, fibrosis, and non-alcoholic steatohepatitis related to metabolic syndrome, are the primary risk variables for HCC [68]. Of all HCCs, about 25% have possibly responsive mutations that have not yet been implemented in clinical settings [66]. Molecular information that necessitates tissue or liquid biopsies is currently posing a challenge to diagnosis based on noninvasive criteria. As a result, the majority of liver malignancies are discovered when they have progressed beyond the point at which early surgical resection, liver transplantation, or percutaneous ablation are viable therapeutic choices. Further, the first-line therapeutic options like multi-kinase inhibitors only provide limited clinical advantage for patients with advanced liver cancer [69]. Therefore, there is an unmet need to identify alternate therapeutic agents to combat liver cancer.
EA has shown potential in the prevention and treatment of liver cancer [18]. The radio-sensitizing effect of EA has been reported on the growth of the HepG2 cells via enhancement of reactive oxygen species, increased expression of p53, and cleavage of caspase-3 protein for the induction of apoptosis. EA is also reported to decrease the levels of inflammatory markers TNF-α and IL-6 as well as survival markers p-Akt, p-NF-kB, and p-STAT3 [70]. Zaazaa et al. [71] further confirmed the effectiveness of EA in reducing the risk of hepatocarcinogenesis in rats by showing a considerable decrease in the serum levels of AFP, GPC-3, and STAT3 and an increase in SOCS3. Likewise, EA was found to modulate the tumor microenvironment of the HCC rat model by decreasing liver injury biomarkers such as alanine transaminase (ALT), alkaline phosphatase (ALP), and aspartate aminotransferase (AST) and downregulating the mRNA expression of TGF-α, TGF-β, vascular endothelial growth factor (VEGF), and rescued p53 levels while simultaneously decreasing CD44 hepatic cancer stem cells (HCSCs) and increasing apoptosis marker caspase-3 in immunostaining of liver sections [72]. Additionally, the transcriptomic study of HepG2 cells revealed that by simulating p21 and suppressing MCM2-7 genes, EA triggered G1 phase cell cycle arrest and encouraged apoptosis in HCC, respectively [73]. Although both in vitro and in vivo studies present encouraging results about the anticancer benefits (Fig. 2) of EA in liver cancer, more investigation is required to confirm its safety and efficacy in clinical settings.
Role of Nanotechnology and Synergism
Optimized nano-systems have proven beneficial in various domains, such as improved drug toxicity reduction, improved contrast agent efficacy, increased specificity of detection, and improved GI cancer diagnosis and treatment. The use of nanoparticles (NPs) is very beneficial for early diagnosis of GI cancer. High permeability, specificity, and sensitivity are attributes of NPs. Currently, the primary application of nanotechnologies in improved magnetic imaging is as contrast media. For instance, a contrast agent based on superparamagnetic iron oxide NPs has been developed for clinical use in the detection of metastases and guidance of surgical treatment for both gastric and esophageal malignancies [74,75,76]. Gastrointestinal malignancies were detected using nano-devices based on gold, carbon nanotubes, iron oxide nanoparticles, and quantum dots. The development of tailored therapy for the early detection and treatment of GI malignancies will be aided by nano-devices. For the targeted delivery and ablation of colorectal cancer, the function of the nano-shell is also crucial. A nonconductive core and a metal shell make up the nano-shell [77, 78].
EA is a useful chemical whose medicinal benefits can be enhanced by using a nanoparticle delivery method. EA encapsulated in hexanuclear metal prisms has been employed as a potent anticancer drug against A549 cell lines (lung cancer), AGS (gastric cancer), and SK-hep-1 (liver cancer) because of its low toxicity and strong anticancer potential. Through increased bioavailability, these metal prisms enhance the anticancer efficacy of the encapsulated drugs. Encapsulated ellagic acid has been demonstrated to suppress the development of cancer cells by upregulating the production of granulocyte colony-stimulating factor (G-CSF) and decreasing the secretion of Rantes [79]. The combination of EA and nanotechnology opens up new avenues for targeted drug administration and early detection in the treatment of gastrointestinal cancer.
Safety Aspects
The safety aspect is an important feature of a chemical for medical and industrial applications. The activity of EA against Plasmodium vinckei petteri was studied in vivo, and no toxicity was found for a 50% effective dose by the intraperitoneal route inferior to 1 mg/kg/day [80]. Scientists also evaluated the cytotoxic effects of EA on chondrocytes. EA did not exhibit cytotoxicity to mouse chondrocytes at 0–50 μM concentrations after 24 or 48 h [81]. In another study, EA showed in vitro parasiticidal activity with an IC50 of 18.55 µg/mL and thwarted cell-cycle progression at the sub-G0/G1 phase. This study was carried out for mice, and according to the author, EA is safe and nontoxic to the THP-1 cell line and to the liver and kidneys of mice [82]. Table 1 represents a bird-eye view of mechanistic insight of EA antitumor effects in various experimental models.
Conclusion and Future Perspectives
The various biological effects of EA present significant potential for the prevention and treatment of GI cancers. EA exhibits promising chemopreventive and therapeutic properties against esophageal, gastric, colorectal, pancreatic, and liver cancers. Its ability to inhibit carcinogen-induced tumor development, suppress tumor growth, induce apoptosis, and modulate various signaling pathways offers a comprehensive approach to combat GI malignancies. EA's synergistic effects with nanotechnology provide opportunities for targeted drug delivery and improved efficacy. A focus on several key areas is required. Firstly, clinical trials are needed to validate the efficacy and safety of EA in patients with GI cancer. Interpretation of EA's pharmacokinetics and optimal dosage regimens will be crucial for its clinical application. Also, exploring the synergistic effects of EA with conventional therapies could enhance treatment outcomes and reduce side effects. Investigating EA's mechanisms of action at the molecular level will provide insights into its therapeutic potential and identify novel targets for drug development. The development of novel nanocarriers for EA delivery could improve its bioavailability and enhance its anticancer effects. Overall, continued research into the therapeutic potential of EA against GI cancers holds promise for the development of novel treatment strategies and improved patient outcomes.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Lu L, Mullins CS, Schafmayer C, Zeißig S, Linnebacher M. A global assessment of recent trends in gastrointestinal cancer and lifestyle-associated risk factors. Cancer Commun. 2021;41:1137–51. https://doi.org/10.1002/cac2.12220.
Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024. https://doi.org/10.3322/caac.21834.
Davoodvandi A, Sadeghi S, Alavi SMA, Alavi SS, Jafari A, Khan H, Aschner M, Mirzaei H, Sharifi M, Asemi Z. The therapeutic effects of berberine for gastrointestinal cancers. Asia Pac J Clin Oncol. 2024;20:152–67. https://doi.org/10.1111/ajco.13941.
Haque A, Brazeau D, Amin ARMR. Perspectives for natural compounds in chemoprevention and treatment of cancer: an update with new promising compounds. Eur J Cancer Oxf Engl. 2021;1990(149):165–83. https://doi.org/10.1016/j.ejca.2021.03.009.
Tuli HS, Rath P, Chauhan A, Ramniwas S, Vashishth K, Varol M, et al. Phloretin, as a potent anticancer compound: from chemistry to cellular interactions. Molecules. 2022;27(24):8819.
Čižmáriková M, Michalková R, Mirossay L, Mojžišová G, Zigová M, Bardelčíková A, Mojžiš J. Ellagic acid and cancer hallmarks: insights from experimental evidence. Biomolecules. 2023;13(11):1653.
Amakura Y, Okada M, Tsuji S, Tonogai Y. High-performance liquid chromatographic determination with photodiode array detection of ellagic acid in fresh and processed fruits. J Chromatogr A. 2000;896:87–93. https://doi.org/10.1016/S0021-9673(00)00414-3.
Ceci C, Lacal PM, Tentori L, De Martino MG, Miano R, Graziani G. Experimental evidence of the antitumor, antimetastatic and antiangiogenic activity of ellagic acid. Nutrients. 2018;10:1756. https://doi.org/10.3390/nu10111756.
Zhang H-M, Zhao L, Li H, Xu H, Chen W-W, Tao L. Research progress on the anticarcinogenic actions and mechanisms of ellagic acid. Cancer Biol Med. 2014;11:92–100. https://doi.org/10.7497/j.issn.2095-3941.2014.02.004.
Mannino F, Imbesi C, Bitto A, Minutoli L, Squadrito F, D’Angelo T, Booz C, Pallio G, Irrera N. Anti-oxidant and anti-inflammatory effects of ellagic and punicic acid in an in vitro model of cardiac fibrosis. Biomed Pharmacother Biomedecine Pharmacother. 2023;162: 114666. https://doi.org/10.1016/j.biopha.2023.114666.
Tošović J, Bren U. Antioxidative action of ellagic acid—a kinetic DFT study. Antioxidants. 2020;9:587. https://doi.org/10.3390/antiox9070587.
Choi YH, Yan GH. Ellagic acid attenuates immunoglobulin E-mediated allergic response in mast cells. Biol Pharm Bull. 2009;32:1118–21. https://doi.org/10.1248/bpb.32.1118.
Ramadan DT, Ali MAM, Yahya SM, El-Sayed WM. Correlation between antioxidant/antimutagenic and antiproliferative activity of some phytochemicals. Anti-Cancer Agents Med Chem-Anti-Cancer Agents. 2019;19:1481–90. https://doi.org/10.2174/1871520619666190528091648.
Beserra AMSES, Calegari PI, Souza MDC, dos Santos RAN, Lima JCDS, Silva RM, Balogun SO, Martins DTDO. Gastroprotective and ulcer-healing mechanisms of ellagic acid in experimental rats. J Agric Food Chem. 2011;59:6957–65. https://doi.org/10.1021/jf2003267.
Salinger-Martinovic S, Cosic V, Stojiljkovic N, Ilic S, Stojanovic N, Dencic T. Impact of ellagic acid application on doxorubicin-induced cardiovascular toxicity model. Can J Physiol Pharmacol. 2021;99:185–91. https://doi.org/10.1139/cjpp-2020-0404.
Chen F, Lu K, Bai N, Hao Y, Wang H, Zhao X, Yue F. Oral administration of ellagic acid mitigates perioperative neurocognitive disorders, hippocampal oxidative stress, and neuroinflammation in aged mice by restoring IGF-1 signaling. Sci Rep. 2024;14:2509. https://doi.org/10.1038/s41598-024-53127-8.
Gupta A, Singh AK, Kumar R, Jamieson S, Pandey AK, Bishayee A. Neuroprotective potential of ellagic acid: a critical review. Adv Nutr. 2021;12(4):1211–38.
Aishwarya V, Solaipriya S, Sivaramakrishnan V. Role of ellagic acid for the prevention and treatment of liver diseases. Phytother Res. 2021;35:2925–44. https://doi.org/10.1002/ptr.7001.
Zhao L, Mehmood A, Soliman MM, Iftikhar A, Iftikhar M, Aboelenin SM, Wang C. Protective effects of ellagic acid against alcoholic liver disease in mice. Front Nutr. 2021. https://doi.org/10.3389/fnut.2021.744520.
Lu G, Wang X, Cheng M, Wang S, Ma K. The multifaceted mechanisms of ellagic acid in the treatment of tumors: state-of-the-art. Biomed Pharmacother. 2023;165: 115132. https://doi.org/10.1016/j.biopha.2023.115132.
Umesalma S, Nagendraprabhu P, Sudhandiran G. Ellagic acid inhibits proliferation and induced apoptosis via the Akt signaling pathway in HCT-15 colon adenocarcinoma cells. Mol Cell Biochem. 2015;399:303–13. https://doi.org/10.1007/s11010-014-2257-2.
Kim JY, Choi YJ, Kim H-J. Determining the effect of ellagic acid on the proliferation and migration of pancreatic cancer cell lines. Transl Cancer Res. 2021;10:424–33. https://doi.org/10.21037/tcr-20-2446.
Lim SC, Hwang H, Han SI. Ellagic acid inhibits extracellular acidity-induced invasiveness and expression of COX1, COX2, snail, twist 1, and c-myc in gastric carcinoma cells. Nutrients. 2019;11:3023.
Zhao J, Li G, Wei J, Dang S, Yu X, Ding L, Shang C, Zhang H, Zhang Z, Chen H, Liu M. Ellagic acid induces cell cycle arrest and apoptosis via the TGF-β1/Smad3 signaling pathway in human colon cancer HCT-116 cells. Oncol Rep. 2020;44:768–76. https://doi.org/10.3892/or.2020.7617.
Baradaran Rahimi V, Ghadiri M, Ramezani M, Askari VR. Antiinflammatory and anti-cancer activities of pomegranate and its constituent, ellagic acid: evidence from cellular, animal, and clinical studies. Phytother Res. 2020;34(4):685–720.
Mohammadinejad A, Mohajeri T, Aleyaghoob G, Heidarian F, Kazemi Oskuee R. Ellagic acid as a potent anticancer drug: a comprehensive review on in vitro, in vivo, in silico, and drug delivery studies. Biotechnol Appl Biochem. 2022;69(6):2323–56.
Golmei P, Kasna S, Roy KP, Kumar S. A review on pharmacological advancement of ellagic acid. J Pharmacol Pharmacother. 2024;15(2):93–104. https://doi.org/10.1177/0976500X24124063.
Nyamba I, Lechanteur A, Semdé R, Evrard B. Physical formulation approaches for improving aqueous solubility and bioavailability of ellagic acid: a review. Eur J Pharm Biopharm. 2021;159:198–210.
Ding Y, Zhang B, Zhou K, Chen M, Wang M, Jia Y, et al. Dietary ellagic acid improves oxidant-induced endothelial dysfunction and atherosclerosis: role of Nrf2 activation. Int J Cardiol. 2014;175(3):508–14.
Khuda-Bukhsh AR, Das S, Saha SK. Molecular approaches toward targeted cancer prevention with some food plants and their products: inflammatory and other signal pathways. Nutr Cancer. 2014;66(2):194–205.
Mertens-Talcott SU, Percival SS. Ellagic acid and quercetin interact synergistically with resveratrol in the induction of apoptosis and cause transient cell cycle arrest in human leukemia cells. Cancer Lett. 2005;218(2):141–51.
García-Niño WR, Zazueta C. Ellagic acid: pharmacological activities and molecular mechanisms involved in liver protection. Pharmacol Res. 2015;97:84–103.
Ebrahimi R, Sepand MR, Seyednejad SA, Omidi A, Akbariani M, Gholami M, Sabzevari O. Ellagic acid reduces methotrexate-induced apoptosis and mitochondrial dysfunction via up-regulating Nrf2 expression and inhibiting the IĸBα/NFĸB in rats. DARU J Pharm Sci. 2019;27:721–33.
Whitley AC, Stoner GD, Darby MV, Walle T. Intestinal epithelial cell accumulation of the cancer preventive polyphenol ellagic acid—extensive binding to protein and DNA. Biochemical pharmacology. 2003;66(6):907–15.
Keszei AP, Alexandra Goldbohm R, Schouten LJ, Jakszyn P, van den Brandt PA. Dietary N-nitroso compounds, endogenous nitrosation, and the risk of esophageal and gastric cancer subtypes in the Netherlands cohort study. Am J Clin Nutr. 2013;97(1):135–46. https://doi.org/10.3945/ajcn.112.043885.
Mandal S, Stoner GD. Inhibition of N-nitrosobenzylmethylamine-induced esophageal tumorigenesis in rats by ellagic acid. Carcinogenesis. 1990;11(1):55–61.
Siglin JC, Brach DH, Stoner GD. Effects of dietary phenethyl isothiocyanate, ellagic acid, sulindac and calcium on the induction and progression of N-nitrosomethylbenzylamine-induced esophageal carcinogenesis in rats. Carcinogenesis. 1995;16(5):1101–6.
Stoner GD, Chen T, Kresty LA, Aziz RM, Reinemann T, Nines R. Protection against esophageal cancer in rodents with lyophilized berries: potential mechanisms. Nutr Cancer. 2006;54(1):33–46.
Ma RJ, Ma C, Hu K, Zhao MM, Zhang N, Sun ZG. Molecular mechanism, regulation, and therapeutic targeting of the STAT3 signaling pathway in esophageal cancer (Review). Int J Oncol. 2022;61(3):105. https://doi.org/10.3892/ijo.2022.5395.
Li LW, Na C, Tian SY, Chen J, Ma R, Gao Y, Lou G. Ellagic acid induces HeLa cell apoptosis via regulating signal transducer and activator of transcription 3 signaling. Exp Ther Med. 2018;16(1):29–36.
Zapolnik P, Pyrkosz A. Rnf6 as an oncogene and potential therapeutic target—a review. BioTech. 2020;9(4):22. https://doi.org/10.3390/biotech9040022.
Cota D, Patil D. Antibacterial potential of ellagic acid and gallic acid against IBD bacterial isolates and cytotoxicity against colorectal cancer. Nat Prod Res. 2023;37(12):1998–2002. https://doi.org/10.1080/14786419.2022.2111560. (Epub 2022 Aug 15).
Ni X, Shang F-S, Wang T-F, Wu D-J, Chen D-G, Zhuang B. Ellagic acid induces apoptosis and autophagy in colon cancer through the AMPK/mTOR pathway. Tissue Cell. 2023;81: 102032. https://doi.org/10.1016/j.tice.2023.102032.
Smyth EC, Nilsson M, Grabsch HI, van Grieken NC, Lordick F. Gastric cancer. Lancet. 2020;396:635–48.
Cheshomi H, Bahrami AR, Matin MM. Ellagic acid and human cancers: a systems pharmacology and docking study to identify principal hub genes and main mechanisms of action. Mol Divers. 2021;25:333–49.
Sathianarayanan S, Ammanath AV, Biswas RBA, Sukumaran S, Venkidasamy B. A new approach against Helicobacter pylori using plants and its constituents: a review study. Microb Pathog. 2022;168: 105594.
Cheshomi H, Bahrami AR, Rafatpanah H, Matin MM. The effects of ellagic acid and other pomegranate (Punica granatum L.) derivatives on human gastric cancer AGS cells. Hum Exp Toxicol. 2022;41:09603271211064534.
Bellini MF, Cadamuro ACT, Succi M, Proença MA, Silva AE. Alterations of the TP53 gene in gastric and esophageal carcinogenesis. BioMed Res Int. 2012;2012(1):891961.
Marcellinaro R, Spoletini D, Grieco M, Avella P, Cappuccio M, Troiano R, Lisi G, Garbarino GM, Carlini M. Colorectal cancer: current updates and future perspectives. J Clin Med. 2023;13:40. https://doi.org/10.3390/jcm13010040.
Scherman P, Syk I, Holmberg E, Naredi P, Rizell M. Risk factors for postoperative complications following resection of colorectal liver metastases and the impact on long-term survival: a population-based national cohort study. World J Surg. 2023;47:2230–40. https://doi.org/10.1007/s00268-023-07043-z.
De S, Paul S, Manna A, Majumder C, Pal K, Casarcia N, Mondal A, Banerjee S, Nelson VK, Ghosh S, Hazra J, Bhattacharjee A, Mandal SC, Pal M, Bishayee A. Phenolic phytochemicals for prevention and treatment of colorectal cancer: a critical evaluation of in vivo studies. Cancers. 2023;15:993. https://doi.org/10.3390/cancers15030993.
Mirsane S, Mirsane S. Benefits of ellagic acid from grapes and pomegranates against colorectal cancer. Casp J Int Med. 2017;8:226–7. https://doi.org/10.22088/cjim.8.3.226.
Fang Y, Zhou H, Xia J-F, Lin J-J, Li R-Z, Yang D-Q, Xu M-Y, Li X-Y. Ellagic acid regulates Wnt/Î2-catenin signaling pathway and CDK8 in HCT 116 and HT 29 colon cancer cells. Bangladesh J Pharmacol. 2015;10:47–56.
Lin Z, Lin C, Fu C, Lu H, Jin H, Chen Q, Pan J. The protective effect of ellagic acid (EA) in osteoarthritis: an in vitro and in vivo study. Biomed Pharmacotherapy. 2020;125: 109845. https://doi.org/10.1016/j.biopha.2020.109845.
Kong R, Zhang EB, Yin DD, You LH, Xu TP, Chen WM, et al. Long noncoding RNA PVT1 indicates a poor prognosis of gastric cancer and promotes cell proliferation through epigenetically regulating p15 and p16. Mol Cancer. 2015;14:1–14.
Yousef AI, El-Masry OS, Abdel Mohsen MA. Impact of cellular genetic make-up on colorectal cancer cell lines response to ellagic acid: implications of small interfering RNA. Asian Pac J Cancer Prev APJCP. 2016;17:743–8. https://doi.org/10.7314/apjcp.2016.17.2.743.
Yakobov S, Dhingra R, Margulets V, Dhingra A, Crandall M, Kirshenbaum LA. Ellagic acid inhibits mitochondrial fission protein Drp-1 and cell proliferation in cancer. Mol Cell Biochem. 2023;478:2029–40. https://doi.org/10.1007/s11010-022-04627-6.
Nuñez-Sánchez MA, González-Sarrías A, García-Villalba R, Monedero-Saiz T, García-Talavera NV, Gómez-Sánchez MB, et al. Gene expression changes in colon tissues from colorectal cancer patients following the intake of an ellagitannin-containing pomegranate extract: a randomized clinical trial. J Nutr Biochem. 2017;42:126–33.
Zhao J, Li G, Bo W, Zhou Y, Dang S, Wei J, et al. Multiple effects of ellagic acid on human colorectal carcinoma cells identified by gene expression profile analysis. Int J Oncol. 2017;50(2):613–21.
Kao WY, Hwang CY, Chang YT, Su CW, Hou MC, Lin HC, et al. Cancer risk in patients with pyogenic liver abscess: a nationwide cohort study. Aliment Pharmacol Ther. 2012;36(5):467–76.
Cheng H, Janakiram M, Borczuk A, Lin J, Qiu W, Liu H, et al. HHLA2, a new immune checkpoint member of the B7 family, is widely expressed in human lung cancer and associated with EGFR mutational status. Clin Cancer Res. 2017;23(3):825–32.
Aslan K, Haberal A, Akıllı H, Meydanli MM, Ayhan A. Prognostic value of the number of the metastatic lymph nodes in locally early-stage cervical cancer: squamous cell carcinoma versus non-squamous cell carcinoma. Arch Gynecol Obstet. 2021.
Zhao L, Li W, Zang W, Liu Z, Xu X, Yu H, et al. JMJD2B promotes epithelial–mesenchymal transition by cooperating with β-catenin and enhances gastric cancer metastasis. Clin Cancer Res. 2013;19(23):6419–29.
Suzuki Y, Suda T, Furuhashi K, Suzuki M, Fujie M, Hahimoto D, et al. Increased serum kynurenine/tryptophan ratio correlates with disease progression in lung cancer. Lung Cancer. 2010;67(3):361–5.
Masamune A, Satoh M, Kikuta K, Suzuki N, Satoh K, Shimosegawa T. Ellagic acid blocks activation of pancreatic stellate cells. Biochem Pharmacol. 2005;70(6):869–78.
Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, Lencioni R, Koike K, Zucman-Rossi J, Finn RS. Hepatocellular carcinoma. Nat Rev Dis Primer. 2021;7:1–28. https://doi.org/10.1038/s41572-020-00240-3.
Bruix J, Takayama T, Mazzaferro V, Chau G-Y, Yang J, Kudo M, Cai J, Poon RT, Han K-H, Tak WY, Lee HC, Song T, Roayaie S, Bolondi L, Lee KS, Makuuchi M, Souza F, Berre M-AL, Meinhardt G, Llovet JM, STORM investigators,. Adjuvant sorafenib for hepatocellular carcinoma after resection or ablation (STORM): a phase 3, randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2015;16:1344–54. https://doi.org/10.1016/S1470-2045(15)00198-9.
Rayginia TP, Keerthana CK, Shifana SC, Maria Joy P, Abhishek A, Anto R. Phytochemicals as potential lead molecules against hepatocellular carcinoma. Curr Med Chem. 2024. https://doi.org/10.2174/0109298673275501231213063902.
Abenavoli L, Montori M, Svegliati Baroni G, Argenziano ME, Giorgi F, Scarlata GGM, Ponziani F, Scarpellini E. Perspective on the role of gut microbiome in the treatment of hepatocellular carcinoma with immune checkpoint inhibitors. Med Kaunas Lith. 2023;59:1427. https://doi.org/10.3390/medicina59081427.
Das U, Biswas S, Chattopadhyay S, Chakraborty A, Dey Sharma R, Banerji A, Dey S. Radiosensitizing effect of ellagic acid on growth of hepatocellular carcinoma cells: an in vitro study. Sci Rep. 2017;7:14043. https://doi.org/10.1038/s41598-017-14211-4.
Zaazaa AM, Lokman MS, Shalby AB, Ahmed HH, El-Toumy SA. Ellagic acid holds promise against hepatocellular carcinoma in an experimental model: mechanisms of action. Asian Pac J Cancer Prev APJCP. 2018;19:387–93. https://doi.org/10.22034/APJCP.2018.19.2.387.
Ramadan WS, Alkarim S, Moulay M, Alrefeai G, Alkudsy F, Hakeem KR, Iskander A. Modulation of the tumor microenvironment by ellagic acid in rat model for hepatocellular carcinoma: a potential target against hepatic cancer stem cells. Cancers. 2023;15:4891. https://doi.org/10.3390/cancers15194891.
Qiu S, Zhong C, Zhao B, Li G, Wang J, Jehan S, Li J, Zhao X, Li D, Sui G. Transcriptome analysis of signaling pathways targeted by ellagic acid in hepatocellular carcinoma cells. Biochim Biophys Acta BBA Gen Subj. 2021;1865: 129911. https://doi.org/10.1016/j.bbagen.2021.129911.
Ishiyama K, Motoyama S, Tomura N, Sashi R, Imano H, Ogawa J, Narita K, Watarai J. Visualization of lymphatic basin from the tumor using magnetic resonance lymphography with superparamagnetic iron oxide in patients with thoracic esophageal cancer. J Comput Assist Tomogr. 2006;30:270–5. https://doi.org/10.1097/00004728-200603000-00020].
Pultrum BB, van der Jagt EJ, van Westreenen HL, van Dullemen HM, Kappert P, Groen H, Sietsma J, Oudkerk M, Plukker JT, van Dam GM. Detection of lymph node metastases with ultrasmall superparamagnetic iron oxide (USPIO)-enhanced magnetic resonance imaging in oesophageal cancer: a feasibility study. Cancer Imaging. 2009;9:19–28. https://doi.org/10.1102/1470-7330.2009.0004].
Tokuhara T, Tanigawa N, Matsuki M, Nomura E, Mabuchi H, Lee SW, Tatsumi Y, Nishimura H, Yoshinaka R, Kurisu Y, Narabayashi I. Evaluation of lymph node metastases in gastric cancer using magnetic resonance imaging with ultrasmall superparamagnetic iron oxide (USPIO): diagnostic performance in post-contrast images using new diagnostic criteria. Gastric Cancer. 2008;11:194–200. https://doi.org/10.1007/s10120-008-0480-9].
Fortina P, Kricka LJ, Graves DJ, Park J, Hyslop T, Tam F, Halas N, Surrey S, Waldman SA. Applications of nanoparticles to diagnostics and therapeutics in colorectal cancer. Trends Biotechnol. 2007;25:145–52. https://doi.org/10.1016/j.tibtech.2007.02.005].
Liang M, Li LD, Li L, Li S. Nanotechnology in diagnosis and therapy of gastrointestinal cancer. World J Clin Cases. 2022;10(16):5146–55. https://doi.org/10.12998/wjcc.v10.i16.5146.PMID:35812681;PMCID:PMC9210884.
Manzari-Tavakoli A, Babajani A, Tavakoli MM, Safaeinejad F, Jafari A. Integrating natural compounds and nanoparticle-based drug delivery systems: a novel strategy for enhanced efficacy and selectivity in cancer therapy. Cancer Med. 2024;13(5): e7010. https://doi.org/10.1002/cam4.7010.PMID:38491817;PMCID:PMC10943377.
Soh PN, Witkowski B, Olagnier D, Nicolau ML, Garcia-Alvarez MC, Berry A, Benoit-Vical F. In vitro and in vivo properties of ellagic acid in malaria treatment. Antimicrob Agents Chemother. 2009;53(3):1100–6. https://doi.org/10.1128/AAC.01175-08. (Epub 2008 Nov 17).
Zeng M, Su Y, Li K, Jin D, Li Q, Li Y, Zhou B. Gallic acid inhibits bladder cancer T24 cell progression through mitochondrial dysfunction and PI3K/Akt/NF-κB signaling suppression. Front Pharmacol. 2020;11:1222.
Keshav P, Goyal DK, Kaur S. In vitro and in vivo therapeutic antileishmanial potential of ellagic acid against Leishmania donovani in murine model. Med Microbiol Immunol. 2023;212:35–51. https://doi.org/10.1007/s00430-022-00754-5.
Xu YY, Wang WW, Huang J, Zhu WG. Ellagic acid induces esophageal squamous cell carcinoma cell apoptosis by modulating SHP-1/STAT3 signaling. Kaohsiung J Med Sci. 2020;36(9):699–704.
Tan Z, Li X, Chen X, Wang L, Chen B, Ren S, Zhao M. Ellagic acid inhibits tumor growth and potentiates the therapeutic efficacy of sorafenib in hepatocellular carcinoma. Heliyon. 2023. https://doi.org/10.1016/j.heliyon.2023.e23931.
Funding
No funding was received for this study. The journal’s Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Abhishek Chauhan, Monika Yadav, Ritu Chauhan, Vinay Mohan Pathak, Rajpal Srivastav, and Rupesh Kumar Basniwal conceived the conceptualization, methodology, validation, and writing—review. Vinay Mohan Pethak, Seema Ramniwas, Raj Kishor Kapardar, and Anuj Ranjan organized references and edited the manuscript. Shafiul Haque, Darin Mansor Mathkor, Arif Hussain, and Hardeep Singh Tuli revised the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Abhishek Chauhan, Monika Yadav, Ritu Chauhan, Vinay Mohan Pathak, Rajpal Srivastav, Rupesh Kumar Basniwal, Seema Ramniwas, Raj Kishor Kapardar, Anuj Ranjan, Shafiul Haque, Darin Mansor Mathkor, Arif Hussain, and Hardeep Singh Tuli declare no conflict of interests.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chauhan, A., Yadav, M., Chauhan, R. et al. Exploring the Potential of Ellagic Acid in Gastrointestinal Cancer Prevention: Recent Advances and Future Directions. Oncol Ther (2024). https://doi.org/10.1007/s40487-024-00296-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40487-024-00296-1