Abstract
Purpose
The passive leg raising test (PLR) produces a reversible increase in venous return and, if the patient’s ventricles are preload dependent, in the cardiac output. As this effect occurs in seconds, the transthoracic echocardiography is optimal for its real time assessment. The utility of the PLR for monitoring fluid responsiveness through the measurement of the left ventricle outflow tract velocity–time integral (LVOT VTI) in an apical 5-chamber view is well stablished. To achieve this view in critically ill patients is often challenging. The aim of this study is to explore the accuracy for predicting fluid responsiveness of the change in the right ventricle outflow tract velocity–time integral (RVOT VTI) from a subcostal view during a PLR.
Methods
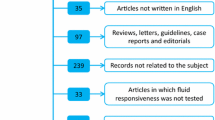
This is a diagnostic accuracy study carried out in two centers in Argentina. We included patients admitted to the intensive care unit from January 2022 to April 2022, that required fluid expansion due to signs of tissular hypoperfusion. We measured the RVOT VTI from a subcostal view in a semi-recumbent position and during the PLR, and the LVOT VTI in an apical 5-chamber view before and after a fluid bolus. If the LVOT VTI increased by 15% after the fluid bolus, the patients were considered fluid responders.
Results
We included 43 patients. The area under the ROC curve for a change in the RVOT VTI during the PLR was 0.879 (95% CI 0.744–0.959). A change of 15.36% in the RVOT VTI with the PLR predicted fluid responsiveness with a sensitivity of 85.7% (95% CI 57.2%–98.2%) and specificity of 93.1% (95% CI 77.2–99.2). The positive predictive value was 85.7% (95% CI 60.8%–95.9%) and the negative predictive value was 93.1% (95% CI 78.8%–98%). The positive likelihood ratio was 12.43 and the negative predictive value was 0.15.
Conclusion
The RVOT VTI change during a PLR is suitable for the prediction of fluid responsiveness in critically ill patients.





Similar content being viewed by others
References
Wang J, Zhou D, Gao Y, Wu Z, Wang X, Lv C. Effect of VTILVOT variation rate on the assessment of fluid responsiveness in septic shock patients. Medicine (Baltimore) [Internet]. 2020 Nov 20;99(47):e22702. https://journals.lww.com/https://doi.org/10.1097/MD.0000000000022702
Monnet X, Marik PE, Teboul J-L. Prediction of fluid responsiveness: an update. Ann Intensive Care [Internet]. 2016 Dec 17;6(1):111. http://annalsofintensivecare.springeropen.com/articles/https://doi.org/10.1186/s13613-016-0216-7
Maizel J, Airapetian N, Lorne E, Tribouilloy C, Massy Z, Slama M. Diagnosis of central hypovolemia by using passive leg raising. Intensive Care Med [Internet]. 2007 Jul 17;33(7):1133–8. http://link.springer.com/https://doi.org/10.1007/s00134-007-0642-y
Biais M, Vidil L, Sarrabay P, Cottenceau V, Revel P, Sztark F. Changes in stroke volume induced by passive leg raising in spontaneously breathing patients: comparison between echocardiography and VigileoTM/FloTracTM device. Crit Care [Internet]. 2009;13(6):R195. http://ccforum.biomedcentral.com/articles/https://doi.org/10.1186/cc8195
Préau S, Saulnier F, Dewavrin F, Durocher A, Chagnon J-L. Passive leg raising is predictive of fluid responsiveness in spontaneously breathing patients with severe sepsis or acute pancreatitis*. Crit Care Med [Internet]. 2010 Mar;38(3):819–25. http://journals.lww.com/00003246-201003000-00012
Guinot P-G, Zogheib E, Detave M, Moubarak M, Hubert V, Badoux L, et al. Passive leg raising can predict fluid responsiveness in patients placed on venovenous extracorporeal membrane oxygenation. Crit Care [Internet]. 2011;15(5):R216. http://ccforum.biomedcentral.com/articles/https://doi.org/10.1186/cc10451
Lamia B, Ochagavia A, Monnet X, Chemla D, Richard C, Teboul J-L. Echocardiographic prediction of volume responsiveness in critically ill patients with spontaneously breathing activity. Intensive Care Med [Internet]. 2007 Jul 17;33(7):1125–32. Available from: http://link.springer.com/https://doi.org/10.1007/s00134-007-0646-7
Brun C, Zieleskiewicz L, Textoris J, Muller L, Bellefleur J-P, Antonini F, et al. Prediction of fluid responsiveness in severe preeclamptic patients with oliguria. Intensive Care Med [Internet]. 2013 Apr 6;39(4):593–600. http://link.springer.com/https://doi.org/10.1007/s00134-012-2770-2
Maizel J, Salhi A, Tribouilloy C, Massy ZA, Choukroun G, Slama M. The subxiphoid view cannot replace the apical view for transthoracic echocardiographic assessment of hemodynamic status. Crit Care [Internet]. 2013;17(5):R186. http://ccforum.biomedcentral.com/articles/https://doi.org/10.1186/cc12869
Cheong I, Castro VO, Gómez RA, Merlo PM, Tamagnone FM. A modified subcostal view: a novel method for measuring the LVOT VTI. J Ultrasound [Internet]. 2022 Apr 21; https://link.springer.com/https://doi.org/10.1007/s40477-022-00671-6
Gürsel G, Özdemir U, Güney T, Karaarslan N, Tekin Ö, Öztürk B. The usefulness of subxiphoid view in the evaluation of acceleration time and pulmonary hypertension in ICU patients. Echocardiography [Internet]. 2020 Sep 13;37(9):1345–52. https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/echo.14822
Cheong I, Bermeo M, Merlo PM, Tamagnone FM. A new approach of non‐invasive hemodynamic assessment by echocardiography in the intensive care unit: The right intercostal transhepatic window. Echocardiography [Internet]. 2022 May 17;39(5):752–4. https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/echo.15353
Monnet X, Marik P, Teboul J-L. Passive leg raising for predicting fluid responsiveness: a systematic review and meta-analysis. Intensive Care Med [Internet]. 2016 Dec 29;42(12):1935–47. http://link.springer.com/https://doi.org/10.1007/s00134-015-4134-1
Jozwiak M, Mercado P, Teboul J-L, Benmalek A, Gimenez J, Dépret F, et al. What is the lowest change in cardiac output that transthoracic echocardiography can detect? Crit Care [Internet]. 2019 Dec 11;23(1):116. Available from: https://ccforum.biomedcentral.com/articles/https://doi.org/10.1186/s13054-019-2413-x
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, et al. Relation between Respiratory Changes in Arterial Pulse Pressure and Fluid Responsiveness in Septic Patients with Acute Circulatory Failure. Am J Respir Crit Care Med [Internet]. 2000 Jul;162(1):134–8. http://www.atsjournals.org/doi/abs/https://doi.org/10.1164/ajrccm.162.1.9903035
Tavernier B, Makhotine O, Lebuffe G, Dupont J, Scherpereel P. Systolic Pressure Variation as a Guide to Fluid Therapy in Patients with Sepsis-induced Hypotension. Anesthesiology [Internet]. 1998 Dec 1;89(6):1313–21. https://pubs.asahq.org/anesthesiology/article/89/6/1313/37185/Systolic-Pressure-Variation-as-a-Guide-to-Fluid
Preisman S, Kogan S, Berkenstadt H, Perel A. Predicting fluid responsiveness in patients undergoing cardiac surgery: functional haemodynamic parameters including the Respiratory Systolic Variation Test and static preload indicators †. Br J Anaesth [Internet]. 2005 Dec;95(6):746–55. https://linkinghub.elsevier.com/retrieve/pii/S0007091217350274
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
conceptualization: IC; methodology: IC; formal analysis and investigation: IC, VOC, MB, MFF; writing—original draft preparation: IC; writing—review and editing: IC, VOC; supervision: IC, PMM, FMT.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non/financial interests to disclose.
Ethical approval
The study was conducted following the principles of the Helsinki Declaration and within the precautions established by ethical and legal standards. The study was approved by the Institutional Review Board and Ethic Committee of Clínica y Maternidad Suizo-Argentina (approval number 6517).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the images in Figs. 1, 2, and 3.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cheong, I., Otero Castro, V., Brizuela, M. et al. Passive leg raising test to predict fluid responsiveness using the right ventricle outflow tract velocity–time integral through a subcostal view. J Ultrasound (2022). https://doi.org/10.1007/s40477-022-00719-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40477-022-00719-7