Abstract
Purpose of Review
Coronavirus disease 2019 (COVID-19) has caused a spike in newly diagnosed diabetes mellitus (NDDM). NDDM and COVID-19 infection are not well established as a cause-and-effect relationship; hence, the present review aims to define the underlying causes and consequences of COVID-19 infection in relation to the condition.
Recent Findings
β-Cells are infiltrated by SARS-CoV-2, causing glycometabolic dysfunction and insulin dysregulation. The disease causes systemic inflammation and pro-inflammatory cytokines, as well as hormonal changes that lead to insulin resistance and hyperglycemia that are difficult to manage. As a result of NDDM, complications related to COVID-19 infection become more severe.
Summary
NDDM related to COVID-19 infection complicates hospitalization outcomes and adversely affects quality of life in patients. There are many possible causes and consequences associated with NDDM, but for establishing preventive measures and treatments for NDDM, more evidence regarding its epidemiology, physiopathology, etiology, and nutritional aspects is required.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19) has affected the world in a variety of ways, ranging from the disease itself to lockdowns and changes in lifestyle and behavior. Approximately 565,207,160 cases of COVID-19 have been confirmed as of mid-July of 2022, according to the World Health Organization (WHO) [1]. While the disease has been thoroughly studied, evidence of post-acute sequelae is still being analyzed [2]. These post-acute sequelae are often referred to as “long COVID'' which is defined by the National Institute for Health and Care Excellence (NICE) as “signs and symptoms that emerge during or after an infection consistent with COVID-19, persist for more than 12 weeks, and are not explained by an alternative diagnosis” [3]. There are multiple manifestations of long COVID, including pulmonary and multiorganic signs and symptoms that can impair the quality of life of patients who have recovered from the illness [2, 4].
Several studies have reported a link between diabetes mellitus (DM) and COVID-19, ranging from and increased risk of poor prognosis and increased mortality to newly diagnosed diabetes mellitus (NDDM) precipitated by COVID-19 [5,6,7]. NDDM causes are still being debated among researchers, as it could be caused by direct viral entry into β-cells, resulting in dysfunction, systemic inflammation resulting in insulin resistance, or endocrine changes triggering this response [5, 6, 8••]. Also, glucocorticoids are usually prescribed for moderate and severe COVID-19, which are reported to cause hyperglycemia and insulin resistance, which could exacerbate the incidence of NDDM [6].
In comparison with previously diagnosed DM, NDDM is known to increase the odds of being admitted to the intensive care unit (ICU), having a longer length of stay and a higher mortality from SARS-CoV-2 infection [9•, 10]. The purpose of this review is to evaluate the existing evidence surrounding the causes and consequences of NDDM. It is imperative that we have a better understanding of the findings of NDDM due to the pandemic’s ongoing spread and the increase in NDDM cases that are occurring.
COVID-19: A Nightmare for Glycemic Management
Glycemic levels can fluctuate for many reasons when the body goes through a state of stress caused by an infectious and inflammatory process. The immune and endocrine systems interact closely to keep glucose metabolism in homeostasis [11]. As a result of metabolic stress induced by a pathogen, an inflammatory response leads to hormonal changes as the overproduction of counterregulatory hormones such as glucagon and catecholamines, as well as an adrenocortical response, resulting in insulin resistance and contributing to the blood sugar imbalance [12•] (Table 1). Hyperglycemia with or without a history of DM is a strong predictor of adverse outcomes, increasing the risk of mortality [9•, 13]. According to Huang Y et al., patients with abnormal fasting plasma glucose levels without having DM had a crude mortality of COVID-19 of 3.54 times higher than those with normal glycemic levels (OR = 3.54; p = 0.018) [13]. A meta-analysis conducted by Sathish T et al. showed that 14.4% of hospitalized patients with COVID-19 developed NDDM, even though it is important to consider that some of the patients could have not been diagnosed before infection [14]. There are many mechanisms that may contribute to COVID-19’s ability to cause glycemic imbalance and cause the development of NDDM.
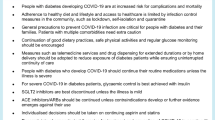
It is well known that SARS-CoV-2 is a respiratory tract infection; despite this, growing evidence has allowed the emergence of a different hypothesis that suggests that other cells can be infected, leading to extrapulmonary pathological changes and complications [15, 16]. As a result of the acute inflammatory process involving C-reactive protein (CRP) and interleukin-6 (IL-6), damage may occur to β-cells, resulting in dysfunction of these pancreatic cells [17] (Fig. 1). This was demonstrated by Yavropoulou A. et al.’s study, which assessed levels of IL-6, salivary cortisol, and CRP levels in COVID-19 patients, finding that CRP and IL-6 levels were 6 times higher in infected patients (p < 0.001). Related to cortisol levels, evidence showed that nocturnal salivary cortisol was higher compared to the control group [17]. This metabolic response during a period of COVID-19 infection can result in hyperglycemia secondary to insulin resistance [6, 18].
Causes of glycometabolic disruptions during COVID-19 infection. Interactions of SARS-CoV-2 and pancreatic β-cells and molecular components needed for viral infiltration in the cells and systemic inflammation and its effects on increasing cytokine levels as the cause glycometabolic disruption. Adapted from: Steenblock C, Richter S, Berger I, et al. [5] Montefusco, L, Ben Nasr, M, D’Addio, F. et al. [8••], Wu CT, Lidsky PV, Xiao Y. et al. [26••], and Müller, J.A., Groß, R., Conzelmann, C. et al. [28]
Adipose tissue plays an important endocrine role by secreting hormones; dysfunction of this carefully controlled system can be associated with insulin resistance [18]. Adiponectin is an anabolic hormone secreted by the adipose tissue, which during metabolic stress related to infection tends to decrease, as there is a significant correlation between the severity of the inflammatory process and adiponectin levels [19, 20]. Reiterer M et al. found that adiponectin level was 50–60% decreased in patients with COVID-19 and ARDS, compared with ICU patients without ARDS (p = 0.003) [18]. These results can be compared with those obtained by Filippo et al., where the adiponectin/leptin ratio was evaluated in patients with COVID-19 as a marker of survival and inflammatory load. The results showed that patients with a higher adiponectin/leptin ratio tended to have more cardiometabolic disturbances (NDDM, HTA, obesity, etc.), more death, and ICU admission (p = 0.010) [20]. Also, it showed that patients with severe COVID-19 had significantly higher CRP serum levels (p < 0.001) and that this ratio was significantly associated with CRP serum levels (p = 0.023) [20, 21].
In addition to the previously described metabolic and endocrine alterations, it is important to consider that the COVID-19 treatment guidelines recommend the use of systemic corticosteroids for some nonhospitalized and all hospitalized patients since it has been seen that this therapy improves clinical outcomes by mitigating the inflammatory response [22]. It is worth considering that it helps in reducing inflammation, and the use of glucocorticosteroids has a key effect on NDDM on COVID-19 patients [23]. Significant levels of glucose variation were found in patients who used corticosteroids for COVID-19 treatment (p < 0.026), basal glucose increased by 23.9 mg/dl (p = 0.010), and postprandial blood sugar increased by 46.5 mg/dl (p < 0.001) [24]. These results can be compared to the meta-analysis by Chaudhuri et al. who found that there was an increase in glycemic levels with corticosteroid use (RR 1.11, CI 95% 1.01–1.23); however, the results are not certain there is variability in definitions for hyperglycemia used across studies [25].
How Does COVID-19 Affect the Pancreas?
There are different ways in which the pancreas could be affected by SARS-CoV-2 infection. There is evidence that the pancreatic islet endocrine cells, specially β-cells, can be harmed by viral infections, such as SARS-CoV-2 [5, 26••]. Moreover, β-cell dysfunction can happen when there is an inflammatory state, which is the case in COVID-19 patients [8••]. There is still a debate regarding whether infection or inflammation is the primary cause of β-cell dysfunction.
SARS-CoV-2 is capable of infecting pancreatic cells through multiple entry factors besides angiotensin-converting enzyme 2 (ACE2). In endocrine pancreatic cells, ACE2 expression has been reported to be low, but when compared to α-cells, β-cells express higher levels of ACE2 (colocalization rate: ACE2-INS 57.6 ± 19.3% vs. ACE2-GCG 6.8 ± 5.4%; p < 0. ± 0001 [27, 28]. The entry of viruses into insulin-producing cells might be facilitated by a number of receptors and factors. It was evidenced by Wu CT et al. that β-cells, obtained from isolated human islets from healthy pancreatic donors ex vivo, express a large amount of neuropilin 1 (NRP1) and the transferrin receptor (TFRC) proteins, a small number of ACE2, and transmembrane serine protease 2 (TMPRSS2). Furthermore, NRP1 expression in patients positive for COVID-19 was significantly higher than in controls (p < 0.05) [26••]. These results compared to the ones obtained by Steenblock C et al. which evaluated SARS-CoV-2 entry factors in pancreatic islets obtained from 18 pancreatic donors, 11 who passed from COVID-19 and 6 from other causes. In this study, it was evidenced that human islets expressed NRP1, which could facilitate virus uptake. They also evaluated the MERS-CoV receptor dipeptidyl-peptidase 4 (DPP4), which is expressed by cells of the endocrine and exocrine pancreas, and that it could work as a receptor for SARS-CoV-2 in β-cells [5]. The S protein of the virus can also invade other cells by binding through the same receptor DPP4 [29]. Consequently, these findings demonstrate that these cells are specifically equipped with the molecular components that permit SARS-CoV-2 to infect β-cells in the pancreas and that ACE2 is not the only factor in determining whether these cells become infected with this virus.
Based on RT-PCR and SARS-CoV-2 spike transcripts, there is evidence of SARS-CoV-2 viral positivity in the pancreas of patients who died from COVID-19–related complications [26••]. Steenblock C et al. stained the pancreas of all deceased patients with SARS-CoV-2 viral antigens, which were detected in endocrine and exocrine pancreas of patients who died from COVID-19 and negative in the control group [5]. Concerning endocrine function and insulin secretion, there is evidence that cells infected with SARS-CoV-2 lack hormone expression [28]. Wu CT et al. quantified the insulin content and glucose-stimulated insulin secretion in β-cells ex vivo, and the results showed a decrease in insulin and glucose-stimulated insulin secretion in SARS-CoV-2–infected human islets when compared to the control (p < 0.05) [26••]. A similar finding was reported by Müller JA et al. demonstrating that infected cells had a lower response to glucose-stimulated insulin secretion when compared to control cells (p = 0.006) [28]. Additionally, Steenblock C et al. suggested that this metabolic dysfunction might be caused by necrosis mediated by MLKL protein, which was detected in a small percentage of islets in all COVID-19 patient samples [5]. The data presented here shows that β-cells are infected by SARS-CoV-2 via various mechanisms and that it might lead to dysfunction of insulin secretion and production. β-Cell infection or apoptosis could cause this dysfunction, leading to hyperglycemia or NDDM.
NDDM: What Evidence Do We Have Until Now?
At the beginning of SARS-CoV-2 pandemic, DM was called as one of the comorbidities with worse outcomes and highest mortality rates. However, researchers have discovered and are gathering up information about NDDM and how these patients may have a worse outcome than patients who had already been diagnosed with DM before the infection with COVID-19 [9•, 17]. A retrospective study found that 4.0% of the patients (n = 1902) had NDDM, and they reported that 42.9% of them had evidence of prediabetes prior to hospital admission. Additionally, they reported that NDDM was more common in younger patients and less common in non-Hispanic white patients and that inflammatory parameters were higher in these patients, longer ICU stay, but not in deaths [10]. The CORONADO study found that 2.8% (80 patients) of the patients they analyzed had NDDM and that these patients were younger than those who had already been diagnosed (60.2 ± 12.5 vs 70.5 ± 12.3 years, p < 0.001), and the majority were of African or Caribbean origin (31.1 vs 16.7%, p = 0.0055) (Table 2). The interesting fact is that NDDM patients did not have as many comorbidities as the previously diagnosed patients, but still had a more severe infection [9•]. In another study, they analyzed retrospectively 453 patients from Wuhan China with severe acute respiratory syndrome caused by COVID-19. They classified patients into groups based on glucose levels and separated patients with an existing DM diagnosis. The results showed that NDDM patients had the highest probability of admission to the ICU (11.7%) [7]. These results can be compared to the ones obtained by Fadini G et al. in a study that included 437 patients who tested positive for COVID-19 in Italy, including 107 who had DM, of which 21 had NDDM; NDDM had a stronger association with ICU admission or death compared to patients with pre-existing DM (RR 1.55, 95% C.I. 1.06–2.27; p = 0.004) [30]. A discrepancy still exists between the results, as some indicate that NDDM patients have a poorer prognosis than previously diagnosed patients, while others do not.
Long-term NDDM-related outcomes are still being investigated; according to a meta-analysis, patients post-acute COVID-19 have a 59% higher risk of developing NDDM than healthy controls (HR:1.59; 95% CI:1.40–1.81, p < 0.001, I2 = 94%, random-effects model) [31]. Maestre-Muñiz M et al. evaluated patients one year after hospitalization due to complications of the infection, in order to analyze the long-term effects caused by COVID-19. Regarding NDDM, they found out that 1.3% of the patients (n = 543) had been diagnosed with the condition during 1 year of recovery, that patients with a previous diagnosis required higher doses of oral antidiabetic drugs and insulin, and that some had developed DM complications like diabetic retinopathy or peripheral neuropathy [32]. According to another study, 56.3% of NDDM patients continue to have DM and that 40.6% had glycemic parameters back to normal range or prediabetes [10].
Could Lifestyle Changes During COVID-19 Lockdown Have an Effect on NDDM?
It has been well established that the pandemic has caused multiple changes in the lifestyle of people. The quality of diet changed according to a study performed in North India, reporting an increase in carbohydrate and fat intake during the pandemic compared to before (21% and 13% increased intake, respectively) [33]. These results can be compared to the ones obtained by Ammar A et al. which performed an international online survey of 1047 subjects. The surveys showed that when compared to before lockdown, unhealthy food consumption and “eating out of control” were significantly higher during lockdown (t = − 3.46, p < 0.001; t = − 9.44, p < 0.001, respectively) [34].
In terms of physical activity during the pandemic, it was found that minutes/day of general physical activity, vigorous activity, and moderate activity decreased by 33.5%, 33.1%, and 33.4%, respectively (p < 0.001) [34]. Furthermore, 87% of subjects reported high psychological stress during lockdown in Ghosh A et al. study [33]. The combination of these results with the fact that there is an association between physical inactivity, changes in dietary habits, and insulin resistance could provide a potential explanation for the changes in NDDM [35, 36]. As evidenced by Ghosh A et al., the NDDM patients diagnosed during pandemic had a higher fasting blood glucose, postprandial blood glucose, glycated hemoglobin, and fasting C-peptide when compared patients diagnosed with DM before the pandemic [37]. All of these changes during the pandemic, even though necessary in order to flatten the curve, may have negatively impacted patients, increasing the risk of NDDM and the differences seen between NDDM during COVID-19 pandemic and before the pandemic started.
Conclusion
There are many theories surrounding the causes of NDDM, including β-cell dysfunction, systemic inflammation, medication use, and metabolic and hormonal disturbances. It is possible that NDDM is caused by a combination of all of these systemic effects as well as lifestyle changes. There is still a lack of definitive evidence regarding the definition, duration, and etiology of NDDM. There are a number of challenges in studying NDDM, including a lack of reports on prediabetes and other conditions that may predispose to the condition. To better understand how to prevent and treat this long-term sequela of COVID-19, as well as future treatment options, more evidence is needed.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
World Health Organization. WHO coronavirus disease (COVID-19) dashboard with vaccination data | WHO coronavirus (COVID-19) dashboard with vaccination data. World Heal Organ. Published online 2022. Accessed July 23, 2022. https://covid19.who.int/
Alkodaymi MS, Omrani OA, Fawzy NA, et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: a systematic review and meta-analysis. Clin Microbiol Infect. 2022;28(5):657–66. https://doi.org/10.1016/j.cmi.2022.01.014.
National Institute for Health and Care Excellence (NICE) SIGN (SIGN) and RC of GP (RCGP). COVID-19 rapid guideline: managing the long-term effects of COVID-19. Published online 2022:1–106.
Xie Y, Al-Aly Z. Risks and burdens of incident diabetes in long COVID: a cohort study. Lancet Diabetes Endocrinol. 2022;10(5):311–21. https://doi.org/10.1016/S2213-8587(22)00044-4.
Steenblock C, Richter S, Berger I, et al. Viral infiltration of pancreatic islets in patients with COVID-19. Nat Commun. 2021;12(1). https://doi.org/10.1038/s41467-021-23886-3
Reiterer M, Rajan M, Gómez-Banoy N, et al. Hyperglycemia in acute COVID-19 is characterized by insulin resistance and adipose tissue infectivity by SARS-CoV-2. Cell Metab. 2021;33(11):2174-2188.e5. https://doi.org/10.1016/j.cmet.2021.09.009.
Li H, Tian S, Chen T, et al. Newly diagnosed diabetes is associated with a higher risk of mortality than known diabetes in hospitalized patients with COVID-19. Diabetes Obes Metab. 2020;22(10):1897. https://doi.org/10.1111/DOM.14099.
•• Montefusco L, Ben Nasr M, D’Addio F, et al. Acute and long-term disruption of glycometabolic control after SARS-CoV-2 infection. Nat Metab. 2021;3(6):774–85. https://doi.org/10.1038/s42255-021-00407-. Montefusco L et al described in a complete manner all of the changes regarding metabolic control and disorders, which contribute information that is needed in order to understand this article.
• Cariou B, Pichelin M, Goronflot T, et al. Phenotypic characteristics and prognosis of newly diagnosed diabetes in hospitalized patients with COVID-19: results from the CORONADO study. Diabetes Res Clin Pract. 2021;175(January):108695. https://doi.org/10.1016/j.diabres.2021.108695. The CORONADO study provided major results in describing the characteristics of newly diagnosed diabetes, which contributes to the explanation of this outcome in patients and also provides valuable information regarding the prognosis and differences wirh pre-existing diabetes.
Cromer SJ, Colling C, Schatoff D, et al. Newly diagnosed diabetes vs pre-existing diabetes upon admission for COVID-19 Associated factors, short-term outcomes, and long-term glycemic phenotypes. J Diabetes Complications. 2022;36(4):108145. https://doi.org/10.1016/j.jdiacomp.2022.108145.
Beisel W. Endocrine and immune system responses to stress. In: Food Components to Enhance Performance. National Academies Press; 1994:177–199. https://doi.org/10.17226/4563
• Bar-Or D, Rael LT, Madayag RM, et al. Stress hyperglycemia in critically Ill patients: insight into possible molecular pathways. Front Med. 2019;6:54. https://doi.org/10.3389/FMED.2019.00054/BIBTEX. Bar-Or et al. described possible metabolic alterations triggered by an infection, and the way in which they contribute to glycemic imbalance, which has relevance to our current article.
Huang Y, Guo H, Zhou Y, et al. The associations between fasting plasma glucose levels and mortality of COVID-19 in patients without diabetes. Diabetes Res Clin Pract. 2020;169:108448. https://doi.org/10.1016/j.diabres.2020.108448.
Sathish T, Kapoor N, Cao Y, Tapp RJ, Zimmet P. Proportion of newly diagnosed diabetes in COVID-19 patients: a systematic review and meta-analysis. Diabetes, Obes Metab. 2021;23(3):870–4. https://doi.org/10.1111/DOM.14269.
Bugra A, Das T, Arslan MN, Ziyade N, Buyuk Y. Postmortem pathological changes in extrapulmonary organs in SARS-CoV-2 rt-PCR–positive cases: a single-center experience. Ir J Med Sci. 2022;191(1):81. https://doi.org/10.1007/S11845-021-02638-8.
Cheung CCL, Goh D, Lim X, et al. Residual SARS-CoV-2 viral antigens detected in GI and hepatic tissues from five recovered patients with COVID-19. Gut. 2022;71(1):226–9. https://doi.org/10.1136/GUTJNL-2021-324280.
Yavropoulou MP, Filippa MG, Mantzou A, et al. Alterations in cortisol and interleukin-6 secretion in patients with COVID-19 suggestive of neuroendocrine-immune adaptations. Endocrine. 2022;75(2):317–27. https://doi.org/10.1007/S12020-021-02968-8/FIGURES/5.
Reiterer M, Rajan M, Gomez-Banoy N, et al. Hyperglycemia in Acute COVID-19 is characterized by adipose tissue dysfunction and insulin resistance. medRxiv. Published online May 5, 2021. https://doi.org/10.1101/2021.03.21.21254072
Caterino M, Gelzo M, Sol S, et al. Dysregulation of lipid metabolism and pathological inflammation in patients with COVID-19. Sci Rep. 2021;11(1):2941. https://doi.org/10.1038/S41598-021-82426-7.
Di Filippo L, De Lorenzo R, Sciorati C, et al. Adiponectin to leptin ratio reflects inflammatory burden and survival in COVID-19. Diabetes Metab. 2021;47(6): 101268. https://doi.org/10.1016/J.DIABET.2021.101268.
Li J, He X, Zhang W, et al. Meta-analysis investigating the relationship between clinical features, outcomes, and severity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia. Am j infect Control. 2020;(January). https://doi.org/10.1016/j.ajic.2020.06.008
National Institutes of Health. COVID-19 Treatment guidelines panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. Published 2022. Accessed July 26, 2022. https://www.covid19treatmentguidelines.nih.gov/therapies/immunomodulators/corticosteroids/
Li G. Inpatient use of glucocorticoids may mediate the detrimental effect of new-onset hyperglycemia on COVID-19 severity. Diabetes Res Clin Pract. 2020;168:108441. https://doi.org/10.1016/j.diabres.2020.108441.
Cardoza-Jiménez KJ, Carranza-Zavala B, Manrique-Franco K, Espinoza-Morales F, Mejia CR. Daily glucose variation influenced by the use of corticosteroids in COVID-19 patients treated in Lima-Peru. Diabetes Metab Syndr Clin Res Rev. 2021;15(4):102188. https://doi.org/10.1016/J.DSX.2021.102188.
Chaudhuri D, Sasaki K, Karkar A, et al. Corticosteroids in COVID-19 and non-COVID-19 ARDS: a systematic review and meta-analysis. Intensive Care Med. 2021;47(5):521–37. https://doi.org/10.1007/S00134-021-06394-2/FIGURES/3.
•• Wu CT, Lidsky PV, Xiao Y, et al. SARS-CoV-2 infects human pancreatic β cells and elicits β cell impairment. Cell Metab. 2021;33(8):1565-1576 e5. https://doi.org/10.1016/j.cmet.2021.05.013. Wu CT et al described important aspects regarding the infectivity and impairment that COVID-19 causes in the pancreas of infected patients, these results are relevant to the article and to understanding how the disease works.
Fignani D, Licata G, Brusco N, et al. SARS-CoV-2 receptor angiotensin I-converting enzyme type 2 (ACE2) is expressed in human pancreatic β-cells and in the human pancreas microvasculature. Front Endocrinol (Lausanne). 2020;11(November):1–19. https://doi.org/10.3389/fendo.2020.596898.
Müller JA, Groß R, Conzelmann C, et al. SARS-CoV-2 infects and replicates in cells of the human endocrine and exocrine pancreas. Nat Metab. 2021;3(2):149–65. https://doi.org/10.1038/s42255-021-00347-1.
Gao Q, Zhang W, Li T, et al. Interrelationship between 2019-nCov receptor DPP4 and diabetes mellitus targets based on protein interaction network. Sci Rep. 2022;12(1):1–8. https://doi.org/10.1038/s41598-021-03912-6.
Fadini GP, Morieri ML, Boscari F, et al. Newly-diagnosed diabetes and admission hyperglycemia predict COVID-19 severity by aggravating respiratory deterioration. Diabetes Res Clin Pract. 2020;168. https://doi.org/10.1016/J.DIABRES.2020.108374
Banerjee M, Pal R, Dutta S. Risk of incident diabetes post-COVID-19: a systematic review and meta-analysis. Prim Care Diabetes. 2022;(January). https://doi.org/10.1016/j.pcd.2022.05.009
Maestre-Muñiz MM, Arias Á, Mata-Vázquez E, et al. Long-term outcomes of patients with coronavirus disease 2019 at one year after hospital discharge. J Clin Med. 2021;10(13). https://doi.org/10.3390/JCM10132945/S1
Ghosh A, Arora B, Gupta R, Anoop S, Misra A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India. Diabetes Metab Syndr. 2020;14(5):917. https://doi.org/10.1016/J.DSX.2020.05.044.
Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 Home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. 2020;12(6). https://doi.org/10.3390/NU12061583
Kelly SJ, Ismail M. Stress and type 2 diabetes: a review of how stress contributes to the development of type 2 diabetes. Annu Rev Public Health. 2015;36:441–62. https://doi.org/10.1146/ANNUREV-PUBLHEALTH-031914-122921.
Kim KS, Kim SJ, Kim S, Choi DW, Ju YJ, Park EC. Association of self-reported sedentary time with insulin resistance among Korean adults without diabetes mellitus: a cross-sectional study. BMC Public Health. 2018;18(1):1–8. https://doi.org/10.1186/S12889-018-6237-4/TABLES/3.
Ghosh A, Anjana RM, Shanthi Rani CS, et al. Glycemic parameters in patients with new-onset diabetes during COVID-19 pandemic are more severe than in patients with new-onset diabetes before the pandemic: NOD COVID India Study. Diabetes Metab Syndr Clin Res Rev. 2021;15(1):215–20. https://doi.org/10.1016/j.dsx.2020.12.033.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and analysis were performed by Nicole Knebusch Toriello, Natalia María Prato Alterio, and Lourdes María Ramirez Villeda. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interest.
Human and Animal Rights Statement
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Metabolism in Tropical Medicine
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Knebusch Toriello, N., Prato Alterio, N.M. & Ramírez Villeda, L.M. Newly Diagnosed Diabetes Mellitus During COVID-19: The New Pandemic – A Literature Review. Curr Trop Med Rep 9, 250–256 (2022). https://doi.org/10.1007/s40475-022-00268-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40475-022-00268-3