Abstract
Purpose of review
In this study we describe the impact of COVID-19 infection on the immunological response of kidney transplant recipients of a single transplant center. We evaluated the seroconversion after vaccination and COVID-19 disease, the management of immunosuppressive therapy, and the effects of the withdrawal of immunosuppressive therapy on renal function and clinical outcome.
Recent findings
A prospective and cross-sectional observational study was performed on 156 kidney transplant recipients with a positive PCR test for SARS-CoV-2 and vaccinated with mRNA vaccine from November 2021 to September 2022. After examining the anti-Spike antibody production before and after COVID-19 infection, we detected a significant increase after disease both in kidney transplant recipients with three doses (p = 0.011, 180.9 vs. 1186 IU/mL) and with four doses of vaccine (p = 0.002, 19.5 vs. 1557.0 IU/mL). We also observed a correlation between age and critical symptoms of COVID-19 disease (p = 0.005, R = 0.224); the pre-COVID-19 antibody levels are found to be linearly correlated to resolution time of disease (p = 0.05, F = 3.986). Regarding the management of immunosuppressive therapy after infection, we noticed that the kidney transplant recipients with mycophenolate mofetil withdrawal had a stable graft function, in terms of serum creatinine and proteinuria, and a significant increase of the immune response, expressed as SARS-CoV-2 seroconversion (1557.0 vs. 32.4 IU/mL, p = 0.001).
Summary
We learned how to manage kidney transplant recipients affected by Covid-19 with patient-tailored therapy, thus improving the disease outcome without worsening the renal function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Some 3 years ago, the viral sequence of a new virus was deposited in the international database virological.org: this was called SARS-CoV-2 (severe acute respiratory syndrome coronavirus) [1]. The latter was found to be responsible for the COVID-19 (coronavirus disease-19) pandemic, and in recent years, the coronavirus has officially caused the deaths of almost 7 million people worldwide. This might be a somewhat cautious, conservative estimate: according to data released in December 2022 by the World Health Organization (WHO), indeed, deaths from Covid-19 could even be twice as high [2]. However, without the vaccines, that were made available since January 2021, the scenario might have been much worse. In fact, anti-SARS-CoV-2 mRNA vaccines unlocked the situation, paving the way to a gradual return to everyday life. Developed in a stunningly short amount of time — although mRNA technology had already been under study for over a decade in the oncological field — the first injections took place at the end of 2020.
A great step forward in the battle against the pandemic consisted in the arrival of the first antiviral drugs developed specifically against SARS-CoV-2. Furthermore, the antiviral drugs may be a viable option in kidney transplant recipients (KTRs) with limited access to monoclonal antibodies, due to significant drug–drug interactions with immunosuppressive agents [3]. Transplanted subjects are critical patients, owing to their pharmacologically induced immunosuppression. A lowered lymphocyte B activation leads, indeed, in these subjects to a reduced antibody production both after vaccination and COVID-19 disease [4,5,6].
For this reason, disease management in these immunosuppressed individuals requires the application of a personalized therapy after transplantation, considering the risks and benefits of therapy for the patient [7, 8].
Several factors complicate the risk of infection in KTRs, like a shorter time since transplant (for the heavier immunosuppression regimens) and triple immunosuppressive therapy, but the development of therapies for SARS-CoV-2 infection, like monoclonal antibodies, antiviral agents, and vaccines [9, 10], has represented a pivotal change to the evolution of the pandemic.
In this study, we aimed to describe 3 years after the onset of the pandemic disease the impact of COVID-19 infection on a population of KTRs of a single transplant center in Italy. Specifically, we report, here, our evaluation of the seroconversion after vaccination and COVID-19 disease, the management of immunosuppressive therapy, and the effects of the withdrawal of immune-suppressive therapy on renal function and clinical outcome.
Materials and Methods
A prospective and cross-sectional observational study was performed on 156 KTRs, followed up at the Organ Transplant Center in L'Aquila from November 2021 to September 2022 with a positive reverse transcriptase-PCR test for SARS-CoV2. The cohort study included all patients aged 18 years or older with a diagnosis of SARS-CoV-2 infection. Despite the lack of knowledge of the SARS-CoV-2 viral variant in these patients, we can speculate that recipients considered in this period may have been infected by variants as indicated in the 2021–2022 reports from the National Institute of Health (ISS): the predominant one between November 2021 and January 2022 in Italy was the so-called Delta variant, while from February 2022 to September 2022 it was the Omicron one. Patients were followed at home or continuously monitored over time through the collection of clinical data and medical reports if they were hospitalized. The hospitalization was indicated in cases of moderate-severe or critical disease. Subsequently, after a negative test, the patients were monitored in the outpatient clinic. They were followed up once a month for 6 months; afterwards, the follow-up protocol depended on their specific clinical conditions. During the outpatient checkup, patients underwent blood count, renal function (creatinine, proteinuria), liver function, and anti-HLA antibody response. Demographic data (age, sex, etiology of primary kidney disease, type of donor, duration of follow-up, maintenance immunosuppression therapy, and other drugs), clinical characteristics (duration of hospitalization, symptoms after Covid-19 infection, laboratory results), and COVID-19 medication were collected from electronic medical records. Every patient was SARS-CoV-2 vaccinated with two, three, or four doses of the anti-SARS-CoV-2 mRNA Comirnaty (BNT162b2, Pfizer/BionTech) monovalent vaccine. All participants provided written informed consent, in accordance with the Declaration of Helsinki Ethical Principles for Medical Research involving Human subjects. We evaluated the anti-Spike seroconversion after administration of the last vaccine dose (mRNA Pfizer), about 53 days later (median value, IQR: 28.5–105.0 days), and after about 1 month from the COVID-19 positivity (median value: 29.5 days, IQR: 21.2–51.2 days). The relevant parameter taken into consideration was the serum value of anti-SARS-CoV-2 Spike IgG evaluated after the administration of the last vaccine and the value after the infection by means of blood sampling and enzyme-linked immunosorbent assay. The amount of 15 IU/mL was considered the cutoff value marking the threshold between failure and successful seroconversion.
Immunosuppressive regimen was changed in patients with positive test for SARS-CoV-2. Patients with asymptomatic or mild disease had mycophenolate reduced. Mycophenolate withdrawn was indicated for patients with moderate symptoms. In patients with severe symptoms, we interrupted both mycophenolate mofetil (MMF) and tacrolimus. Mycophenolate and tacrolimus were reintroduced at their usual dosage after negative COVID-19 tests.
We considered “asymptomatic” the individual with no symptoms. We defined with “mild disease” the patients without shortness of breath, dyspnea, or abnormal chest imaging. We talked of “moderate symptoms” if patients showed evidence of lower respiratory disease during clinical assessment or imaging and an oxygen saturation ≥ 94%. If the oxygen saturation was < 94%, we talked of “severe illness.”
Furthermore, the degree of severity of the symptoms after the COVID-19 infection, the humoral anti-Spike response, and the use of monoclonal antibodies and the recovery time from the disease were also considered.
Statistical Analysis
The clinical and experimental data have been analyzed through standard statistical tools and have been interpreted via mean (SD) or (in the presence of a skewed distribution) median (IQR) values. Kurtosis has been measured to check whether the data follow a normal distribution. To compare the characteristics of the groups, Fisher’s exact test or Pearson’s X2 (categorical variables) or the Mann–Whitney U test, as appropriate, was used. The characteristics of the groups with or without seroconversion and other clinical events were calculated using the Wilcoxon signed rank analysis of variance for nonparametric paired continuous variables and with the X2 test for the categorical variables. Values were considered statistically significant with 2-tailed p ≤ 0.05. Binary logistic regression analyses were also performed to evaluate dichotomous differences between groups for different variables. Only the statistically significant variables in the univariate analysis (p < 0.1) were included in a multivariate logistic regression, and a backward conditional method was chosen to select significant independent covariates. All the factors considered in the univariate analysis were derived from data in the literature or from clinical data. In the multivariate logistic regression for the risk factors of the anti-Spike antibody response, in addition to significance ≤ 0.05, we used the odds ratio (OR; risk index), Wald factor (how the independent variable increases the risk of the dependent variable), 95% CI, and beta coefficient (standardized regression coefficient). The correlation between the variables was performed with the Pearson or Spearman test, depending on the distribution of the data (parametric or nonparametric) by evaluating their significance (p < 0.05) and the correlation coefficient R (value from 1 to + 1). The calculations and graphic processing were performed using SPSS v.13.0 software (IBM SPSS, Inc, Armonk, NY) and GraphPad Prism 8 (GraphPad Software, La Jolla, CA).
Results
Demographic and clinical parameters of the patients’ cohort with COVID-19 infection are illustrated in Table 1. The mean age of the KTRs was 57.2 years and the cohort was composed of 53 females and 103 males. A total of 140 patients were transplanted from deceased donor and 16 from living donors. Out of the 156 patients considered, 8.9% had received only two doses of mRNA vaccine, 75.8% three doses of vaccine, 14.6% four doses, and 0.7% no dose. Regarding immunosuppressive therapy, 114 patients at the time of enrollment were treated with the TAC-MMF-corticosteroids (CS) triple regimen, 9 patients with TAC-MMF without CS, 7 patients with TAC-EVE-CS, 20 patients with cyclosporine A (CsA), and 6 with other regimens.
After COVID-19 infection, 11.5% of patients had been hospitalized, 80.8% developed a mild disease, 10.9% developed a moderate-severe disease, 5.1% had critical symptoms, and 22.3% had a long Covid. The mean time of disease resolution was 14.6 days (± 6.7 days). Seven patients (4.5%) died of pneumonia. In four cases after COVID-19 disease, a biopsy-proven organ rejection episode occurred (2.6%).
Immunosuppressive regimen was changed in COVID-19-affected recipients. Mycophenolate mofetil (MMF) (n = 10), or everolimus (EVE) (n = 10), was reduced in patients with asymptomatic or mild disease. Mycophenolate withdrawal was prescribed to patients reporting mild or moderate symptoms (n = 86). In patients with severe symptoms, we interrupted both mycophenolate mofetil (MMF) and tacrolimus (TAC) (n = 9). MMF and TAC were reintroduced at their usual dosage after negative tests. In patients undergoing biopsy, due to the worsening of the renal function, MMF was not paused longer than in other patients. Such patients had mild disease and had no prior risk factors for rejection. None of the four patients had donor-specific antibodies (DSA) before disease. In one case, it was a living donor transplant (donor mother) and the biopsy after Covid positivity showed a cell-mediated acute rejection. This patient was successfully treated with cortisone boluses. In two cases, the biopsy revealed a chronic active antibody-mediated rejection, and in one of the two, there was the appearance of de novo DSA development. In one case, a transplant glomerulopathy was also found. The mean follow-up time was 8 months (range: 4–12 months).
1. Seroconversion and Covid-19.
Examining altogether the pre- (n = 67) and post-COVID-19 (n = 51) anti-Spike antibody levels in KTRs, we observed a significant increase in the post-period (median values: 1190.0 IU/mL, IQR = 595.2–2380.0 vs. pre-Covid-19: 127.8 IU/mL, IQR = 4.0–1004.0, Mann–Whitney p < 0.0001). Precisely, in 33 transplant recipients with both pre- and post-COVID-19 anti-spike antibody dosing, the difference was remarkable (p = 0.005, Wilcoxon paired-rank test).
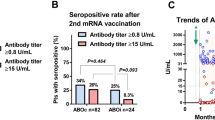
Upon distinguishing patients by the number of SARS-CoV-2 vaccine doses performed, the anti-Spike antibody production before and after Covid-19 infection showed significant differences, both in the case of KTRs with two doses of vaccine (p = 0.042, median: 33.5 UI/mL, IQR = 4.0–135.0 vs. 1229.0, IQR = 374.8–24,543.0), three doses (p = 0.011, 180.9 UI/mL, IQR: 4.0–1632.0 vs. 1186, IQR = 417.9–1795.0 UI/ml), and four doses (p = 0.002, 19.5 UI/mL, IQR: 11.4–391.2 vs. 1557 UI/mL, IQR: 730.9–5410.0 UI/mL), individually (see Fig. 1). However, differences in post-Covid-19 antibody levels in KTRs after 3 or 4 doses were not significant (p = 0.341), even if the antibody mean titers in recipients with 4 doses were doubled (mean: 4911.5 IU/mL ± SD 7108.5 vs. 2233.2 IU/mL ± 3259.10).
Comparison of anti-Spike antibody response measured before and after COVID-19 infection (IU/mL), stratified for number of vaccine doses in KTRs with MMF withdrawal and maintenance of IS therapy. Column bar graph of data (mean with SD). *2 vaccine doses: p = 0.042; **3 vaccine doses: p = 0.011; **4 vaccine doses: p = 0.002, Wilcoxon signed ranks
The number of prior vaccinations did not significantly affect the severity of the disease, despite the fact that we observed a moderate/severe or critical presentation of disease in 28.6% (4/14 pts, 1 death) of KTRs with 2 doses, in 17.8% (21/118, 6 deaths) with 3 doses, and in 0.0% (0/21) with 4 doses.
It is also worth pointing out that the seroconversion rate after Covid-19 disease turned out not to be significantly affected by the type of the variant, whether it was the Delta or the Omicron one. The difference, in fact, is not significant (p = 0.853, median Delta 1274 IU/mL and Omicron 1257 IU/mL).
In our sample, the severity of the disease did not have a noteworthy impact on the development of antibodies after infection. In fact, the difference in post-COVID antibody production in asymptomatic/mild patients versus moderate/severe-critical patients appears not to be very significant (p = 0.077; Mann–Whitney U test: median 1557 vs. 268.6 IU/mL), probably due to the low number of patients with severe symptoms.
2. Correlation between demographic, clinical data, and anti-Spike pre- and post-COVID-19 seroconversion.
The analysis of Spearman’s R-test between the seroconversion and clinical data leads us to the following conclusions: (a) there exists a positive correlation between age and critical symptoms of COVID-19 disease (p = 0.005, R = 0.224) and a negative one with healing time (p = 0.006, R = − 0.223); (b) there also exists a negative correlation of pre-COVID-19 anti-Spike antibody levels with the times of recovery from the disease (p = 0.001, R = − 0.416), with the usage of MMF (p = 0.001, R = − 0.388) and/or TAC (p = 0.011, R = − 0.308) in IS regimens and with triple therapy (p = 0.012, R = − 0.303). The pre-COVID-19 antibody levels and resolution time of disease follow a linear regression trend (p = 0.05, F = 3.986, beta = − 0.242); (c) the pre-COVID-19 seroconversion is negatively related to an earlier period after transplantation (4–5 years: p = 0.05, R = − 0.238 or 6–10 years: p = 0.017, R = − 0.289), while it increases after 10 years from transplantation (p = 0.026, R = 0.271), as previously described in our previous analysis on risk factors for a low immune response to SARS-CoV-2 vaccination in KTRs [10]; (d) a negative correlation also exists between post-COVID-19 antibody levels and triple therapy (p = 0.012, R = − 0.303) and between cyclosporine use and healing time (p = 0.007, R = − 0.222) (cf. Table 2).
Moreover, an univariable logistic regression shows that the age of patient is an independent risk factor of moderate/severe (p = 0.046, Exp(B) = 1.062) to critical form (p = 0.011, OR = 1.127) of COVID-19 disease. Gender, on the other hand, is not related to symptoms. Furthermore, examining the association of the use of immunosuppressive regimens with TAC and/or MMF and pre-COVID-19 antibody production, an inhibitory effect of TAC alone on the antibody response (p = 0.050, Exp(B) = 0.121, B = -2.11) is confirmed, while the inhibitory effect of MMF becomes significant in transplant recipients only in combination, MMF/TAC (p = 0.017, Exp(B) = 0.147, B = − 1.919). A shorter time (years) since the transplant to vaccination is also negatively associated with pre-COVID-19 antibody production (p = 0.037, Exp(B) = 0.095, B = − 2.531). The multivariate regression of the two previous variables indicates a preponderant inhibitory role of the MMF/TAC regimen (p = 0.035, Exp(B) = 0.181, 95%CI: 0.037–0.884) on anti-Spike antibody production, which acts as an independent variable.
3. Impact of immunosuppressant management on clinical outcome after COVID-19 infection.
Patients with asymptomatic or mild disease had MMF reduced. MMF withdrawal was indicated for patients with moderate symptoms. In patients with severe symptoms, we interrupted both MMF and TAC. MMF and TAC were reintroduced at their usual IS dosage after anti-SARS-CoV-2 negative test. We examined the impact of this change of immunosuppressive therapy on renal function parameters and clinical outcome. Regarding the renal function, we noticed that MMF withdrawal appears to be negatively correlated with 24-h proteinuria levels in the post-COVID-19 period (Spearman’s r-test p = 0.079, r = − 0.153), as well as the TAC reduction (n = 5, p = 0.015, r = − 0.211). In addition, EVE reduction (n = 8) in a univariable regression resulted in an independent risk factor for anti-DSA antibodies production (p = 0.028, Exp(B) = 10.091, B = 2.312) after COVID-19.
Comparing altogether the pre- and post-COVID-19 renal function parameters, a significant difference in proteinuria values (p = 0.044, Wilcoxon signed ranks, median value: 228 mg/L vs. 185 mg/L) and class II PRA antibodies (p = 0.002, median: 0.50% vs. 0.30%) was observed, while creatinine and anti-DSA antibodies were not significantly different. Distinguishing KT recipients with (n = 98) and without (n = 47) MMF withdrawal, we evidenced a stable graft function after Covid-19 infection, regarding creatinine (MMF withdrawal: median value 1.46 (IQR = 1.08–1.98) vs. 1.51 mg/dL (IQR = 1.08–1.91), p = NS and standard IS therapy: 1.39 (IQR = 1.07–2.07) vs. 1.35 mg/dL (IQR = 1.03–1.88), p = 0.016) (Fig. 2), and proteinuria, with an improvement in patients without MMF (median value: 172.5.0 mg/L vs. 281.0 mg/L, Mann–Whitney U test p = 0.079) (Fig. 3).
Renal function monitoring before and after COVID-19 infection: creatinine levels (mg/dL), stratified for MMF withdrawal and maintenance of IS therapy. Box plot distribution of data (10–90% percentile) with median value. Stable serum creatinine values in KTRs both with MMF withdrawal (median value: 1.46 (IQR = 1.08–1.98) vs. 1.51 mg/dL (IQR = 1.08–1.91), p = NS and standard IS therapy: 1.39 (IQR = 1.07–2.07) vs. 1.35 mg/dL (IQR = 1.03–1.88), p = 0.016)
Renal function monitoring before and after COVID-19 infection: proteinuria at 24H (mg/L), stratified for MMF withdrawal and standard IS therapy. Box plot distribution of data (10–90% percentile) with median value. Reduced proteinuria values in KTRs with MMF withdrawal after COVID-19 in comparison to patients with standard IS (median value: 172.5.0 mg/L vs. 281.0 mg/L, Mann–Whitney U test, p = 0.079)
Regarding the seroconversion after the COVID-19 infection, we evidenced a significant increase of antibody titers in patients with MMF withdrawal (median values: 1557.0 vs. 32.4 IU/mL, p = 0.001, Wilcoxon signed ranks), with median values even twice as high as those of patients with standard IS therapy (1557.0 vs. 712.0 IU/mL, p = 0.078). Moreover, patients with MMF suspension had a significant reduction of the class II PRA antibody response (p = 0.010, 0.30% vs. 0.45%), while the DSA increased after Covid-19 infection (61.5% vs. 38.5% with standard IS therapy).
Discussion
Based on the current literature, it should be emphasized that even in the healthy population, individuals affected by mild-to-moderate COVID-19 disease demonstrate a robust immunoglobulin G-antibody response against the viral spike protein. Furthermore, these titers remain stable for at least 5 months after infection [11].
This observational study showed that after SARS-CoV-2 infection also in KTRs the seroconversion significantly increases 1 month after infection, if compared to the neutralizing response induced by vaccines, both in patients receiving three doses and even more strongly in those treated with 4 doses of the vaccine. This finding is in agreement with recent research by Benning L et al. [12], who however by studying a smaller sample of patients had observed a stronger neutralizing response against COVID-19 variants of concern, compared with 2-dose BNT162b2 vaccination in renal transplant recipients.
Considering demographics and clinical features of these transplanted patients affected by COVID-19, we noticed that an older age of recipients represents a risk factor for the onset of a severe form of disease. Moreover, we also found that the pre-COVID-19 antibody levels are linearly correlated to recovery time from infection and that the immunosuppressive therapy influences the seroconversion induced by vaccines. In particular, the use of MMF, TAC, or triple IS regimen has an inhibitory effect on seroconversion. These results confirmed our previous analysis on risk factors for a low immune response to SARS-CoV-2 vaccination in kidney transplant recipients [9].
Another important outcome of our analysis concerns the effect of the immunosuppressive change after COVID-19 infection in kidney transplant recipients. Since the outbreak of the pandemic, it was recommended to reduce the use of anti-proliferative medication after COVID-19 infection. On the other hand, the maintenance of calcineurin inhibitors (CNIs) was also recommended [13]. However, stopping or decreasing these drugs may lead to harmful outcome, such as allograft rejection [14]. CNIs seem to have a role in increasing COVID-19-induced cytokine storm. CNIs inhibit T-cell activation and suppress cytokines interleukin (IL)-2, IL-4, tumor necrosis factor-a, and interferon-γ, which mediate the cytokine storm, very harmful after infection [15]. Also, mTOR inhibitors seem to hinder the effect of IL-37 and IL-38 in the inflammatory state, determining a potential anti-COVID-19 effect [16].
In our analysis, we observed that the kidney transplant recipients affected by COVID-19 who were subject to MMF withdrawal had a stable graft function, in terms of serum creatinine and proteinuria within the first 3 months after disease. In addition, such discontinuation induced a significant increase of the immune response, expressed as neutralizing activity against SARS-CoV-2 virus, after at least 1 month from disease, and anti-DSA humoral response. This effect has been already observed in previous studies by Kühn T. et al. [17] on non-responder kidney transplant recipients after short-term suspension of mycophenolate mofetil, ensuing from an additional vaccine dose. On the other hand, this immunosuppressive change reduced class II PRA antibody response towards graft. For this reason, MMF withdrawal should be critically evaluated in addition to vaccines to enhance the humoral response after SARS-CoV-2 infection, thus improving clinical outcomes without damaging graft function. Because also other agents influence seroconversion, attention should be paid to immunosuppressant dosages and interaction with antiviral and other drugs in kidney transplant recipients. Our clinical experience suggests that the management of immunosuppressants (reduction or withdrawal) may represent a useful therapeutic choice in kidney transplant patients infected by COVID-19, depending on the specific patient’s conditions.
It is noteworthy that our study concerns a quite large cohort of kidney transplant recipients, which allowed us to collect a reasonably high number of clinical data that have been meaningfully analyzed and interpreted. We also point out that the outcome of our research endeavor is a prospective study, in which all patients were regularly followed up by the medical staff of the transplant center.
Our study paves the way to a future research development, which may focus, for instance, on a more systematic analysis of the correlation existing between the severity of the disease and SARS-CoV-2 antibody titers in the post-infection regime with the causative SARS-CoV-2 strain. However, it would be interesting to investigate other correlated immunological factors such as the cellular response.
Conclusion
Three years after the outbreak of the pandemic, we have learned how to manage the COVID-19 infection even in the most fragile patients, such as renal transplant recipients. In our clinical experience, we have studied the results stemming from changes in the immunosuppressive therapy. The introduction of patient-tailored immunosuppressive regimens, combined with a mass COVID-19 vaccination and antiviral therapies, allowed us to safely treat transplanted patients affected by COVID-19 infection.
Data Availability
The data that support the fundings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus
- COVID-19:
-
Coronavirus disease-19
- WHO:
-
World Health Organization
- KTR:
-
Kidney Transplant Recipient
- ISS:
-
Italian National Institute of Health
- IS:
-
Immunosuppressive
- TAC:
-
Tacrolimus
- MMF:
-
Mycophenolate mofetil
- EVE:
-
Everolimus
- CS:
-
Corticosteroids
- CsA:
-
Ciclosporine A
- DSA:
-
Donor-specific antibodies
- CNI:
-
Calcineurin inhibitor
References
Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–33.
Msemburi W, Karlinsky A, Knutson V, Aleshin-Guendel S, Chatterji S, Wakefield J. The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature. 2023;613(7942):130–7.
Radcliffe C, Palacios CF, Azar MM, Cohen E, Malinis M. Real-world experience with available, outpatient COVID-19 therapies in solid organ transplant recipients during the omicron surge. Am J Transplant. 2022;22(10):2458–63.
Tavares J, Oliveira JP, Reis P, Ribeiro B, Silva F, Malheiro J, Almeida M, Martins S, Cabrita A, Henriques AC, Dias L. COVID-19 in kidney transplant recipients: what have we learned one year later? A cohort study from a tertiary center. J Bras Nefrol. 2022;44(4):533–42.
Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97(5):829–38.
Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–6.
Lai Q, Spoletini G, Bianco G, Graceffa D, et al. SARS-COV-2 and immunosuppression: a double-edged sword. Transpl Infect Dis. 2020;22:e13404.
Abu Jawdeh BG. COVID-19 in kidney transplantation: outcomes, immunosuppression management, and operational challenges. Adv Chronic Kidney Dis. 2020;27(5):383–9.
Panarese A, Canossi A, Fabiani R, et al. Analysis of risk factors for a low immune response to messenger RNA COVID-19 vaccine in kidney transplant recipients and differences between second and third dose. Transplant Proc. 2022;54(10):2646–51.
Russo G, Lai Q, Poli L, Perrone MP, Gaeta A, Rossi M, Mastroianni CM, Garofalo M, Pretagostini R. SARS-COV-2 vaccination with BNT162B2 in renal transplant patients: risk factors for impaired response and immunological implications. Clin Transplant. 2022;36(1):e14495.
Wajnberg A, Amanat F, Firpo A, Altman DR, Bailey MJ, Mansour M, McMahon M, Meade P, et al. Robust neutralizing antibodies to SARS-CoV-2 infection persist for months. Science. 2020;370(6521):1227–30.
Benning L, Morath C, Bartenschlager M, Reineke M, Töllner M, Nusshag C, Kälble F, Reichel P, Schaier M, Schnitzler P, Zeier M, Süsal C, Bartenschlager R, Speer C. Natural SARS-CoV-2 infection results in higher neutralization response against variants of concern compared with 2-dose BNT162b2 vaccination in kidney transplant recipients. Kidney Int. 2022;101(3):639–42.
Daoud A, Alqassieh A, Alkhader D, Posadas Salas MA, Rao V, Fülöp T, Soliman KM. Immunosuppression in kidney transplant recipients with COVID-19 infection - where do we stand and where are we heading? Ren Fail. 2021;43(1):273–80.
Nair V, Jandovitz N, Hirsch JS, et al. COVID-19 in kidney transplant recipients. Am J Transplant. 2020;20(7):1819–25.
Hage R, Steinack C, Schuurmans MM. Calcineurin inhibitors revisited: a new paradigm for COVID-19? Braz J Infect Dis. 2020;24(4):365–7.
Conti P, Ronconi G, Caraffa A, et al. Induction of proinflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVID-19 or SARS-CoV-2): anti-inflammatory strategies. J Biol Regul Homeost Agents. 2020;34(2):327–31.
Kühn T, Speer C, Morath C, Bartenschlager M, Kim H, Beimler J, Buylaert M, Nusshag C, Kälble F, Reineke M, Töllner M, Klein K, Blank A, Parthé S, Schnitzler P, Zeier M, Süsal C, Bartenschlager R, Tran TH, Schaier M, Benning L. Immune response to COVID-19 mRNA vaccination in previous nonresponder kidney transplant recipients after short-term withdrawal of mycophenolic acid 1 and 3 months after an additional vaccine dose. Transplantation. 2023;107(5):1139–50.
Funding
Open access funding provided by Università degli Studi dell’Aquila within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
PA, CA, and PF were responsible for the conception, design, analysis, and writing of the study; PA, CA, and SV were involved with the collection and interpretation of data; PA, CA, and TDB participated in data management, review, and editing of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Canossi, A., Panarese, A., Savino, V. et al. COVID-19 in Kidney Transplant Recipients: What Did We Understand After Three Years Since the Pandemic Outbreak in Kidney Transplant Recipients?. Curr Transpl Rep 10, 253–260 (2023). https://doi.org/10.1007/s40472-023-00414-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-023-00414-4