Abstract
Purpose of Review
We explore how to develop Maastricht category I and II donation in the UK. We discuss lessons learned from previous UK pilots and define future steps in the journey to establishing a sustainable uDCD programme in the UK.
Recent Findings
The emergence of normothermic regional perfusion (NRP) as a successful strategy in cDCD donation with excellent clinical results creates the optimal platform for the development of a uDCD programme. Coordinated logistics with ambulance services and ED departments, embedded donor coordination in ED, public acceptance and wider discussion on acceptable peri-mortem interventions are key for future developments.
Summary
A uDCD programme in the UK is feasible. Despite an increase in public awareness and recent changes in legislation, there remain several challenges. Recent advances in perfusion and preservation and an established national retrieval infrastructure, create the premises for future sustainable developments.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
In the United Kingdom (UK), the number of deceased organ donors has almost doubled over the past decade. This achievement is in part attributed to the strategy to embrace organ donation as a usual part of end-of-life care as well as initiatives aimed at increasing consent and authorisation rates [1]. The number of donors after circulatory death (DCD) (previously known as donors after cardiac death or non-heart beating donors) has increased substantially and now accounts for approximately 40% of all deceased donation in the UK [2]. Despite this remarkable progress, there is an ongoing mismatch between the supply and demand of organs for transplantation and this necessitates the exploration of all possible means to further expand the donor pool.
Currently, all DCD donation in the UK is classified as “controlled” and occurs when a critically ill patient on the intensive care unit undergoes a planned and expected cardiac arrest following the withdrawal of life-sustaining cardiorespiratory support (Maastricht category III or IV, Table 1). Uncontrolled donation after circulatory death (uDCD) occurs after sudden and unexpected cardiac arrest and donors are either dead on arrival to hospital (Maastricht category I) or have had an unsuccessful attempt at resuscitation (Maastricht category II). Uncontrolled DCD has the potential to significantly increase the number of organs available for transplantation. Some countries such as Spain, Portugal, and France have successfully utilised uDCD Maastricht category II donors. Spain is the global leader in deceased organ donation with 49.6 deceased donors per million population (pmp) and 16.1 DCD donors pmp in 2019 [3]. By comparison, the 2019 deceased donor and DCD rates in the UK were 24.7 pmp and 10.3 pmp respectively, highlighting a substantial scope for improvement.
In the 1990s, a limited number of UK centres operated small uDCD programmes (Leicester, Newcastle and London) [4, 5, 6••]. These programmes became inactive as some of the practices used at that time (e.g. re-instituting cardiac massage after declaration of death) conflicted with revised ethical guidance and consensus statements for DCD donation, which deemed any intervention with the potential to inadvertently restore cerebral circulation as unacceptable [7, 8]. Furthermore, there was a reluctance to utilise uDCD organs due to the inevitably longer warm ischaemia times, leading to concern over poorer graft outcomes and ischaemic complications.
At the same time, the organ retrieval process in the UK has undergone significant changes and is now currently provided as a National Organ Retrieval Service (NORS) delivered by ten abdominal and six cardio-thoracic retrieval teams, on a zonal allocation.
The emergence of novel perfusion and preservation technologies such as normothermic regional perfusion (NRP) as a means of mitigating the warm ischaemic insult to DCD grafts [9, 10] has led to renewed interest in uDCD in the UK. NRP uses ECMO-like technology with a pump and an extracorporeal membrane oxygenator to restore blood circulation to the isolated abdominal organs prior to retrieval and allows recovery from warm ischaemia and replenishment of ATP reserves. Between 2013 and 2015, a pilot uDCD programme for donation from Maastricht category II donors using NRP was established at the Royal Infirmary of Edinburgh, Scotland [6••]. This review provides an overview of uDCD and discusses lessons learned and future steps in the journey to developing a uDCD programme in the UK.
UDCD Protocol
Prior to the introduction of the pilot uDCD programme in Edinburgh, extensive consultation with all relevant stakeholders took place including staff from the emergency department (ED), transplant and retrieval teams, the ambulance service, the procurator fiscal (PF) (equivalent of the coroner in England and Wales), the police, lawyers and patient representatives. A local protocol was developed (Fig. 1) which was based on the Spanish model and had similar inclusion criteria (Box 1), but was adapted to comply with the UK ethical, legal and logistical requirements. The ED were alerted by the ambulance service when a patient had a witnessed out of hospital cardiac arrest and the ED would in turn contact the specialist nurses in organ donation (SNODs). Only patients attended to by the ambulance service within 15 min were eligible for inclusion in the pilot. Out of hospital cardiopulmonary resuscitation (CPR) was commenced using an automated mechanical device, Autopulse® (Zoll®, USA) which uses load distributing band technology to deliver chest compressions. On arrival to hospital, resuscitation was continued as per national guidelines [11] to allow time for information gathering as to whether the patient was suitable for organ donation and to allow for discussions with the patient’s family. Up until the point that futility was declared, the SNODs did not have any interaction with the resuscitation team, the patient or the family. It was only after the resuscitation team leader had informed the patient’s family that resuscitation had been unsuccessful that the SNODs were introduced to the family. SNODs are highly trained in communication surrounding end-of-life decisions and used a staged approach by first seeking consent for organ preservation. If the family agreed to organ preservation, the surgical team were activated, resuscitation was stopped, death was declared and the mandatory 5 min “no-touch” period observed. The patient was transferred to a dedicated NRP room within the ED department that was geographically separated from the resuscitation area, but close enough to allow rapid transfer and commencement of organ preservation. The NRP room was set up in a way similar to the operating theatre to provide a sterile environment for cannulation. During NRP, the femoral artery was cannulated to allow perfusion of oxygenated blood to the abdominal organs using an extracorporeal membrane oxygenator circuit with venting through a catheter in the femoral vein. Perfusion was restricted to the abdominal compartment using an intra-aortic balloon that prevented re-perfusion of the brain and heart. The position of the radio-opaque balloon was confirmed on a plain radiograph and a balloon transducer port allowed measurement of the pressure above the balloon to confirm complete occlusion of the aorta. Absence of cerebral perfusion was confirmed with carotid ultrasound and radial artery pressure measurements. During organ preservation, the PF was contacted and if authorisation for organ donation was witheld, NRP was stopped and the surgical team were stood down. If the PF granted authorisation for organ donation to proceed, the SNODs continued discussions with the family to gain consent for organ donation whilst organ preservation continued. If consent was gained for organ donation, family members were given the opportunity to see the donor once they were established on NRP, before they were transferred to theatre for organ retrieval.

Source: Reed MJ, Currie I, Forsythe J, Young I, Stirling J, Logan L, et al. Lessons from a pilot for uncontrolled donation after circulatory death in the ED in the UK. Emerg Med J. 2020;37(3):155–61. https://doi.org/10.1136/emermed-2019-208650, with permission from BMJ publishing group LTD
Edinburgh pilot uDCD protocol. GP, general practitioner; NG, nasogastric; NRP, normothermic regional perfusion; PMH, past medical history; SNOD, specialist nurse in organ donation; TRAK, MedTrak systems electronic medical record.
Box 1 Inclusion criteria for the Edinburgh uncontrolled donation after circulatory death pilot
Age 16–60 years |
Unsuccessful resuscitation from a witnessed out of hospital cardiac arrest (or witnessed |
unsuccessful resuscitation from a cardiac arrest occurring in the ED) |
Scottish Ambulance Service on scene < 15 min |
Self-authorisation for donation, whether because the patient was on the NHS ODR, or was carrying an organ donor card, or had otherwise indicated their wishes |
Logistical Considerations
Uncontrolled DCD donation is a logistically challenging process due to the time constraints that are fundamental in reducing warm ischaemia time and the coordination of the numerous team members required in the organ donation process. For an uDCD programme to be established, an onsite organ retrieval team with experience in NRP must be available at all times and able to attend the ED at short notice. This includes a transplant surgeon, a surgical assistant, a scrub nurse, a perfusionist and an advanced organ perfusion specialist trained in operating the NRP machine. Because the pilot scheme in Edinburgh was not established as part of the National Organ Retrieval Service (NORS), it was not feasible to ensure that a dedicated retrieval team with this skillset would be available 24/7. Therefore, the pilot scheme was restricted to the working week (Monday to Friday between 0900 and 1700). Unfortunately, there were still several clashes due to the primary on-call commitment to NORS, and the team were unable to attend three potential uDCD donors in the ED. The integration of uDCD retrievals into the NORS remit would provide appropriate cover and prevent missed opportunities going forward.
In addition to the retrieval team, it became clear that having two SNODs available for uDCD donations was key to the successful running of the donation process. This allowed one SNOD to focus on communication with the family whilst the other SNOD coordinated the donation process. This required a change in working for the SNOD team to provide this level of cover but enabled a much smoother and efficient process. Funding for embedded SNODs would be highly valuable to the development of a successful uDCD programme.
Coordination of the various team members involved in the rapid response required for uDCD required a robust and failsafe communication system. An important lesson was learned after issues with the pager system resulted in missed opportunities and therefore alternative robust communication systems should be in place with regular test calls.
All cases in the pilot scheme were discussed with the PF after commencement of organ preservation. An expedited referral pathway was agreed with the Crown Office to allow a rapid response (within 10 min) as to whether organ donation could proceed.
An important logistical requirement of the pilot programme was the availability of a room within which to set up and initiate NRP that was separate from the resuscitation area. This helped to completely separate the process of resuscitation and declaration of death from the process of organ donation and recovery, and it was anticipated to make the programme more acceptable to patients and staff.
Potential Donor Numbers
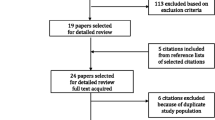
In preparation for the Edinburgh pilot programme, a 1 year potential donor analysis was undertaken between 2008 and 2009 [12]. The analysis used the same inclusion criteria as the pilot (Box 1) and was restricted to patients who attended the ED during weekday working hours so as to correspond with the planned level of cover for the pilot programme. Of the 564 out of hospital arrests during the analysis period, 213 were unwitnessed (Maastricht category Ia) and 351 were witnessed (Maastricht category IIa). Data on in-hospital cardiac arrests was not collected (Maastricht category Ib/IIb). Of the 351 witnessed cardiac arrests, 9 patients ultimately fit the pilot study inclusion criteria (Fig. 2). When accounting for the fact that 41% if the Scottish population at that time were on the ODR, this left an estimate of 4 potential donors per year, but it is important to bear in mind that this represented only one centre in the UK using highly restrictive criteria in the early stages of programme development. The main success of the programme was that it was able to identify potential donors in the ED and strengthened the concept of donation (solid organ and tissues) as part of end-of-life care in the setting of emergency department. It also provided a proof of concept, which was acceptable in the existing UK ethical and legal framework and was feasible from a technical and logistical point of view and that could be used to inform future programmes. A similar uDCD pilot was undertaken in the Netherlands between 2014 and 2016 [13••]. This was a regional programme involving 3 centres; however, no potential donors could be converted to actual donations. The main reasons cited were the strict inclusion criteria, the high refusal rate for organ donation and the policy whereby the ambulance team were able to decide on futility of cardiac arrest and stop resuscitation before arrival at the ED. In contrast, in our pilot programme, the focus was on Maastricht category IIa especially as no resuscitation futility decision was made prior to arrival in ED. A further analysis from the Netherlands concluded that low population density in the areas piloted was another possible reason for the failure of the programme [14•]. In 2019, there were 208 uDCD donors worldwide, with a utilisation rate of 68% (Table 2). Much can be learned from other countries with successful uDCD programmes. In Spain, all out of hospital cardiac arrest patients are transferred to the ED or intensive care unit (ICU) even if resuscitation is deemed futile before arrival at hospital. However, even in Spain which undertakes the highest number of uDCD donations worldwide, it is estimated that there is potential for a further 571 uDCD donors per year which would quadruple the current number of uDCD donations [15•].
Ethical and Legal Issues
The acknowledgement of the increasingly important contribution of DCD to transplantation in the UK has led to the publication of much needed guidance on the key ethical and legal issues surrounding DCD donation.
There was previously a grey area regarding the acceptability of interventions to reduce warm ischaemia following the declaration of death in DCD donation (e.g. reinstating CPR). The UK donation ethics committee guidance provided clarity on this topic in line with the growing consensus from the transplant community that any intervention with the potential of restoring cerebral blood flow should be prohibited [8]. This is in contrast to the guidance in Spain where reinstating CPR is allowable following declaration of death and is considered for the purpose of organ preservation. The development of the Edinburgh pilot programme respected the UK ethical guidelines by ensuring that post-mortem CPR was not reinstated, that an aortic occlusion balloon was placed prior to perfusion of the abdominal organs and that absence of cerebral perfusion was monitored with carotid ultrasound and radial arterial pressure (which used a radial line placed as part of the resuscitation process prior to any considerations of futility or donation). In the UK, no ante-mortem interventions are allowed and therefore there was no ethical issue at stake when undertaking groin cannulation as the patient has already been pronounced dead at the time of the intervention.
A further important ethical consideration in uDCD centres on the institution of in situ organ preservation after death, but before consent from relatives has been obtained. The legal framework in the UK (The Human Tissue Act 2004 and The Human Tissue (Scotland) Act 2006) [16, 17] does specifically allow this; however, the potential to cause distress to the family was taken in consideration and therefore in the Edinburgh pilot programme, consent was gained from relatives whenever possible. In Spain, the presumed consent framework is interpreted in a way that supports post-mortem interventions including organ preservation without the requirement of family consent. The revised UK legislation which centres around presumed consent provides now further grounds for starting organ preservation prior to discussion with relatives.
Given the time-sensitive way in which death is diagnosed in the setting of DCD donation and the rapid shift from resuscitative activities towards organ donation, it is of paramount importance to follow a clear protocol for the determination of irreversible circulatory death. In the Edinburgh pilot programme, guidance from the Academy of Medical Royal Colleges on the diagnosis and confirmation of death was followed. Death was diagnosed by two ED doctors by 5 min of the absence of cardiopulmonary activity as demonstrated by asystole on the continuous ECG, no cardiac movement on focused echocardiography and the absence of respiratory effort [18]. The mandatory 5 min no touch period was also observed.
A clear separation between the team treating the patient and the team retrieving the organs is an overriding principle to avoid any perceived conflict of interest. The decisions around futility and cessation of resuscitation as well as determination of death of the patient should lie solely with the treating team [19].
Future Steps
Although the pilot only resulted in one uDCD donation, many lessons have been learned that can be considered in the development of future programmes.
Results from Spain’s and France’s uDCD programmes clearly illustrate that excellent clinical results can be obtained with the use of NRP as it enables a better organ preservation and assessment and as a result informs the utilisation decisions [20, 21]. Therefore, no modern uDCD programme should be developed without in situ NRP. However, in order to deliver an NRP-based uDCD retrieval service, a substantial amount of training and acquisition of new knowledge is required for the whole team. As more centres adopt NRP for organ retrieval in cDCD donation, there will be significant overlap in the training, skills, equipment and facilities required for uDCD. This will significantly reduce the learning curve and will encourage other centres to explore the development of uDCD programmes. Training courses for NRP are already offered by established NRP centres, however further expansion of the training programmes is required.
In addition to changes in surgical approach, an increased use of advanced resuscitative procedures in the management of out-of-hospital cardiac arrest could further facilitate the development of uDCD programmes. A more aggressive approach to resuscitation effort will increase the use of ECMO which, should these efforts fail, could enable the use of NRP post-mortem and streamline the subsequent donation process.
Establishing a sustainable uDCD programme requires several key logistical considerations. Ideally, all uDCD retrievals should be part of the UK National Organ Retrieval Service (NORS) in order to provide the 24/7 team availability to undertake the surgery for all types of donors (DBD, cDCD and uDCD). However, the current zonal distribution and reliance on ten abdominal and six cardio-thoracic teams to cover the entirety of the country are likely to be a limiting factor in the response time needed for the uDCD programmes. Therefore, the next iteration of development needs to consider the co-location of the large ED departments that care for patients that may proceed to this type of donation with NORS retrieval teams that could provide a rapid response and have the NRP infrastructure and manpower to support such developments.
The development of uDCD programmes is also dependant on embedding specialist nurses in organ donation in the designated ED hospitals, defining distinct roles and distributing the tasks involved in such a programme (e.g. requesting consent and looking after the family or delivering the process).
Perhaps the most important factors are the legal and strategic framework and the public support. Despite a recent move to “opt out” legislation, the current UK donation strategy requires some adjustment to acknowledge the untapped uDCD potential (17,000 patients die yearly following unsuccessful resuscitation of out of hospital cardiac arrests [22]) and to take the relevant steps to incorporate this into the vision for the future. Although there is general public acceptance of uDCD processes and a willingness to discuss organ donation soon after the death of a relative [23], there needs to be a wider conversation about acceptable strategies to optimise the quality of the organs following a decision that further resuscitation is futile. This must consider the recommencement of chest compressions after determination of death to maintain organ perfusion and other societal viewpoints that impact on the effectiveness of organ preservation [24].
Conclusion
A uDCD programme in the UK is feasible and several important lessons have been learned during previous pilots. Despite an increase public awareness and recent changes in legislation, there remain a number of practical, logistical and acceptance issues that need addressing. Although there is a long way to go before a national uDCD programme could be established in the UK, the large untapped donor potential, the increasing need for transplantation coupled with recent advances in perfusion and preservation and an established national retrieval infrastructure, create the premises for future sustainable developments. In preparation for this, there need to be extensive discussions with all stakeholders (patients, transplant and emergency department health care professionals, procurator fiscal (coroner), public, government and national transplant organisations) to openly discuss the need for considering these potential donors, the logistics plans and a definition of responsibilities and roles for the ED and transplant teams, the approach to donation strategy as well as the key indicators for defining success in an open and transparent way.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
NHS Blood and Transplant. Organ donation and transplantation 2030: meeting the need. A ten year vision for organ donation and transplantation in the United Kingdom.
NHS Blood and Transplant. Organ donation and transplantation activity report 2019/20. 2020.
Organización Nacional de Trasplantes and Council of Europe. Newsletter Transplant. International Figures on Donation and Transplantation 2019.
Barlow AD, Metcalfe MS, Johari Y, Elwell R, Veitch PS, Nicholson ML. Case-matched comparison of long-term results of non-heart beating and heart-beating donor renal transplants. Br J Surg. 2009;96(6):685–91. https://doi.org/10.1002/bjs.6607.
Balupuri S, Buckley P, Snowden C, Mustafa M, Sen B, Griffiths P, et al. The trouble with kidneys derived from the non heart-beating donor: a single center 10-year experience. Transplantation. 2000;69(5):842–6. https://doi.org/10.1097/00007890-200003150-00029.
•• Reed MJ, Currie I, Forsythe J, Young I, Stirling J, Logan L, et al. Lessons from a pilot for uncontrolled donation after circulatory death in the ED in the UK. Emerg Med J. 2020;37(3):155–61. https://doi.org/10.1136/emermed-2019-208650. (Most recent UK uDCD pilot discussing the role of NRP, protocols, donor coordinators and stakeholder involvement.)
British Transplantation Society and Intensive Care Society. Donation after circulatory death: report of a consensus meeting. 2010.
UK Donation Ethics Committee. Academy of Medical Royal Colleges. An ethical framework for controlled donation after circulatory death. 2011.
Oniscu GC, Randle LV, Muiesan P, Butler AJ, Currie IS, Perera MT, et al. In situ normothermic regional perfusion for controlled donation after circulatory death–the United Kingdom experience. Am J Transplant. 2014 Dec;14(12):2846–54.
Fondevila C, Hessheimer AJ, Ruiz A, Calatayud D, Ferrer J, Charco R, et al. Liver transplant using donors after unexpected cardiac death: novel preservation protocol and acceptance criteria. Am J Transplant. 2007 Jul;7(7):1849–55.
Resuscitation Council UK. Adult Advanced Life Support Guidelines 2021. Available from: https://www.resus.org.uk/sites/default/files/2021-04/Adult%20Advanced%20Life%20Support%20Algorithm%202021.pdf
Reed MJ, Lua SB. Uncontrolled organ donation after circulatory death: potential donors in the emergency department. Emerg Med J. 2014;31(9):741–4. https://doi.org/10.1136/emermed-2013-202675.
•• Venema LH, Brat A, Nijkamp DM, Krikke C, Leuvenink HGD, de Jongh WC, et al. Factors that complicated the implementation of a program of donation after unexpected circulatory death of lungs and kidneys Lessons Learned from a regional trial in the Netherlands. Transplantation. 2019;103(9):e256–62. https://doi.org/10.1097/tp.0000000000002814. (Study highlighting the challenges in setting up a uDCD programme in the Netherlands.)
• Brat A, Venema LH, Bens BWJ, Stieglis R, van der Heijden JJ, Fondevila C, et al. Potential of donation after unexpected circulatory death programs defined by their demographic characteristics. Transplant Direct. 2022;8(1):e1263. https://doi.org/10.1097/txd.0000000000001263. (Study analysing the potential for uDCD programmes and identifying the role of pre-hospitals protocols for a succesful programme.)
Navalpotro-Pascual JM, Echarri-Sucunza A, Mateos-Rodríguez A, Peinado-Vallejo F, Del Valle PF, Alonso-Moreno D, et al. Uncontrolled donation programs after out-of-hospital cardiac arrest. An estimation of potential donors Resuscitation. 2018;122:87–91. https://doi.org/10.1016/j.resuscitation.2017.11.059.
Human Tissue (Scotland) Act. 2006.
Human Tissue Act 2004. London, UK.
Academy of Medical Royal Colleges. A code of practice for the diagnosis and confirmation of death. 2008.
Haase B, Bos M, Boffa C, Lewis P, Rudge C, Valero R, et al. Ethical, legal, and societal issues and recommendations for controlled and uncontrolled DCD. Transpl Int. 2016;29(7):771–9. https://doi.org/10.1111/tri.12720.
Demiselle J, Augusto JF, Videcoq M, Legeard E, Dubé L, Templier F, et al. Transplantation of kidneys from uncontrolled donation after circulatory determination of death: comparison with brain death donors with or without extended criteria and impact of normothermic regional perfusion. Transpl Int. 2016 Apr;29(4):432–42.
Molina M, Guerrero-Ramos F, Fernández-Ruiz M, González E, Cabrera J, Morales E, et al. Kidney transplant from uncontrolled donation after circulatory death donors maintained by nECMO has long-term outcomes comparable to standard criteria donation after brain death. Am J Transplant. 2019 Feb;19(2):434–47.
Hawkes C, Booth S, Ji C, Brace-McDonnell SJ, Whittington A, Mapstone J, et al. Epidemiology and outcomes from out-of-hospital cardiac arrests in England. Resuscitation. 2017;110:133–40.
Bruce CM, Reed MJ, MacDougall M. Are the public ready for organ donation after out of hospital cardiac arrest? Emerg Med J. 2013;30(3):226–31.
Domínguez-Gil B, Duranteau J, Mateos A, Núñez JR, Cheisson G, Corral E, et al. Uncontrolled donation after circulatory death: European practices and recommendations for the development and optimization of an effective programme. Transpl Int. 2016;29(8):842–59.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Topical Collection on Liver Transplantation
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, D.A., Oniscu, G.C. Piloting Uncontrolled DCD Organ Donation in the UK; Overview, Lessons and Future Steps. Curr Transpl Rep 9, 250–256 (2022). https://doi.org/10.1007/s40472-022-00374-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-022-00374-1