Abstract
Purpose of Review
This review describes the basic epidemiologic, clinical, and microbiologic aspects of cholera, highlights new developments within these areas, and presents strategies for applying currently available tools and knowledge more effectively.
Recent Findings
From 1990 to 2016, the reported global burden of cholera fluctuated between 74,000 and 595,000 cases per year; however, modeling estimates suggest the real burden is between 1.3 and 4.0 million cases and 95,000 deaths yearly. In 2018, the World Health Assembly endorsed a new initiative to reduce cholera deaths by 90% and eliminate local cholera transmission in 20 countries by 2030. New tools, including localized GIS mapping, climate modeling, whole genome sequencing, oral vaccines, rapid diagnostic tests, and new applications of water, sanitation, and hygiene interventions, could support this goal. Challenges include a high proportion of fragile states among cholera-endemic countries, urbanization, climate change, and the need for cholera treatment guidelines for pregnant women and malnourished children.
Summary
Reducing cholera morbidity and mortality depends on real-time surveillance, outbreak detection and response; timely access to appropriate case management and cholera vaccines; and provision of safe water, sanitation, and hygiene.
Similar content being viewed by others
Introduction
Epidemic cholera is caused by fecal-oral transmission of the toxigenic bacterium Vibrio cholerae, serogroup O1 or O139. In individual patients, cholera presents with the sudden onset of profuse watery diarrhea that can lead rapidly to dehydration and death. Its public health presentation is no less dramatic, as it spreads rapidly within vulnerable populations, often causing multiple outbreaks or, in severe cases, a rapid epidemic surge capable of crossing national borders and engulfing whole regions. Although its primary route of transmission has been known for over 150 years, and the means to prevent infection and control outbreaks have become increasingly evident since then, cholera remains a major public health concern in countries in Africa, Asia, and the Americas where coverage with safe drinking water and sanitation is low. Promising new tools for cholera prevention, diagnosis, and treatment, and a new initiative for reducing global cholera deaths by 90% and eliminating local cholera transmission in 20 countries by 2030, may mark a turning point in public health control of this persistent plague.
Epidemiology
History
Although references to a cholera-like illness occur in Greek and Sanskrit writings from before the Common Era, the first of seven great cholera pandemics only began when populations became more mobile in the early nineteenth century [1]. Despite extensive knowledge of cholera biology, pathology, prevention, and treatment gained since that time, the current and ongoing seventh pandemic, which began in 1961, has lasted longer, traveled further, and caused far more cases than any of its predecessors.
Cholera causes an estimated 2.9 million cases and 95,000 deaths each year [2•]. The cholera burden disproportionately affects marginalized, poor populations, including those affected by conflict or natural disasters, who live in areas with unsafe water, sanitation, and hygiene conditions, and limited access to healthcare. As countries have invested in expanding coverage with safe water, sanitation, and hygiene (WASH) infrastructure—in the early twentieth century in Europe and the USA, and in the late twentieth century in Thailand, other parts of Asia, and much of Latin America—local cholera transmission has ceased.
To address remaining gaps in cholera prevention and control, the Global Task Force on Cholera Control (GTFCC) recently released “Ending Cholera: A Global Roadmap to 2030” [3••]. This new initiative outlines a strategy to reduce the number of global cholera deaths by 90% and eliminate cholera transmission in 20 countries by 2030. The strategy relies on an integrated multi-sectoral approach to (1) improve timeliness and effectiveness of cholera responses by building capacity for surveillance, laboratory diagnosis, and treatment, and by prepositioning clinical and WASH resources; (2) ensure longer-term prevention through investments in WASH infrastructure; and (3) prevent and control endemic and epidemic cholera in the short-term through appropriate use of oral cholera vaccines. The strategy also depends on identifying cholera “hotspots”—areas and populations with the highest cholera incidence or mortality—and targeting these for intensive, focused efforts. To support implementation, it recommends a governance structure in which national governments are responsible for coordinating internal mechanisms and technical and financial support from external institutions within a structured monitoring and evaluation framework. Urbanization in developing countries, climate change, and the high number of fragile states with endemic cholera will present challenges for achieving GTFCC goals.
Burden of Disease
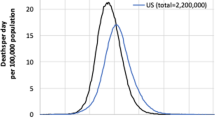
From 1990 to 2016, the global burden of cholera cases and deaths reported annually to WHO has ranged from 74,000 to 595,000 cases, with the greatest variation attributable to epidemic surges associated with the introduction of cholera to Peru in 1991 and to Haiti in 2010–2011 (Figs. 1 and 2a) [4, 5]. In 2017, a surge in epidemic cholera in war-torn Yemen reportedly exceeded 1 million cases [6•]. Reported cholera deaths over the same period have ranged from 1304 to 19,302 per year, with a global case fatality rate (CFR) between 0.8 and 4.4% (Figs. 1 and 2b).
Because many cholera cases and deaths do not present to healthcare facilities, and are therefore not captured by passive surveillance systems, and because political and economic concerns may favor under-reporting,Footnote 1 estimates of cholera burden by public health researchers exceed reported totals several-fold [10, 11]. The most commonly cited estimates, which are based on incidence rates and CFRs from population-based studies, and on estimates of the population without access to sanitation, are that 2.86 million (1.3–4.0 million) cholera cases, including 95,000 (21,000–143,000) cholera deaths, occurred each year from 2008 to 2012 [2•]. Reported cases and deaths during this 5-year period account for only 11.6 and 6.6%, respectively, of the estimated numbers of cases and deaths, which is consistent with WHO estimations that only 5–10% of cholera cases are reported [12, 13]. Other recent estimates of global cholera burden also suggest that reported cholera cases and deaths significantly underestimate the true extent of cholera morbidity and mortality [14, 15].
Sub-Saharan Africa has consistently reported the largest proportion of cholera cases and deaths each year, except during 1991–1993 and 2010–2013 when epidemics in cholera-naïve populations in Latin America and the Caribbean were predominant (Fig. 2a, b). The cholera case-fatality ratio has also been consistently higher in sub-Saharan Africa than in other regions. Although it has gradually decreased, in 2016, it was 2.5%, compared with 1.1% in the Americas and 1.0% in Asia [16]. In recent years, large outbreaks of cholera in Afghanistan, Iraq, and, in 2016–2017, Yemen suggest that cholera has established a firm foothold in the Middle East [6•, 17, 18].
Risk Factors for Cholera Infection, Severity, and Death
Although sporadic cholera cases may arise from consumption of raw or inadequately cooked seafood contaminated by free-living toxigenic Vibrio cholerae O1, cholera epidemics are spread primarily through fecal contamination of drinking water, and occasionally food, by infected persons [19]. A recent review and meta-analysis of the role of water, sanitation, and hygiene exposures in 51 case-control studies of cholera found that cases were significantly more likely than controls to report use of an unimproved water source, contact with surface water, unsafe water transport and storage, untreated drinking water, open defecation, unimproved sanitation, shared sanitation, and poor hand hygiene [20]. Several recent studies found that household contacts of cholera patients had high risk of infection, which could occur through contaminated fomites, food, or drinking water [21,22,23]. Another study found that proximity to a case’s home increased risk of cholera in neighbors [24].
Infection with certain strains of Vibrio cholerae, including the recently described El Tor variant, that produces more cholera toxin of a more potent form, increases the likelihood of severe disease, as does a larger inoculum of Vibrio cholerae ingested [25, 26]. Host factors, such as achlorhydria or blood group O also increase the risk of severe illness [27].
Risk factors for cholera mortality have been studied in outbreaks in rural and urban settings, but can be challenging to investigate due to underreporting and limitations in surveillance [2•, 10, 11]. People at the extremes of age, and those with certain co-morbidities, are more susceptible to the effects of dehydration [28]. However, limited access to healthcare, poor health-seeking behavior, and inadequate rehydration are the salient preventable risk factors for cholera deaths [29,30,31,32]. Despite challenges, simple strategies such as improving access to oral rehydration have been proven to lower mortality rates from dehydrating diarrheal diseases [33].
Cholera Hotspots
Besides the presence of toxigenic V. cholerae O1 or O139, the primary determinant of cholera outbreaks and endemicity is a failure to protect drinking water, food, and the environment from fecal contamination. Many other factors influence cholera risk, including environmental and meteorological conditions, population density, mobility, and immunity, and social customs, such as those associated with burials [34]. A core component of The Global Roadmap to 2030 is the identification of cholera hotspots for intensive prevention and preparedness efforts. A 2017 paper suggests three key types of hotspots: “burden hotspots,” where disease prevalence or incidence is high; “risk hotspots,” where transmission efficacy or risk of disease acquisition and amplification is high; and “emergence hotspots,” where there is increased likelihood of disease emergence [35].
Identifying these hotspots is critical to cost-effective cholera prevention and control. Initial efforts have relied on historical cholera data, enhanced by more granular mapping of GIS data on cholera cases, population density, and drinking water and sanitation services [36•]. Improvements in climate and environmental models that predict conditions where V. cholerae might thrive [37•], the use of migration and cell phone data to predict areas with high transmission risk [38•, 39], and more accurate estimates of cases and fatalities through improved surveillance [40] have helped enable more accurate and timely hotspot identification.
Predicting Disease Emergence: Climate Modeling
The association between cholera outbreaks and environmental drivers has been recognized for decades [41]. V. cholerae are free-living organisms commonly found in brackish waters in close conjunction with zooplankton, shellfish, and other flora and fauna [42,43,44]. Conditions of temperature and salinity that promote growth of these organisms may also promote growth of V. cholerae. These conditions, and algal blooms and other proxy indicators, are measurable by satellite imagery and may help predict cholera outbreak risk in vulnerable nearby populations [45, 46]. The El Niño Southern Oscillation (ENSO), a periodic warming of a section of the Pacific Ocean, was associated with cholera outbreaks in Bangladesh and Peru [47], though its effects are modified by local climate and other variables, complicating accurate outbreak prediction [48, 49]. ENSO also affects inland temperature and rainfall [6•, 45, 50,51,52,53]. A study of cholera incidence in Africa over a 15-year period found decreases in Madagascar and parts of Western, Central, and Southern Africa, and increases in Eastern Africa during El Niño years [37].
Several papers have noted a relationship between cholera incidence and rainfall [6•, 45, 50,51,52, 54]. Proposed pathways include fecal contamination of drinking water sources due to excessive precipitation and flooding; increased use of unsafe water sources due to reduced rainfall and drought; and the effects on other factors related to Vibrio survival and growth in water sources, including zooplankton, bacteriophage, and iron content [55,56,57].
Identifying Transmission Risks: Population Migration
Population mobility can facilitate the spread of cholera, and tracking population movements can help predict areas of increased transmission risk. Bengtsson et al. used mobile phone data in Haiti to retrospectively track the movements of 2.9 million people during the cholera outbreak in 2010. They combined this with surveillance data to create a model that could predict new areas of transmission based on population movements from high incidence areas [39]. Mobile phone and rainfall data were used by Finger et al. to retrospectively model a 2005 cholera outbreak in Sierra Leone. They found that a religious pilgrimage had significant impact on the spread of cholera, likely due to a sudden increase in population that strained water and sanitation services. Following the event, infected individuals disseminated cholera across the country when they returned to their homes [38•].
Identifying Areas of High Incidence and Prevalence: Urbanization
On a larger and longer scale, decades of population migration from rural to urban areas across the developing world has outstripped the capacity of municipal water and sanitation infrastructure in many cities, and led to densely populated, underserved informal settlements, where cholera and other infectious diseases find fertile ground [58,59,60]. In recent years, cholera outbreaks have occurred in the capital cities of Benin, Ghana, Guinea, Guinea Bissau, Haiti, Ivory Coast, Kenya, Sierra Leone, Tanzania, Togo, Uganda, Zambia, and Zimbabwe, while cholera is considered endemic in Dhaka, Bangladesh, and Kolkata, India.
According to data from the Joint Monitoring Programme (JMP), improved sanitation coverage decreased from 2010 to 2015 among urban populations in 36 (67%) of 54 African countries, a net increase of 24 million city-dwellers without access [59, 61]. Crowded urban environments with poor sanitation conditions in Europe and the USA were frequent foci of cholera epidemics in the nineteenth century; similar unsanitary conditions prevail in parts of many cities today [27•, 62,63,64].
Identifying Areas of High Incidence and Prevalence: GIS Methods
A recent paper used spatial analysis and case count data in India to identify areas with high cholera burden and to examine associations with socioeconomic characteristics. The study found that 25% of districts in India, representing 31% of the population, reported cholera and 90 (14%) of these were “hotspots,” defined as areas where clustering of cases was unlikely due to chance. Districts with higher rates of literacy, mobile phone ownership, and households using tap water from a treated source had lower risk of reporting cholera, and districts with higher proportions of households using latrines without a slab or using open drainage for sanitation had higher risk [65].
Identifying Areas of High Incidence and Prevalence: Conflict Areas and Fragile States
The Global Roadmap to 2030 calls for countries and donors to support cholera control efforts, and specifies that countries should coordinate efforts within their own boundaries. Cholera may persist in states with weak governments that under-prioritize healthcare, and in conflict areas where interventions are difficult to implement.
Conflict can damage water and sanitation infrastructure directly, as in Yemen [66], and it weakens economies and health systems, which can limit people from accessing healthcare, safe drinking water, or proper sanitation and hygiene facilities [67, 68]. Conflict can also limit the potential for outside support from NGOs, UN agencies, or bilateral donors. The World Bank’s list of fragile situations includes countries and territories with ongoing conflict or risk of conflict, and those with low performance on indicators of governance [69]. Among people living in fragile states, the proportion without access to safe drinking water is twice, and the proportion who lack basic sanitation is fourfold, that among people living in non-fragile states [70].
Of the 34 countries on the World Bank list of fragile situations for FY 2018, 22 have endemic cholera and 3 more share a border with countries identified by GTFCC as cholera-endemic (Fig. 3) [69, 71]. Fragile states that border states with endemic cholera are at higher than average risk for cholera, and need prevention, detection, and response protocols. Most countries with endemic cholera share a border with at least one other country with endemic cholera, making cross-border coordination essential.
Diagnosis
Isolation and identification of Vibrio cholerae serogroup O1 or O139 by stool culture is the gold standard for confirming a cholera outbreak. Ideally, a stool sample or rectal swab is preserved in Cary-Blair media and transported at room temperature to the nearest diagnostic lab within several days; fresh stool transported without media must arrive at the lab within 2 h [72•, 73, 74].
Identification of the serogroup (O1 or O139), serotype (Inaba or Ogawa), and biotype (El Tor or classical) can be useful for epidemiologic purposes, while antimicrobial susceptibility testing is essential for validating treatment recommendations [72•, 73]. Toxigenic V. cholerae O1 can also be identified in stool by PCR testing, but further subtyping and antimicrobial susceptibility testing require culture.
Antimicrobial-resistant strains of V. cholerae O1 caused major outbreaks in the 1970s [75]. Since then, resistance to over a dozen antimicrobials, including fluoroquinolones, tetracycline/doxycycline, and multidrug resistance, has often been reported [76,77,78,79,80,81,82]. Whole genome sequencing can identify epidemiologically relevant patterns, antimicrobial resistance genes, and virulence factors; however, resources for this are not usually available during outbreak responses [83, 84].
A variety of rapid diagnostic tests (RDTs) are available or under development for point-of-care diagnosis. Most are lateral-flow immune-chromatographic antigen detection tests that use monoclonal antibodies to surface lipopolysaccharide antigens of V. cholerae O1; some also include antibodies to O139 antigens [85, 86]. Because of the varying sensitivity and specificity of available tests, and the lack of standardization and external quality control, WHO recommends they be used for confirming diagnoses, prioritizing samples to be sent for lab confirmation, rapid pre-confirmation screening of suspected new outbreaks, and monitoring outbreak dynamics [85,86,87,88,89,90,91]. Despite clear WHO guidelines, RDTs are often misused for individual diagnosis, which is unnecessary and may lead to inappropriate treatment decisions.
V. cholerae O1 can be identified in water and food samples by culture or PCR. Membrane filtration or ultrafiltration may be used to process water samples; other methods are available for processing food samples [92]. During outbreak responses, these efforts require lab capacity that may be needed for more critical tasks, such as testing clinical samples and monitoring antimicrobial susceptibility [93]. In some situations, data on Vibrio contamination of water or food may strengthen public communication messages about cholera prevention and motivate policy makers to dedicate more resources to the response. However, negative results from environmental samples, even by PCR, do not necessarily mean a total absence of V. cholerae from the water or food source. Escherichia coli is a simpler, more practical, and less expensive proxy indicator of fecal contamination, and therefore of cholera risk.
Treatment
Clinical Presentation and Case Management
The hallmark symptom of cholera is the sudden onset of painless watery diarrhea, often profuse, described as “rice-water” stools. The diarrhea may be accompanied by vomiting and muscle cramps, but is neither bloody nor accompanied by fever. When V. cholerae bacteria are ingested, they attach to intestinal cells and produce a toxin that disrupts normal absorption and secretion of fluid and electrolytes [94]. Cholera infection manifests in a wide range of presentations from asymptomatic, to mild or moderate symptoms that mimic common enteric diseases, to massive outpouring of watery diarrhea that can lead to hypotensive shock and circulatory collapse within hours [95, 96]. Disease severity depends on the virulence of the agent, the dose ingested, and host factors including age, gastric acidity, blood type, and acquired immunity [97,98,99]. In endemic settings, asymptomatic cases may represent nearly half of all cholera cases [99]. Timely rehydration with the proper mix of fluids and electrolytes is the cornerstone of cholera treatment, and can reduce mortality rates from > 50% to less than 1% [100].
Case management begins at home, with administration of oral rehydration solution (ORS) and continued feeding before and while seeking medical care. If a patient can drink sufficient fluids, the preferred treatment is oral rehydration with ORS, prepared by mixing a prepackaged sachet of glucose and electrolytes with 1 l of safe drinking water. Treatment of severe dehydration, and of patents who cannot drink sufficient volumes of ORS, requires intravenous rehydration. Ringer’s lactate is preferred since its electrolyte composition is comparable to that of cholera stools. Cholera patients require replacement for baseline fluid losses and for ongoing losses from vomiting and diarrhea.
Antimicrobial Treatment
Antibiotics are not recommended for mild or moderately ill patients, but when used in conjunction with rehydration treatment of severely ill patients, they can reduce the volume of stool, duration of diarrhea, and duration of V. cholerae carriage [100,101,102,103,104]. By reducing rehydration needs and the duration of hospitalization, this may help conserve resources in busy cholera treatment centers [100]. Because V. cholerae O1 and O139 have demonstrated resistance to several antibiotics, antimicrobial susceptibility testing is essential for informing treatment guidelines [77, 79, 105,106,107].
Zinc
Zinc supplementation significantly reduces the duration and severity of cholera in children < 15 years old [108]. Zinc is administered once a day for 10 to 14 days; dosage is age-dependent [108].
Special Populations
Children
Children with cholera are at higher risk of hypoglycemia than adults [109]. This can lead to lethargy, coma, seizures, and even death. Cholera-affected children also lose more potassium in stool than adults making them more susceptible to hypokalemia [110, 111]. Therefore, ORS, which contains more glucose and a higher concentration of potassium than Ringer’s lactate, is particularly important for rehydration of children. Additionally, to restore stable glucose levels, children should be fed/breastfed as soon as they are able to tolerate oral intake.
Children with Severe Acute Malnutrition
Children suffering from severe acute malnutrition (SAM) are a fragile patient population with a ninefold increased risk of mortality compared with well-nourished children [112]. Several factors, including propensity for hypothermia, hypoglycemia, and a decreased immune response, render these patients extremely vulnerable to infection and death [113]. Moreover, SAM patients require specialized treatment, feedings, and close monitoring when ill. Cholera is difficult to detect and manage in children with SAM because the signs used to determine the level of dehydration are not reliable in these patients. The delicate balance of fluid and electrolytes makes clinical management extremely difficult, especially in low-resource settings. At present, consensus on cholera treatment and evidence on best practices in this vulnerable population are lacking [114].
Pregnancy
Cholera during pregnancy has been associated with higher rates of fetal death, particularly among mothers who are vomiting, severely dehydrated, and in their third trimester [115]. Assessing the level of dehydration in pregnancy can be challenging due to increased plasma volume [116]. Poor fetal outcomes are a result of physiologic changes in the cholera-infected mother [117]. Fetal death may result from electrolyte changes in amniotic fluid following severe vomiting and/or resultant fetal acidosis and hypoxia following severe maternal dehydration and shock [115].
Prevention and Control
Water, Sanitation, and Hygiene Interventions
From the mid-1800s through the early twentieth century, cholera helped drive the “sanitary revolution” that led to its elimination from Europe and North America [118]. Key interventions included improved access to safe drinking water, safe collection and disposal of fecal waste, and hygiene promotion. More recently, water, sanitation, and hygiene (WASH) investments a century later helped eliminate cholera from Central and South America. In each case, cholera elimination was accompanied by dramatic reductions in infant and child mortality, and in the incidence of other enteric diseases [119, 120]. In other countries, such as Thailand and South Africa, cholera has also lost force as population coverage with water and sanitation increased. Between 1991 and 2010, countries in which less than 71% of the population had access to improved water sources, or less than 39% had access to improved sanitation, were more likely to have endemic cholera than countries with higher coverage rates [121].
In addition to the longer-term benefit of cholera elimination, WASH interventions have short-term, but dramatic benefits in response to cholera outbreaks as shown in recent reviews and a meta-analysis (Table 1) [20, 122].
A recent and novel intervention in Tanzania during a cholera outbreak in 2015 attempted to bypass challenges with household-level chlorination by chlorinating water in large tanks operated by private vendors [123]. A similar approach, using emergency public water storage tanks, was recently successfully used in Zambia [124].
The CHOBI-7 randomized controlled-trial in Bangladesh evaluated handwashing and water treatment promotion in the homes of index cholera patients for 1 week after their release from a cholera treatment center. Households that received the intervention had 41% fewer secondary cholera infections than households that did not [125,126,127].
Disinfecting households of cholera patients by spraying them with a chlorine solution is a popular intervention, without evidence of impact. In 2011, UNICEF, CDC, and MSF recommended against spraying chlorine in homes and vehicles and suggested resources should instead be focused on providing water chlorination and improving hygiene [128].
Vaccines
Oral cholera vaccines (OCVs) can be a useful complementary tool for cholera prevention and control when used in conjunction with mainstay measures such as surveillance, appropriate medical treatment, WASH interventions, and community mobilization [129]. OCV campaigns can be considered in endemic settings, pre-emptive or reactive epidemic settings, or during humanitarian emergencies, but must not disrupt other critical cholera control measures [130•, 131]. Currently, three oral cholera vaccines are WHO pre-qualified: Dukoral® (SBL Vaccines), Shanchol® (Shanta Biotec), and Euvichol-Plus®/Euvichol (Eubiologics). All three are killed whole cell vaccines that contain a mix of different Vibrio cholerae biotypes and serotypes. Dukoral is monovalent and contains only V. cholerae serogroup O1 with the recombinant B subunit of cholera toxin. It requires a buffer and is licensed for children ≥ 2 years old. Shanchol and Euvichol are bivalent and contain both O1 and O139 V. cholerae without the toxin subunit, do not require a buffer, and are licensed for children ≥ 1 year old [132,133,134]. All three vaccines are licensed as a two-dose regimen with doses given 14 days apart for Shanchol and Euvichol, and between 1 and 6 weeks apart for Dukoral. OCVs have been found safe in pregnant women. Shanchol has demonstrated protection for 5 years among adults and children 5–15 years old, but not in children ≤ 5 years old [135, 136]. Recent studies have shown that single-dose regimens can be useful in special circumstances and provide short-term effectiveness [137,138,139,140]. In 2013, a global OCV stockpile was established to ensure rapid access to cholera vaccine in endemic and emergency settings. As of April 2017, over 7 million doses of OCV had been deployed for more than 40 mass vaccination campaigns in 14 countries [130•, 131].
Chemoprophylaxis
Antimicrobial chemoprophylaxis or mass treatment may be useful in helping contain and control outbreaks in institutional settings, including prisons and mental hospitals [141,142,143]. In these settings, which are at high-risk for cholera introduction and dissemination, antimicrobial agents can quickly be delivered to the entire population, minimizing the risk of antimicrobial resistance. Institutional WASH assessments and interventions should accompany or precede antibiotic chemoprophylaxis. In some instances, community OCV campaigns have included prison populations with little extra cost or effort [144]. Antibiotic chemoprophylaxis is not recommended for the general population, because its effectiveness is uncertain, it is time- and resource-intensive, and it has been associated with the emergence of antibiotic resistance [145,146,147].
Conclusions
Reducing cholera morbidity and mortality depends on effective, real-time surveillance, detection and response; timely access to appropriate case management; and the provision of safe water, sanitation, and hygiene. More recently, newer oral cholera vaccines (OCVs) that are between 60 and 85% effective for up to 5 years have been used in combination with WASH for cholera prevention and control in high-incidence and high-transmission areas [139, 148, 149]. During the 2018 World Health Assembly, recognizing the unique opportunity for progress toward cholera control offered by new tools and by the Ending Cholera strategy, UN member nations approved a resolution to prioritize cholera and support integrated efforts for its control. If their efforts succeed, the global burden of cholera will be considerably less by 2030.
Notes
Bangladesh and Ethiopia, countries where outbreaks of cholera (sometimes referred to as outbreaks of “acute watery diarrhea”) are known to have occurred, do not typically report cases to WHO, despite publications and reports that attest to patients with culture-confirmed cholera at the time [7,8,9].
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lacey SW. Cholera: Calamitous past, ominous future. Clin Infect Dis. 1995;20(5):1409–19.
• Ali M, Nelson AR, Lopez AL, Sack DA. Updated global burden of cholera in endemic countries. PLoS Negl Trop Dis. 2015;9(6):e0003832. Updated estimates of the number of cholera cases and deaths actually occurring in endemic countries, which are much larger than the numbers reported through global surveillance.
•• WHO. Ending Cholera A Global Roadmap to 2030. WHO [Internet]. WHO; 2018 [cited 2018 May 23]. Available from: http://www.who.int/cholera/publications/global-roadmap/en. Initiative launched by the Global Task Force on Cholera Control in 2017 and approved by the World Health Assembly in 2018, outlines a strategy to reduce the number of global cholera deaths by 90% and eliminate cholera transmission in 20 countries by 2030.
Barzilay EJ, Schaad N, Magloire R, Mung KS, Boncy J, Dahourou GA, et al. Cholera surveillance during the Haiti epidemic—the first 2 years. N Engl J Med. 2013;368(7):599–609.
WHO. Glob Health Observatory data repository: cholera [Internet]. 2017. Available from: http://apps.who.int/gho/data/node.main.174?lang=en
• Camacho A, Bouhenia M, Alyusfi R, Alkohlani A, Naji MAM, de Radiguès X, et al. Cholera epidemic in Yemen, 2016–18: an analysis of surveillance data. Lancet Glob Health. 2018;6(6):e680–90. Describes a cholera outbreak in war-torn Yemen in which over 1 million cases were reported during a 2-year period.
Bartels SA, Greenough PG, Tamar M, VanRooyen MJ. Investigation of a cholera outbreak in Ethiopia’s Oromiya region. Disaster Med Public Health Prep. 2010;4(4):312–7.
WHO. AFRO Outbreaks and Emergencies Bulletin 30 May, 2016 [Internet]. 2016. Available from: https://reliefweb.int/sites/reliefweb.int/files/resources/whoafro-outbreaks-and-emergencies_bulletin_issue-3_-30-may-2016.pdf.
Paul RC, Faruque ASG, Alam M, Iqbal A, Zaman K, Islam N, et al. Incidence of severe diarrhoea due to Vibrio cholerae in the catchment area of six surveillance hospitals in Bangladesh. Epidemiol Infect. 2016;144(5):927–39.
Shikanga O-T, Mutonga D, Abade M, Amwayi S, Ope M, Limo H, et al. High mortality in a cholera outbreak in western Kenya after post-election violence in 2008. Am J Trop Med Hyg. 2009;81(6):1085–90.
McCrickard LS, Massay AE, Narra R, Mghamba J, Mohamed AA, Kishimba RS, et al. Cholera mortality during urban epidemic, Dar es Salaam, Tanzania, August 16, 2015–January 16, 20161. Emerg Infect Dis [Internet]. 2017 Dec [cited 2018 May 31];23(13). Available from: http://wwwnc.cdc.gov/eid/article/23/13/17-0529_article.htm.
WHO. WHO | World Health Statistics 2014 [Internet]. WHO. 2015 [cited 2018 May 24]. Available from: http://www.who.int/gho/publications/world_health_statistics/2014/en/.
Ali M, Lopez AL, Ae You Y, Eun Kim Y, Sah B, Maskery B, et al. The global burden of cholera. Bull World Health Organ. 2012;90(3):209–18.
GBD. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Lond Engl. 2016;388(10053):1459–544.
GBD. Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Lond Engl. 2017;390(10100):1084–150.
WHO. Cholera, 2016. Wkly Epidemiol Rec. 2017;92(36):521–36.
WHO. Meeting of the strategic advisory Group of Experts on immunization, April 2017—conclusions and recommendations. Wkly Epidemiol Rec. 2017;92(22):301–20.
WHO. Cholera, 2015. Wkly Epidemiol Rec. 2016;91(38):432–40.
Estrada-García T, Mintz ED. Cholera: foodborne transmission and its prevention. Eur J Epidemiol. 1996;12(5):461–9.
Wolfe M, Kaur M, Yates T, Woodlin M, Lantagne D. A systematic review and meta-analysis of the association between water, sanitation, and hygiene exposures and cholera in case-control studies Am J Trop Med Hyg. 2018;in press.
Sugimoto JD, Koepke AA, Kenah EE, Halloran ME, Chowdhury F, Khan AI, et al. Household transmission of Vibrio cholerae in Bangladesh. PLoS Negl Trop Dis. 2014;8(11):e3314.
Burrowes V, Perin J, Monira S, Sack DA, Rashid M-U, Mahamud T, et al. Risk factors for household transmission of Vibrio cholerae in Dhaka, Bangladesh (CHoBI7 trial). Am J Trop Med Hyg. 2017;96(6):1382–7.
Weil AA, Khan AI, Chowdhury F, Larocque RC, Faruque ASG, Ryan ET, et al. Clinical outcomes in household contacts of patients with cholera in Bangladesh. Clin Infect Dis Off Publ Infect Dis Soc Am. 2009;49(10):1473–9.
Debes AK, Ali M, Azman AS, Yunus M, Sack DA. Cholera cases cluster in time and space in Matlab, Bangladesh: implications for targeted preventive interventions. Int J Epidemiol. 2016;45(6):2134–9.
Jackson BR, Talkington DF, Pruckler JM, Fouche MDB, Lafosse E, Nygren B, et al. Seroepidemiologic survey of epidemic cholera in Haiti to assess spectrum of illness and risk factors for severe disease. Am J Trop Med Hyg. 2013;89(4):654–64.
Watson AP, Armstrong AQ, White GH, Thran BH. Health-based ingestion exposure guidelines for Vibrio cholerae: technical basis for water reuse applications. Sci Total Environ. 2018;613–614:379–87.
Clemens JD, Nair GB, Ahmed T, Qadri F, Holmgren J. Cholera. Lancet. 2017;390(10101):1539–49.
Gunnlaugsson G, Angulo FJ, Einarsdottir J, Passa A, Tauxe RV. Epidemic cholera in Guinea-Bissau: the challenge of preventing deaths in rural West Africa. Int J Infect Dis. 2000;4(1):8–13.
Tauxe RV, Holmberg SD, Dodin A, Wells JV, Blake PA. Epidemic cholera in Mali: high mortality and multiple routes of transmission in a famine area. Epidemiol Infect. 1988;100(2):279–89.
Quick RE, Vargas R, Moreno D, Mujica O, Beingolea L, Palacios AM, et al. Epidemic cholera in the Amazon: the challenge of preventing death. Am J Trop Med Hyg. 1993;48(5):597–602.
Routh JA, Loharikar A, Fouche M-DB, Cartwright EJ, Roy SL, Ailes E, et al. Rapid assessment of cholera-related deaths, Artibonite department, Haiti, 2010. Emerg Infect Dis. 2011;17(11):2139–42.
Morof D, Cookson ST, Laver S, Chirundu D, Desai S, Mathenge P, et al. Community mortality from cholera: urban and rural districts in Zimbabwe. Am J Trop Med Hyg. 2013;88(4):645–50.
Gutiérrez G, Tapia-Conyer R, Guiscafré H, Reyes H, Martinez H, Kumate J. Impact of oral rehydration and selected public health interventions on reduction of mortality from childhood diarrhoeal diseases in Mexico. Bull World Health Organ. 1996;74(2):189.
McAteer JB, Danda S, Nhende T, Manamike P, Parayiwa T, Tarupihwa A, et al. Notes from the field: outbreak of Vibrio cholerae associated with attending a funeral - Chegutu District, Zimbabwe, 2018. MMWR Morb Mortal Wkly Rep. 2018;67(19):560–1.
McKay HS, Lessler J, Moore SM, Azman AS. What is a hotspot anyway? Am J Trop Med Hyg. 2017;96(6):1270–3.
• Lessler J, Moore SM, Luquero FJ, McKay HS, Grais R, Henkens M, et al. Mapping the burden of cholera in sub-Saharan Africa and implications for control: an analysis of data across geographical scales. Lancet Lond Engl. 2018;391(10133):1908–15. Introduction to the different kinds of hotspots with implications for how these may relate to implementation of the Ending Cholera initiative.
• Moore SM, Azman AS, Zaitchik BF, Mintz ED, Brunkard J, Legros D, et al. El Niño and the shifting geography of cholera in Africa. Proc Natl Acad Sci. 2017;114(17):4436–41. Analytic study of the effects of a particular meteorological phenomenon on cholera incidence in sub-Saharan Africa.
• Finger F, Genolet T, Mari L, de Magny GC, Manga NM, Rinaldo A, et al. Mobile phone data highlights the role of mass gatherings in the spreading of cholera outbreaks. Proc Natl Acad Sci. 2016;113(23):6421–6. Example of the use of mobile phone data to gain insights on cholera epidemiology and patterns of disease spread.
Bengtsson L, Gaudart J, Lu X, Moore S, Wetter E, Sallah K, et al. Using mobile phone data to predict the spatial spread of cholera. Sci Rep [Internet]. 2015 Aug [cited 2018 May 7];5(1). Available from: http://www.nature.com/articles/srep08923
Mintz ED, Tauxe RV. Cholera in Africa: a closer look and a time for action. J Infect Dis. 2013;208(Suppl 1):S4–7.
Colwell RR. Global climate and infectious disease: the cholera paradigm. Science. 1996;274(5295):2025–31.
Huq A, West PA, Small EB, Huq MI, Colwell RR. Influence of water temperature, salinity, and pH on survival and growth of toxigenic Vibrio cholerae serovar O1 associated with live copepods in laboratory microcosms. Appl Environ Microbiol. 1984;48(2):420–4.
Kaneko T, Colwell RR. Ecology of Vibrio parahaemolyticus in Chesapeake Bay. J Bacteriol. 1973;113(1):24–32.
Oliver JD, Warner RA, Cleland DR. Distribution of Vibrio vulnificus and other lactose-fermenting vibrios in the marine environment. Appl Environ Microbiol. 1983;45(3):985–98.
Jutla A, Aldaach H, Billian H, Akanda A, Huq A, Colwell R. Satellite based assessment of hydroclimatic conditions related to cholera in Zimbabwe. Schumann GJ-P, editor. PLoS One. 2015;10(9):e0137828.
Chretien J-P, Anyamba A, Small J, Britch S, Sanchez JL, Halbach AC, et al. Global climate anomalies and potential infectious disease risks: 2014-2015. PLoS Curr 2015;26(7).
Cash BA, Rodó X, Emch M, Yunus M, Faruque ASG, Pascual M. Cholera and shigellosis: different epidemiology but similar responses to climate variability. PLoS One. 2014;9(9):e107223.
Martinez PP, Reiner RC, Cash BA, Rodó X, Shahjahan Mondal M, Roy M, et al. Cholera forecast for Dhaka, Bangladesh, with the 2015-2016 El Niño: lessons learned. PLoS One. 2017;12(3):e0172355.
Ramírez IJ, Grady SC, Niño E. Climate, and cholera associations in Piura, Peru, 1991–2001: a wavelet analysis. EcoHealth. 2016;13(1):83–99.
Munyuli MT, Kavuvu JM, Mulinganya G, Bwinja GM. The potential financial costs of climate change on health of urban and rural citizens: a case study of Vibrio cholerae infections at Bukavu town, south Kivu Province, eastern Democratic Republic of Congo. Iran J Public Health. 2013;42(7):707.
Leckebusch GC, Abdussalam AF. Climate and socioeconomic influences on interannual variability of cholera in Nigeria. Health Place. 2015;34:107–17.
Stoltzfus JD, Carter JY, Akpinar-Elci M, Matu M, Kimotho V, Giganti MJ, et al. Interaction between climatic, environmental, and demographic factors on cholera outbreaks in Kenya. Infect Dis Poverty. 2014;3(1):37.
Rebaudet S, Sudre B, Faucher B, Piarroux R. Environmental determinants of cholera outbreaks in inland Africa: a systematic review of main transmission foci and propagation routes. J Infect Dis. 2013;208(suppl_1):S46–54.
Constantin de Magny G, Thiaw W, Kumar V, Manga NM, Diop BM, Gueye L, et al. Cholera outbreak in Senegal in 2005: was climate a factor? PLoS One. 2012;7(8):e44577.
Ruiz-Moreno D, Pascual M, Bouma M, Dobson A, Cash B. Cholera seasonality in madras (1901–1940): dual role for rainfall in endemic and epidemic regions. EcoHealth. 2007;4:52–62.
Hashizume M, Faruque ASG, Wagatsuma Y, Hayashi T, Armstrong B. Cholera in Bangladesh: climatic components of seasonal variation. Epidemiology. 2010;21(5):706–10.
Rieckmann A, Tamason CC, Gurley ES, Rod NH, Jensen PKM. Exploring droughts and floods and their association with cholera outbreaks in sub-Saharan Africa: a register-based ecological study from 1990 to 2010. Am J Trop Med Hyg. 2018;98(5):1269–74.
Ezeh A, Oyebode O, Satterthwaite D, Chen Y-F, Ndugwa R, Sartori J, et al. The history, geography, and sociology of slums and the health problems of people who live in slums. Lancet. 2017;389(10068):547–58.
UNPOP. World Urbanization Prospects - Population Division - United Nations [Internet]. 2017 [cited 2018 May 24]. Available from: https://esa.un.org/unpd/wup/
Moore S, Dongdem AZ, Opare D, Cottavoz P, Fookes M, Sadji AY, et al. Dynamics of cholera epidemics from Benin to Mauritania. Fuehrer H-P, editor. PLoS Negl Trop Dis 2018;12(4):e0006379.
JMP. JMP [Internet]. 2018 [cited 2018 May 24]. Available from: https://washdata.org/data.
Sack DA, Sack RB, Nair GB, Siddique AK. Cholera. Lancet. 2004;363(9404):223–33.
Snow J. Mode of communication of cholera. Wilson and Oglivy, London; 1855.
Johnson S. The ghost map: the story of London’s most terrifying epidemic—and how it changed science, cities, and the modern world. Riverhead Books, New York; 2007.
Ali M, Gupta SS, Arora N, Khasnobis P, Venkatesh S, Sur D, et al. Identification of burden hotspots and risk factors for cholera in India: an observational study. PLoS One. 2017;12(8):e0183100.
Almosawa S, Hubbard B, Griggs T. It’s a slow death: the World’s worst humanitarian crisis The New York Times [Internet]. 2017 Aug 23 [cited 2018 May 24]; Available from: https://www.nytimes.com/interactive/2017/08/23/world/middleeast/yemen-cholera-humanitarian-crisis.html, https://www.nytimes.com/interactive/2017/08/23/world/middleeast/yemen-cholera-humanitarian-crisis.html.
Bruckner C, Checchi F. Detection of infectious disease outbreaks in twenty-two fragile states, 2000-2010: a systematic review. Confl Health. 2011;5(1):13.
Beyrer C, Villar JC, Suwanvanichkij V, Singh S, Baral SD, Mills EJ. Neglected diseases, civil conflicts, and the right to health. Lancet. 2007;370(9587):619–27.
World Bank. Harmonized List of Fragile Situations [Internet]. World Bank. 2018 [cited 2018 May 24]. Available from: http://www.worldbank.org/en/topic/fragilityconflictviolence/brief/harmonized-list-of-fragile-situations.
JMP. Progress on drinking water, sanitation and hygiene [Internet]. UNICEF, WHO Joint Monitoring Project; 2017. Available from: http://www.who.int/mediacentre/news/releases/2017/launch-version-report-jmp-water-sanitation-hygiene.pdf.
GTFCC. Personal email communication. WHO/GTFCC; 2018.
• CDC. Laboratory Testing for Cholera | Cholera | CDC [Internet]. 2018 [cited 2018 May 24]. Available from: https://www.cdc.gov/cholera/laboratory.html. Guidance on isolation and identification of Vibrio cholerae O1 in specimens from suspected cases.
WHO. Bacterial agents of enteric diseases of public health concern: Salmonella serotype Typhi, Shigella, Vibrio cholerae [Internet]. 2003. Available from: http://www.who.int/csr/resources/publications/drugresist/IIIAMRManual.pdf?ua=1.
CDC. Job aid: how to collect a fecal specimen and transfer to transport medium [Internet]. 2018. Available from: https://www.cdc.gov/cholera/pdf/englishjobaid-stool-col-to-caryblair2.pdf.
Sack D, Lyke C, McLaughlin C, Suwanvanichkij V. Antimicrobial resistance in shigellosis, cholera and campylobacteriosis [internet]. WHO; 2001. Available from: http://www.who.int/drugresistance/Antimicrobial_resistance_in_shigellosis_cholera_and_cam.pdf.
Kim HB, Wang M, Ahmed S, Park CH, LaRocque RC, Faruque ASG, et al. Transferable quinolone resistance in Vibrio cholerae. Antimicrob Agents Chemother. 2010;54(2):799–803.
Klontz EH, Das SK, Ahmed D, Ahmed S, Chisti MJ, Malek MA, et al. Long-term comparison of antibiotic resistance in Vibrio cholerae O1 and Shigella species between urban and rural Bangladesh. Clin Infect Dis. 2014;58(9):e133–6.
Kitaoka M, Miyata ST, Unterweger D, Pukatzki S. Antibiotic resistance mechanisms of Vibrio cholerae. J Med Microbiol. 2011;60(4):397–407.
Dengo-Baloi LC, Semá-Baltazar CA, Manhique LV, Chitio JE, Inguane DL, Langa JP. Antibiotics resistance in El Tor Vibrio cholerae O1 isolated during cholera outbreaks in Mozambique from 2012 to 2015. PLoS One. 2017;12(8):e0181496.
Miwanda B, Moore S, Muyembe J-J, Nguefack-Tsague G, Kabangwa IK, Ndjakani DY, et al. Antimicrobial drug resistance of Vibrio cholerae. Democratic Republic of the Congo Emerg Infect Dis. 2015;21(5):847–51.
Nelson EJ, Nelson DS, Salam MA, Sack DA. Antibiotics for both moderate and severe cholera. N Engl J Med. 2011;364(1):5–7.
Salimi-Khourashad A, Tatabee M, Amirabadi A, Roudbar-Mohamadi S. Vibrio cholerae and changing of microbial resistance patterns in Sistan and Balouchestan Province. Zahedan J Res Med Sci. 2012;14(8):63–6.
Domman D, Quilici M-L, Dorman MJ, Njamkepo E, Mutreja A, Mather AE, et al. Integrated view of Vibrio cholerae in the Americas. Science. 2017;358(6364):789–93.
Weill F-X, Domman D, Njamkepo E, Tarr C, Rauzier J, Fawal N, et al. Genomic history of the seventh pandemic of cholera in Africa. Science. 2017;358(6364):785–9.
Matias WR, Julceus FE, Abelard C, Mayo-Smith LM, Franke MF, Harris JB, Ivers LC. Laboratory evaluation of immunochromatographic rapid diagnostic tests for cholera in Haiti. Azman AS, editor PLoS ONE 2017;12(11):e0186710.
Sayeed MA, Islam K, Hossain M, Akter NJ, Alam MN, Sultana N, et al. Development of a new dipstick (Cholkit) for rapid detection of Vibrio cholerae O1 in acute watery diarrheal stools. PLoS Negl Trop Dis. 2018;12(3):e0006286.
GTFCC. Interim technical note the use of cholera rapid diagnostic tests November 2016 [internet]. WHO/GTFCC; 2016. Available from: http://www.who.int/cholera/task_force/Interim-guidance-cholera-RDT.pdf?ua=1.
Debes AK, Chakraborty S, Ali M, Sack D. Manual for detecting Vibrio cholerae O1 and O139 from fecal samples and from environmental water using a dipstick assay [internet]. JHSPH; 2014. Available from: https://www.stopcholera.org/sites/cholera/files/manual_dipstick_surveillance_using_dipstick_3_30_14_workingdoc.pdf.
WHO. Interim guidance document on cholera surveillance—GTFCC Surveillance Working Group [Internet]. WHO/GTFCC; 2017. Available from: http://www.who.int/cholera/task_force/GTFCC-Guidance-cholera-surveillance.pdf.
Page A-L, Alberti KP, Mondonge V, Rauzier J, Quilici M-L, Guerin PJ. Evaluation of a rapid test for the diagnosis of cholera in the absence of a gold standard. PLoS One. 2012;7(5):e37360.
Dick MH, Guillerm M, Moussy F, Chaignat C-L. Review of two decades of cholera diagnostics—how far have we really come? PLoS Negl Trop Dis. 2012;6(10):e1845.
CDC. The laboratory methods for the diagnosis of Vibrio cholerae. Chapter 5. Examination of food and environmental samples [Internet]. 2016. Available from: https://www.cdc.gov/cholera/pdf/laboratory-methods-for-the-diagnosis-of-vibrio-cholerae-chapter-5.pdf.
Huq A, Haley BJ, Taviani E, Chen A, Hasan NA, Colwell RR. Detection, isolation, and identification of Vibrio cholerae from the environment. In: Coico R, Kowalik T, Quarles J, Stevenson B, Taylor R, editors. Current protocols in microbiology [internet]. Hoboken: John Wiley & Sons, Inc.; 2012. [cited 2018 May 24]. Available from: http://doi.wiley.com/10.1002/9780471729259.mc06a05s26.
Banwell JG, Pierce NF, Mitra RC, Brigham KL, Caranasos GJ, Keimowitz RI, et al. Intestinal fluid and electrolyte transport in human cholera. J Clin Invest. 1970;49(1):183–95.
Tariq M, Memon M, Jafferani A, Shoukat S, Gowani SA, Nusrat R, et al. Massive fluid requirements and an unusual BUN/creatinine ratio for pre-renal failure in patients with cholera. PLoS One. 2009;4(10):e7552.
Pollitzer R. Cholera studies. IX. Symptomatology, diagnosis, prognosis, and treatment. Bull World Health Organ. 1957;16(2):295–430.
Bart KJ, Huq Z, Khan M, Mosley WH. Seroepidemiologic studies during a simultaneous epidemic of infection with El Tor Ogawa and classical Inaba Vibrio cholerae. J Infect Dis. 1970;121(Suppl 121):517–24.
Harris JB, LaRocque RC, Chowdhury F, Khan AI, Logvinenko T, Faruque ASG, et al. Susceptibility to Vibrio cholerae infection in a cohort of household contacts of patients with cholera in Bangladesh. PLoS Negl Trop Dis. 2008;2(4):e221.
Nelson EJ, Harris JB, Morris JGJ, Calderwood SB, Camilli A. Cholera transmission: the host, pathogen and bacteriophage dynamic. Nat Rev Microbiol. 2009;7(10):693–702.
Lindenbaum J, Greenough WB, Islam MR. Antibiotic therapy of cholera in children. Bull World Health Organ. 1967;37(4):529–38.
Greenough WB 3rd, Gordon RSJ, Rosenberg IS, Davies BI, Benenson AS. Tetracycline in the treatment of cholera. Lancet. 1964;1(7329):355–7.
Rahaman MM, Majid MA, AKMJ A, Islam MR. Effects of doxycycline in actively purging cholera patients: a double-blind clinical trial. Antimicrob Agents Chemother. 1976;10(4):610–2.
Kaushik JS, Gupta P, Faridi MM, Das S. Single dose azithromycin versus ciprofloxacin for cholera in children: a randomized controlled trial. Indian Pediatr. 2010;47(4):309–15.
Roy SK, Islam A, Ali R, Islam KE, Khan RA, Ara SH, et al. A randomized clinical trial to compare the efficacy of erythromycin, ampicillin and tetracycline for the treatment of cholera in children. Trans R Soc Trop Med Hyg. 1998;92(4):460–2.
Das S, Choudhry S, Saha R, Ramachandran VG, Kaur K, Sarkar BL. Emergence of multiple drug resistance Vibrio cholerae O1 in East Delhi. J Infect Dev Ctries. 2011;5(4):294–8.
Marin MA, Thompson CC, Freitas FS, Fonseca EL, Aboderin AO, Zailani SB, et al. Cholera outbreaks in Nigeria are associated with multidrug resistant atypical El Tor and non-O1/non-O139 Vibrio cholerae. PLoS Negl Trop Dis. 2013;7(2):e2049.
Sjolund-Karlsson M, Reimer A, Folster JP, Walker M, Dahourou GA, Batra DG, et al. Drug-resistance mechanisms in Vibrio cholerae O1 outbreak strain, Haiti, 2010. Emerg Infect Dis. 2011;17(11):2151–4.
Roy SK, Hossain MJ, Khatun W, Chakraborty B, Chowdhury S, Begum A, et al. Zinc supplementation in children with cholera in Bangladesh: randomised controlled trial. BMJ. 2008;336(7638):266–8.
Zijlmans WCWR, van Kempen AAMW, Serlie MJ, Sauerwein HP. Glucose metabolism in children: influence of age, fasting, and infectious diseases. Metabolism. 2009;58(9):1356–65.
Griffith LS, Fresh JW, Watten RH, Villaroman MP. Electrolyte replacement in paediatric cholera. Lancet Lond Engl. 1967;1(7501):1197–9.
Molla AM, Rahman M, Sarker SA, Sack DA, Molla A. Stool electrolyte content and purging rates in diarrhea caused by rotavirus, enterotoxigenic E. coli, and V. cholerae in children. J Pediatr. 1981;98(5):835–8.
WHO. Guideline: Updates on the management of severe acute malnutrition in infants and children. Geneva: World Health Organization; 2013.
WHO. Management of severe malnutrition: A manual for physicians and other senior health workers [Internet]. WHO; 1999. Available from: http://apps.who.int/iris/bitstream/handle/10665/41999/a57361.pdf;jsessionid=7828902D32C1C1A2CD548642A1F8EEC0?sequence=1.
Ververs M, Narra R. Treating cholera in severely malnourished children in the horn of Africa and Yemen. Lancet. 2017;390(10106):1945–6.
Schillberg E, Ariti C, Bryson L, Delva-Senat R, Price D, GrandPierre R, et al. Factors related to fetal death in pregnant women with cholera, Haiti, 2011-2014. Emerg Infect Dis. 2016;22(1):124–7.
Ciglenecki I, Bichet M, Tena J, Mondesir E, Bastard M, Tran N-T, et al. Cholera in pregnancy: outcomes from a specialized cholera treatment unit for pregnant women in Leogane, Haiti. PLoS Negl Trop Dis. 2013;7(8):e2368.
Hirschhorn N, Chowdhury AK, Lindenbaum J. Cholera in pregnant women. Lancet Lond Engl. 1969;1(7608):1230–2.
Cutler D, Miller G. The role of public health improvements in health advances: the twentieth-century United States. Demography. 2005;42(1):1–22.
Sepúlveda J, Valdespino JL, García-García L. Cholera in Mexico: the paradoxical benefits of the last pandemic. Int J Infect Dis. 2006;10(1):4–13.
Alcayaga S, Alcayaga J, Gassibe P. Changes in the morbidity profile of certain enteric infections after the cholera epidemic. Rev Chile Infect. 1993;1:5–10.
Mintz ED, Blackstock AJ, Nygren BL. Cholera at the crossroads: the association between endemic cholera and national access to improved water sources and sanitation. Am J Trop Med Hyg. 2014;91(5):1023–8.
Taylor DL, Kahawita TM, Cairncross S, Ensink JHJ. The impact of water, sanitation and hygiene interventions to control cholera: a systematic review. Bhutta ZA, editor. PLOS ONE. 2015;10(8):e0135676.
Wang A, Hardy C, Rajasingham A, Martinsen A, Templin L, Kamwaga S, et al. Notes from the field: chlorination strategies for drinking water during a cholera epidemic—Tanzania. 2016 MMWR Morb Mortal Wkly Rep. 2016;65(41):1150–1.
Sinyange N, Brunkard JM, Kapata N, Mazaba ML, Musonda KG, Hamoonga R, et al. Cholera epidemic—Lusaka, Zambia, October 2017-May 2018. MMWR Morb Mortal Wkly Rep. 2018;67(19):556–9.
Alam M, Sack RB, Parvin T, George CM, Zohura F, Shaly NJ, et al. Promotion of cholera awareness among households of cholera patients: a randomized controlled trial of the cholera-hospital-based-intervention-for-7 days (CHoBI7) intervention. Am J Trop Med Hyg. 2016;95(6):1292–8.
George CM, Monira S, Sack DA, Rashid M, Saif-Ur-Rahman KM, Mahmud T, et al. Randomized controlled trial of hospital-based hygiene and water treatment intervention (CHoBI7) to reduce cholera. Emerg Infect Dis. 2016;22(2):233–41.
Sack RB, Saif-Ur-Rahman KM, Bhuyian SI, Akhter S, Mahmud T, Sack D, et al. Chlorination of household drinking water among cholera patients’ households to prevent transmission of toxigenic Vibrio cholerae in Dhaka, Bangladesh: CHoBI7 trial. Am J Trop Med Hyg. 2016;95(6):1299–304.
UNICEF, CDC, MSF. Draft document for a position paper against chlorine spraying at households of cholera patients [internet]. UNICEF, CDC, MSF; 2011. Available from: https://www.unicef.org/cholera/Chapter_9_community/Haiti-POs_paper_against_chlorine_HH_spraying_cholera.docx.
ICG. Oral cholera vaccine stockpile for cholera emergency response [Internet]. ICG; 2013. Available from: http://www.who.int/cholera/vaccines/Briefing_OCV_stockpile.pdf.
• WHO. Cholera vaccines: WHO Position paper—August 2107. Wkly Epidemiol Rec. 2017;92(34):477–500. Review of oral cholera vaccines currently in use.
WHO. Deployments from the oral cholera vaccine stockpile, 2013-2017. Wkly Epidemiol Rec. 2017;92(32):437–42.
Khan AI, Ali M, Chowdhury F, Saha A, Khan IA, Khan A, et al. Safety of the oral cholera vaccine in pregnancy: retrospective findings from a subgroup following mass vaccination campaign in Dhaka. Bangladesh Vaccine. 2017;35(11):1538–43.
Hashim R, Khatib AM, Enwere G, Park JK, Reyburn R, Ali M, et al. Safety of the recombinant cholera toxin B subunit, killed whole-cell (rBS-WC) oral cholera vaccine in pregnancy. PLoS Negl Trop Dis. 2012;6(7):e1743.
Grout L, Martinez-Pino I, Ciglenecki I, Keita S, Diallo AA, Traore B, et al. Pregnancy outcomes after a mass vaccination campaign with an oral cholera vaccine in Guinea: a retrospective cohort study. PLoS Negl Trop Dis. 2015;9(12):e0004274.
Bhattacharya SK, Sur D, Ali M, Kanungo S, You YA, Manna B, et al. 5 year efficacy of a bivalent killed whole-cell oral cholera vaccine in Kolkata, India: a cluster-randomised, double-blind, placebo-controlled trial. Lancet Infect Dis. 2013;13(12):1050–6.
Ivers LC, Hilaire IJ, Teng JE, Almazor CP, Jerome JG, Ternier R, et al. Effectiveness of reactive oral cholera vaccination in rural Haiti: a case-control study and bias-indicator analysis. Lancet Glob Health. 2015;3(3):e162–8.
Azman AS, Parker LA, Rumunu J, Tadesse F, Grandesso F, Deng LL, et al. Effectiveness of one dose of oral cholera vaccine in response to an outbreak: a case-cohort study. Lancet Glob Health. 2016;4(11):e856–63.
Qadri F, Wierzba TF, Ali M, Chowdhury F, Khan AI, Saha A, et al. Efficacy of a single-dose, inactivated oral cholera vaccine in Bangladesh. N Engl J Med. 2016;374(18):1723–32.
Desai SN, Pezzoli L, Alberti KP, Martin S, Costa A, Perea W, et al. Achievements and challenges for the use of killed oral cholera vaccines in the global stockpile era. Hum Vaccines Immunother. 2017;13(3):579–87.
Qadri F, Ali M, Lynch J, Chowdhury F, Khan AI, Wierzba TF, et al. Efficacy of a single-dose regimen of inactivated whole-cell oral cholera vaccine: results from 2 years of follow-up of a randomised trial. Lancet Infect Dis 2018;18(6):666–74.
Guevart E, Solle J, Noeske J, Amougou G, Mouangue A, Fouda AB. Mass antibiotic prophylaxis against cholera in the new bell central prison in Douala during the 2004 epidemic. Sante. 2005;15(4):225–7.
Bwire G, Makumbi I, Mintz E, Malimbo M, Mengel MA, Kagirita A, et al. Nosocomial cholera outbreak in a mental hospital: challenges and lessons learnt from Butabika National Referral Mental Hospital. Uganda Am J Trop Med Hyg. 2015;93(3):534–8.
UNICEF. UNICEF cholera toolkit [internet]. UNICEF; 2017. Available from: https://www.unicef.org/cholera/index_71222.html.
WHO/AFRO. Situational report No. 141 [Internet]. 2018. Available from: http://www.afro.who.int/sites/default/files/2018-03/Zambia_Sitrep_Cholera%20-%201%20March%202018%20final.docx_.pdf.
Reveiz L, Chapman E, Ramon-Pardo P, Koehlmoos TP, Cuervo LG, Aldighieri S, et al. Chemoprophylaxis in contacts of patients with cholera: systematic review and meta-analysis. von Seidlein L, editor. PLoS ONE. 2011;6(11):e27060.
Weber JT, Mintz ED, Canizares R, Semiglia A, Gomez I, Sempertegui R, et al. Epidemic cholera in Ecuador: multidrug-resistance and transmission by water and seafood. Epidemiol Infect. 1994;112(1):1–11.
Towner KJ, Pearson NJ, Mhalu FS, O’Grady F. Resistance to antimicrobial agents of Vibrio cholerae E1 Tor strains isolated during the fourth cholera epidemic in the United Republic of Tanzania. Bull World Health Organ. 1980;58(5):747–51.
WHO. Cholera vaccines: WHO position paper—August 2017 [Internet]. WHO/WER; 2017. Available from: http://apps.who.int/iris/bitstream/handle/10665/258763/WER9234.pdf?sequence=1.
Bi Q, Ferreras E, Pezzoli L, Legros D, Ivers LC, Date K, et al. Protection against cholera from killed whole-cell oral cholera vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2017;17(10):1080–8.
Acknowledgments
We gratefully acknowledge the assistance of Maryann Turnsek and Amy Lang in preparing this manuscript.
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Infectious Disease Epidemiology
Rights and permissions
About this article
Cite this article
Davis, W., Narra, R. & Mintz, E.D. Cholera. Curr Epidemiol Rep 5, 303–315 (2018). https://doi.org/10.1007/s40471-018-0162-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40471-018-0162-z