Abstract
Purpose of Review
It has been suggested that similar brain regions are activated to ultra-processed food as in substance addiction, giving rise to the concept of “food addiction”. However, few neuroimaging studies have used specific assessment tools for food addiction, with obesity often used as a proxy, leading to considerable variability in neural activation patterns associated with food addiction. This systematic review aimed to synthesise published studies using task-related and resting-state fMRI to assess neural responses associated with food addiction, using a validated assessment tool, the Yale Food Addiction Scale (YFAS). A systematic review was conducted from 2008 to July 2022 according to the PRISMA guidelines. Studies were included if they reported YFAS food addiction outcomes in combination with task-related or resting-state fMRI outcomes. Two reviewers independently appraised studies and data were synthesised descriptively.
Recent Findings
Seven task-related and four resting-state fMRI studies were included, involving 675 predominantly female participants. Brain areas involved in reward, craving, and appetitive responses were associated with YFAS-assessed food addiction in response to high-calorie processed foods in task-related fMRI studies, as well as impaired inhibition in non-food-related tasks. In the resting-state studies, altered connectivity in reward-related regions and cognitive control were commonly reported. However, activation across included studies was not consistent, with some studies reporting no relationship between food addiction scores and neural activation.
Summary
There was a lack of consistency in activation across studies which may be due to the heterogeneity of study designs. It is difficult to ascertain if there are indeed neural activation patterns that are unique to food addiction and what components of food may have addictive potential. Future studies are required with replicable study designs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A growing body of evidence suggests that there are behavioural, neurobiological, and genetic overlaps between the consumption of certain foods and addiction-related disorders [1, 2]. The term “food addiction” has been used to describe compulsive eating patterns that resemble addictive-related disorders and has frequently been operationalized using the Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria for substance use disorders [3]. However, food addiction is not currently recognised as a diagnosable condition according to the DSM-5. There is also ongoing debate as to whether food addiction is better characterised as a substance-use disorder, i.e. a certain food, ingredient, or nutrient facilitating an addictive-like response (e.g. sugar), or behavioural addiction, (i.e. an eating addiction irrespective of nutritional composition) [4], or a subgroup of eating disorder [5]. Evidence to date suggests that highly processed foods with a combination of fat and refined sugars are those that are more likely to facilitate an addictive-like response [6•]. The prevalence of food addiction has been reported to be 15–20% across published studies and is higher in females, those of higher weight status, and clinical populations such as those with mental health disorders including eating disorders [7, 8•].
The Yale Food Addiction Scale (YFAS) is a validated tool specifically developed in 2008 to assess addictive eating according to the DSM-IV criteria for substance use disorders [9]. The YFAS utilises two scoring outputs, a symptom score based on the number of food addiction symptoms that are endorsed, as well as a “diagnosis” of food addiction when three or more symptoms are endorsed, plus clinical impairment or distress. The tool was updated in 2016 to reflect the DSM-5 criteria for substance use disorders, with the updated tool also reflecting the severity of food addiction [10]. The YFAS has been adapted for different populations, including the YFAS-C [9, 11], designed for children by modifying the reading level, as well as the modified YFAS (mYFAS) [12], a shortened version of the tool. While other tools have been designed to assess aspects of addictive and reward-based eating [13,14,15,16], the YFAS is the most widely used and reported tool. The YFAS has been used in combination with several biomarkers, genetics, and neuroimaging techniques to provide insight into the mechanisms associated with addictive eating symptomatology [17, 18].
Reward networks in the brain have been suggested to be involved in the development and maintenance of addictive-like eating behaviours [19, 20]. Neuroimaging techniques, such as functional magnetic resonance imaging (fMRI), have identified activation of brain regions in response to visual and gustatory food cues, particularly highly palatable ultra-processed foods, in a similar way to other illicit substances [21] and eating disorders such as binge eating disorder [22]. This has led to suggestions that there may be similar underlying mechanisms and aetiology between certain pathological eating behaviours and other addictions. Importantly, higher body mass index (BMI) has often been used as a proxy to assess addictive eating in neuroimaging studies [23] rather than as a validated assessment tool for food addiction. This has led to inconsistency in neural responses associated with addictive eating as it is unclear as to how many people within these samples may truly exhibit addictive behaviours towards foods.
A narrative review (2020) of neuroimaging and food addiction reported limited consistency in the activation of brain networks and limited evidence of neural activation mirroring that of substance use disorders [24•]. This was attributed by the authors to the heterogeneous nature of the construct of food addiction, overinterpretation of results, and lack of replicability of study designs across published studies [24•]. In contrast, another review of 15 neuroimaging studies reported similar activation of areas associated with addiction including executive functioning, reward activity and sensitivity, and sensory and motor areas associated with food intake and eating [25•]. This previous review, however, included several neuroimaging techniques and various assessment measures for food addiction, which may have introduced variability into the study findings [25•]. No reviews have systematically evaluated neural responses associated food addiction using a consistent assessment tool to evaluate the construct, such as the YFAS.
In summary, there has been limited consistency in neural responses associated with food addiction in imaging reviews to date [24•, 25•], which may be due to the range of neuroimaging techniques used, range of assessment measures for addictive eating, use of obesity as a proxy for addictive eating, and narrative nature of existing reviews [24•]. It is important to better understand the underlying neural responses associated with addictive eating using a validated tool to identify consistencies or inconsistencies in neural activation across studies to date. This may assist in better understanding whether food addiction is a standalone, diagnosable phenomenon and may help to identify and develop more effective treatment targets, as well as assess the efficacy of interventions aiming to manage food addiction symptoms. Understanding the neural activation patterns associated with food addiction may also assist in identifying whether there are specific foods or nutrients associated with addictive-like activation, assisting to disentangle whether this construct better resembles a substance use or behavioural addiction. It is timely to synthesise existing evidence regarding neural responses associated with addictive eating to better understand the neurobiology associated with the phenomenon and identify potential gaps in the research. This systematic review aimed to synthesise published studies using task-related and resting state fMRI to assess neural responses associated with addictive eating, as assessed by the YFAS.
Methods
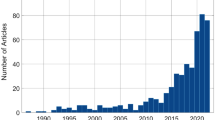
A systematic search strategy was conducted from 2008, the year of YFAS development, to July 2022. Seven databases were searched including Cochrane Database, CINAHL, EMBASE, MEDLINE, PsycINFO, Scopus, and Web of Science. Two sets of terms were used for the search strategy, (1) terms relating to addictive eating and the Yale Food Addiction Scale; and (2) terms relating to functional magnetic resonance imaging. Searches were limited to humans and publications in the English language. The search strategy is available in Appendix 1. The review methodology was registered with OSF (Open Science Framework) Registries (https://osf.io/uvy84) and conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Guidelines [26].
Study Criteria
This review included studies that use task-related or resting state functional MRI to explore the neural responses associated with addictive eating, as assessed using a version of the Yale Food Addiction Scale (e.g. YFAS, mYFAS, YFAS 2.0, or YFAS-c). Males and females aged > 10 years who had completed a version of the YFAS and undergone a task-related or resting state fMRI scan were included in the review. Children < 10 years were excluded as their dietary intakes may be more influenced by their parents and carers. Studies that included younger children in the age range, but the mean age of the sample was > 10 years of age were included in the review. Other forms of assessment or identification of addictive eating such as self-identification or other self-report tools were excluded from the review. Studies using a comparator group such as low food addiction symptoms or individuals classified as non-food addicted using the YFAS as a comparator as well as studies with no comparator were included. All study designs were considered for inclusion in the review including randomised controlled trials, non-randomised or quasi-randomised controlled trials, cohort studies, and pre-post and cross-sectional studies. Narrative reviews, theses, commentaries, letters to the editor, and studies with inadequate information regarding the methodological details of the study were not included in the review.
Study Selection
After the removal of duplicates, identified studies were imported into Covidence web-based software (www.covidence.org). Titles and abstracts were screened by two independent reviewers. Full-text articles were subsequently retrieved and screened by two reviewers for inclusion in the review. In any case of uncertainty about a study’s inclusion in the review, a third reviewer was consulted until a consensus was reached.
Quality of Evidence and Risk of Bias
Quality of retrieved studies was assessed by two independent reviewers (KMP and KB) using the Academy of Nutrition and Dietetics Quality Criteria Checklist for Primary Research [27], a standardised 10-item tool that can be applied to a broad range of study designs. This checklist includes 10 criteria which relate to the presence or absence of threats to the validity of research including clarity of the research question, subject selection, comparability of study groups, handling of withdrawals, blinding, descriptions of the intervention, validity of outcome measures, appropriateness of statistical methods and data synthesis, conclusions drawn, and likelihood of funding bias. Each item was classified as present “yes” (high risk of bias), “no” (low risk of bias), absent, or “unclear” for each included study. The overall study quality was then rated as positive (i.e. low risk of bias) if criteria 2, 3, 6, 7, and 1 other were yes, neutral if criteria 2, 3, 6, and/or 7 were no, unclear, or negative (i.e. high risk of bias) if 6 or more criteria were no. Discrepancies were resolved through discussion among the independent reviewers, and no studies were excluded based on quality ratings. The quality assessment was visualised using the Robvis tool [28].
Data Extraction and Synthesis
Data extraction was conducted using a standardised table developed for this review. Data extracted included sample characteristics, YFAS outcomes, nutritional standardisation such as fasting times and nutritional composition of food cues, fMRI tasks and cues, fMRI paradigm and analysis, and fMRI outcomes. One author extracted the data from the included studies, and a second author independently checked the extracted data (KP, KB). Studies were synthesised in a narrative summary. Studies were grouped according to task-related or resting-state fMRI for subgroup analysis. Effect sizes reported in papers were reported, and for those that did not report effect sizes, Cohen’s d was calculated [29]. Effect sizes were interpreted as small (0.2), medium (0.5), or large (0.8) [29]. Due to an insufficient number of studies with similar fMRI outcomes and comparable fMRI paradigms, a meta-analysis of primary outcome measures was not able to be conducted.
Results
The search strategy identified 4654 studies, of which 11 papers describing 11 studies were included in the final synthesis (Fig. 1). Seven studies investigated task-related fMRI [30,31,32,33,34,35,36] and four investigated resting-state responses associated with YFAS-assessed food addiction [37,38,39,40]. All studies were cross-sectional in design with one pre-post study [38].
Risk of Bias
The risk of bias across nine of the eleven included studies was considered low, with two studies classified as neutral (Fig. 2). Reporting of blinding (n = 11 studies), handling of withdrawals (n = 3 studies), and comparability of study groups at baseline (n = 2 studies) were not clearly reported.
Task-Related Studies
A total of 411 participants were included in the seven task-related studies (range 13–165 participants) (Table 1). Five studies investigated adults [30, 33,34,35,36] and two studies in children and adolescents [31, 41] (age range 8 to 55 years). Participants were predominantly female, with four studies investigating females only [30, 33, 34, 36], while the remaining three included both males and females. Across studies, BMI ranged from 21 to 51 kg/m2, with nine studies recruiting participants with a mean BMI in the overweight and obese categories. Five studies used the original YFAS, one used the YFAS 2.0, one used the YFAS-C, and one used the modified YFAS.
Fasting across three task-related studies ranged from 4 to 6 h [30, 34, 36], while standardised fasting was unclear in four studies. Only one study reported standardisation of the meal provided prior to fasting [34]. A range of tasks was used across studies, including visual food cues (n = 3) [30, 34, 36], gustatory food cues (n = 2) [30, 31], and non-food tasks (n = 3; Go-No go task, number guessing paradigm) [33, 35, 41]. In those that used food cues, foods were described as “high calorie” or “low calorie”, and “highly processed” or “minimally processed”, with only two studies reporting the nutritional composition of food cues presented [34, 36]. Three studies used a regions of interest (ROI) [30, 34, 35] analysis, and five used whole brain analysis, with one of these studies using both ROI and whole brain analysis.
In the three studies that used visual food cues including high-calorie, processed foods and low-calorie, minimally processed foods [30, 34, 36], YFAS assessed food addiction was significantly associated with elevated activation in brain regions associated with reward, craving, reward-seeking, and appetitive behaviours (Table 2). In one study, higher YFAS scores were positively associated with left anterior cingulate cortex (ACC), left medial orbitofrontal cortex (mOFC), and left amygdala response to an image of a chocolate milkshake in females (4). Further, females with high versus low YFAS scores showed elevated left dorsolateral prefrontal cortex (dlPFC) and right caudate response to the milkshake image [30]. In another study, females of higher weight status with food addiction showed an elevated response in the superior frontal gyrus (SFG), an area associated with reward-related decision making, to highly processed food cues such as pizza and diminished SFG activation to minimally processed foods such as fruit [36]. In a third study, females with elevated YFAS symptom scores showed greater basolateral amygdala response, an area associated with reward-seeking and promoting appetitive behaviours, to high-calorie foods (e.g. chocolate, chips) compared to low-calorie, naturally occurring foods (e.g. fruits and vegetables) when fasted but not when fed [34]. No significant associations were found between YFAS scores and central amygdala response or other brain regions as determined by whole brain analysis in the fasted or fed conditions in response to high- vs low-calorie food cues [34], suggesting that the basolateral response during the fasted condition may be a distinctive marker. Two studies used gustatory food cues. Ewing et al. did not find significant correlations between YFAS scores and neural response to the taste of sugar-sweetened beverages (i.e. soda) [31]. Similarly, Gearhardt et al. did not find significant correlations between YFAS scores and neural response to a chocolate milkshake taste [30]. However, those with high FA symptoms showed less lateral OFC response to the milkshake taste compared to those with low FA symptoms [30]. Effect sizes for food-related tasks were large (d = 1.00–2.40).
In the three studies that used tasks with non-food cues, two studies reported impairments in response inhibition during a Go-No go task in adolescents [32] and in adult females [33] with elevated YFAS scores (Table 2). Greater activation in the insula and putamen was also reported in females during commission errors in a Go-No go task, regions associated with the error processing function [33]. Food addiction scores were inversely related to activity in the ventral striatum in a monetary incentive paradigm, suggesting blunted reward-related activity to a general reward [35]. Effect sizes for non-food tasks were medium to large (d = 0.46–1.39).
Resting-State Studies
A total of 264 participants were included across four resting-state studies (range 14 to 150 participants per study) (Table 1) [37,38,39,40]. Three studies recruited both males and females, while one recruited female participants only [38]. All resting-state studies investigated adults over 18 years of age, with one study recruiting participants undergoing bariatric surgery [38]. The original YFAS was used in all resting-state studies.
Nutritional standardisation before the scan was reported in only one study, which included a fasted scan after 4 to 10 h and a fed scan after a standardised meal [39]. Instructions for the scan included closing eyes in two studies [37, 40], while a third study instructed participants to lie still and think of nothing [39]. One study did not report standardised instructions to participants [38]. Region of interest analyses were conducted in all four studies, focusing on areas and networks associated with food intake, reward processing, and executive functioning. For further information regarding specific brain areas for analysis, please refer to Table 2.
Changes in connectivity of reward-related regions were reported across all resting-state studies (Table 2). In a study of females undergoing bariatric surgery, a negative correlation was observed between functional connectivity strength in the left DLPFC and YFAS symptom scores, indicating weaker connectivity in an area associated with reward-related decision making [37]. Higher symptoms of food addiction were positively related to greater changes in functional connectivity between the ventral striatum and bilateral hippocampus in the fasted state and from fasted to fed scans in both males and females [39]. These latter findings suggest that food addiction is related to changes in reward prediction signalling as a function of homeostatic status [39]. In both males and females of higher weight status, food addiction was associated with greater connectivity among reward regions and between the brainstem and central autonomic networks and lower connectivity among the executive functioning, sensorimotor, and default-mode network (DMN). In the same study, when analysed by sex, females versus males with food addiction showed greater connectivity in the emotional regulation networks and salience networks, and lower connectivity in the brainstem, central executive, and DMN, suggesting greater emotional eating behaviours in females and greater cognitive control and homeostatic processing in males [40]. In the final study, negative correlations were reported between functional connectivity strength of the left DLPFC and YFAS scores post bariatric surgery, suggesting that food addiction symptoms are associated with disrupted executive functioning, as well as the reward network (i.e. connectivity between the precuneus and putamen) [38]. Effect sizes of altered connectivity ranged from small to large (d = 0.32–0.83). Effect sizes could not be calculated for two of the studies.
Discussion
This is the first review to systematically appraise studies investigating the neural responses associated with food addiction, as assessed using the YFAS. This review found that brain areas related to reward, craving, and appetitive responses in response to highly processed, high-calorie foods were associated with YFAS-assessed food addiction, as well as impaired inhibition in task-related fMRI studies. In the resting-state studies, altered connectivity in reward-related regions and cognitive control were commonly reported. The effect sizes varied from medium to large across task-related fMRI studies and small to large across resting-state studies. However, across included studies there was a lack of consistency in the specific areas of activation associated with food addiction. This may be due to the variability in study designs, participant characteristics, sample sizes, types of food cues used and mode of delivery, and paradigms used across published studies. Consequently, it is difficult to ascertain whether there are indeed unique neural activation patterns associated with YFAS food addiction.
Across task-related studies using food cues, associations were found between YFAS food addiction scores and activation in the left ACC, left medial OFC, left amygdala, basolateral amygdala, and right SFG in response to images of high calorie, processed foods compared to minimally processed, low-calorie foods. Areas such as the ACC and medial OFC have been implicated in motivation to feed [42, 43], while the basolateral amygdala has been shown to drive external cues to hypothalamic feeding centres, coding food reward, food reward-seeking behaviours, and relapse to food seeking [44,45,46]. This suggests that individuals with higher food addiction symptomatology may be susceptible to environmental food cues, specifically highly palatable ultra-processed foods, and motivation to feed, which may lead to overeating. In two studies using non-food-related tasks, food addiction was negatively related with inhibitory control region response during a go/no-go task. This was similar to studies of food-related tasks, where decreased activation in executive control systems in response to consumption of a high-calorie milkshake [30] was reported in people with high food addiction scores. Moreover, the SFG, associated with reward-related decision-making [47], was shown to have diminished activation in individuals with food addiction in response to images of highly processed foods. Taken collectively, this suggests that people with greater food addiction symptoms may experience impairments in food-related decision-making and response inhibition, which may impact on nutritional intake, particularly of high-calorie, processed foods.
This is the first review to evaluate resting-state responses associated with YFAS food addiction. Four studies explored changes in connectivity associated with food addiction using resting-state fMRI and all reported changes in reward-related networks, indicative of altered functioning of the reward network. Moreover, two studies found that food addiction was associated with lower connectivity in executive control regions. Executive control regions are responsible for working memory, information processing, and decision making [48], with impaired executive functioning linked to prediction of weight gain and impaired appetite control [49, 50]. In addition, Contreras–Rodriguez et al. reported associations between food addiction and changes in reward circuitry in fasted compared to fed individuals, which may indicate increases in food reward reactivity when hungry. This may assist in informing future management approaches for addictive-like eating, by recommending regular meals to avoid a severe hunger state and subsequent hyper-responsiveness to food reward. Similarly, future treatment approaches may consider working with people experiencing addictive-like eating behaviours to identify signs of physical hunger as well as internal and external cues to eating, similarly to the management of other types of disordered eating behaviours such as binge eating disorder [51].
Despite activation of regions overlapping those of substance use disorders, the areas of activation across studies in this review were inconsistent, and one study (29) did not find significant associations between food addiction symptoms and neural activation associated with visual or gustatory food cues of a sugar-sweetened beverage. Despite this, those studies that did report associations between YFAS-assessed food addiction and neural activity reported medium to large effect sizes in the task-related studies, indicating strong activation in these brain regions. However, resting-state studies reported lower effect sizes, which may indicate a lower strength of alterations in connectivity related to food addiction. This variability may be due to the range of fMRI paradigms and tasks used including different types and descriptions of food cues (e.g. high calorie vs low calorie, highly processed vs minimally processed), as well as non-food related tasks. The lack of consistency found in the current review is in line with the narrative findings of Garcia–Garcia et al. [24•], which found considerable heterogeneity in their review of studies assessing neural responses associated with addictive eating. The lack of consistency may also be due to the potentially heterogeneous nature of the food addiction construct and associated behaviours, which would be linked with different neurobiological mechanisms. Alternatively, the use of a self-reported assessment tool may introduce variation in study findings. There is a need for standardisation and replication of study designs to identify if there are indeed unique patterns of activation associated with food addiction.
Exploring the divergence in study designs in further detail, motivational states, types of food cues, and tasks differed significantly. Motivational state and energy density of food cues have been reported to affect neural responses [23, 24•]; however, across both task-related and resting state designs, few studies reported this. Foods that have typically been the foci of food addiction research have been high-calorie, ultra-processed foods. However, a recent review reported that while processed foods with high concentrations of both fat and sugar are most likely to be those that facilitate an addictive-like response [52], there is a need for further scientific evidence to support this [6•]. With few studies reporting the nutritional composition of food cues presented in combination with the YFAS, it is difficult to ascertain whether there is a specific food, nutrient, or level of processing that may contribute to an addictive-like neural response. However, from the small number of studies using food cues in the current review, there were significant associations between processed and high-calorie foods with food addiction scores, compared to minimally processed and low-calorie foods, warranting further investigation. In addition, it is important to understand the motivational state of participants and its effects on responsivity to inform future management approaches intersecting hunger state and external food environment cues. It is recommended that future studies investigating neural responses to YFAS food addiction standardise the fasting times of participants and report the nutritional composition of food cues used to better understand the influence of motivational states and types of foods presented on addictive-like responses.
Strengths of this review include the inclusion of studies that use the YFAS to assess food addiction specifically with the view to disentangling studies that have conflated food addiction with elevated BMI, which has been acknowledged as a limitation in previous research [24•]. A further strength is the inclusion of both task-related and resting-state studies, to give a better understanding of both task-related activation as well as potential changes in connectivity associated with food addiction. This review is limited by the heterogeneity of studies included in the review, which precluded meta-analysis of fMRI outcomes. Further studies are required using comparable study designs to facilitate meta-analysis. Small sample sizes, females and individuals of higher BMI were overrepresented across included studies, limiting the generalisability of the review findings to males and those of different BMIs. Few studies investigated children, adolescents, and older adults, highlighting a need for further studies investigating young people and older adults to better understand neural activation patterns associated with food addiction in these age groups. Finally, published studies to date are overwhelmingly cross-sectional in nature, highlighting the need for longitudinal studies investigating potential changes in neural responses associated with food addiction over time, or in the context of an intervention.
Conclusions
While this review did find some changes in neural activation and connectivity in reward-related regions of the brain associated with YFAS-assessed food addiction, particularly with highly processed high-calorie food cues, there was a lack of consistency across included studies. This may be due in part to the lack of consistency in study designs and participant characteristics across included studies. Future studies with reproducible, standardised paradigms are required to better understand the underlying neural mechanisms associated with food addiction, including the potential foods that may elicit an addictive-like response.
References
Papers of particular interest, published recently, have been highlighted as: • Of major importance
Gordon EL, Ariel-Donges AH, Bauman V, Merlo LJ. What is the evidence for “food addiction?” A systematic review. Nutrients. 2018;10(4):477. https://doi.org/10.3390/nu10040477.
Gearhardt AN, Schulte EM. Is food addictive? A review of the science. Annu Rev Nutr. 2021;41(1):387–410.
Gearhardt AN, Corbin WR, Brownell KD. Food addiction: an examination of the diagnostic criteria for dependence. J Addict Med. 2009;3(1):1–7.
Hebebrand J, Albayrak Ö, Adan R, Antel J, Dieguez C, De Jong J, et al. “Eating addiction”, rather than “food addiction”, better captures addictive-like eating behavior. Neurosci Biobehav Rev. 2014;47:295–306.
Davis C. Compulsive overeating as an addictive behavior: overlap between food addiction and binge eating disorder. Curr Obes Rep. 2013;2(2):171–8.
• Pursey KM, Skinner J, Leary M, Burrows T. The relationship between addictive eating and dietary intake: a systematic review. Nutrients. 2021;14(1):164. https://doi.org/10.3390/nu14010164. Systematic review of foods and dietary profiles associated with food addiction.
Pursey KM, Stanwell P, Gearhardt AN, Collins CE, Burrows TL. The prevalence of food addiction as assessed by the Yale Food Addiction Scale: a systematic review. Nutrients. 2014;6(10):4552–90.
• Praxedes DRS, Silva-Júnior AE, Macena ML, Oliveira AD, Cardoso KS, Nunes LO, et al. Prevalence of food addiction determined by the Yale Food Addiction Scale and associated factors: a systematic review with meta-analysis. Eur Eat Disord Rev. 2022;30(2):85–95. Recent systematic review and meta-analysis of the prevalence of food addiction.
Gearhardt AN, Roberto CA, Seamans MJ, Corbin WR, Brownell KD. Preliminary validation of the Yale Food Addiction Scale for children. Eat Behav. 2013;14(4):508–12.
Gearhardt AN, Corbin WR, Brownell KD. Development of the Yale Food Addiction Scale Version 2.0. Psychol Addict Behav. 2016;30(1):113.
Schiestl ET, Gearhardt AN. Preliminary validation of the Yale Food Addiction Scale for Children 2.0: a dimensional approach to scoring. Eur Eat Disord Rev. 2018;26(6):605–17.
Schulte EM, Gearhardt AN. Development of the modified Yale Food Addiction Scale Version 2.0. Eur Eat Disord Rev. 2017;25(4):302–8.
Ruddock HK, Christiansen P, Halford JCG, Hardman CA. The development and validation of the Addiction-like Eating Behaviour Scale. Int J Obes. 2017;41(11):1710–7.
Schulte EM, Smeal JK, Lewis J, Gearhardt AN. Development of the Highly Processed Food Withdrawal Scale. Appetite. 2018;131:148–54.
Boggiano MM. Palatable Eating Motives Scale in a college population: distribution of scores and scores associated with greater BMI and binge-eating. Eat Behav. 2016;21:95–8.
Epel ES, Tomiyama AJ, Mason AE, Laraia BA, Hartman W, Ready K, et al. The Reward-Based Eating Drive Scale: a self-report index of reward-based eating. PLoS One. 2014;9(6):e101350.
Long CG, Blundell JE, Finlayson G. A systematic review of the application and correlates of YFAS-diagnosed ‘food addiction’ in humans: are eating-related ‘addictions’ a cause for concern or empty concepts? Obes Facts. 2015;8(6):386–401.
Davis C, Loxton NJ, Levitan RD, Kaplan AS, Carter JC, Kennedy JL. ‘Food addiction’and its association with a dopaminergic multilocus genetic profile. Physiol Behav. 2013;118:63–9.
Volkow ND, Wang GJ, Tomasi D, Baler RD. Obesity and addiction: neurobiological overlaps. Obes Rev. 2013;14(1):2–18.
Avena NM, Rada P, Hoebel BG. Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev. 2008;32(1):20–39.
Kenny PJ. Reward mechanisms in obesity: new insights and future directions. Neuron. 2011;69(4):664–79.
Kessler RM, Hutson PH, Herman BK, Potenza MN. The neurobiological basis of binge-eating disorder. Neurosci Biobehav Rev. 2016;63:223–38.
Pursey KM, Stanwell P, Callister RJ, Brain K, Collins CE, Burrows TL. Neural responses to visual food cues according to weight status: a systematic review of functional magnetic resonance imaging studies. Front Nutr. 2014;1:7.
• García-García I, Morys F, Michaud A, Dagher A. Food Addiction, Skating on thin ice: a critical overview of neuroimaging findings. Curr Addict Rep. 2020;7(1):20–29. https://doi.org/10.1007/s40429-020-00293-0. Narrative review of neuroimaging studies in food addiction.
• Gordon EL, Lent MR, Merlo LJ. The effect of food composition and behavior on neurobiological response to food: a review of recent research. Curr. 2020;9(2):75–82. Review of neurimaging studies and eating behaviour.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1–9.
Handu D, Moloney L, Wolfram T, Ziegler P, Acosta A, Steiber A. Academy of nutrition and dietetics methodology for conducting systematic reviews for the evidence analysis library. J Acad Nutr Diet. 2016;116(2):311–8. https://doi.org/10.1016/j.jand.2015.11.008.
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12(1):55–61. https://doi.org/10.1002/jrsm.1411.
Cohen J. Statistical power analysis for the behavioral sciences. Academic press; 2013.
Gearhardt AN, Yokum S, Orr PT, Stice E, Corbin WR, Brownell KD. Neural correlates of food addiction. Arch Gen Psychiatry. 2011;68(8):808–16.
Feldstein Ewing S, Claus E, Hudson K, Filbey F, Yakes Jimenez E, Lisdahl K, et al. Overweight adolescents’ brain response to sweetened beverages mirrors addiction pathways. Brain imaging behav. 2017;11(4):925–35.
Hardee J, Gearhardt A, Cope LM, Zucker R, Heitzeg M. Reduced precuneus activation in adolescents at risk for food addiction. Drug Alcohol Depend. 2017;171:e82.
Hsu JS, Wang PW, Ko CH, Hsieh TJ, Chen CY, Yen JY. Altered brain correlates of response inhibition and error processing in females with obesity and sweet food addiction: a functional magnetic imaging study. Obes Res Clin Pract. 2017;11(6):677–86.
Pursey KM, Contreras-Rodriguez O, Collins CE, Stanwell P, Burrows TL. Food addiction symptoms and amygdala response in fasted and fed states. Nutrients. 2019;11(6):06.
Romer AL, Su Kang M, Nikolova YS, Gearhardt AN, Hariri AR. Dopamine genetic risk is related to food addiction and body mass through reduced reward-related ventral striatum activity. Appetite. 2019;133:24–31.
Schulte EM, Yokum S, Jahn A, Gearhardt AN. Food cue reactivity in food addiction: a functional magnetic resonance imaging study. Physiol Behav. 2019;208:112574.
Ding Y, Ji G, Li G, Zhang W, Hu Y, Liu L, et al. Altered interactions among resting-state networks in individuals with obesity. Obesity. 2020;28(3):601–8.
Dong TS, Gupta A, Jacobs JP, Lagishetty V, Gallagher E, Bhatt RR, et al. Improvement in uncontrolled eating behavior after laparoscopic sleeve gastrectomy is associated with alterations in the brain–gut–microbiome axis in obese women. Nutrients. 2020;12(10):1–16.
Contreras-Rodriguez O, Burrows T, Pursey KM, Stanwell P, Parkes L, Soriano-Mas C, et al. Food addiction linked to changes in ventral striatum functional connectivity between fasting and satiety. Appetite. 2019;133:18–23.
Ravichandran S, Bhatt RR, Pandit B, Osadchiy V, Alaverdyan A, Vora P, et al. Alterations in reward network functional connectivity are associated with increased food addiction in obese individuals. Sci Rep. 2021;11(1):3386.
Hardee JE, Phaneuf C, Cope L, Zucker R, Gearhardt A, Heitzeg M. Neural correlates of inhibitory control in youth with symptoms of food addiction. Appetite. 2020;148:104578.
Rolls ET, Cheng W, Feng J. The orbitofrontal cortex: reward, emotion and depression. Brain Commun. 2020;2(2):fcaa196.
De Araujo IE, Rolls ET. Representation in the human brain of food texture and oral fat. J Neurosci. 2004;24(12):3086–93.
Sun X, Kroemer NB, Veldhuizen MG, Babbs AE, Araujo IE, Gitelman DR, et al. Basolateral amygdala response to food cues in the absence of hunger is associated with weight gain susceptibility. J Neurosci. 2015;35(20):7964–76.
McLaughlin RJ, Floresco SB. The role of different subregions of the basolateral amygdala in cue-induced reinstatement and extinction of food-seeking behavior. Neuroscience. 2007;146(4):1484–94.
Campbell EJ, Barker DJ, Nasser HM, Kaganovsky K, Dayas CV, Marchant NJ. Cue-induced food seeking after punishment is associated with increased Fos expression in the lateral hypothalamus and basolateral and medial amygdala. Behav Neurosci. 2017;131(2):155–67.
Wu M, Brockmeyer T, Hartmann M, Skunde M, Herzog W, Friederich HC. Reward-related decision making in eating and weight disorders: a systematic review and meta-analysis of the evidence from neuropsychological studies. Neurosci Biobehav Rev. 2016;61:177–96.
Shen KK, Welton T, Lyon M, McCorkindale AN, Sutherland GT, Burnham S, et al. Structural core of the executive control network: a high angular resolution diffusion MRI study. Hum Brain Mapp. 2020;41(5):1226–36.
Tuulari JJ, Karlsson HK, Hirvonen J, Salminen P, Nuutila P, Nummenmaa L. Neural circuits for cognitive appetite control in healthy and obese individuals: an fMRI study. PLoS One. 2015;10(2):16.
Kishinevsky FI, Cox JE, Murdaugh DL, Stoeckel LE, Cook EW, Weller RE. fMRI reactivity on a delay discounting task predicts weight gain in obese women. Appetite. 2012;58(2):582–92.
McMaster CM, Franklin J, Hart M, Matthews-Rensch K, Pursey K, Hart S (2023) The role of the dietitian. In: Patel VB, Preedy VR (eds) Eating Disorders. Cham: Springer. https://doi.org/10.1007/978-3-031-16691-4_92.
Pursey KM, Davis C, Burrows TL. Nutritional aspects of food addiction. Curr Addict Rep. 2017;4(2):142–50.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions This work was supported by the School of Health Sciences Pilot Grant, University of Newcastle (KMP).
Author information
Authors and Affiliations
Contributions
Conceptualization KMP; Data curation KMP KB SY; Formal analysis KMP; Methodology KMP TB; Roles/Writing - original draft KMP; Writing - review & editing KB SY TB.
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare no competing interests.
Human Rights and Informed Consent
Informed consent was not required as part of this project as it is a systematic review.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pursey, K.M., Yokum, S., Brain, K. et al. Neural Responses in Addictive Eating: a Systematic Review. Curr Addict Rep 11, 173–190 (2024). https://doi.org/10.1007/s40429-023-00538-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-023-00538-8