Abstract
Purpose of Review
Food addiction (FA) has been found to be associated with impulsivity, mainly urgency (negative and positive) and lack of perseverance. The present systematic review aimed to identify differences in impulsivity by gender and current implications of treatment regarding FA and impulsivity in clinical populations. The search was conducted in PubMed, Scopus, and Web of Science (WOS) databases, using the following search terms: “food addiction” and “impuls*.” Studies were included if they were written in English, had an observational design (e.g., cross-sectional, longitudinal, case-control), and used a quantitative methodology, without a limited search period to avoid selection bias.
Recent Findings
We included twenty-nine articles that aimed to examine whether there is a relationship between FA and impulsivity in clinical populations. Looking at gender differences, attentional and motor impulsivity were found to be related to FA in samples of women with obesity, whereas in the only study in a sample of men with obesity, cognitive and non-planning impulsivity appeared to be more associated with FA. Moreover, we identified three studies on the effects of interventions which included motivational, psychosocial, nutritional, and mindfulness components to address impulsivity and FA in cohorts with overweight/obesity and with substance use disorder (SUD). While some studies reported decreased levels of impulsivity, in other studies only FA decreased, and only one study showed significant changes in both FA and impulsivity after treatment.
Summary
Further research is needed to better understand the association between impulsivity and FA. Specifically, more studies with male populations could provide further evidence on how to better tailor treatment designs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Impulsivity is a multidimensional construct which describes how an individual reacts to urges and stimuli present in their environment [1], the primary focus being on obtaining a positive reward without adequate deliberation of any potential negative consequences [2, 3]. There are two prevailing models relating to trait impulsivity in the literature: Barratt (1959, 1995) [4, 5] and Whiteside and Lynam (2001) [6]. The former can be assessed by means of a self-report scale with various adaptations: the BIS-11 and BIS-15 [4, 7] assess three traits of impulsivity: (1) motor impulsivity, characterized by acting without thinking (including lack of perseverance as the tendency to give up a task, especially when it appears difficult or boring) [4, 8]; (2) attentional/cognitive impulsivity, linked to an inability to maintain focused attention and associated with rapid decision making [9••, 10]; and (3) non-planning impulsivity, characterized by a lack of planning for the future (including dimensions of self-control and cognitive complexity) [4, 10]. Both scales also include a total score. The BIS-brief scale or BIS-8 [11] includes 8 of the original BIS-11 items. The second model (UPPS-P) entails a multidimensional measure addressing five impulsive dispositions consisting of (1) urgency, a predisposition to strong impulses which may come along with negative affect, (2) lack of premeditation, the trouble recognizing potential consequences of a situation or action prior to proceeding to it, (3) lack of perseverance, the incapacity of staying focused on an arduous task, (4) sensation seeking, i.e., participating in precarious novel or stimulating activities, and lastly (5) positive urgency, a dimension that was added later and relates to having strong responses in highly positive emotional settings [12]. When examining the literature, higher rates of impulsivity have been linked to obesity and eating disorders (EDs) such as bulimia nervosa (BN) and binge-eating disorder (BED) [13], which, in turn, have a higher likelihood of comorbidity with substance use disorders (SUDs) as well as behavioral addictions [14•, 15•].
Additionally, over the years, one concept which has been viewed as rather similar to both EDs and addictive patterns, is that of food addiction (FA) [16, 17]. Until now, FA has not been labeled as a formal clinical diagnosis according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). However, the SUD criteria from the DSM-5 are implemented to determine whether or not an individual has FA [18, 19]. FA is marked by excessive overeating of high caloric foods with a loss of control and intense food cravings [20]. The self-report instrument which is used to determine FA using the DSM-5 criteria is the Yale Food Addiction Scale 2.0 (YFAS), which was created to offer a validated questionnaire for addictive-like eating behaviors [21]. Studies have shown that individuals with higher YFAS scores are also more impulsive, especially in terms of negative urgency, motor impulsivity, and a lack of perseverance [13, 22]; these traits are also found in individuals with obesity [23,24,25]. Additionally, there are also other adaptations of this scale, the mYFAS 2.0 (short version), and YFAS-C (version for children) [26, 27]. However, due to the fact that FA is mainly based on how individuals identify themselves and is assessed by the YFAS in mostly cross-sectional studies, there is growing concern about how this may limit the understanding of causality inferences between FA and other constructs such as impulsivity [28]. Perhaps longitudinal studies could help to further clarify the concept of FA and its associations with other parameters.
FA has been found to be present in both ED and SUD groups and might represent more than solely intense food and substance cravings in these individuals; studies have demonstrated the involvement of the mesolimbic dopamine pathway, the reward circuit of the brain, leading to the inability to suppress impulses to consume high fat, high refined sugar foods [16, 29,30,31,32,33,34]. Furthermore, animal models have associated the excessive consumption of sugar to tolerance, withdrawal, and continued use despite negative consequences [35,36,37,38,39]. Given these phenotypical similarities between SUD and FA, it has been hypothesized that personality traits like impulsivity–often described as an underlying mechanism of addictive patterns–may also be linked to FA. Impulsivity has been examined in various studies along with FA [1, 9••, 13].
The concepts of “urgency” (negative and positive, i.e., emotional impulsivity, tendency to act suddenly when experiencing extreme emotions) [40] and “lack of perseverance” (i.e., cognitive impulsivity, inability to sustain attention and motivation to complete tasks) [1, 22, 41, 42] have been described as relevant in the context of FA in several studies. Thus, individuals with FA may be more likely to act instantaneously by choosing immediate gratification with food rather than waiting, especially in situations of inconsistency between their personal needs and the present condition [1, 13, 32, 43, 44]. Difficulties in regulating negative (or positive) emotional states cause food intake, with impulsivity being the mediator of this link in individuals with FA [13]. This facet of trait impulsivity in individuals with FA could be related to low inhibitory control, which refers to the incapacity to suppress inadequate or undesirable behaviors [45]. However, studies have yielded mixed results regarding trait impulsivity and inhibitory control, especially in terms of concurrent FA [46].
Moreover, some studies have recognized gender differences regarding FA. For example, a study investigating FA in adults reported that women were significantly more likely to show FA traits than men (24.4% vs. 13.3%) and 3.65 times more likely to have severe FA [47]. Gender differences have also been related to impulsivity. A meta-analysis reported that men are more impulsive than women and more likely to present psychopathologies characterized by impulsive behaviors [48]. This meta-analysis also found differences between cognitive impulsivity in men and women using the BIS-11 scale, indicating that men had greater difficulty concentrating and focusing their attention. On the non-planning subscale of the BIS-11, men also reported a lower tendency to engage in future planning. Similarly, the same analysis found that men tend to experience greater sensation seeking and take more risks compared to women. Given these findings, it might be expected that such gender differences in impulsivity may also reflect onto the relationship between impulsivity and FA. In Parkinson’s disease, e.g., women who exhibit greater attentional impulsivity are more likely to also have FA compared to men [49••].
Although research has begun to investigate the relationship between FA and impulsivity, studies that include gender aspects are lacking. The predominantly female samples in most studies may hinder observations regarding gender differences. These differences are important to better understand the underlying potential causes of FA, how it may manifest differently between genders, and how these factors are linked to impulsivity. Likewise, additional evidence is missing regarding non-planning and motor impulsivity. Some scales of impulsivity (e.g., BIS-11) include these aspects, but no associations have been made with FA so far. Considering the various phenotypes of impulsivity, it is important to delineate their distinct impact, especially in co-occurrence with FA.
Previous studies [50, 51•] have reported possible mechanisms related to FA, impulsivity, and reward sensitivity. This review not only extends the work of Loxton (2018) and Maxwell et al. (2020) but also focuses on the clinical implications of impulsivity and FA. Additionally, this review aimed to identify differences in impulsivity and FA by gender.
Methods
Search Parameters
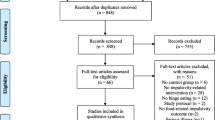
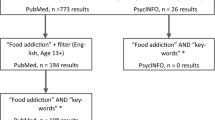
The methodology employed in this review adheres to principles of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [52]. The bibliographic search was carried out through the databases PubMed, Scopus, and Web of Science (WOS), using the following search terms: “food addiction” AND “impuls*” and filtered by title and abstract (food addiction [Title/Abstract]) AND (impuls*[Title/Abstract]). The bibliographic search was carried out between February 13 and 14, 2023.
Study Selection
The only studies considered for inclusion were the ones written in English with an observational design (e.g., cross-sectional, longitudinal, case-control) and a quantitative methodology, without a limited search period to avoid selection bias. Articles with no abstract, as well as publications that were not full articles, that had a qualitative design, or were literature reviews, books, dissertations, case reports or series, editorials, commentaries, systematic reviews, and narrative reviews were excluded. Special interest was given to those studies that used any version of the Yale Food Addiction Scale (YFAS) for the assessment of FA in clinical populations and the administration of at least one psychometric instrument to assess the presence of impulsivity. Only articles that aimed to search for a relationship between FA and impulsivity in a clinical population were included.
Once duplicate results were excluded, all abstracts were screened for inclusion and exclusion criteria. For all studies identified for inclusion, a full text version was retrieved, and all studies were reviewed regarding their quality and eligibility for this review. The exclusion criteria for these studies were documented. Subsequently, included studies were read thoroughly, and the former defined measures were extracted in tables.
Study Assessment and Data Extraction
The complete screening process was carried out using the COVIDENCE software, based on the PRISMA standards and recommended by Cochrane Reviews [53]. The article selection process was carried out in two steps. First, two reviewers (CBR and AGP) screened titles and abstracts of all potential studies individually. In the second phase of the screening and in accordance with the eligibility criteria, two different authors (AS and AGP) performed a detailed review of the full text of the identified articles. Differences in ratings between both reviewers were resolved through consensus, with the assistance of a third reviewer (LMG).
A total of 274 original articles were identified from the selected databases. A total of 119 duplicate articles were eliminated. Then, 110 articles were excluded based on title and abstract. In the next step, the full text of 45 articles was examined, 16 of which were excluded based on the following criteria: no reported associations between FA and impulsivity, not relevant to FA, non-clinical samples. Finally, 29 articles were included in this review (Fig. 1).
Risk of Bias Assessment
The risk of bias and the quality of the articles included in this review were assessed using the Newcastle-Ottawa Scale (NOS) [54], developed by the Cochrane Collaboration [55]. The face/content validity of the NOS has been established based on a critical review of the items by several experts in the field who evaluated its clarity and completeness for the specific task of assessing the quality of studies to be used in a meta-analysis [54].
This scale assigns up to a maximum of nine points for the least risk of bias in three domains: (1) selection of study groups (four points); (2) comparability of groups (two points); and (3) ascertainment of exposure and outcomes (three points) for case-control and cohort studies, respectively [54].
Results
Study Characteristics
The 29 studies included had a cross-sectional design, and two studies [56••, 57••] additionally included a longitudinal design. One study included men only [58], five studies included women only [19, 59, 60, 61••, 62••], and the rest had varying percentages of men and women, with the percentage of women being higher in most cases. Studies were primarily from developed countries, with most conducted in Germany (n = 7, 24.1%) [19, 63,64,65,66,67, 68••] and Spain (n = 4, 13.9%) [13, 56••, 58, 69••, 70]. Only eleven articles (37.93 %) included a control group [19, 49••, 56••, 57••, 58,59,60, 63, 71, 72, 73••].
The majority of studies enlisted samples with obesity (n = 12, 41.3%) [29, 56••, 57••, 58,59,60, 62••, 63, 68••, 72, 74, 75]. Furthermore, five studies (17.24%) included cohorts with ED [9••, 13, 61••, 69••, 70], only one study (3.4%) included individuals with obesity and ED [63], 6 studies (20.6%) included patients undergoing bariatric surgery [64, 65, 67, 73••, 75, 76], and two studies (7.4%) included adolescents with obesity [66, 77]. There was one study (3.7%) in patients with type 2 diabetes [78] and one study (3.4%) that included individuals with Parkinson’s disease [49••]. With regard to substance use, three studies (10.3%) were identified [57••, 69••, 70] (Table 1).
Assessment of Impulsivity and FA and Their Associations
Trait Impulsivity
In this review, the instruments most commonly used to quantify impulsive personality traits and study their association with FA were the Barratt Impulsivity Scale (BIS) [4] and the UPPS-P Impulsive Behavior Scale [6].
Most of the studies in this review (n = 12, 41.3%) assessed impulsivity using the BIS-11 [9••, 29, 49••, 58,59,60, 71, 72, 73••, 74, 75, 78]; six studies (20.6%) used the short version with 15 items (BIS-15) [19, 64,65,66,67, 68••], and only one study used the BIS-8 scale [76]. The results showed that four of the studies recorded significant positive associations between BIS total score and FA [19, 29, 60, 73••], while two studies, using the BIS-11 scale, did not find associations between FA and impulsivity levels [9••, 75]. The motor impulsivity subscale and the subscale of attentional impulsivity were the measures most frequently associated with FA [65,66,67, 71, 72, 74]. A study reported that FA and cognitive/attentional impulsivity interactively predicted alcohol use [65]. Non-planning impulsivity was associated with FA in patients with Parkinson’s disease, and was also identified as a cross-sectional predictor of BMI in patients with type 2 diabetes [78]. In another study which applied the Brief Self-Control Scale (BSCS) [72], the group with FA reported significantly greater disturbances with regard to impulsivity and self-control compared to the control group.
Eight studies (27.5%) used the UPPS-P scale [13, 56••, 61••, 62••, 69••, 70, 77]. Negative urgency and lack of perseverance showed significant associations with FA [13, 56••, 62••, 69••, 70]. One study reported that lack of premeditation, sensation seeking, and positive urgency may be predictors for developing one or two addictive behaviors [69••]. Another study found that high scores in negative urgency and reward dependency but low scores in lack of premeditation may increase the likelihood of FA [70].
Another scale used to evaluate personality profiles was the Personality and Risk Profiles Scale (SURPS), with the least frequent personality profile being the impulsive one. This instrument was applied in one of the three treatment studies included in this review. However, no changes in impulsivity scores were reported after the three-session intervention (brief motivational interview) [57••].
Neurocognitive Measures of Impulsivity
Based on cognitive and behavioral models of impulsivity, objective tests have been developed to measure inhibitory control processes using tasks that assess performance in terms of accuracy and reaction time data. These neurocognitive measures for assessing impulsivity are (1) measures of response inhibition. These are based on the suppression of a prepotent or dominant automatic response. The most commonly used behavioral or laboratory tests to assess this component are the Go/No-Go (GNG) Task and the Stroop Colour and Word Test [79, 80]. In this review, two studies included the GNG [60, 63], but only one of these studies reported significant differences in the FA group, indicating that the group with obesity and sweet food addiction (O&SFA) had a tendency to make more incorrect No-Go responses compared to the control group and to have a higher perceived difficulty in the task than the control group [60]. (2) Measures of delay-discounting: in these, impulsivity is mirrored by the preference for a small reward (available immediately or after a short delay) over a larger reward available at some future point in time [79, 81]. Two studies included the delay discounting task (DDT) [29, 63] and one of these studies also included the delay of gratification task [29], but only in one study the participants with FA reported higher impulsivity and showed poorer performances in the delay of gratification and delay discounting tasks [29]. In a similar realm, another study assessed impulsivity using the Food Related Inhibitory Control (FRIS) and the Impulsive Eating Behavior Interference subscale (FEV_In) [68••] and found negative associations between FA symptom severity and the subscales action withdrawal, action cancelation, reward sensitivity, and delay discounting of the FRIS. (3) Measures of cognitive impulsivity, referring to impulsive decision making behavior: in these tasks, subjects may select between a conservative option and a riskier option that offers a gain [82]. Such measures include the Iowa Gambling Task (IGT), the Cambridge Gamble Task (CGT), the Risky Gains Task (RGT), the CPT Conner's Continuous Performance Test, and the Trail Making Test [79, 83,84,85,86]. Two studies used the IGT [56••, 63] and one of these studies also utilized the CPT [56••]; no impact in executive functioning among individuals with FA was found.
Assessment of FA
The most widely used scale to measure FA has been the Yale Food Addiction Scale (YFAS). This scale was developed in 2009 by Gearhardt, Corbin, and Brownell, showing adequate internal reliability as well as good convergent and discriminant validity [20]. This self-report questionnaire examines eating behaviors during the past 12 months. The DSM-IV criteria for substance dependence were taken as a basis for the development of the items and were adapted to the consumption of foods rich in fats and sugars. Using this measure, FA can be assessed as a continuous variable (symptom count) and as a categorical variable (presence or absence of FA), and a “diagnosis” of FA is established if a person reports three or more symptoms in the past 12 months with clinically significant distress or impairment [87]. Currently, there are several translations of the YFAS, including the newer version YFAS 2.0 adapted to consider changes in the fifth edition of the DSM (DSM-5; measures of severity and craving) [21]. The YFAS 2.0 contains 35 questions that assess the 11 criteria of SUD. Abbreviated forms of the YFAS are the mYFAS [26] and the YFAS-C (version for children) [27].
In this review, FA was assessed using the Yale Food Addiction Scale (YFAS) in most studies (n = 16, 55.1%). One study used the Yale Food Addiction Scale for Children (YFAS-C) [77], and another study in participants with Parkinson’s disease used 2 items from the DSM-5 criteria to assess FA symptoms (food often consumed in larger amounts or over a longer period or more frequently than was intended; and craving, or a strong desire or urge to eat specific foods) [49••]. The rest of the studies used the YFAS 2.0 (37.9%). One study used the Food Cravings Questionnaire-Trait (FCQ-T) as a complement to FA assessment [88]. Finally, only one study used two different instruments in the assessment of FA; mYFAS at baseline and the YFAS 2.0 at the end of treatment [57••].
Impulsivity and Gender Differences
Only one article evaluated the relationship between FA and impulsivity in a 100% male sample [58] of individuals with obesity. Three further articles were identified that included a majority of men (10.3%) [49••, 56••, 88]. The majority of the studies (n = 12, 41.3%) had a higher percentage of women, and five articles (17.2%) [19, 59, 60, 61••, 62••] had 100% female cohorts.
In men, associations between FA and cognitive impulsivity, greater lack of planning, and weaker impulse control performance were found [58]. In the studies that had a higher percentage of men in their sample, FA was found to play a mediating role between impulsivity and BMI [56••]. One study did not detect FA in men [49••], while in another study, FA and impulsivity were not associated with the male gender [88].
In women, FA was associated with greater attentional and motor impulsivity, especially in women with obesity undergoing bariatric surgery. One study reported that high attentional impulsivity scores increased the risk for FA [49••]. The results of a study reporting gender differences showed that women were 6.7 times more likely to exhibit FA than men [73••]. In patients with Parkinson’s disease, FA was associated with the female gender and impulsivity (higher attentional non-planning factor) [49••]. In women with ED, negative urgency had a significant association with FA [13, 62••, 69••, 70].
Treatment
Three studies evaluated the effectiveness of an intervention and assessed both FA and impulsivity outcomes [56••, 57••, 88]. Two controlled studies included a cohort with overweight and obese individuals and a 3-month [57••] and 1-year follow-up [56••]. The third study conducted an intervention in participants with SUD without follow-ups [88]. Table 2 displays treatment approaches and intervention components that were different in each of the 3 studies.
The study by Mallorquí-Bagué et al. [54] aimed to investigate whether overweight/obesity was related to increased impulsivity, FA, and depressive symptoms, and whether these variables could be modified following a multimodal intervention based on a traditional Mediterranean diet (energy restricted), the promotion of physical activity and psychosocial (behavioral-motivational) support. This study was the only one of the treatment studies that performed a randomization of participants to intervention and control groups. The results showed that higher levels of impulsivity were related to higher FA. Multiple regression analysis and path analysis (a special case of structural equation modeling: SEM) revealed FA to play a mediating role between impulsivity and BMI. After 1 year of treatment, patients in both groups (intervention and control) reported a significant decrease in BMI and FA, along with significant tendencies in decreases of different characteristics of impulsivity (i.e., trait impulsivity and inhibitory control)–with further decreases in patients in the intervention group. Also, lack of perseverance and negative urgency were related to obesity/overweight through the presence of FA. Among the most important observations and conclusions of this study was the modifiable nature of FA and BMI in part through the improvement of impulsivity characteristics. The study also highlighted the usefulness of an intensive multimodal intervention (promoting a healthy dietary pattern such as the Mediterranean diet, physical activity, and behavioral-motivational support).
The FoodFix intervention in the study by Burrows et al. [68••] was designed as a brief motivational interview (of three sessions) to improve dietary profiles. This interview was developed and modeled according to a previous efficacious intervention for alcohol addiction, adapting its content to the dominant personality profile following a baseline assessment. Session content and structure were centered around the social cognitive theory (SCT) and the acceptance and commitment therapy (ACT). After the intervention, changes in individual symptoms of FA and in dietary intakes were found for both the intervention and control group; there were no changes in BMI over time. Because participants did not present an impulsive profile to begin with, no changes in impulsivity were reported. The intervention design was based on principles from the addiction research field, in which brief interventions are common.
The intervention by Koball et al. [88] was designed for participants with SUD and included group and individual therapy options with topics such as meditation, mindfulness, nutrition, and spirituality. In this study, no significant differences between pre- and post-treatment in scores measuring FA were found; however, impulsivity levels decreased following treatment. No change in the number of participants screening positive for FA emerged. A relevant finding of this study was that the BMI slightly (significantly) increased in the follow-up. The authors interpreted this result as a possible use of food as a substitute for abused substances; however, an artifact of abstinence from weight gain–promoting substances (e.g., alcohol or marijuana, the two most common substances used in this sample) could have also been a plausible explanation for the increase in BMI.
Risk of Bias Assessment
Only one multicenter randomized clinical trial [56••] and one randomized controlled trial were identified [57••]; the rest of the studies were cross-sectional. In addition, only 37.93% (n = 11) of the studies included a control group, including two of the three treatment studies [19, 49••, 56••, 57••, 58,59,60, 63, 71, 72, 73••]. Samples were generally individuals who were already diagnosed with an ED in a clinical setting or were preparing to receive bariatric surgery. Lack of control groups and aspects of selection bias were features of poor quality. Only a few (31%) of the studies were cross-sectional studies which had both a clinical and a control group with samples from hospital and community settings, thus showing good quality [19, 49••, 56••, 57••, 58,59,60, 72, 73••]. Two studies had a longitudinal design and a cross-sectional portion (case-control and cohort studies) with a good quality [56••, 88] (Tables 3 and 4).
Discussion
The current review focused on FA and impulsivity in clinical settings. The most commonly used instruments to measure impulsivity were the Barratt Impulsivity Scale (BIS) [4] and the UPPS-P Impulsive Behavior Scale [6]. The YFAS remains the most used measure to assess the presence and severity of FA. Most of the clinical samples were mainly women, with only one cohort consisting of men only [58]. This current research found that many studies included individuals with obesity, with or without FA. Looking at patients with an ED vs. ED and co-present FA, studies found that the comorbid groups had higher attentional and motor impulsivity than the groups with only ED [66, 73••, 74]. The results affirm the presence of a significant association between impulsivity and FA in clinical samples [19, 29, 60, 73••]. Negative urgency was identified as linked to FA, and like lack of perseverance, it showed significant associations with FA. Several studies have shown that negative urgency is one of the main features of impulsivity related to the development and maintenance of FA [32, 70], while lack of perseverance has been identified as relevant in addictive behaviors [89]. Results also show that motor impulsivity and attention impulsivity subscales were the measures most frequently associated with FA.
Although one of our objectives was to identify gender differences in impulsivity and its associations with FA, we were only able to identify four studies which included a majority of men [49••, 56••, 58, 88], and even fewer studies that analyzed gender differences. While attentional and motor impulsivity was related to FA in samples of women with obesity, the only study in men with obesity [58] found that, unlike women, cognitive and non-planning impulsivity was more closely associated with FA, which may indicate a specific clinical profile in men presenting with this association between impulsivity and FA. A meta-analysis reported similar results in identifying gender differences related to impulsivity; in that meta-analysis, men showed higher scores in cognitive/attentional and non-planning impulsivity than women. However, these results were reported in samples of the general population without FA [48].
Gender differences regarding FA and impulsivity have been studied independently (gender differences in FA have not been analyzed in relation to impulsivity before, while impulsivity has been studied in individuals without FA or showing other pathologies). The results presented here indicate that although the highest prevalence of FA is in women–with the largest samples in the studies included in this review consisting of women–men are also affected by FA. Little is known about the clinical manifestations of FA in men and putative differences to clinical manifestations of women with FA. Despite the evidence of differences in impulsivity between men and women, these differences have not yet been considered in recent studies on FA. There is scarcity of evidence regarding clinical correlates related to both FA and impulsivity; not only have very few treatment studies been conducted in individuals with FA including impulsivity as one of their treatment targets, but even the existing studies either lack the adequate power to identify statistical differences or have not included control groups. These observations warrant further investigations in larger samples including men, as this might have important implications for the design of treatments.
We were able to identify 3 studies addressing the effects of interventions on impulsivity and FA. Burrows et al. (2021) implemented a brief intervention with a focus on motivational interviewing (vs. control) in individuals with overweight and obesity. Both groups showed significant reductions in food addiction traits at the 3-month follow up; however, these changes were not significantly different between the groups. Mallorqui-Bagué et al. (2021) examined the effects of a psychosocial intervention (vs. control) on metabolic parameters, weight, dietary habits, and psychological variables in individuals with obesity and metabolic syndrome. After 1 year, participants in both groups reported significant decreases in BMI, FA, and impulsivity, although BMI decrease and impulsivity improvements were higher in the intervention group. The beneficial outcome on FA and impulsivity in the control group may provide evidence for the positive effects of unspecific interventions, thus those interventions that were not designed to specifically address impulsivity and food addiction. Although the actual intervention in this study was also not designed to specifically target FA and impulsivity, it may be assumed that psychosocial interventions of the kind that typically aim at modifying behaviors related to diet, physical activity, and stress management (e.g., by means of cognitive-behavioral approaches) most probably do address underlying psychological factors contributing to unhealthy eating behaviors and metabolic dysregulation, such as impulsivity and FA. Koball et al. (2009) aimed to investigate the phenomenon of addiction shift (which refers to the transition from substance addiction to FA) in individuals undergoing residential treatment for substance use. The results showed that scores for FA did not change following treatment–but the authors argued that scores were low at baseline to begin with. On the other hand, decreased scores in impulsivity were observed. These results are in somewhat contrast to those by Mallorqui-Bagué et al. (2021) and Burrows et al. (2021) in that they may be indicative of the fact that–despite the association and co-occurence of impulsivity and FA–the management of the two traits may need to be specifically targeted. This contrast may, hypothetically, be attributed to the different cohorts under investigation; Mallorqui-Bagué et al. (2021) and Burrows et al. (2021) examined individuals with overweight/obesity, while Koball et al. (2009) examined individuals with SUD (and low baseline scores in FA). The intervention per se (length, specific content, etc.) may also be of relevance, but this is another aspect that needs to be backed up by further evidence. For example, an integrated treatment approach that addresses both impulsivity and FA may be beneficial and could involve techniques from cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT) for emotion regulation or impulse control as well as interventions specifically targeting FA, such as psychoeducation about addictive-like eating behaviors and skills to manage cravings and triggers related to addictive eating.
Limitations and Future Research
This review has notable limitations. First, most of the studies were cross-sectional, which does not allow for causality considerations to be inferred, and most of the studies did not include a control group to allow conclusions of specificity and comparison of results. Then, several studies had unbalanced samples, with very low representation of men. The quality of most of the studies was low, which also made it difficult to identify gender differences. Additionally, studies were conducted in hospital settings, so their results cannot be generalized to different populations (e.g., the general population).
These findings demonstrate the need for longitudinal studies designed to achieve lower risk of bias. Future studies may improve methodological quality and specifically address gender differences, which is an understudied aspect in current research. Therefore, little is known about the clinical manifestations of impulsivity in men with FA. At the clinical level, such manifestations might have relevant implications for future treatment designs.
Conclusion
Understanding the relationship between impulsivity and FA may potentially inform treatment approaches and interventions. However, conclusive empirical data on the clinical significance of the co-existence of high impulsivity and distinct FA traits with regard to treatment outcomes (e.g., for individuals with problematic eating behaviors) is lacking. Further research is needed to better understand the clinical significance of the co-presence of impulsivity and FA traits and to evaluate the effectiveness of tailored treatment approaches in affected individuals. In the same sense, gender studies on the co-existence of impulsivity and FA should provide further evidence on how the bi-directional associations between impulsivity and FA may differ by gender.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
VanderBroek-Stice L, Stojek MK, Beach SRH, VanDellen MR, MacKillop J. Multidimensional assessment of impulsivity in relation to obesity and food addiction. Appetite. 2017;112:59–68. https://linkinghub.elsevier.com/retrieve/pii/S0195666316307541
Freimuth M, Moniz S, Kim SR. Clarifying exercise addiction: differential diagnosis, co-occurring disorders, and phases of addiction. Int J Environ Res Public Health. 2011;8:4069–81. http://www.mdpi.com/1660-4601/8/10/4069
Grant JE, Potenza MN. Compulsive aspects of impulse-control disorders. Psychiatr Clin North Am. 2006;29:539–51. https://linkinghub.elsevier.com/retrieve/pii/S0193953X06000153
Patton JH, Stanford MS, Barratt ES. Factor structure of the barratt impulsiveness scale. J Clin Psychol. 1995;51:768–74. https://onlinelibrary.wiley.com/doi/10.1002/1097-4679(199511)51:6%3C768::AID-JCLP2270510607%3E3.0.CO;2-1
Barratt ES. Anxiety and impulsiveness related to psychomotor efficiency. Percept Mot Skills. 1959;9:191–8. https://doi.org/10.2466/pms.1959.9.3.191.
Whiteside SP, Lynam DR. The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Pers Individ Differ. 2001;30:669–89. https://linkinghub.elsevier.com/retrieve/pii/S0191886900000647
Spinella M. Normative data and a short form of the Barratt Impulsiveness Scale. Int J Neurosci. 2007;117:359–68. https://doi.org/10.1080/00207450600588881.
Stanford MS, Mathias CW, Dougherty DM, Lake SL, Anderson NE, Patton JH. Fifty years of the Barratt Impulsiveness Scale: an update and review. Pers Individ Differ. 2009;47:385–95. https://linkinghub.elsevier.com/retrieve/pii/S0191886909001639
•• Tran H, Poinsot P, Guillaume S, Delaunay D, Bernetiere M, Bégin C, et al. Food Addiction as a proxy for Anorexia Nervosa severity: new data based on the Yale Food Addiction Scale 2.0. Psychiatry Res. 2020;293:113472. https://linkinghub.elsevier.com/retrieve/pii/S0165178120331334. Study included in the systematic review of FA and impulsivity.
Kotbagi G, Morvan Y, Romo L, Kern L. Which dimensions of impulsivity are related to problematic practice of physical exercise? J Behav Addict. 2017;6:221–8. https://akjournals.com/view/journals/2006/6/2/article-p221.xml
Steinberg L, Sharp C, Stanford MS, Tharp AT. New tricks for an old measure: the development of the Barratt Impulsiveness Scale–Brief (BIS-Brief). Psychol Assess. 2013;25:216–26. https://doi.org/10.1037/a0030550.
Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, Peterson C. Integration of impulsivity and positive mood to predict risky behavior: development and validation of a measure of positive urgency. Psychol Assess. 2007;19:107–18. https://doi.org/10.1037/1040-3590.19.1.107.
Wolz I, Granero R, Fernández-Aranda F. A comprehensive model of food addiction in patients with binge-eating symptomatology: the essential role of negative urgency. Compr Psychiatry. 2017;74:118–24. https://linkinghub.elsevier.com/retrieve/pii/S0010440X16305508
• Devoe DJ, Dimitropoulos G, Anderson A, Bahji A, Flanagan J, Soumbasis A, et al. The prevalence of substance use disorders and substance use in anorexia nervosa: a systematic review and meta-analysis. J Eat Disord. 2021;9:161. https://doi.org/10.1186/s40337-021-00516-3. Systematic review and meta-analysis of anorexia nervosa (AN) and substance use (SUD).
• Devoe DJ, Anderson A, Bahji A, Singh M, Patten SB, Soumbasis A, et al. The prevalence of impulse control disorders and behavioral addictions in eating disorders: a systematic review and meta-analysis. Front Psychiatry. 2022;12:724034. https://doi.org/10.3389/fpsyt.2021.724034/full. Meta-analysis on the comorbid prevalence of eating disorders (EDs), impulse control disorders (ICDs) and behavioral addictions (BAs).
Zhang H, Tong T, Gao Y, Liang C, Yu H, Li S, et al. Translation of the Chinese version of the modified Yale Food Addiction Scale 2.0 and its validation among college students. J Eat Disord. 2021;9:116. https://doi.org/10.1186/s40337-021-00471-z.
Hauck C, Cook B, Ellrott T. Food addiction, eating addiction and eating disorders. Proc Nutr Soc. 2020;79:103–12. https://www.cambridge.org/core/product/identifier/S0029665119001162/type/journal_article
Granero R, Hilker I, Agüera Z, Jiménez-Murcia S, Sauchelli S, Islam MA, et al. Food addiction in a Spanish sample of eating disorders: DSM-5 diagnostic subtype differentiation and validation data. Eur Eat Disord Rev. 2014;22:389–96. https://doi.org/10.1002/erv.2311.
de Vries S-K, Meule A. Food addiction and bulimia nervosa: new data based on the Yale Food Addiction Scale 2.0. Eur Eat Disord Rev. 2016;24:518–22. https://doi.org/10.1002/erv.2470.
Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale Food Addiction Scale. Appetite. 2009;52:430–6. https://linkinghub.elsevier.com/retrieve/pii/S0195666308006223
Gearhardt AN, Corbin WR, Brownell KD. Development of the Yale Food Addiction Scale Version 2.0. Psychol Addict Behav. 2016;30:113–21. https://doi.org/10.1037/adb0000136.
Murphy CM, Stojek MK, MacKillop J. Interrelationships among impulsive personality traits, food addiction, and body mass index. Appetite. 2014;73:45–50. https://linkinghub.elsevier.com/retrieve/pii/S0195666313004182
Nederkoorn C, Smulders FTY, Havermans RC, Roefs A, Jansen A. Impulsivity in obese women. Appetite. 2006;47:253–6. https://linkinghub.elsevier.com/retrieve/pii/S0195666306003874
Pepino MY, Finkbeiner S, Mennella JA. Similarities in food cravings and mood states between obese women and women who smoke tobacco. Obesity. 2009;17:1158–63. https://doi.org/10.1038/oby.2009.46.
Elfhag K, Morey LC. Personality traits and eating behavior in the obese: poor self-control in emotional and external eating but personality assets in restrained eating. Eat Behav. 2008;9:285–93. https://linkinghub.elsevier.com/retrieve/pii/S1471015307000852
Schulte EM, Gearhardt AN. Development of the Modified Yale Food Addiction Scale Version 2.0. Eur Eat Disord Rev. 2017;25:302–8. https://doi.org/10.1002/erv.2515.
Gearhardt AN, Roberto CA, Seamans MJ, Corbin WR, Brownell KD. Preliminary validation of the Yale Food Addiction Scale for children. Eat Behav. 2013;14:508–12. https://linkinghub.elsevier.com/retrieve/pii/S147101531300072X
Pursey K, Stanwell P, Gearhardt A, Collins C, Burrows T. The Prevalence of food addiction as assessed by the Yale Food Addiction Scale: a systematic review. Nutrients. 2014;6:4552–90. http://www.mdpi.com/2072-6643/6/10/4552
Davis C, Curtis C, Levitan RD, Carter JC, Kaplan AS, Kennedy JL. Evidence that ‘food addiction’ is a valid phenotype of obesity. Appetite. 2011;57:711–7. https://linkinghub.elsevier.com/retrieve/pii/S0195666311005617
Lindgren E, Gray K, Miller G, Tyler R, Wiers CE, Volkow ND, et al. Food addiction: a common neurobiological mechanism with drug abuse. Front Biosci-Landmark. 2018;23:811–36. https://doi.org/10.2741/4618.
Schulte EM, Avena NM, Gearhardt AN. Which foods may be addictive? The roles of processing, fat content, and glycemic load. PLoS One. 2015;10:e0117959. https://doi.org/10.1371/journal.pone.0117959.
Pivarunas B, Conner BT. Impulsivity and emotion dysregulation as predictors of food addiction. Eat Behav. 2015;19:9–14. https://linkinghub.elsevier.com/retrieve/pii/S1471015315000768
Volkow ND, Wang G-J, Baler RD. Reward, dopamine and the control of food intake: implications for obesity. Trends Cogn Sci. 2011;15:37–46. https://linkinghub.elsevier.com/retrieve/pii/S1364661310002470
Volkow ND, Wang G-J, Fowler JS, Telang F. Overlapping neuronal circuits in addiction and obesity: evidence of systems pathology. Philos Trans R Soc B Biol Sci. 2008;363:3191–200. https://doi.org/10.1098/rstb.2008.0107.
Avena NM, Long KA, Hoebel BG. Sugar-dependent rats show enhanced responding for sugar after abstinence: evidence of a sugar deprivation effect. Physiol Behav. 2005;84:359–62. https://linkinghub.elsevier.com/retrieve/pii/S0031938405000065
Berner LA, Avena NM, Hoebel BG. Bingeing, self-restriction, and increased body weight in rats with limited access to a sweet-fat diet. Obesity. 2008;16:1998–2002. https://doi.org/10.1038/oby.2008.328.
Hoebel BG, Avena NM, Bocarsly ME, Rada P. A behavioral and circuit model based on sugar addiction in rats. J Addict Med. 2009;3:33–41. https://journals.lww.com/01271255-200903000-00005
Hoebel BG, Rada PV, Mark GP, Pothos EN. Neural systems for reinforcement and inhibition of behavior: relevance to eating, addiction, and depression. In: Kahneman D, Diener E, Schwarz N, editors. Well-being Found hedonic Psychol. Russell Sage Foundation; 1999. p. 558–72.
Johnson PM, Kenny PJ. Dopamine D2 receptors in addiction-like reward dysfunction and compulsive eating in obese rats. Nat Neurosci. 2010;13:635–41. http://www.nature.com/articles/nn.2519
Mobbs O, Crépin C, Thiéry C, Golay A, Van der Linden M. Obesity and the four facets of impulsivity. Patient Educ Couns. 2010;79:372–7. https://linkinghub.elsevier.com/retrieve/pii/S0738399110001199
Rømer Thomsen K, Joensson M, Lou HC, Møller A, Gross J, Kringelbach ML, et al. Altered paralimbic interaction in behavioral addiction. Proc Natl Acad Sci. 2013;110:4744–9. https://doi.org/10.1073/pnas.1302374110.
Claes L, Islam MA, Fagundo AB, Jimenez-Murcia S, Granero R, Agüera Z, et al. The relationship between non-suicidal self-injury and the UPPS-P impulsivity facets in eating disorders and healthy controls. PLoS One. 2015;10:e0126083. https://doi.org/10.1371/journal.pone.0126083.
Gearhardt AN, White MA, Masheb RM, Morgan PT, Crosby RD, Grilo CM. An examination of the food addiction construct in obese patients with binge eating disorder. Int J Eat Disord. 2012;45:657–63. https://doi.org/10.1002/eat.20957.
Wenzel KR, Weinstock J, McGrath AB. The clinical significance of food addiction. J Addict Med. 2020;14:e153–9. https://doi.org/10.1097/ADM.0000000000000626.
Bartholdy S, Dalton B, O’Daly OG, Campbell IC, Schmidt U. A systematic review of the relationship between eating, weight and inhibitory control using the stop signal task. Neurosci Biobehav Rev. 2016;64:35–62. https://linkinghub.elsevier.com/retrieve/pii/S0149763415303092
Meule A, Lutz A, Vögele C, Kübler A. Women with elevated food addiction symptoms show accelerated reactions, but no impaired inhibitory control, in response to pictures of high-calorie food-cues. Eat Behav. 2012;13:423–8. https://linkinghub.elsevier.com/retrieve/pii/S1471015312000876
Burrows T, Hides L, Brown R, Dayas C, Kay-Lambkin F. Differences in dietary preferences, personality and mental health in Australian adults with and without food addiction. Nutrients. 2017;9:285. http://www.mdpi.com/2072-6643/9/3/285
Cross CP, Copping LT, Campbell A. Sex differences in impulsivity: a meta-analysis. Psychol Bull. 2011;137:97–130. https://doi.org/10.1037/a0021591.
•• de Chazeron I, Durif F, Lambert C, Chereau-Boudet I, Fantini ML, Marques A, et al. A case–control study investigating food addiction in Parkinson patients. Sci Rep. 2021;11:10934. https://www.nature.com/articles/s41598-021-90266-8. Study included in the systematic review that identifies gender differences between FA and impulsivity.
Loxton NJ. The role of reward sensitivity and impulsivity in overeating and food addiction. Curr Addict Reports. 2018;5:212–22. https://doi.org/10.1007/s40429-018-0206-y.
• Maxwell AL, Gardiner E, Loxton NJ. Investigating the relationship between reward sensitivity, impulsivity, and food addiction: a systematic review. Eur Eat Disord Rev. 2020;28:368–84. https://onlinelibrary.wiley.com/doi/10.1002/erv.2732. Previous systematic review of FA.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–12. https://linkinghub.elsevier.com/retrieve/pii/S0895435609001796
Kellermeyer L, Harnke B, Knight S. Covidence. J Med Libr Assoc. 2018;106. http://jmla.pitt.edu/ojs/jmla/article/view/513
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2003. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0. 2011. http://www.cochrane-handbook.org
•• Mallorquí-Bagué N, Lozano-Madrid M, Vintró-Alcaraz C, Forcano L, Díaz-López A, Galera A, et al. Effects of a psychosocial intervention at one-year follow-up in a PREDIMED-plus sample with obesity and metabolic syndrome. Sci Rep. 2021;11:9144. https://www.nature.com/articles/s41598-021-88298-1. Study included in the systematic review of treatment in FA and impulsivity.
•• Burrows T, Collins R, Rollo M, Leary M, Hides L, Davis C. The feasibility of a personality targeted intervention for addictive overeating: FoodFix. Appetite. 2021;156:104974. https://linkinghub.elsevier.com/retrieve/pii/S0195666320315968. Study included in the systematic review of treatment in FA and impulsivity.
Babaei S, Asgharnejad farid A, Lavasani F, Birashk B. Comparing impulse control and emotional regulation in patients with and without food addiction. Iran J Psychiatry Clin Psychol. 2017;23:22–37. http://ijpcp.iums.ac.ir/article-1-2435-en.html
ElNasser MO, ElRasheed AH, Azzam HMEE, ElZoheiry AK, ElSerafi DM, ElGhamry RH, et al. Personality profile and affect regulation in relation to food addiction among a sample of Egyptian females. Addict Disord Their Treat. 2016;15:143–8. https://journals.lww.com/00132576-201609000-00006
Hsu J-S, Wang P-W, Ko C-H, Hsieh T-J, Chen C-Y, Yen J-Y. Altered brain correlates of response inhibition and error processing in females with obesity and sweet food addiction: a functional magnetic imaging study. Obes Res Clin Pract. 2017;11:677–86. https://linkinghub.elsevier.com/retrieve/pii/S1871403X17300443
•• Fauconnier M, Rousselet M, Brunault P, Thiabaud E, Lambert S, Rocher B, et al. Food addiction among female patients seeking treatment for an eating disorder: prevalence and associated factors. Nutrients. 2020;12:1897. https://www.mdpi.com/2072-6643/12/6/1897. Study included in the systematic review with a complete sample of women.
•• Schulte EM, Gearhardt AN. Attributes of the food addiction phenotype within overweight and obesity. Eat Weight Disord - Stud Anorexia, Bulim Obes. 2021;26:2043–9. https://doi.org/10.1007/s40519-020-01055-7. Study included in the systematic review with a complete sample of women.
Blume M, Schmidt R, Hilbert A. Executive functioning in obesity, food addiction, and Binge-eating disorder. Nutrients. 2018;11:54. http://www.mdpi.com/2072-6643/11/1/54
Meule A, de Zwaan M, Müller A. Attentional and motor impulsivity interactively predict ‘food addiction’ in obese individuals. Compr Psychiatry. 2017;72:83–7. https://linkinghub.elsevier.com/retrieve/pii/S0010440X16303224
Meule A, Heckel D, Jurowich CF, Vögele C, Kübler A. Correlates of food addiction in obese individuals seeking bariatric surgery. Clin Obes. 2014;4:228–36. https://doi.org/10.1111/cob.12065
Meule A, Hermann T, Kübler A. Food Addiction in overweight and obese adolescents seeking weight-loss treatment. Eur Eat Disord Rev. 2015;23:193–8. https://doi.org/10.1002/erv.2355.
Meule A, Müller A, Gearhardt AN, Blechert J. German version of the Yale Food Addiction Scale 2.0: Prevalence and correlates of ‘food addiction’ in students and obese individuals. Appetite. 2017;115:54–61. https://linkinghub.elsevier.com/retrieve/pii/S0195666316305050
•• Pape M, Herpertz S, Schroeder S, Seiferth C, Färber T, Wolstein J, et al. Food addiction and its relationship to weight- and addiction-related psychological parameters in individuals with overweight and obesity. Front Psychol. 2021;12:736454. https://doi.org/10.3389/fpsyg.2021.736454/full. Study included in the systematic review of FA and impulsivity.
•• Miranda-Olivos R, Agüera Z, Granero R, Vergeer RR, Dieguez C, Jiménez-Murcia S, et al. Food addiction and lifetime alcohol and illicit drugs use in specific eating disorders. J Behav Addict. 2022;11:102–15. https://akjournals.com/view/journals/2006/11/1/article-p102.xml. Study included in the systematic review of participants with substance use (SUD), FA and impulsivity.
Wolz I, Hilker I, Granero R, Jiménez-Murcia S, Gearhardt AN, Dieguez C, et al. “Food addiction” in patients with eating disorders is associated with negative urgency and difficulties to focus on long-term goals. Front Psychol. 2016;7:61. http://journal.frontiersin.org/Article/10.3389/fpsyg.2016.00061/abstract
Brunault P, Ducluzeau P-H, Courtois R, Bourbao-Tournois C, Delbachian I, Réveillère C, et al. Food addiction is associated with higher neuroticism, lower conscientiousness, higher impulsivity, but lower extraversion in obese patient candidates for bariatric surgery. Subst Use Misuse. 2018;53:1919–23. https://doi.org/10.1080/10826084.2018.1433212.
Ivezaj V, White MA, Grilo CM. Examining binge-eating disorder and food addiction in adults with overweight and obesity. Obesity. 2016;24:2064–9. https://doi.org/10.1002/oby.21607.
•• Sönmez Güngör E, Çelebi C, Akvardar Y. The relationship of food addiction with other eating pathologies and impulsivity: a case-control study. Front Psychiatry. 2021;12:747474. https://www.frontiersin.org/articles/10.3389/fpsyt.2021.747474/full. Study included in the systematic review that identifies gender differences between FA and impulsivity.
Ceccarini M, Manzoni GM, Castelnuovo G, Molinari E. An evaluation of the Italian Version of the Yale Food Addiction Scale in obese adult inpatients engaged in a 1-month-weight-loss treatment. J Med Food. 2015;18:1281–7. https://doi.org/10.1089/jmf.2014.0188.
Rodrigue C, Ouellette A-S, Lemieux S, Tchernof A, Biertho L, Bégin C. Executive functioning and psychological symptoms in food addiction: a study among individuals with severe obesity. Eat Weight Disord - Stud Anorexia, Bulim Obes. 2018;23:469–78. https://doi.org/10.1007/s40519-018-0530-1.
Ouellette A-S, Rodrigue C, Lemieux S, Tchernof A, Biertho L, Bégin C. An examination of the mechanisms and personality traits underlying food addiction among individuals with severe obesity awaiting bariatric surgery. Eat Weight Disord - Stud Anorexia, Bulim Obes. 2017;22:633–40. https://doi.org/10.1007/s40519-017-0440-7.
Rose MH, Nadler EP, Mackey ER. Impulse control in negative mood states, emotional eating, and food addiction are associated with lower quality of life in adolescents with severe obesity. J Pediatr Psychol. 2018;43:443–51. https://academic.oup.com/jpepsy/article/43/4/443/4555058
Raymond K-L, Lovell GP. Food addiction symptomology, impulsivity, mood, and body mass index in people with type two diabetes. Appetite. 2015;95:383–9. https://linkinghub.elsevier.com/retrieve/pii/S0195666315003475
Verdejo-García A, Lawrence AJ, Clark L. Impulsivity as a vulnerability marker for substance-use disorders: review of findings from high-risk research, problem gamblers and genetic association studies. Neurosci Biobehav Rev. 2008;32:777–810. https://linkinghub.elsevier.com/retrieve/pii/S0149763408000067
Verbruggen F, Logan GD. Long-term aftereffects of response inhibition: memory retrieval, task goals, and cognitive control. J Exp Psychol Hum Percept Perform. 2008;34:1229–35. https://doi.org/10.1037/0096-1523.34.5.1229.
Reynolds B, Richards JB, de Wit H. Acute-alcohol effects on the experiential discounting task (EDT) and a question-based measure of delay discounting. Pharmacol Biochem Behav. 2006;83:194–202. https://linkinghub.elsevier.com/retrieve/pii/S0091305706000219
Kagan J. Reflection-impulsivity: the generality and dynamics of conceptual tempo. J Abnorm Psychol. 1966;71:17–24. https://doi.org/10.1037/h0022886.
Bechara A, Damasio AR, Damasio H, Anderson SW. Insensitivity to future consequences following damage to human prefrontal cortex. Cognition. 1994;50:7–15. https://linkinghub.elsevier.com/retrieve/pii/0010027794900183
Paulus MP, Rogalsky C, Simmons A, Feinstein JS, Stein MB. Increased activation in the right insula during risk-taking decision making is related to harm avoidance and neuroticism. Neuroimage. 2003;19:1439–48. https://linkinghub.elsevier.com/retrieve/pii/S1053811903002519
Rogers RD, Owen AM, Middleton HC, Williams EJ, Pickard JD, Sahakian BJ, et al. Choosing between small, likely rewards and large, unlikely rewards activates inferior and orbital prefrontal cortex. J Neurosci. 1999;19:9029–38. https://doi.org/10.1523/JNEUROSCI.19-20-09029.1999.
Conners CK, Sitarenios G. Conners’ Continuous performance test (CPT). In: Encycl Clin Neuropsychol. New York, NY: Springer New York; 2011. p. 681–3. https://doi.org/10.1007/978-0-387-79948-3_1535.
Penzenstadler L, Soares C, Karila L, Khazaal Y. Systematic review of food addiction as measured with the Yale Food Addiction Scale: implications for the food addiction construct. Curr Neuropharmacol. 2019;17:1–3. http://www.eurekaselect.com/167164/article
Koball AM, Glodosky NC, Ramirez LD, Kallies KJ, Gearhardt AN. From substances to food: an examination of addiction shift in individuals undergoing residential treatment for substance use. Addict Res Theory. 2019;27:322–7. https://doi.org/10.1080/16066359.2018.1516757.
Mallorquí-Bagué N, Vintró-Alcaraz C, Verdejo-García A, Granero R, Fernández-Aranda F, Magaña P, et al. Impulsivity and cognitive distortions in different clinical phenotypes of gambling disorder: profiles and longitudinal prediction of treatment outcomes. Eur Psychiatry. 2019;61:9–16. https://linkinghub.elsevier.com/retrieve/pii/S092493381930104X
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This manuscript and research were supported by grants from the Delegación del Gobierno para el Plan Nacional sobre Drogas (2021I031), Ministerio de Ciencia e Innovación (PDI2021-124887OB-I00), Instituto de Salud Carlos III (ISCIII) (FIS PI20/00132), and co-funded by FEDER funds/European Regional Development Fund (ERDF), a way to build Europe. CIBERObn is an initiative of ISCIII. The funders had no role in the study design, data collection, and analysis, decision to publish, or preparation of the manuscript. LCB was supported by Sara Borrell fellowship–CD22/00171–Instituto de Salud Carlos III (ISCIII) and co-founded by the European Union. MR is supported by a FI grant from the Catalan Agency for the Management of Grants for University - AGAUR (2020 FISDU 00579).
Author information
Authors and Affiliations
Contributions
AGP, GP, FFA, LM, and SJM contributed to the development of the study concept and design. RMO, LCB, CB, AS, and BP aided with data collection. AGP, MR, and GP wrote the original manuscript. FFA and SJM obtained funding. GP, FFA, and SJM revised the manuscript and provided substantial comments. All authors had full access to all study data.
Corresponding author
Ethics declarations
Ethics Approval
The present article is a systematic review of the literature and no studies with human participants or animals were performed by any of the authors to conduct this work.
Conflict of Interest
FFA and SJM received consultancy honoraria from Novo Nordisk and FFA editorial honoraria as EIC from Wiley. The rest of the authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gaspar-Pérez, A., Paslakis, G., Rosinska, M. et al. Food Addiction and Impulsivity in Clinical Populations by Gender: a Systematic Review. Curr Addict Rep 10, 793–816 (2023). https://doi.org/10.1007/s40429-023-00514-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-023-00514-2