Abstract
Purposeof the review
Chemsex mainly concerned men who have sex with men, but seems to spread in general population. Clinical characteristics and expected effects are diverse. This paper aims at reviewing existing literature on chemsex and providing treatment guidelines.
Recent findings
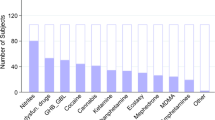
The use of substances for improving or extending sexual intercourses is commonly referred to as chemsex. Substances used are mainly methamphetamine, GHB/GBL, cocaine and cathinones. Prevalence is estimed between 3 and 42% of MSM. Risk factors are mainly living in a metropolis, using dating apps and practicing "hard-sex". Chemsex practice is not necessarily pathological and only the loss of control, the association with addictive, psychiatric and/or infectious comorbidities should require care.
Summary
Management of problematic chemsex should be multidisciplinary and must take into account psychiatric, addictive and infectious comorbidities. Information and education are crucial in order to reduce risks and potential harm associated to chemsex.
Similar content being viewed by others
References
Turner D, Briken P, Grubbs J, Malandain L, Mestre-Bach G, Potenza MN, et al. The World Federation of Societies of Biological Psychiatry guidelines on the assessment and pharmacological treatment of compulsive sexual behaviour disorder. Dialogues Clin Neurosci. 2022;24:10–69.
Stuart D. Chemsex: origins of the word, a history of the phenomenon and a respect to the culture. Drugs Alcohol Today. 2019;19:3–10.
Deimel D, Stöver H, Hößelbarth S, Dichtl A, Graf N, Gebhardt V. Drug use and health behaviour among German men who have sex with men: Results of a qualitative, multi-centre study. Harm Reduct J. 2016;13:36.
Bourne A, Reid D, Hickson F, Torres Rueda S, Weatherburn P, The Chemsex study: drug use in sexual settings among gay and bisexual men in Lambeth, Southwark and Lewisham. Technical Report. Sigma Research, London School of Hygiene & Tropical Medicine, London. 2014. https://researchonline.lshtm.ac.uk/id/eprint/2197245
Blomquist PB, Mohammed H, Mikhail A, Weatherburn P, Reid D, Wayal S, et al. Characteristics and sexual health service use of MSM engaging in chemsex: results from a large online survey in England. Sex Transm Infect. 2020;96:590–5.
Sewell J, Cambiano V, Speakman A, Lampe FC, Phillips A, Stuart D, et al. Changes in chemsex and sexual behaviour over time, among a cohort of MSM in London and Brighton: Findings from the AURAH2 study. Int J Drug Policy. 2019;68:54–61.
Edmundson C, Heinsbroek E, Glass R, Hope V, Mohammed H, White M, et al. Sexualised drug use in the United Kingdom (UK): A review of the literature. Int J Drug Policy. 2018;55:131–48.
Íncera-Fernández D, Gámez-Guadix M, Moreno-Guillén S. Mental Health Symptoms Associated with Sexualized Drug Use (Chemsex) among Men Who Have Sex with Men: A Systematic Review. Int J Environ Res Public Health. 2021;18:13299.
Hammoud MA, Vaccher S, Jin F, Bourne A, Haire B, Maher L, et al. The new MTV generation: Using methamphetamine, Truvada™, and Viagra™ to enhance sex and stay safe. Int J Drug Policy. 2018;55:197–204.
Drückler S, van Rooijen MS, de Vries HJC. Chemsex Among Men Who Have Sex With Men: a Sexualized Drug Use Survey Among Clients of the Sexually Transmitted Infection Outpatient Clinic and Users of a Gay Dating App in Amsterdam, the Netherlands. Sex Transm Dis. 2018;45:325–31.
Pakianathan M, Whittaker W, Lee MJ, Avery J, Green S, Nathan B, Hegazi A. Chemsex and new HIV diagnosis in gay, bisexual and other men who have sex with men attending sexual health clinics. HIV Med. 2018 May 22. https://doi.org/10.1111/hiv.12629
Hibbert MP, Brett CE, Porcellato LA, Hope VD. Psychosocial and sexual characteristics associated with sexualised drug use and chemsex among men who have sex with men (MSM) in the UK. Sex Transm Infect. 2019 Aug;95(5):342–50. https://doi.org/10.1136/sextrans-2018-053933
Frankis J, Clutterbuck D. What does the latest research evidence mean for practitioners who work with gay and bisexual men engaging in chemsex? Sex Transm Infect. 2017;93:153–4.
Maxwell S, Shahmanesh M, Gafos M. Chemsex behaviours among men who have sex with men: A systematic review of the literature. Int J Drug Policy. 2019;63:74–89.
Malandain L, Mosser S, Mouchabac S, Blanc J-V, Alexandre C, Thibaut F. Chemical sex (chemsex) in a population of French university students. Dialogues Clin Neurosci. 2021;23:39–43.
Glynn RW, Byrne N, O’Dea S, Shanley A, Codd M, Keenan E, et al. Chemsex, risk behaviours and sexually transmitted infections among men who have sex with men in Dublin. Ireland Int J Drug Policy. 2018;52:9–15.
Milhet M, Chemsex NT, slam. Renouvellement des usages de drogues en contextes sexuels parmi les HSH. Saint‐Denis: OFDT Théma TREND, 2017. Available from: https://bdoc.ofdt.fr/doc_num.php?explnum_id=24951.
Bui H, Zablotska-Manos I, Hammoud M, Jin F, Lea T, Bourne A, et al. Prevalence and correlates of recent injecting drug use among gay and bisexual men in Australia: Results from the FLUX study. Int J Drug Policy. 2018;55:222–30.
Lim SH, Akbar M, Wickersham JA, Kamarulzaman A, Altice FL. The management of methamphetamine use in sexual settings among men who have sex with men in Malaysia. Int J Drug Policy. 2018;55:256–62.
Schmidt AJ, Bourne A, Weatherburn P, Reid D, Marcus U, Hickson F, et al. Illicit drug use among gay and bisexual men in 44 cities: Findings from the European MSM Internet Survey (EMIS). Int J Drug Policy. 2016;38:4–12.
Léobon A, Dussault É, Otis J. « Chemsex » chez des hommes français ayant des relations sexuelles avec des hommes. Drogue Santé Société. 2018;17:53.
McCormack S, Dunn DT, Desai M, Dolling DI, Gafos M, Gilson R, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. The Lancet. 2016;387:53–60.
Rajasingham R, Mimiaga MJ, White JM, Pinkston MM, Baden RP, Mitty JA. A Systematic Review of Behavioral and Treatment Outcome Studies Among HIV-Infected Men Who Have Sex with Men Who Abuse Crystal Methamphetamine. AIDS Patient Care STDs. 2012;26:36–52.
Blanc J-V, Burdairon J-D, Malandain L, Ferreri F, Mouchabac S, Adrien A. Attachment and mental health of menhaving sex with men engaging in chemsex: is substance abuse only the tip of the iceberg? In Press.
Tan RKJ, Wong CM, Chen MI-C, Chan YY, Bin Ibrahim MA, Lim OZ, et al. Chemsex among gay, bisexual, and other men who have sex with men in Singapore and the challenges ahead: A qualitative study. Int J Drug Policy. 2018;61:31–7.
Weatherburn P, Hickson F, Reid D, Torres-Rueda S, Bourne A. Motivations and values associated with combining sex and illicit drugs (’chemsex’) among gay men in South London: findings from a qualitative study. Sex Transm Infect. 2017;93:203–6.
Ahmed A-K, Weatherburn P, Reid D, Hickson F, Torres-Rueda S, Steinberg P, et al. Social norms related to combining drugs and sex (“chemsex”) among gay men in South London. Int J Drug Policy. 2016;38:29–35.
Milhet M. APACHES - Attentes et PArcours liés au CHEmSex [Internet]. 2019. Available from: https://www.ofdt.fr/publications/collections/rapports/rapports-d-etudes/rapports-detudes-ofdt-parus-en-2019/apaches-attentes-et-parcours-lies-au-chemsex/
Tomkins A, George R, Kliner M. Sexualised drug taking among men who have sex with men: a systematic review. Perspect Public Health. 2019;139:23–33.
Antonio N, Diehl A, Niel M, Pillon S, Ratto L, Pinheiro MC. Sexual addiction in drug addicts: The impact of drug of choice and poly-addiction. Rev Assoc Médica Bras Mai. 2017;63:414–21.
Achterbergh RCA, Vries HJC, Boyd A, Davidovich U, Drückler S, Hoornenborg E, et al. Identification and characterization of latent classes based on drug use among men who have sex with men at risk of sexually transmitted infections in Amsterdam, the Netherlands. Addiction. 2020;115:121–33.
Pufall E, Kall M, Shahmanesh M, Nardone A, Gilson R, Delpech V. Sexualized drug use (“chemsex”) and high-risk sexual behaviours in HIV-positive men who have sex with men. HIV Med Avr. 2018;19:261–70.
Schecke H, Lea T, Bohn A, Köhler T, Sander D, Scherbaum N, Deimel D. Crystal Methamphetamine Use in Sexual Settings Among German Men Who Have Sex With Men. Front Psychiatry. 2019 Dec 6;10:886. https://www.frontiersin.org/article/10.3389/fpsyt.2019.00886/full.
Prestage G, Hammoud M, Jin F, Degenhardt L, Bourne A, Maher L. Mental health, drug use and sexual risk behavior among gay and bisexual men. Int J Drug Policy. 2018;55:169–79.
Batisse A, Eiden C, Deheul S, Monzon E, Djezzar S, Peyrière H. Chemsex practice in France: An update in Addictovigilance data. Fundam Clin Pharmacol. 2022;36:397–404.
Sewell J, Miltz A, Lampe FC, Cambiano V, Speakman A, Phillips AN, et al. Poly drug use, chemsex drug use, and associations with sexual risk behaviour in HIV-negative men who have sex with men attending sexual health clinics. Int J Drug Policy. 2017;43:33–43.
Hegazi A, Lee M, Whittaker W, Green S, Simms R, Cutts R, et al. Chemsex and the city: sexualised substance use in gay bisexual and other men who have sex with men attending sexual health clinics. Int J STD AIDS. 2017;28:362–6.
for the ANRS-Prevagay group, Vaux S, Chevaliez S, Saboni L, Sauvage C, Sommen C, et al. Prevalence of hepatitis C infection, screening and associated factors among men who have sex with men attending gay venues: a cross-sectional survey (PREVAGAY), France, 2015. BMC Infect Dis [Internet]. 2019 [cited 2019 Jun 25];19. Available from: https://www.bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-019-3945-z
Benyamina A. Rapport Chemsex 2022 pour le Ministre de la Santé [Internet]. 2022. Available from: https://www.vie-publique.fr/sites/default/files/rapport/pdf/284486.pdf
Pakianathan MR, Lee MJ, Kelly B, Hegazi A. How to assess gay, bisexual and other men who have sex with men for chemsex. Sex Transm Infect Déc. 2016;92:568–70.
Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction. 1993;88:791–804.
Carnes PJ, Green BA, Merlo LJ, Polles A, Carnes S, Gold MS. PATHOS: a brief screening application for assessing sexual addiction. J Addict Med. 2012;6:29–34.
Tiffany ST, Singleton E, Haertzen CA, Henningfield JE. The development of a cocaine craving questionnaire. Drug Alcohol Depend. 1993;34:19–28.
Khazaee-Pool M, Jahangiry L, Pashaei T, Ramezani-Badr F, Nadrian H, Ponnet K. Development and psychometric properties of the methamphetamine decisional balance scale (METH-DBS) for young adults. Subst Abuse Treat Prev Policy. 2018 Oct 29;13(1):38. https://www.substanceabusepolicy.biomedcentral.com/articles/10.1186/s13011-018-0175-0
Nutt D, King LA, Saulsbury W, Blakemore C. Development of a rational scale to assess the harm of drugs of potential misuse. The Lancet. 2007;369:1047–53.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders [Internet]. Fifth Edition. American Psychiatric Association; 2013 [cité 3 mai 2023]. Disponible sur: https://psychiatryonline.org/doi/book/10.1176/appi.books.9780890425596
Almeida MSC, Sousa Filho LF, Rabello PM, Santiago BM. International Classification of Diseases - 11th revision: from design to implementation. Rev Saude Publica. 2020 Nov 9;54:104. https://doi.org/10.11606/s1518-8787.2020054002120
Bydlowski L, Karila L. Risk and harm reduction practices related to chemsex and their direct application to users: a systematic review of the international literature. 2022 In Press;
Hofmann SG, Asnaani A, Vonk IJJ, Sawyer AT, Fang A. The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cogn Ther Res. 2012;36:427–40.
Beck AT. Cognitive therapy: nature and relation to behavior therapy - republished article. Behav Ther. 2016 Nov;47(6):776-84. https://doi.org/10.1016/j.beth.2016.11.003
Ellis A. Reason and emotion in psychotherapy. New York: Lyle Stuart; 1962.
Balandeh E, Omidi A, Ghaderi A. A Narrative Review of Third-Wave Cognitive-Behavioral Therapies in Addiction. Addict Health. 2021;13:52–65.
Morley KC, Cornish JL, Faingold A, Wood K, Haber PS. Pharmacotherapeutic agents in the treatment of methamphetamine dependence. Expert Opin Investig Drugs. 2017;26:563–78.
Ballester J, Valentine G, Sofuoglu M. Pharmacological treatments for methamphetamine addiction: current status and future directions. Expert Rev Clin Pharmacol. 2017;10:305–14.
Coffin PO, Santos G-M, Hern J, Vittinghoff E, Santos D, Matheson T. Extended-release naltrexone for methamphetamine dependence among men who have sex with men: a randomized placebo-controlled trial: Naltrexone for methamphetamine dependence. Addict Févr. 2018;113:268–78.
Stauffer CS, Moschetto JM, McKernan SM, Hsiang E, Borsari B, Woolley JD. Oxytocin-enhanced motivational interviewing group therapy for methamphetamine use disorder in men who have sex with men: study protocol for a randomized controlled trial. Trials. 2019 Feb 21;20(1):145. https://doi.org/10.1186/s13063-019-3225-7
Anderson AL, Li S-H, Markova D, Holmes TH, Chiang N, Kahn R, et al. Bupropion for the treatment of methamphetamine dependence in non-daily users: A randomized, double-blind, placebo-controlled trial. Drug Alcohol Depend. 2015;150:170–4.
Galloway GP, Newmeyer J, Knapp T, Stalcup SA, Smith D. A controlled trial of imipramine for the treatment of methamphetamine dependence. J Subst Abuse Treat. 1996;13:493–7.
Shoptaw S, Huber A, Peck J, Yang X, Liu J, Dang Jeff, et al. Randomized, placebo-controlled trial of sertraline and contingency management for the treatment of methamphetamine dependence. Drug Alcohol Depend. 2006;85:12–8.
Briones M, Shoptaw S, Cook R, Worley M, Swanson A-N, Moody DE, et al. Varenicline treatment for methamphetamine dependence: A randomized, double-blind phase II clinical trial. Drug Alcohol Depend. 2018;189:30–6.
Lam L, Anand S, Li X, Tse M, Zhao JX, Chan EW. Efficacy and safety of naltrexone for amfetamine and methamfetamine use disorder: a systematic review of randomized controlled trials. Clin Toxicol. 2019;57:225–33.
Siefried KJ, Acheson LS, Lintzeris N, Ezard N. Pharmacological Treatment of Methamphetamine/Amphetamine Dependence: A Systematic Review. CNS Drugs. 2020;34:337–65.
Galloway GP, Buscemi R, Coyle JR, Flower K, Siegrist JD, Fiske LA, et al. A Randomized, Placebo-Controlled Trial of Sustained-Release Dextroamphetamine for Treatment of Methamphetamine Addiction. Clin Pharmacol Ther. 2011;89:276–82.
Coffin PO, Santos G-M, Hern J, Vittinghoff E, Walker JE, Matheson T, et al. Effects of Mirtazapine for Methamphetamine Use Disorder Among Cisgender Men and Transgender Women Who Have Sex With Men: A Placebo-Controlled Randomized Clinical Trial. JAMA Psychiat. 2020;77:246.
Lev-Ran S. A Case of Treating Cathinone Dependence and Comorbid Depression Using Bupropion. J Psychoactive Drugs. 2012;44:434–6.
Habibian S, Ahamad K, McLean M, Socias ME. Successful management of gamma-hydroxybutyrate (GHB) withdrawal using Baclofen as a standalone therapy: a case report. J Addict Med. 2019 Sep/Oct;13(5):415-7. https://doi.org/10.1097/ADM.0000000000000514
Beurmanjer H, Kamal RM, de Jong CAJ, Dijkstra BAG, Schellekens AFA. Baclofen to Prevent Relapse in Gamma-Hydroxybutyrate (GHB)-Dependent Patients: A Multicentre, Open-Label, Non-Randomized. Controlled Trial CNS Drugs. 2018;32:437–42.
Wainberg ML, Muench F, Morgenstern J, Hollander E, Irwin TW, Parsons JT, et al. A double-blind study of citalopram versus placebo in the treatment of compulsive sexual behaviors in gay and bisexual men. J Clin Psychiatry. 2006;67:1968–73.
Malandain L, Blanc JV, Ferreri F, Thibaut F. Pharmacotherapy of sexual addiction. Curr Psychiatry Rep. 2020 May 7;22(6):30. https://www.link.springer.com/10.1007/s11920-020-01153-4
Malandain L, Blanc J-V, Ferreri F, Giorgiadis T, Mosser S, Mouchabac S, et al. First case report of tDCS efficacy in severe chemsex addiction. Dialogues Clin Neurosci. 2020;22:295–7.
Füllhase C, Soler R, Gratzke C. New strategies in treating male lower urinary tract symptoms. Curr Opin Urol. 2014;24:29–35.
Yafi FA, Sharlip ID, Becher EF. Update on the Safety of Phosphodiesterase Type 5 Inhibitors for the Treatment of Erectile Dysfunction. Sex Med Rev. 2018;6:242–52.
Radaelli D, Manfredi A, Zanon M, Fattorini P, Scopetti M, Neri M, et al. Synthetic Cannabinoids and Cathinones Cardiotoxicity: Facts and Perspectives. Curr Neuropharmacol. 2021;19:2038–48.
Schwarzbach V, Lenk K, Laufs U. Methamphetamine-related cardiovascular diseases. ESC. Heart Fail. 2020;7:407–14.
Hales G, Roth N, Smith D. Possible fatal interaction between protease inhibitors and methamphetamine. Antivir Ther. 2000;5:19.
Papaseit E, Vázquez A, Pérez-Mañá C, Pujadas M, de la Torre R, Farré M, et al. Surviving life-threatening MDMA (3,4-methylenedioxymethamphetamine, ecstasy) toxicity caused by ritonavir (RTV). Intensive Care Med. 2012;38:1239–40.
Funding
This research received no specific grant from any funding agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This scientific article is not concerned with ethical permissions nor informed consent.
Conflicts of Interest
L. Malandain has no conflict of interest to declare for this paper.
F. Thibaut has no conflict of interest to declare for this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Malandain, L., Thibaut, F. Chemsex: review of the current literature and treatment guidelines. Curr Addict Rep 10, 563–571 (2023). https://doi.org/10.1007/s40429-023-00488-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-023-00488-1