Abstract
Purpose
The main purpose was to study young patients’ self-reports on dental fear over a 5-year period, prospectively. Also, to compare these to professionals’ proxy reports for dental fear during invasive and non-invasive dental visits. The research question was, to what extent the self-reports and dental professionals’ proxy reports are congruent, and if there were patient age-dependent differences.
Methods
3134 patients from 11 public dental clinics, representing urban and rural areas, were invited. Four age cohorts were formed: 3, 7, 11, and 15 years of age and followed between the years 2008 and 2012. Dental examinations (non-invasive) and restorative treatments + extractions (invasive) were registered. During the treatments, self-reports regarding fear and professional proxy reports were registered: Not afraid at all = 0, little nervous = 1, quite afraid = 2, very scared = 3, terrified = 4.
Results
2363 patients completed the cohort periods (51% girls and 49% boys). In all, 9708 dental examinations, restorations and extractions were performed. The fear prevalence increased with the invasiveness of the dental procedure; 7–56%. For dental examinations and restorations, fear declined with ascending age. The highest fear prevalence was reported for dental extractions. Younger children reported fear more frequently than older children, p < 0.001. Frequent inconsistencies between self-reports and proxy reports were observed among the younger children (16%) compared to the older children (8%), p < 0.001.
Conclusion
Non-congruence was observed for self-reports and proxy reports regarding all age cohorts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite experiencing fear, children and adolescents often cooperate during dental procedures, such as examinations, restorations, or extractions (Ghanei et al. 2018; Krekmanova et al. 2009; Krekmanova and Robertson 2020). However, some children and adolescents have difficulty to interrupt and stop an ongoing dental treatment. Dental fear and anxiety (DFA) may be triggered by temperament, upbringing, and patient–dentist-dependence, as well as insensitive dentists (Klingberg and Broberg 1998), (Wondimu and Dahllof 2005). In addition, the perceived DFA or the perception of being compelled to cooperate may magnify the negative experience. Also, negative expectations are known as powerful modulators for future experiences (Williams et al. 2015). Therefore, dental professionals’ sensitivity to the young patient’s subtle DFA reaction is critical (Krekmanova et al. 2009). In contrast, behavior management problems (BMPs) are detectable by the unwillingness to cooperate (Klingberg 1995).
The Convention on the Rights of the Child highlights that all children should be given the possibility to express their own needs and have access to the best available medical methods (UNICEF). Consequently, children need to be given an opportunity to deal with and learn to feel safe during dental procedures. They should be offered reasonable chances to deal with challenging circumstances and to develop an understanding for the dental care session. Patient cooperation in the long run may positively reinforce the relation with the dental team. Based on the above, dental professionals should identify DFA while treating young patients (Klingberg 1995; Krekmanova et al. 2009; Krekmanova et al. 2009; Krekmanova and Robertson 2020).
Children’s dental fear is best communicated through self-reports, which constitutes the golden standard (Measelle et al. 2005). On the other hand, proxy reports reinforce or compensate for the individual’s insufficient maturity or ability to verbally communicate the own needs. The medical literature holds considerable knowledge on the congruence between children's self-reports and proxy assessments on pain (Mack et al. 2020). Often, these studies focus on medically ill children and highlight the inconsistency between their experiences and the proxy assessments (Pinheiro et al. 2018). The dental literature holds some information on the congruence between young patients’ fear and the dental professionals’ estimation during dental sessions. A poor agreement between self- and proxy reports is found in the literature (AlGharebi et al. 2021; Klein et al. 2015; Klingberg and Broberg 2007; Krikken et al. 2013; Luoto et al. 2010; Morgan 2015; Patel et al. 2015; Tollili et al. 2020). However, there is a knowledge gap regarding longitudinal prospective studies performed on a larger scale. Therefore, the aim was to study young patients’ self-reports on fear in comparison to professionals’ proxy reports during invasive and non-invasive dental visits, over a five-year period, prospectively.
Methods
Study design and patients
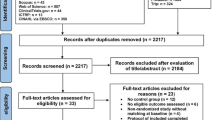
This study was approved by the Swedish Public Dental Service in Region Västra Götaland and Region Örebro County, and the National Ethical Review Board. The survey is a 5-year cohort study of an accelerated, longitudinal design.
3134 children and adolescents aged 3–15 years were eligible and invited to participate. The individuals were geographically seen at 11 Public Dental Clinics, selected to represent a young population from urban and rural areas. All parents gave written consent to their child’s participation. Also, each child gave assent through a written consent if ≥ 12 years old, or together with a parent if ≤ 12 years old.
In 2008 at baseline, four age cohorts were formed: 1 = 3 ≥ 7 years old, 2 = 7 ≥ 11 years old, 3 = 11 ≥ 15 years old, and 4 = 15 ≥ 19 years old. E.g., those children who turned 11 years old are only included in Group 3. Each child was regularly followed up till 2012 through an individually determined dental care need and oral health revision. Consequently, the children in Group 3 were not consistent with those children in Group 3 5 years later; an accelerated, longitudinal design.
The eligible licensed general dentists were working full or part time at the 11 participating clinics. Their professional experience varied, which reflected the actual circumstances. However, they were calibrated beforehand regarding the outcome measures.
Clinical registrations
For this study’s analysis, dental examinations were defined as non-invasive treatment, while restorative dental treatments and/or extractions were defined as invasive treatment. During each dental session, the operating professional registered the performed treatments. If any invasive treatment was included during the dental session, the session was classified as invasive treatment.
Self-reported DFA
Each patient was given the possibility to assess and report a possibly perceived fear, subsequent to each dental session, by answering the question: How did you feel today? Not afraid at all = 0, little nervous = 1, quite afraid = 2, very scared = 3, terrified = 4.
In cases where the youngest children had difficulty with self-reporting, parental help was used.
Proxy-reported DFA
Each concerned dental professional gave a proxy report on the patient’s fear using the DFA graded scale, subsequent to each dental session: Did the patient experience DFA? Not afraid at all = 0, little nervous = 1, quite afraid = 2, very scared = 3, terrified = 4.
The dental professionals were calibrated on the DFA outcome measures through meetings before the study start.
Statistical methods
Statistical data described patients, gender, and dental examinations (non-invasive dental treatments), as well as restorations and extractions (invasive treatment).
The self-reported DFA was dichotomized into new variables; Not afraid at all (0) = 0, and Afraid (1–4) = 1. The dichotomization of DFA scores in the current study was performed to clearly separate the children who were not afraid, from the children who were somewhat nervous or more; DFA ≥ 1.
The self-reported DFA prevalence (%) was calculated for each age cohort, respectively. The age cohorts were also dichotomized into new variables: Younger children (Cohorts 1 + 2), and Older children (Cohorts 3 + 4). Chi-square tests were applied on dichotomized variables to analyze for possible significant DFA differences.
The congruencies and discrepancies between patients’ self-reported DFA and professional proxy reports were calculated. The corresponding congruencies were calculated also when DFA was dichotomized. Thereby, DFA scores 1–4 were grouped together, versus DFA = 0. The patient’s positive DFA (1–4) and the corresponding positive proxy report (1–4) were considered congruent. Also, the patient’s negative DFA (0) self-report and the corresponding negative proxy report (0) were considered congruent.
The inconsistency between the DFA reports (positive self-report/negative proxy report, or vice versa) conveyed a discrepancy.
The sensitivity and specificity, as well as the positive predictive value (PPV) and the negative predictive value (NPV), were calculated for the self-reported and professional proxy reports of DFA.
IBM SPSS Statistics for Windows, Version 26.0 (IBM Corp., NY, USA), was used for the statistical analyses, and p values below 0.05 represented statistical significance.
Results
Out of the 3134 eligible registered children at baseline, 2363 completed the cohort periods: 1: (3–7 years) n = 695 children, 2: (7–11 years) n = 642 children, 3: (11–15 years) n = 574 children, and 4: (15–19 years) n = 452 children, in total 1215 girls (51%) and 1148 boys (49%).
During the study period, 9708 dental sessions with both self-reported and professional proxy reports of DFA were registered; 8070 sessions of dental examinations, and 1202 sessions of restorations, as well as 436 sessions of extractions, were completed (Table 1). The self-reported DFA prevalence (%) ranged with the invasiveness of the dental procedure by 7–57%. The frequencies and prevalence for each age cohort and dental treatment are presented in Table 1.
For both dental examinations and restorations, the self-reported DFA declined with age. The DFA prevalence (%) was highest for the extractions and varied only slightly between the age cohorts (Table 1). The gender distribution at baseline was reflected in both the non-invasive as well as the invasive treatments (Table 2).
The chi-square analysis for the dichotomized DFA showed a significant statistical difference since younger children reported fear more frequently, compared to older children, p < 0.001 (Table 1). The corresponding analysis for the dental extractions showed a non-significant difference, p > 0.05 (Table 1).
Considering the dental treatments in general, a more frequent inconsistency between DFA reports was observed regarding younger children (16%), compared to older children (8%), p < 0.001. This was also true for non-invasive sessions with younger children (449 sessions; 12%), compared to older children (231 sessions; 7%), (Table 3). Considering DFA for the invasive treatments and younger children’s 106 sessions (15.7%), compared to 84 sessions (10.8%) of older children, the statistical difference was also significant, p < 0.05 (Table 4).
As seen in Table 5, sensitivity drops with increased age, while specificity rises with age.
The positive predictive values (PPV) and the negative predictive values (NPV) are presented in Table 5, the largest PPV data for invasive treatments; 0.85 (age cohort 11–15 years).
DFA-fluctuations regarding the sexes
22.8% of the girls reported fear compared to 17.7% of the boys for all dental procedures, p < 0.001. The girls reported significantly more DFA regarding sessions which included dental restorations and examinations; χ2 p < 0.001. For sessions including extractions, no statistically significant differences were observed regarding the sexes’ DFA reports; χ2, p > 0.05. At sessions including extractions, 45% of the boys and 55% of the girls reported DFA (mean 53%).
The DFA analyses regarding the non-invasive and invasive dental procedures showed that 11% of the girls were mis-rated in comparison to 9% of the boys, p < 0.014. Regarding invasive treatment, 12.5% of the girls were mis-rated in comparison to 12% of the boys, p > 0.70. More girls (10%) than boys (8%) were mis-rated when it comes to non-invasive treatments, p < 0.014.
Discussion
The main results showed the young patients’ self-reported DFA increased with invasive dental procedures. Furthermore, children < 11 years of age more frequently reported DFA during dental examinations and restorations than older children. The results also revealed that among 11–19-year-olds, 7–12% experienced fear when undergoing regular dental examinations. Regarding extractions, 41–56% of all 3–19-year-olds rated themselves as experiencing some degree of fear, which is considered noteworthy. The findings are in congruence with previous studies, indicating that preventive measures to minimize young patients’ DFA have not yet reached the desired outcome (Cianetti et al. 2017; Ghanei et al. 2018; Krekmanova and Robertson 2020).
DFA is a complex phenomenon with various intrinsic and extrinsic influencing factors that all are individually interpreted by the patient. Numerous instruments have been developed and are used in research settings to measure DFA’s various fear aspects (Porritt et al. 2013; Yon et al. 2020).
A frequently used tool in research is the Children's Fear Survey Schedule-Dental Subscale (CFSS-DS) (Klingberg 1994). However, a drawback for this instrument is its time-consuming nature, as this tool consists of 15 questions. It also requires the younger patient to be literate. In comparison, this current study design used two questions in the DFA self-report and proxy report.
Berggren and Meynert 1984, emphasized that DFA developed in adulthood is often triggered by traumatically experienced dental treatments during childhood (Berggren and Meynert 1984), showed that pre-schoolers treated for carious lesions are at a higher risk for developing DFA by 10 years of age (Raadal et al. 2002). Recurrent painful procedures and lack of control, as well as insensitive dentists, are often the triggers (Krekmanova et al. 2009). Today, up to 37% of the adult population still report DFA, apart from 5% reporting dental phobia for the same reasons (Svensson et al. 2016). Dental injection is found to be the highest ranked DFA-trigger among children and adolescents (Vanhee et al. 2020). Furthermore, some dentists consider themselves to be challenged by children < 10 years of age, having to meet their fear and uncooperativeness when using local anesthesia (Ronneberg et al. 2015).
Children with behavior management problems (BMP) frequently score high on the CFSS-DS (Wogelius et al. 2003). Therefore, dental care offered to children and adolescents requires a high level of expertise. Positive dental treatment experiences may lead to latent inhibition, i.e., a higher resistance for developing DFA (van Waaijen et al. 2001).
A notable result was the inconsistency between the patients’ DFA reports and the DFA proxy assessments as every fourth child between the ages of 3–11 years was mis-rated during regular dental examinations. The youngest of the age group could be considered especially vulnerable due to insufficient maturity and understanding of the own participation in the dental situation. This in itself could negatively affect the treatment outcome. No comparable data exist to confirm these findings. On the other hand, the inconsistency between the DFA self-reports and proxy reports may have mirrored the dental professional’s sensitivity and child competency when treating children.
The current study indicates that the DFA sensitivity drops with increasing age, with DFA specificity rising accordingly, i.e., fewer patients are correctly defined as anxious. Simultaneously, more patients are correctly defined as non-anxious. The finding is congruent with the dental fear prevalence, which normally decreases with age (Cianetti et al. 2017).
Preventing DFA often requires a high level of skill and competency to balance what leads to prevention, especially where young children are concerned. It is often considered a simple task for the dental staff to strive to prevent DFA for each dental setting. However, the methods for the prevention of DFA may be unintentionally misused by the general dental practitioners due to habitual and reoccurring daily praxis. There is substantial knowledge on how to prevent DFA, but this knowledge may not be consistently applied by dental practitioners.
A limitation of this study is that comparable data are lacking to match the methodology, a prospective and prolonged study design. The advantage of this study is that each age cohort holds a substantial number of young patients, facilitating a careful generalization of the findings.
The current findings generate further scientific questions for future research. Readily applicable DFA tools are needed to be systematically evaluated in clinical settings.
Conclusion
Considering the limitations of the present study, the following conclusions can be made:
-
Consistent DFA tools are needed to be used in clinical and research settings.
-
Children should be addressed regarding their DFA experience in every dental treatment session.
-
A knowledge gap exists regarding the congruence of self-reports and proxy reports in longitudinal, prospective studies.
-
The dental professionals’ sensitivity to the young patient’s fear is crucial for a successful treatment outcome.
References
AlGharebi S, Al-Halabi M, Kowash M, et al. Children’s dental anxiety (self and proxy reported) and its association with dental behaviour in a postgraduate dental hospital. Eur Arch Paediatr Dent. 2021;1:29–40. https://doi.org/10.1007/s40368-020-00517-x.
Berggren U, Meynert G. Dental fear and avoidance: causes, symptoms, and consequences. J Am Dent Assoc. 1984;2:247–51. https://doi.org/10.14219/jada.archive.1984.0328.
Cianetti S, Lombardo G, Lupatelli E, et al. Dental fear/anxiety among children and adolescents. A systematic review. Eur J Paediatr Dent. 2017;2:121–30. https://doi.org/10.23804/ejpd.2017.18.02.07.
Ghanei M, Arnrup K, Robertson A. Procedural pain in routine dental care for children: a part of the Swedish BITA study. Eur Arch Paediatr Dent. 2018;5:365–72. https://doi.org/10.1007/s40368-018-0368-2.
Klein U, Manangkil R, DeWitt P. Parents’ ability to assess dental fear in their six- to 10-year-old children. Pediatr Dent. 2015;5:436–41.
Klingberg G. Reliability and validity of the Swedish version of the dental subscale of the children’s fear survey schedule CFSS-DS. Acta Odontol Scand. 1994;52(4):255–6. https://doi.org/10.3109/00016359409029055.
Klingberg, G. Dental fear and behavior management problems in children. A study of measurement, prevalence, concomitant factors, and clinical effects. Swed Dent J Suppl. 1995; 1–78. https://www.ncbi.nlm.nih.gov/pubmed/7740439. Accessed 16 Dec 2021.
Klingberg G, Broberg AG. Temperament and child dental fear. Pediatr Dent. 1998;4:237–43.
Klingberg G, Broberg AG. Dental fear/anxiety and dental behaviour management problems in children and adolescents: a review of prevalence and concomitant psychological factors. Int J Paediatr Dent. 2007;6:391–406. https://doi.org/10.1111/j.1365-263X.2007.00872.x.
Krekmanova L, Robertson A. Children’s and adolescents’ pain, discomfort, fear, cooperation, and parental presence during dental extractions. IPDOAJ. 2020;1:389–94. https://doi.org/10.32474/IPDOAJ.2020.05.000202.
Krekmanova L, Bergius M, Robertson A, et al. Everyday- and dental-pain experiences in healthy Swedish 8–19 year olds: an epidemiological study. Int J Paediatr Dent. 2009;6:438–47. https://doi.org/10.1111/j.1365-263X.2009.01016.x.
Krikken JB, van Wijk AJ, ten Cate JM, et al. Measuring dental fear using the CFSS-DS. Do children and parents agree? Int J Paediatr Dent. 2013;2:94–100. https://doi.org/10.1111/j.1365-263X.2012.01228.x.
Luoto A, Tolvanen M, Rantavuori K, et al. Can parents and children evaluate each other’s dental fear? Eur J Oral Sci. 2010;3:254–8. https://doi.org/10.1111/j.1600-0722.2010.00727.x.
Mack JW, McFatrich M, Withycombe JS, et al. Agreement between child self-report and caregiver-proxy report for symptoms and functioning of children undergoing cancer treatment. JAMA Pediatr. 2020;11: e202861. https://doi.org/10.1001/jamapediatrics.2020.2861.
Measelle JR, John OP, Ablow JC, et al. Can children provide coherent, stable, and valid self-reports on the big five dimensions? A longitudinal study from ages 5 to 7. J Pers Soc Psychol. 2005;1:90–106. https://doi.org/10.1037/0022-3514.89.1.90.
Morgan A. Summary of: inter-rater agreement between children’s self-reported and parents’ proxy-reported dental anxiety. Br Dent J. 2015;4:236–7. https://doi.org/10.1038/sj.bdj.2015.125.
Patel H, Reid C, Wilson K, et al. Inter-rater agreement between children’s self-reported and parents’ proxy-reported dental anxiety. Br Dent J. 2015;4:E6. https://doi.org/10.1038/sj.bdj.2015.98.
Pinheiro LC, McFatrich M, Lucas N, et al. Child and adolescent self-report symptom measurement in pediatric oncology research: a systematic literature review. Qual Life Res. 2018;2:291–319. https://doi.org/10.1007/s11136-017-1692-4.
Porritt J, Buchanan H, Hall M, et al. Assessing children’s dental anxiety: a systematic review of current measures. Community Dent Oral Epidemiol. 2013;2:130–42. https://doi.org/10.1111/j.1600-0528.2012.00740.x.
Raadal M, Strand GV, Amarante EC, et al. Relationship between caries prevalence at 5 years of age and dental anxiety at 10. Eur J Paediatr Dent. 2002;1:22–6.
Ronneberg A, Strom K, Skaare AB, et al. Dentists’ self-perceived stress and difficulties when performing restorative treatment in children. Eur Arch Paediatr Dent. 2015;4:341–7. https://doi.org/10.1007/s40368-014-0168-2.
Svensson L, Hakeberg M, Boman UW. Dental anxiety, concomitant factors and change in prevalence over 50 years. Community Dent Health. 2016;2:121–6.
Tollili C, Katsouda M, Coolidge T, et al. Child dental fear and past dental experience: comparison of parents’ and children’s ratings. Eur Arch Paediatr Dent. 2020;5:597–608. https://doi.org/10.1007/s40368-019-00497-7.
van Waaijen D, ten Berge M, Veerkamp JS. Dental fear in children: dental experiences during childhood. Ned Tijdschr Tandheelkd. 2001;11:466–9.
Vanhee T, Mourali S, Bottenberg P, et al. Stimuli involved in dental anxiety: What are patients afraid of?: a descriptive study. Int J Paediatr Dent. 2020;3:276–85. https://doi.org/10.1111/ipd.12595.
Williams LE, Oler JA, Fox AS, et al. Fear of the unknown: uncertain anticipation reveals amygdala alterations in childhood anxiety disorders. Neuropsychopharmacology. 2015;6:1428–35. https://doi.org/10.1038/npp.2014.328.
Wogelius P, Poulsen S, Sorensen HT. Prevalence of dental anxiety and behavior management problems among six to eight years old Danish children. Acta Odontol Scand. 2003;3:178–83. https://doi.org/10.1080/00016350310003468.
Yon MJY, Chen KJ, Gao SS, et al. An introduction to assessing dental fear and anxiety in children. Healthcare (Basel). 2020. https://doi.org/10.3390/healthcare8020086.
Wondimu B, Dahllöf G. Attitudes of Swedish dentists to pain and pain management during dental treatment of children and adolescents. Eur J Paediatr Dent. 2005;2:66–72. https://www.ncbi.nlm.nih.gov/pubmed/16004534
Funding
Open access funding provided by University of Gothenburg. This study was funded by the Public Dental Service, Region Västra Götaland and Region Örebro County, Sweden.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethical approval
The application for ethical review (No. 286-07) was approved.
Informed consent
Informed consent was obtained from all participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Krekmanova, L., Sotirianou, M. & Sabel, N. Young patients’ self-reported fear compared to professionals’ assessments during invasive and non-invasive dental visits: a prospective, longitudinal study. Eur Arch Paediatr Dent 23, 309–315 (2022). https://doi.org/10.1007/s40368-021-00685-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40368-021-00685-4