Abstract
Subsolid pulmonary nodules (SSNs) are frequent findings on CT scans, and their reported prevalence ranges between 9 and 20% in the literature. The management of SSNs requires specific knowledge. In this review, we report the standard imaging approach and the potential role of positron emission tomography/computed tomography (PET/CT) in the detection of pulmonary SSNs, to help clinicians by providing evidence-based recommendations. The classification of the basic histology, nomenclature, and behaviours of the different lesions is described, with the typical imaging patterns and main recommendations for their management when detected on CT imaging. A comprehensive review of the literature has been performed to determine the potential role of 18F-fluorodeoxyglucose (18F-FDG) PET/CT in the evaluation of SSNs. Finally, we describe the synergy of CT and 18F-FDG PET in the evaluation and management of SSNs. We hypothesise that in cases of 18F-FDG-positive findings, it would be worth considering pre-emptive local treatment with ablation, radiotherapy, or surgical resection. New prospective studies with greater homogeneity of data acquisition, including imaging time points, would be beneficial when reappraising the role of 18F-FDG PET/CT following new technical developments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Owing to the worldwide availability of multi-detector computed tomography and screening studies, a large amount of information has been collected about pulmonary nodules. In 2005, the Fleischner Society published recommendations regarding the management of small occult lung nodules, which have since been used as the gold standard for interpretation [1]. Other systems are available and in common use, such as the British Thoracic Society (BTS) guidelines on the investigation and management of pulmonary nodules [2].
Several papers reported significantly higher cancer risk in the case of part-solid nodules, than in solid nodules. Henschke et al. found a 34% malignancy rate in part-solid nodules as opposed to 7% in solid nodules [P < 0.001] [3]. Similarly, markedly higher malignancy was demonstrated in part-solid nodules by Zheng et al. [75% vs. 39% in solid nodules, P = 0,001] [4].
However, the complexity of subsolid nodules (SSNs) makes their assessment, management, and even prognosis more difficult, and a clear consensus has yet to be determined. SSNs are frequent findings on computed tomographic scans: the prevalence of these nodules varies between 9 and 20% in the literature [3, 5]. 18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) is a widely used technique for the assessment of solid nodules and the staging of non-small cell lung cancer (NSCLC), which also allows the detection of nodal and distant metastases; however, its role in the evaluation and management of pulmonary SSNs is still unclear, and only limited literature is available [6, 7].
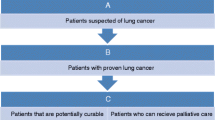
This study reviews the standard imaging approach and the potential role of PET/CT in the detection of pulmonary SSNs, with the aim of helping clinicians by providing evidence-based recommendations.
Background
Basic nomenclature
In contrast to solid pulmonary nodules, which contain only solid tissue components [2], pulmonary SSNs always have a ground-glass component and can have additional solid elements. Pulmonary SSNs can be further divided into pure ground-glass nodules (GGNs) and part-solid nodules (PSNs) [5, 8, 9] (Fig. 1). Pure GGNs (sometimes termed ground-glass opacities) are small to medium-sized (3–30 mm) focal areas of increased lung attenuation, where the underlying pulmonary structures can be visualized [10, 11]. PSNs are defined as focal lung lesions ranging in size up to 30 mm on CT scans with both solid and ground-glass components [1, 12].
Classification and basic histology of pulmonary SSNs
The revised classification of pulmonary adenocarcinoma in situ (AIS) precursor lesions is based on the assessment of the growth pattern of the lesion. It was proposed by the International Association for the Study of Lung Cancer, the American Thoracic Society, and the European Respiratory Society [13] (Table 1). Since the term ‘bronchiolo-alveolar carcinoma’ (BAC) has fallen out of favour, the respective growth patterns of BACs are now described as ‘lepidic’. Briefly, lepidic growth refers to neoplastic tumour cell growth alongside normal pulmonary structures without the formation of papillary composition and signs of inflammation [14]. These lesions are classified based on their histopathological characteristics as either preinvasive or invasive neoplasms.
Role of CT in the evaluation of SSNs
As described above, the morphological category of ‘pulmonary SSNs’ includes pure GGNs and PSNs. Godoy et al. [15] introduced a morphological classification of SSNs on multi-detector CT imaging (Fig. 2). However, this classification is not suitable for differentiating between low-risk and high-risk groups as per Fleischner Society criteria [1, 15].
Pulmonary nodules, as mentioned earlier, are classified into preinvasive and invasive lesions. In this section we summarize these adenocarcinoma subtypes based on their histopathological features and imaging morphology.
Summary of histopathological and radiological correlations in lung adenocarcinoma subtypes is shown in Table 2. Summary of histopathological and radiological correlations in lung adenocarcinoma subtypes is shown in Table 2 and divided in:
Preinvasive lesions
Atypical adenomatous hyperplasia (AAH) is the first putative precursor lesion of adenocarcinoma of the lung [16]. On CT imaging, AAH usually presents as a well-defined round pure GGN < 5 mm in diameter (Fig. 3a) [17].
a Atypical adenomatous hyperplasia; demonstrated as focal pure GGN. b Adenocarcinoma in situ; seen as a small part-solid nodule. c Minimally invasive adenocarcinoma demonstrated a part-solid nodule with a dominant peripheral GGO component. d Invasive adenocarcinoma (predominant lepidic growth), seen as a part-solid nodule with a large central solid component
Adenocarcinoma in situ (AIS) is a moderately sized (≤ 30 mm) solitary neoplastic lesion, in which cellular atypia is more strongly expressed [14]. AIS can manifest on CT based on its histological composition. Non-mucinous AIS usually appear as pure GGNs; however, owing to the presence of collapsed alveoli they can be seen as part-solid nodules (Fig. 3b). Mucinous AIS can appear either as a solid nodule or as consolidation [17].
Lymphatic, vascular, or pleural invasion are not features of either AAH or AIS [14].
Invasive lesions
Minimally invasive adenocarcinoma (MIA). It is also a small to medium-sized (≤ 30 mm) lesion containing limited invasive foci (< 5 mm stromal invasion), without lymphatic, vascular, or pleural invasion [14, 18]. Imaging features of MIA described in the literature are less consistent. Generally, non-mucinous MIA usually appears in the form of a pure GGN or as a PSN (Fig. 3c). Mucinous MIA is far less frequently observed and predominantly presents as a solid nodule [11].
Invasive adenocarcinoma. Previously divided into non-mucinous and mucinous types. However, non-mucinous adenocarcinomas are now described pathologically based on their predominant subtype. Lepidic predominant invasive adenocarcinoma (LPA) is a tumour of varying size, which has a > 5 mm lymphatic, vascular or pleural invasion. The CT morphology of LPAs is variable, but they mostly appear as an SSN or a mass (Fig. 3d) [14, 18, 19]. Invasive mucinous adenocarcinoma is a subtype of invasive adenocarcinoma with an especially wide range of appearance, from SSNs to consolidation [17].
Overall, the preinvasive lesions (atypical adenomatous hyperplasia and adenocarcinoma in situ) mainly correspond to pure GGNs and less frequently to PSNs, whereas the majority of invasive tumour types almost always correspond to part-solid or solid nodules. However, it is essential to emphasize that, similarly to the histological delineation between preinvasive and invasive lesions, there is a wide overlap in their features on imaging; therefore, there is no definitive morphological description [20].
Regarding the imaging characteristics for malignancy in SSNs, the presence and size of the solid component, upper lobe location, spiculated nodule contour, and pleural involvement are all major predictors [21]. However, it should be emphasized that these ‘red flags’ for malignancy must be considered together with the individual patient’s medical history.
Recommendations for the management of SSNs detected on CT
Owing to the heterogeneity of pulmonary SSNs, it is difficult to make recommendations on their subsequent management since it has not been standardized. SSNs with similar phenotypes can have profoundly different behaviours, therefore it is essential to use a technique that provides not only structural findings but also metabolic details of these tumours. As a reference, we extrapolated from the prior literature review by Naidich et al. on the management of pulmonary SSNs [22]. These guidelines are also consistent with those based on morphological classification by Godoy et al. [15], which are outlined in Fig. 2.
Overall, solitary pure GGNs up to 5 mm in size do not need further intervention. Solitary pure GGNs > 5 mm require a follow-up evaluation after 3 months. In case of persistent nodules, annual CT surveillance for a minimum of 3 years is recommended (Table 3) [22]. Regarding solitary PSNs, especially lesions with solid components ≥ 5 mm, these should be considered malignant until proven otherwise. Consequently, after the initial examination, follow-up CT should be performed at 3 months to rule out transient nodules. In case of persistent PSNs, if the solid component is < 5 mm, annual CT surveillance for a minimum of 3 years should be performed. If the solid component is 5 mm or larger, percutaneous transthoracic needle biopsy or surgical resection is recommended. For PSNs in which the solid component is 10 mm larger, PET/CT is recommended before more invasive interventions, for preoperative staging and for more precise prediction of the prognosis (Table 4) [22]. Multiple well-defined pure GGNs measuring < 5 mm each should be treated conservatively; hence, in the case of persistent nodules < 5 mm, follow-up CT scans should be performed at 2 and 4 years. If among the multiple pure GGNs there is at least one that reaches or exceeds 5 mm in size and there is no dominant lesion (nodule), an initial follow-up CT is required at 3 months, followed by yearly CT surveillance for a minimum of 3 years. In the case of multiple SSNs (i.e. pure GGNs and PSNs) if there is at least one dominant nodule, either part-solid or solid, the nature of the dominant lesion will define the management strategy. After an initial CT at 3 months, in the case of persistent nodules (> 5 mm) with at least one existing dominant lesion, percutaneous transthoracic needle biopsy and/or a surgical approach (video-assisted thoracoscopic surgery, wedge or segmental resection) should be considered. If there is one persistent, dominant subsolid or solid nodule in which the solid component reaches 10 mm, an initial PET/CT examination can be useful for a more accurate estimation of the prognosis and for preoperative staging (Table 5) [22].
Possible role of PET/CT in the evaluation of SSNs
Distinguishing minimally invasive adenocarcinoma (MIA) from lepidic predominant invasive adenocarcinoma (LPA) is of paramount importance because these conditions have distinctly different clinical courses and differing treatment pathways [14]. 18F-FDG PET/CT has a key role in the differentiation of benign lesions from malignant neoplasms. However, owing to conflicting data in the literature, the exact place of 18F-FDG PET/CT in the evaluation of pulmonary SSNs is not currently fully established [15, 23].
It has been shown in several studies that the sensitivity of 18F-FDG PET/CT to detect pulmonary nodules with a lepidic growth pattern is limited, especially when exclusively GGNs are present [24, 25]. Small pure GGNs (< 10 mm) are usually negative on 18F-FDG PET. It has also been demonstrated that in cases of small pure GGNs, PET/CT does not have significant value in providing additional information about nodal status or extrathoracic metastases [26, 27]. In concordance with these studies, Yap et al. [28] found that out of 46 SSNs that were confirmed to be ‘mixed’ adenocarcinomas, 67% of those presenting with a pure GGN pattern were negative on 18F-FDG PET scans [30]. Kim et al. [29] found that for the staging of a pure GGN, 18F-FDG PET/CT is not recommended, since the incidence of an occult nodal or distant metastasis of these lesions is very low. An opposing view was reported by Naidich et al. [22] In their paper, the authors complemented the original Fleischner Society recommendations for incidentally detected solid nodules by introducing novel recommendations specifically aimed at pulmonary SSNs. In this review, 18F-FDG PET/CT was advised as a first-line examination for solitary PSNs with a solid nodule greater than 10 mm in size.
Okada et al. [30] demonstrated that CT and 18F-FDG PET/CT findings are essential to set up proper treatment strategies in cases of adenocarcinoma (including solid and sub-solid nodules), and that high 18F-FDG tumour activity of different nodules on pre-treatment PET/CT scans was associated with poor survival rates. The authors determined that the maximum standard uptake value (SUVmax) was a potential tool for estimating the prognosis. Tsutani et al. [31] evaluated 502 patients with stage IA lung adenocarcinoma and found that both the size of the solid compartment on high-resolution CT and the SUVmax on 18F-FDG PET/CT were significant independent predictors of nodal involvement. However, it is worth noting that in these studies the investigators analysed early-stage NSCLC as a whole group and did not distinguish whether the nodules were PSNs or solid nodules. Therefore, no data were provided in these two studies on the role of 18F-FDG PET/CT in the detection of lung SSNs.
Chun et al. [32] assessed the feasibility of 18F-FDG PET/CT in distinguishing malignancy from inflammation. A total of 68 SSNs (14 pure GGNs and 54 PSNs) were assessed in 45 patients. In this study, SUVmax values of PSNs were found to be higher in inflammatory lesions than in malignant tumours (Fig. 4a). Hence, the authors of this study recommended a follow-up 18F-FDG PET/CT examination if the SUVmax of an SSN exceeds the value of 2.6 (Fig. 2). This paradoxical finding is only valid regarding sub-solid lung nodules and is worth considering during evaluation and during a final review at multidisciplinary team meetings.
Given the fact that management protocols differ not only between nations but even in different hospitals in the same country, we suggest that the degree of lung nodule uptake measured by SUVmax should always be evaluated in the context of the mediastinal blood pool SUVmax. In addition, multidisciplinary team discussion involving radiologists, nuclear medicine physicians, and clinicians is essential for the most appropriate follow-up timing and patient management.
Discussion
In this review, we have summarised the current knowledge surrounding the use of conventional CT imaging and 18F-FDG PET/CT in the assessment of pulmonary SSNs. To date, there have been only a few dedicated studies examining the role of 18F-FDG PET/CT in SSNs [29, 32].
CT remains the standard technique for evaluating SSNs given, the good anatomical/morphological detail provided by this modality and the possibility of performing serial follow-up imaging to assess for changes [2]. Nevertheless, the technique does not take into consideration the dynamic processes that occur in the small airways of these patients, with the potential for mutations to arise in the cells of the epithelium, which may remain quiescent for many years and demonstrate changes in morphology and size only much later in their clinical course [14]. In this regard, 18F-FDG PET is an exquisitely sensitive imaging tool to evaluate potential changes in the viability of cancers at earlier stages. As for the limit of PET/CT imaging, the tracer avidity of SSNs is generally very low. However, previous studies demonstrated that in preinvasive conditions, molecular imaging helps to prognosticate the behaviour of these lesions; in fact, those lesions showing some uptake were more likely to progress to cancer than those with no uptake [33, 34].
In the authors’ experience, in SSNs with 18F-FDG-positive findings, it is worthwhile considering a pre-emptive approach to treatment with conventional radiotherapy, focal stereotactic ablative radiotherapy (SABR), or surgery (depending on fitness), rather than proceed to biopsy given the high rate of negative biopsies and the additional morbidity [35, 36].
Of note, most of the current literature refers to studies performed with older scanners and sometimes with heterogeneous protocols and methods of assessment. New developments in technology, including the availability of new digital PET cameras with more detectors and new methods of image reconstruction, have led to a revolution in the sensitivity of the technique so that it can identify/detect nodules with very low levels of metabolic activity. In a similar manner, the established role of high-resolution CT can be used in synergy with molecular imaging in lesion detection/characterization and in the follow-up of these patients, thus providing a ‘one-stop shop’ examination [37, 38].
The standardization of parameters, including existing measurements such as SUV max, minimum SUV (SUV min), target–background ratio (TBR) and SUV normalised to lean body mass (SUV lean), would be beneficial in future studies. New and developing parameters, such as those based on artificial intelligence-based analysis of images (e.g. texture analysis), might be useful to further enhance the information that would be otherwise hidden at routine clinical evaluation, potentially providing additional value and eventually a more comprehensive analysis of data in a research context.
Finally, we want to acknowledge that the above is the opinion of experts in a tertiary oncology hospital with the largest flow of lung cancer patients in the UK, and we performed FDG PET/CT for over 20 years in a large screening population with lung pre-invasive conditions, including, in the last decade, subsolid and ground glass nodules. Nonetheless, we made a literature search at the best of our capacity by using the most common (PubMed, Medline) search engines to provide the information we think may be useful for the readers regarding this particular entity.
Conclusion
We hypothesise that 18F-FDG-positive findings may be used as an additional predictive variable for the management of these patients. Further data will be necessary to understand whether the composite prediction models based on clinical, radiological and metabolic factors might better estimate the probability that a subsolid pulmonary nodule is malignant and eventually lead to the best therapeutic option.
Likewise, new prospective studies with greater homogeneity of data acquisition, including imaging time points, would be beneficial when reappraising the role of 18F-FDG PET/CT following new technical developments in treatment.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
References
MacMahon H, Naidich DP, Goo JM, Lee KS, Leung ANC, Mayo JR et al (2017) Guidelines for management of incidental pulmonary nodules detected on CT images: from the fleischner society 2017. Radiol. Radiol Soc North Am Inc 284:228–43
Callister MEJ, Baldwin DR, Akram AR, Barnard S, Cane P, Draffan J et al (2015) British thoracic society guidelines for the investigation and management of pulmonary nodules. Thorax 70:ii1-54
Claudia I. Henschke OSM. CT Screening for Lung Cancer: Frequency and Significance of Part-Solid and Nonsolid Nodules [Internet]. Available from: www.ajronline.org
Zhang R, Tian P, Chen B, Zhou Y, Li W (2020) Predicting lung cancer risk of incidental solid and subsolid pulmonary nodules in different sizes. Cancer Manag Res 12:8057–8066
Hammer MM, Palazzo LL, Kong CY, Hunsaker AR (2019) Cancer risk in subsolid nodules in the national lung screening trial. Radiology 293(2):441–448
Suh YJ, Park CM, Han K, Jeon SK, Kim H, Hwang EJ et al (2020) Utility of FDG PET/CT for preoperative staging of non-small cell lung cancers manifesting as subsolid nodules with a solid portion of 3 cm or smaller. Am J Roentgenol 214(3):514–523
Veronesi G, Travaini LL, Maisonneuve P, Rampinelli C, Bertolotti R, Spaggiari L et al (2015) Positron emission tomography in the diagnostic work-up of screening-detected lung nodules. Eur Respir J 45(2):501–510
Seidelman JL, Myers JL, Quint LE (2013) Incidental, subsolid pulmonary nodules at CT: etiology and management. Cancer Imaging 13:365–73
Heidinger BH, Silva M, De Margerie-Mellon C, VanderLaan PA, Bankier AA. (2019) The natural course of incidentally detected, small, subsolid lung nodules-is follow-up needed beyond current guideline recommendations? Vol. 8, Translational Lung Cancer Research. AME Publishing Company, p. S412–7
Cozzi D, Cavigli E, Moroni C, Smorchkova O, Zantonelli G, Pradella S, et al. (2021) Ground-glass opacity (GGO): a review of the differential diagnosis in the era of COVID-19. Vol. 39, Japanese Journal of Radiology. Springer Japan,. p. 721–32.
Kim H, Park CM, Koh JM, Lee SM, Goo JM. (2014) Pulmonary subsolid nodules: What radiologists need to know about the imaging features and management strategy. Vol. 20, Diagnostic and Interventional Radiology. AVES Ibrahim Kara, p. 47–57.
Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J (2008) Fleischner society: glossary of terms for thoracic imaging. Radiology 246:697–722
Travis WDBENM et al (2012) International association for the study of lung cancer/American thoracic society/European respiratory society international multidisciplinary classification of lung adenocarcinoma. Yearbook Diagn Radiol 2012:2–5
Weichert W, Warth A (2014) Early lung cancer with lepidic pattern: adenocarcinoma in situ, minimally invasive adenocarcinoma, and lepidic predominant adenocarcinoma. Curr Opin Pulm Med. Lippincott Williams Wilkins 20:309–16
Godoy MCB, Naidich DP. (2012) Overview and Strategic Management of Subsolid Pulmonary Nodules [Internet]. Available from: www.thoracicimaging.com
Chang Min Park MD et al. CT Findings of Atypical Adenomatous Hyperplasia in the Lung
Lambe G, Durand M, Buckley A, Nicholson S, McDermott R (2020) Adenocarcinoma of the lung: from BAC to the future. Insights Imaging 11(1):69
Iwata H (2016) Adenocarcinoma containing lepidic growth. J Thorac Dis 8:E1050-2
Strand TE, Rostad H, Strøm EH, Hasleton P (2015) The percentage of lepidic growth is an independent prognostic factor in invasive adenocarcinoma of the lung. Diagn Pathol. https://doi.org/10.1186/s13000-015-0335-8
Austin JHM, Garg K, Aberle D, Yankelevitz D, Kuriyama K, Lee HJ et al (2016) Radiologic implications of the 2011 classification of adenocarcinoma of the lung. Radiology 266:62–71
Oda S, Awai K, Liu D, Nakaura T, Yanaga Y, Nomori H et al (2008) Ground-glass opacities on thin-section helical CT: differentiation between bronchioloalveolar carcinoma and atypical adenomatous hyperplasia. Am J Roentgenol 190(5):1363–1368
Naidich DP, Bankier AA, MacMahon H, Schaefer-Prokop CM, Pistolesi M, Goo JM et al (2013) Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the fleischner society. Radiology 266:304–17
McDermott S, Kilcoyne A, Wang Y, Scott JA, Halpern EF, Ackman JB (2019) Comparison of the 18 F-FDG avidity at PET of benign and malignant pure ground-glass opacities: a paradox? Clin Radiol 74(3):187–195
Tsunezuka Y, Shimizu Y, Tanaka N, Takayanagi T, Kawano M (2007) Positron emission tomography in relation to Noguchi’s classification for diagnosis of peripheral non-small-cell lung cancer 2 cm or less in size. World J Surg 31(2):314–317
Evangelista L, Panunzio A, Scagliori E, Sartori P (2018) Ground glass pulmonary nodules: their significance in oncology patients and the role of computer tomography and 18F–fluorodeoxyglucose positron emission tomography. Eur J Hybrid Imaging. https://doi.org/10.1186/s41824-017-0021-z
Lee HY, Lee KS, Han J, Kim BT, Cho YS, Shim YM et al (2009) Mucinous versus nonmucinous solitary pulmonary nodular bronchioloalveolar carcinoma: CT and FDG PET findings and pathologic comparisons. Lung Cancer 65(2):170–175
Tsunezuka Y, Shimizu Y, Tanaka N, Takayanagi T, Kawano M (2007) Positron emission tomography in relation to Noguchi’s classification for diagnosis of peripheral non-small-cell lung cancer 2 cm or less in size. World J Surg 31(2):314–317
Yap C, Schiepers C, Fishbein M, Phelps M, Czernin J (2002) FDG-PET imaging in lung cancer: How sensitive is it for bronchioloalveolar carcinoma? Eur J Nucl Med 29(9):1166–1173
Kim TJ, Park CM, Goo JM, Lee KW (2012) Is there a role for FDG PET in the management of lung cancer manifesting predominantly as ground-glass opacity? Am J Roentgenol 198(1):83–88
Okada M, Nakayama H, Okumura S, Daisaki H, Adachi S, Yoshimura M et al (2011) Multicenter analysis of high-resolution computed tomography and positron emission tomography/computed tomography findings to choose therapeutic strategies for clinical stage IA lung adenocarcinoma. J Thorac Cardiovasc Surg 141(6):1384–1391
Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M et al (2012) Prediction of pathologic node-negative clinical stage IA lung adenocarcinoma for optimal candidates undergoing sublobar resection. J Thorac Cardiovasc Surg 144(6):1365–1371
Chun EJ, Lee HJ, Kang WJ, Kim KG, Goo JM, Park CM et al (2009) Differentiation between malignancy and inflammation in pulmonary ground-glass nodules: the feasibility of integrated 18F-FDG PET/CT. Lung Cancer 65(2):180–186
Volpi S, Ali JM, Tasker A, Peryt A, Aresu G, Coonar AS (2018) The role of positron emission tomography in the diagnosis, staging and response assessment of non-small cell lung cancer. Ann Transl Med 6(5):95–95
Deppen SA, Blume JD, Kensinger CD, Morgan AM, Aldrich MC, Massion PP et al (2014) Accuracy of FDG-PET to diagnose lung cancer in areas with infectious lung disease: a meta-analysis. JAMA - J Am Med Assoc 312(12):1227–1236
Montagne F, Guisier F, Venissac N, Baste JM. (2021) The role of surgery in lung cancer treatment: Present indications and future perspectives—state of the art. Vol. 13, Cancers. MDPI AG
Kepka L, Socha J. (2015) PET-CT limitations in early stage non-small cell lung cancer: To whom more aggressive approach in radiotherapy and surgery should be directed? Vol. 7, Journal of Thoracic Disease. Pioneer Bioscience Publishing. p. 1887–90
Jones T, Townsend D (2017) History and future technical innovation in positron emission tomography. J Med Imaging 4(1):011013
Kitajima K, Doi H, Kanda T, Yamane T, Tsujikawa T, Kaida H, et al. (2016) Present and future roles of FDG-PET/CT imaging in the management of lung cancer. Vol. 34, Japanese Journal of Radiology. Springer Tokyo, p. 387–99
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript. Please note that this work was done at UCLH/UCL, which received a proportion of funding from the UK’s Department of Health’s NIHR Biomedical Centres (BRC UCLH 2012) funding scheme.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. The idea for the article originated from Francesco Fraioli. Literature search, data collection and analysis were performed by Zoltan Kaplar. The first draft of the manuscript was written by Zoltan Kaplar and Francesco Fraioli. All authors commented on the previous versions of the manuscript. All authors read, revised, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
There are no conflicts of interest.
Ethical approval
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kaplar, Z., Essa, N.B., Balaji, N. et al. Conventional CT and PET/CT imaging in the evaluation and management of subsolid pulmonary nodules: an overview of the literature and author recommendations. Clin Transl Imaging 11, 413–420 (2023). https://doi.org/10.1007/s40336-023-00576-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-023-00576-2