Abstract
The Society of Nuclear Medicine and Molecular Imaging (SNMMI), founded in 1954, is an international scientific and professional organization with a purpose to promote the science, technology, and practical application of nuclear medicine. The European Association of Nuclear Medicine (EANM), founded in 1985, is a nonprofit professional medical association with a purpose to facilitate international communication among individuals in nuclear medicine pursuing clinical and academic excellence. Members of the SNMMI and EANM are physicians, technologists, and scientists who specialize in the research and practice of nuclear medicine. The SNMMI and EANM will periodically publish new guidelines for nuclear medicine practice to further advance the science of nuclear medicine and improve patient care. Existing standards/guidelines will be reviewed for revision or renewal, as appropriate. Each standard/guideline, representing a policy statement by the SNMMI/EANM, has undergone a thorough review, and represents an expert consensus. The SNMMI and EANM recognize that the safe and effective use of diagnostic nuclear medicine imaging requires specific training and skills, as described in each document. These standards/guidelines are educational resources designed to assist practitioners in providing appropriate nuclear medicine care for patients. They are consensus documents, and are not mandatory provisions or requirements of practice. They are not intended, nor should they be used, to establish a legal standard of care. For these reasons and those set forth below, the SNMMI and the EANM cautions against the use of these standards/guidelines in litigation procedures that call into question the clinical decisions of a practitioner. The ultimate judgment regarding the appropriateness and propriety of any specific procedure or course of action must be made by medical professionals, taking into account the unique context of each case. Thus, there is no implication that action differing from what is detailed in these standards/guidelines, on its own, is below the standard of care. On the contrary, a conscientious practitioner may responsibly adopt a course of action different from that set forth in the standards/guidelines when, based on the reasonable judgment of the practitioner, such course of action is warranted based on the condition of the patient, limitations of available resources, or advances in knowledge or technology subsequent to publication of the standards/guidelines. Practicing medicine involves not only the science, but also the art of dealing with the prevention, detection, diagnosis, and treatment of disease. The variety and complexity of human conditions make it impossible for general guidelines to consistently allow for an accurate diagnosis to be reached or a specific treatment response to be predicted. Therefore, it should be recognized that adhering to these standards/guidelines does not ensure a successful outcome. All that should be expected is that a practitioner follows a reasonable course of action based on their level of training, the current landscape of knowledge, the resources at their disposal, and the needs/context of the particular patient being treated. The purpose of this document is to provide nuclear medicine physicians, radiologists, and other clinicians with guidelines for the recommendation, performance and interpretation of 99mTc-dimercaptosuccinic acid renal cortical scintigraphy ([99mTc] Tc-DMSA scintigraphy) in pediatric patients. These recommendations represent the expert opinions of experienced leaders in this field, and these recommendations are not all supported by a high level of evidence. Further studies are required to have evidence-based recommendations for the application of [99mTc] Tc-DMSA renal cortical scintigraphy in pediatrics. This guideline summarizes the views of the SNMMI Renal Cortical Scintigraphy in Children Working Group and the EANM Pediatrics Committee. It reflects recommendations for which the SNMMI and EANM cannot be held responsible. The recommendations should be taken into context of good practice of nuclear medicine and do not substitute for national and international legal or regulatory provisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
99mTc- dimercaptosuccinic acid ([99mTc] Tc-DMSA) is the radiopharmaceutical of choice for functional imaging of the renal parenchyma. Uptake of [99mTc] Tc-DMSA reflects regional blood flow and functional renal cortex. Therefore, [99mTc] Tc-DMSA scintigraphy provides an accurate method for assessing differential renal function and evaluating a renal regional parenchymal function, with a high sensitivity for detection of the cortical defects in a variety of acquired and congenital renal abnormalities [1, 2]. [99mTc]Tc-DMSA scintigraphy is more sensitive than ultrasound for the detection of renal cortical defects [3,4,5]. However, findings on [99mTc] Tc-DMSA scintigraphy are non-specific. Thus, the combined use of [99mTc] Tc-DMSA scintigraphy and ultrasound allows for superior diagnostic accuracy. SPECT/CT with low dose CT of the kidneys can be an alternative diagnostic approach [6, 7]. However, further studies are needed to weigh the risk-benefit relationship of added ionizing radiation versus the benefit of CT correlation.
At the time of writing this guideline, the evidence regarding using [99mTc] Tc-DMSA for evaluation of absolute renal function was limited. Therefore, a working group was created to investigate this.
Animal studies investigating [99mTc] Tc-DMSA scintigraphy for the detection of both acute pyelonephritis and subsequent cortical scars have validated it as an accurate technique when compared to other cross-sectional modalities [8,9,10,11,12,13,14]. Contrast-enhanced computed tomography (CT) has a similar sensitivity and specificity to [99mTc] Tc-DMSA scintigraphy for detecting acute pyelonephritis, however, it is associated with higher exposure to ionizing radiation, and risk of contrast reaction and contrast-induced nephropathy. Magnetic resonance imaging (MRI) including diffusion-weighted MRI is a promising modality for visualizing pyelonephritis, with no ionizing radiation exposure and no need for iodinated contrast materials, but it typically requires sedation or general anesthesia in younger children [15, 16]. Gadolinium-based MRI contrast agents are also associated with the risk of contrast reaction and contrast-induced nephropathy.
The deficits in renal cortical function seen in acute pyelonephritis may recover without scarring if the infection is detected early and appropriately treated [17]. [99mTc] Tc-DMSA scintigraphy is the method of choice in monitoring for sequelae of acute pyelonephritis, with the minimum time interval being approximately six months following acute infection to consider cortical defects as permanent renal scarring [18,19,20]. Standard use of [99mTc] Tc-DMSA scan in the acute setting is debated [21,22,23]. Some argue that it aids in accurate diagnosis, as clinical signs and symptoms can be diverse and nonspecific to renal parenchymal infection, particularly in infants [24]. [99mTc]Tc-DMSA scintigraphy in the acute setting also helps to risk stratify those who may go on to develop permanent sequelae of pyelonephritis such as parenchymal scarring, chronic renal failure, and hypertension [25, 26]. Others postulate that [99mTc] Tc-DMSA scintigraphy is unnecessary in the acute setting as only permanent scarring contributes to clinical decision making [20, 27].
The use of renal cortical scintigraphy can be particularly helpful in a clinical management pathway for urinary tract infection that does not include routine evaluation for vesicoureteral reflux (VUR); detection of acute pyelonephritis increases the likelihood that VUR is present. Higher grades of VUR are associated with a greater risk of developing pyelonephritis; however, acute pyelonephritis can occur in the absence of demonstrable vesicoureteral reflux [28]. Some believe that a normal [99mTc]Tc-DMSA scan in the acute setting is helpful, as evaluation for VUR may not be necessary since only reflux sufficiently severe to cause pyelonephritis will require prophylaxis/treatment [27, 29,30,31,32,33]. Since renal scarring can occur in patients with pyelonephritis without VUR, and the outcome of VUR also depends on the patient characteristics, and not only on the grade of VUR, the imaging approach to pyelonephritis has in many places shifted toward a “top–down” that prioritizes detection of pyelonephritis, and away from “bottom–up” approach that prioritizes detection of VUR [34,35,36,37,38].
Goals
The goal of this document is to provide a harmonized guideline for the performance and interpretation of [99mTc] Tc-DMSA renal cortical scintigraphy in pediatric patients.
Definitions
-
[99mTc]Tc-DMSA is a combination of dimercaptosuccinic acid, a pharmaceutical that is taken up by the proximal convoluted tubules directly from the peritubular vessels or by endocytosis, and technetium-99 m, a radionuclide [39,40,41,42]
-
[99mTc]Tc-DMSA scanning involves the intravenous injection of [99mTc]Tc-DMSA followed by planar imaging using high-, or ultra-high-resolution collimator, when possible with additional pinhole collimator planar imaging or single-photon emission computed tomography (SPECT) [2]
Clinical indications
The following is a list of indications for [99mTc] Tc-DMSA scintigraphy in children:
-
Detection of permanent renal parenchymal scarring at least six months following an acute urinary tract infection.
-
Detection of acute pyelonephritis.
-
Detection of parenchymal damage after trauma.
-
Characterization of structural renal abnormalities: e.g. solitary kidney, duplex kidney, small kidney, dysplastic kidney, horseshoe kidney, and pseudo-horseshoe kidney.
-
Detection of ectopic renal tissue, including cross-fused renal ectopia
-
Quantitation of each kidney’s contribution to total renal function (i.e. differential renal function).
-
Confirmation of non-functional multicystic dysplastic kidney.
-
Evaluation of unexplained hypertension when there is clinical suspicion for renal disease such as dysplasia or scarring
-
Evaluation of renal parenchymal function in patients with renovascular hypertension before and after revascularization procedures.
-
Renal parenchymal function regional assessment in patients with complex renal calculi before and after treatment.
-
Surgical decision-making for ureteropelvic junction obstruction (UPJO) or refractory VUR based on differential renal function:
-
Nephrectomy is usually performed for a very poorly functioning kidney due to the increased risk of hypertension and infection.
-
Otherwise pyeloplasty is performed for UPJO, and ureteral reimplantation for refractory VUR.
-
Evaluation of renal parenchyma when there is an allergy to iodinated CT contrast, and MRI is unavailable/contraindicated.
Qualifications and responsibilities of personnel
All clinicians and personnel involved in performing and interpreting [99mTc] Tc-DMSA scintigraphy should be qualified in accordance with the applicable regional laws. Responsibilities afforded to various individuals involved in the performance and interpretation of these scans should be documented in standard operating procedures. The study should be supervised and interpreted by a nuclear medicine physician or diagnostic radiologist with specific training in nuclear medicine. The [99mTc] Tc-DMSA scintigraphy should be performed by a qualified registered/certified nuclear medicine technologist. Please refer to the following documents for further details: Performance Responsibility and Guidelines for Nuclear Medicine Technologists 3.1 (https://www.eanm.org/content-eanm/uploads/2017/02/Advanced-Performance-and-Responsibility-Guidelines.pdf) and the EANM Benchmark Document Nuclear Medicine Technologists ‘Competencies (http://www.eanm.org/content-eanm/uploads/2016/11/EANM_2017_TC_Benchmark.pdf or SNMMI Nuclear Medicine Technologist Scope of Practice and Performance Standards (https://www.eanm.org/content-eanm/uploads/2017/02/Advanced-Performance-and-Responsibility-Guidelines.pdf) [43, 44] [99mTc]Tc-DMSA scanning must adhere to international dosimetry and radiation precautions for patients and staff.
Procedure/specifications of the examination
Request
A written or electronic request for [99mTc] Tc-DMSA scintigraphy should be initiated by a physician or otherwise appropriately licensed health care practitioner. The nuclear medicine physician/technologist and the referring practitioner should collaborate closely to achieve a safe, and appropriate study. The request should contain sufficient clinical information to justify the examination and aid its interpretation. The request should specify the clinical presentation (clinical signs and symptoms), the purpose of the study (clinical indication), any relevant past medical history (e.g. known structural abnormalities, previous history of pyelonephritis, and date of most recent urinary tract infection (UTI)). History of previous relevant studies (e.g. fluoroscopy studies, ultrasound data, previous radionuclide imaging), previous interventions/therapies (e.g. prior surgery to the urinary tract), medications, allergies, and whether sedation or analgesia will be necessary (and any complications experienced with previous sedation) are also useful for an appropriate study. Structural renal abnormalities may dictate the need for additional views, attenuation correction, and/or appropriate timing for imaging (e.g. hydronephrosis, duplex kidney, and ectopic kidney).
Patient preparation and Precautions
Patient preparation
Parents/caregivers and children should receive detailed information, both written and verbal, about the procedure in advance of their appointment. This includes the clinical indication for the study, the waiting period between injection and image acquisition, and the imaging duration. No patient preparation is required if sedation is not being used for the study.
Sedation
High-resolution pinhole collimation and Single Photon Emission Computed Tomography (SPECT) require prolonged imaging times of at least 20–30 min. Motion impairs visualization of renal cortical defects. Thus, sedation may be required particularly in younger children or uncooperative older children who must remain motionless for a prolonged period of time. However, in the majority of cases, other strategies can be successfully employed to achieve immobilization during the acquisition, and circumvent the need for sedation. By creating an appropriate child-friendly environment, with cooperation between parents/caregivers, child life/play specialists, and other properly trained staff, a successful [99mTc] Tc-DMSA scanning can be achieved in almost all cases. Some infants and young children will fall asleep if kept awake for several hours and then fed just prior to the imaging. Other distraction techniques such as a video or music during scanning can also be useful to avoid sedation. If sedation is required, informed consent, appropriate patient preparation, and pre-sedation evaluation are necessary [2, 45,46,47,48] Further details on pediatric sedation can be found in the Society of Nuclear Medicine Procedure Guideline for Pediatric Sedation in Nuclear Medicine and the guidelines published by the American Academy of Pediatrics [46, 49].
Preparation prior to injection of the radiopharmaceutical
Before injection of the radiopharmaceutical, the procedure should be explained to caregivers and children old enough to understand. A topical anesthetic cream may be used at the discretion of the patient and their caregiver [50]. When used, it should be applied to the injection site 30–60 min prior to accessing the vein. Continuous open communication and reassurance while explaining each step of the procedure are integral to cooperation and successful intravenous radiopharmaceutical injection.
Radiopharmaceutical
Radionuclide: Technetium-99 m (99mTc)
Pharmaceutical: Dimercaptosuccinic acid (DMSA)
Radiopharmaceutical: [99mTc]Tc-DMSA
[99mTc]Tc-DMSA is the primary radiopharmaceutical available for renal cortical imaging. [99mTc]Tc-DMSA is taken up from peritubular vessels directly by tubular cells in the pars recta [40]. Two hours after injection, 40–65% of the administered activity is present in the renal cortex. Alteration of biodistribution of [99mTc] Tc-DMSA (higher activity in bones, stomach and intestine) has been reported in animal models treated with cytotoxic drugs such as sodium methotrexate [51].
Alternative radiopharmaceuticals
If [99mTc] Tc-DMSA is not available another radiotracer, 99mTc-glucoheptonate ([99mTc] Tc-GH), may be used. [99mTc] Tc-GH partially binds to renal tubular cells, but fell out of favor as only 10–20% of the injected dose is present in the proximal convoluted tubules of the cortex two hours after injection [14, 52,53,54]. An important disadvantage of [99mTc] Tc-GH is the possible accumulation and stasis of activity in the collecting system, particularly in the hydronephrotic kidney. This may limit visualization of the renal cortex and accurate evaluation of differential function. The dynamic radiotracers 99mTc-diethylenetriaminepentaacetic acid (([99mTc] Tc-DTPA), 99mTc-mercaptoacetyltriglycine ([99mTc] Tc-MAG3) and 99mTc-ethylenedicysteine ([99mTc] Tc-EC) are in general not recommended for imaging the renal cortex. They have a high rate of excretion, thus giving less accurate information regarding regional cortical abnormalities—especially when the parenchymal defect is small.
Administered activity
The administered activity should be the lowest possible that produces an image of sufficient quality for interpretation. The administered activity should follow the 2016 Update of the North American Consensus Guidelines for Pediatric Administered Radiopharmaceutical Activities or the 2016 EANM pediatric Dosage Card [55, 56]. The EANM pediatric Dosage Card can be found at “https://www.eanm.org/content-eanm/uploads/2017/01/EANM_Dosage_Card_040214.pdf”. The North American Guidelines for Pediatric Nuclear Medicine for high-quality images at low radiation dose can be found at “http://snmmi.files.cms-plus.com/docs/GoWithGuidelines_files/ImageGentlyPoster_2017.pdf”. The radiation effective dose per examination, irrespective of age, is approximately 1 mSv, provided that the dose is correctly adapted to body size (Table 1) [15, 57, 58].
Protocol/image acquisition
Imaging Timing
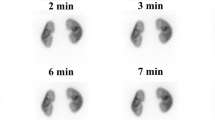
Imaging typically is performed approximately 2–3 h after radiopharmaceutical injection. In the setting of poor renal function or clearance, a longer delay may be required to increase renal uptake and decrease background activity, thus improving lesion detectability. If there is a severely obstructed collecting system, imaging may be delayed up to 24 h after injection for quantitation of differential renal function [48].
Imaging Techniques
Imaging is usually performed with the patient in the supine position to minimize renal depth difference and patient movement. To further reduce movement, consideration should be given to supporting the patient with sandbags and Velcro straps, or placing them in a vacuum cushion; infants can be swaddled. For planar and SPECT images, a high or ultra-high-resolution collimator is used. SPECT acquisition is suggested for all patients, if possible. [61, 62]. When performing [99mTc] Tc-DMSA scan in infants, pinhole-collimator images are acquired in lieu of SPECT. When using a pinhole collimator each kidney should be imaged separately to obtain magnified, high-spatial resolution images. The optimal size of the pinhole aperture is 3–4 mm.
Image Acquisition
-
1.
The patient should be encouraged to void prior to the scanning and before leaving the department (changing the diaper for younger children). Posterior, anterior, and posterior oblique images of both kidneys are acquired for 300,000–500,000 counts using a high or ultra-high-resolution parallel-hole collimator in a 128 × 128 or 256 × 256 matrix format. It is recommended that anterior and posterior images are acquired simultaneously on a dual-head gamma camera. The geometric mean differential function using anterior and posterior images can be useful when the kidneys are not in the normal position. A zoom acquisition is recommended, varying between 1 and 2 as a function of body size, potentially requiring increased acquisition time. An alternative method is to acquire data in dynamic mode over a given pre-set time and reframe to a single image, after correcting for movement and discarding blurred frames. The matrix and minimal counts during acquisition must be maintained in order to utilize this alternative approach.
-
2.
Posterior and posterior oblique views using a pinhole collimator separately for each kidney are useful for infants and smaller children to obtain high-quality, high-resolution images. The image count is usually 150 000 counts (approximately 6–8 min per image) using a 256 ×256 matrix format. This provides higher sensitivity in the detection of smaller cortical defects.
-
3.
When measuring geometric mean differential function in horseshoe or pelvic kidneys, both anterior and posterior planar images should be acquired to account for renal tissue located anterior to the spine and pelvic bones. SPECT images should also be acquired when possible. In patients with a history of a high congenital spinal defect (e.g. meningomyelocele) with horseshoe or pseudo-horseshoe kidneys, the examination should be performed with the patient in prone or lateral decubitus position, as their kidneys lie deep within the kyphotic fossa. If there is a clinical question regarding whether there is an ectopic kidney or not, the entire abdomen and pelvis should be included in the field of view.
-
4.
SPECT imaging requires 360 of sampling, typically on a 128 × 128 matrix with a multi-head camera. 120 views in total (3° spacing) with 15–20 s per view can be used for most cameras. Alternative angular sampling / view times can be used with more advanced reconstructions.
Special Considerations
In rare instances, the presence of VUR or retained urinary activity in the renal collecting system with the use of cortical agents can interfere with the calculation of differential renal function. Retained activity in the collecting system can also be caused by a distended neuropathic bladder resulting in backpressure—this can be prevented by catheterization and continuous drainage. If the collecting system is capacious or the system is obstructed, a diuretic such as furosemide may be administered prior to delayed imaging, or the patient may return for delayed imaging up to 24 h following radiopharmaceutical injection. SPECT combined with a low dose CT may also be useful for a more accurate evaluation of differential function or scarring if the appearance on planar imaging is affected by patient body habitus or abnormal kidney position [6].
Patients with renal tubular acidosis demonstrate reduced tubular concentration of [99mTc] Tc-DMSA and increased urinary excretion. Patients with tubular defects such as those seen in Fanconi’s syndrome or nephronophthisis may have poor renal visualization due to defective binding of the radioisotope within renal tubular cells and urinary excretion [63].
More accurate measurement of differential renal function is achieved using both anterior and posterior views and the geometric mean method. The geometric mean method should be used when significant hydronephrosis or ectopic renal tissue (e.g., ptotic kidney, horseshoe kidney, cross-fussed renal ectopia) is present. In hydronephrotic kidneys, late images (4–24 h) or furosemide administration may result in improved parenchymal visualization. A differential function may be overestimated in a hydronephrotic kidney due to the enlarged kidney being closer in position to the camera, as well as due to retention of activity in the pelvicalyceal system if delayed images are not captured [64]. When available, dedicated pediatric beds/chairs should be used for infants and young children. These beds/chairs allow closer proximity of the gamma camera detectors in the lateral projections of SPECT, significantly improving spatial resolution. Several attempts have been made to quantify the DMSA uptake in the kidneys using both SPECT and planar images but these methods are not widely used or reported and require further validation [65, 66].
SPECT acquisition can be useful for the detection of small defects; particularly for patients with ectopic or transplanted kidneys whereby boney structures, superimposed bowel, and patient-detector distance can make it difficult to evaluate the kidney profile using planar or pinhole imaging.
Processing
Processing
For calculation of differential (relative, or split) renal function, it is recommended that region of interest (ROI) be drawn to include the entire kidney. The renal pelvis may be excluded from ROI if desired. Background activity correction should be done by subtracting the background activity close to the kidney from the renal activity, taking care to exclude renal parenchyma or any areas of increased tracer activity. In most cases of routine clinical evaluation, differential function based on only the posterior view is sufficient, and no attenuation correction is required [67]. Geometric mean differential function, based on both anterior and posterior views, should be used when there is severe hydronephrosis or other anatomical abnormality (i.e., pelvic or other ectopic kidney, horseshoe kidney or another fusion anomaly, etc.). In the context of a pelvic kidney, measurement of differential function has reduced accuracy, even when using the geometric mean, due to photon attenuation from the bony pelvis and asymmetric position and orientation of the kidneys. Nevertheless, measurement of differential function, done consistently in the same way every time in a given patient, can be helpful in monitoring renal function over time.
When available, it is recommended to use iterative reconstruction techniques such as an ordered subsets-expectation maximization (OSEM) algorithm or resolution recovery software [68]. For all [99mTc] Tc-DMSA studies, planar or SPECT, a grayscale image is recommended as an output rather than color images. Image intensity should be adapted to best differentiate the higher-intensity cortex of the kidney from the lower-intensity medulla, calyces, and vascular structures that comprise the central structures of the kidney.
Interpretation
Differential function (relative uptake)
After confirming that images were acquired with the correct protocol and are of acceptable quality, the differential renal function can be calculated. The differential function of one kidney compared to the other normally ranges from 50–50% to 45–55% [2, 57]. Results outside of this range may indicate renal pathology such as scarring, acute pyelonephritis, parenchymal atrophy, or hydronephrosis. On follow-up scans after a confirmed renal scarring when the patient has a subsequent UTI, the differential function may reduce on the scarred side with no new lesion. This may be due to the differential grown on the contra-lateral side. Values outside of the normal range may also be seen in the case of a rotated kidney or an uncomplicated unilateral duplex kidney [48]. Conversely, differential function values within the normal range may be seen in cases of chronic renal failure or bilateral renal atrophy/scarring [69].
Normal variants/sources of error
[99mTc]Tc-DMSA scanning is not performed in children without suspected pathology. The features discussed in this section may be found in a normal examination:
-
Kidney contours are typically rounded and there is a contrast between the hyperactive cortex and hypoactive central portions of the kidneys.
-
Kidney contour can be flat without suggesting a lesion—the lateral aspect of the superior half of the left kidney may be flattened due to the splenic impression, and the lateral margins may be flat in young children with triangular-shaped kidneys.
-
A rotated kidney can appear as a ‘slender’ kidney with a short transverse axis on the posterior view.
-
The transverse axis can be shorter at either the upper or the lower pole, giving rise to an appearance described as a ‘pear-shaped’ kidney.
-
-
- The renal poles, particularly the upper pole, can sometimes appear focally hypointense due to relatively higher activity in a column of Bertin in the adjacent renal midzone, or due to attenuation by the adjacent liver. The number and size of columns of Bertin vary between patients leading to the variable thickness of the renal cortex, which may cause some difficulty in interpreting images. Relative hyperintensity in midzone parenchyma can create the illusion of bipolar hypointensity.
-
A linear area of no tracer uptake, extending from the renal hilum into the parenchyma and visible on SPECT imaging only, may be seen: this represents an inter-renicular septum and should not be confused with a scar.
-
The presence of fetal lobulation or a junctional parenchymal defect (both anatomic variants) can be difficult to distinguish from scarring with renal scintigraphy alone, and ultrasound imaging may be required to make the distinction.
Abnormal patterns
Any areas of decreased to absent cortical activity should be noted and described in terms of number, size, location, shape, distinctness of margins and whether associated parenchymal volume loss or deformation of the renal contour is present [69].
Acute pyelonephritis may be evident as a single defect or multiple defects—there may be a regional increase in volume in an affected area, or a diffusely enlarged kidney with multiple defects visible. The cortical defect in the setting of acute pyelonephritis may demonstrate reduced or absent localization of tracer, with indistinct margins and no retraction deformity of the renal contour.
A mature cortical scar will appear as a photopenic defect with relatively well-defined margins, parenchymal volume loss, and focal retraction of the renal contour. Scarring may also manifest scintigraphically as cortical thinning, flattening, or a wedge or ovoid-shaped defect.
Differentiating acute pyelonephritis that will improve/heal versus permanent scarring is not always possible on [99mTc] Tc-DMSA scintigraphy. A larger hypointense area that is polar, does not deform the renal contours, and has indistinct margins is more likely to represent an acute infection that will likely heal. A photopenic area with localized retraction deformity of the renal contour and/or volume loss is more likely to represent permanent scarring. A focal defect from acute pyelonephritis takes a variable amount of time to resolve. Therefore, if assessing only for renal scarring, [99mTc]Tc-DMSA scan is suggested at a minimum of 6 months following the most recent UTI, at which time any focal cortical defects can be considered suspicious for scarring [18, 19, 70]. If the purpose of a [99mTc] Tc-DMSA scan is to confirm the diagnosis of acute pyelonephritis, the scan should be done during (or within two weeks from) the episode of acute infection. If this acute scan shows focal defect(s) a follow-up [99mTc] Tc-DMSA scan should be performed 6 months later to assess for resolution.
[99mTc]Tc-DMSA scintigraphy is also helpful in the evaluation of a dysplastic kidney. Usually, a dysplastic kidney is asymmetrically smaller with reduced or absent uptake. The uptake, if present, is mostly heterogeneous throughout the entire kidney or a portion of the kidney (in focal or segmental dysplasia) without a peripheral defect in renal contour [71]. These findings can be seen when there is no evidence of active infection at the time of imaging. Dysplastic kidneys are more prone to infection and scarring so it is possible for the two conditions to co-exist at the same timepoint. Ultrasound is a preferred modality to assess morphological abnormalities (e.g. loss of cortico-medullary differentiation, cystic or solid lesions) in dysplastic kidneys. [99mTc]Tc-DMSA scintigraphy, however, is useful to evaluate the differential function and to assess the contralateral kidney. Any scarring in the contralateral kidney should be managed appropriately to preserve its function [72, 73]. In the case of the congenital multicystic dysplastic kidney (MCDK), an entity that lacks functional renal tissue, tracer activity is completely absent.
Documentation/reporting
A generic report template is provided within the SNMMI guideline for general imaging, found here: http://snmmi.files.cms-plus.com/docs/General_Imaging_Version_6.0.pdf. The report is a tool for communication, and also acts as a legal document. It should answer the clinical question and be comprehensive. It should also be constructed and made available in a timely manner. Should findings come up during the interpretation that require immediate attention, the reporting physician should give a verbal report directly to the referring physician, with appropriate documentation (including the names of the physicians involved, the date, and the time).
Using a structured reporting system increases the comprehensiveness of the report and decreases the likelihood that important elements will be forgotten [74]. The following would be the suggested sections and elements for a structured report:
General information
-
a.
Study identification: procedure, date of the study.
-
b.
Clinical information: diagnosis, indication(s) for the study, history (including symptoms).
-
c.
Comparison exams: name and date of prior examinations related to the current examination (including previous fluoroscopy, ultrasound, and renal scintigraphy). If prior images are not available for direct comparison, but the report from a prior exam is available, state that correlation is made to this report.
Procedure description and imaging protocol
-
a.
Administered activity and route of administration of [99mTc]Tc-DMSA.
-
b.
Sedation/anesthesia procedures, if any.
-
c.
Time of imaging following radiopharmaceutical administration.
-
d.
Specific imaging protocol, including whether pinhole collimation or SPECT was used.
-
e.
If there were any problems that may affect the study quality, such as patient motion.
Body of report
-
a.
Description of findings: describe the position, size, and overall morphology of the functioning kidney tissue, report the differential renal function, indicate the location, size, and a number of areas of cortical defects, and any distinguishing features of acute pyelonephritis versus renal scarring.
-
b.
Any incidental findings should be reported.
-
c.
Comparison: the findings should be compared with the previous relevant studies.
-
d.
Limitations: the limitations, if any (e.g. renal failure, ectopic kidney, patient motion, etc.), and how they may affect the results of the study should be reported.
Impression
-
a.
The reporter's overall interpretation of the findings within the clinical context, with any applicable recommendations (e.g. for additional studies or alterations to treatment), specifically addressing the indication for the study.
-
b.
The clinical question should be addressed even if no abnormality is detected in the area related to the clinical question.
Finally, it is important to review the report to check for spelling and grammar, that all components of a structured report are included, and that the clinical question was adequately addressed.
Quality control and improvement
Before the patient leaves the department following the scan, it is imperative to evaluate the images for renal motion. Blurred or double renal contours generally represent patient movement. Internal renal architecture should be visualized. If air is introduced into the reaction vial, the DMSA complex may degrade. This manifests as decreased renal uptake and increased hepatic and background activity on the images. For quality control of [99mTc] Tc-DMSA renal cortical scintigraphy, see the ’quality control ’section of the American College of Radiology-Society of Pediatric Radiology Parameter for the Performance of Renal Scintigraphy (https://www.acr.org/-/media/ACR/Files/Practice-Parameters/RenalScint.pdf). For quality control of other equipment including computers, software, and monitors, see the SNMMI guideline for general imaging.
Safety, infection control, and patient education concerns
Studies showed that the effect of [99mTc] Tc-DMSA renal cortical scintigraphy is insufficient to create oxidative damage. DNA damage may occur via the direct impact of ionizing radiation which can be repaired again in a short period of time [75, 76]. See SNMMI guideline for general imaging and acr position statement on quality control and improvement, safety, infection control and patient education (https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Quality-Control-and-Improvement).
References
Mandell GA, Eggli DF, Gilday DL et al (1997) Procedure guideline for renal cortical scintigraphy in children. Society of nuclear medicine. J Nucl Med 38(10):1644–1646
Piepsz A, Blaufox MD, Gordon I et al (1999) Consensus on renal cortical scintigraphy in children with urinary tract infection. scientific committee of radionuclides in nephrourology. Semin Nucl Med 29(2):160–174. https://doi.org/10.1016/s0001-2998(99)80006-3
Ayazi P, Mahyar A, Noroozian E, Esmailzadehha N, Barikani A (2015) Comparison of renal ultrasonography and dimercaptosuccinic acid renal scintigraphy in febrile urinary tract infection. Le Infez Med 23(4):323–329 (PMID: 26700082)
Finkelstein JB, Rague JT, Chow J et al (2020) Accuracy of ultrasound in identifying renal scarring as compared to DMSA scan. Urology 138:134–137. https://doi.org/10.1016/j.urology.2020.01.019
Marceau-Grimard M, Marion A, Côté C, Bolduc S, Dumont M, Moore K (2017) Dimercaptosuccinic acid scintigraphy vs. ultrasound for renal parenchymal defects in children. Can Urol Assoc J 11(8):260–264. https://doi.org/10.5489/cuaj.4257 (J l’Association des Urol du Canada)
Reichkendler MH, Berg RMG, de Nijs R, Nørgaard H, Schmidt IM, Borgwardt L (2020) Planar scan vs. SPECT/low-dose CT for estimating split renal function by (99m)Tc-DMSA scintigraphy in children. Eur J Nucl Med Mol Imaging 47(3):729–733. https://doi.org/10.1007/s00259-019-04575-2
Einarsdóttir HS, Berg RMG, Borgwardt L (2020) Interrater reliability of 99mTc-DMSA scintigraphy performed as planar scan vs. SPECT/low dose CT for diagnosing renal scarring in children. Diagnostics 10(12):1101. https://doi.org/10.3390/diagnostics10121101
Wikstad I, Hannerz L, Karlsson A, Eklof AC, Olling S, Aperia A (1990) 99mTechnetium dimercaptosuccinic acid scintigraphy in the diagnosis of acute pyelonephritis in rats. Pediatr Nephrol 4(4):331–334. https://doi.org/10.1007/bf00862511
Rushton HG, Majd M, Chandra R, Yim D (1988) Evaluation of 99mtechnetium-dimercapto-succinic acid renal scans in experimental acute pyelonephritis in piglets. J Urol 140(5 Pt 2):1169–1174. https://doi.org/10.1016/s0022-5347(17)41992-6
Majd M, Rushton HG, Chandra R, Andrich MP, Tardif CP, Rashti F (1996) Technetium-99m-DMSA renal cortical scintigraphy to detect experimental acute pyelonephritis in piglets: comparison of planar (pinhole) and SPECT imaging. J Nucl Med 37(10):1731–1734 (PMID: 8862320)
Rossleigh MA, Farnsworth RH, Leighton DM, Yong JL, Rose M, Christian CL (1998) Technetium-99m dimercaptosuccinic acid scintigraphy studies of renal cortical scarring and renal length. J Nucl Med 39(7):1280–1285 (PMID: 9669411)
Majd M, Nussbaum Blask AR, Markle BM et al (2001) Acute pyelonephritis: comparison of diagnosis with 99mTc-DMSA, SPECT, spiral CT, MR imaging, and power Doppler US in an experimental pig model. Radiology 218(1):101–108. https://doi.org/10.1148/radiology.218.1.r01ja37101
Craig JC, Wheeler DM, Irwig L, Howman-Giles RB (2000) How accurate is dimercaptosuccinic acid scintigraphy for the diagnosis of acute pyelonephritis? A meta-analysis of experimental studies. J Nucl Med 41(6):986–993 (PMID: 10855622)
Craig JC, Irwig L, Ford M et al (2000) Reliability of DMSA for the diagnosis of renal parenchymal abnormality in children. Eur J Nucl Med 27(11):1610–1616. https://doi.org/10.1007/s002590000349
Craig W, Wagner B, Travis M (2008) Pyelonephritis: radiologic-pathologic review. Radio Gr 28:255–276. https://doi.org/10.1148/rg.281075171
Sriman R, Venkatesh K, Mathew C, Pankaj M, Shankar R (2020) Validity of diffusion-weighted magnetic resonance imaging in the evaluation of acute pyelonephritis in comparison with contrast-enhanced computed tomography. Pol J Radiol 85:e137–e143. https://doi.org/10.5114/pjr.2020.93669
Paintsil E (2013) Update on recent guidelines for the management of urinary tract infections in children: the shifting paradigm. Curr Opin Pediatr 25(1):88–94. https://doi.org/10.1097/MOP.0b013e32835c14cc
Saadeh SA, Mattoo TK (2011) Managing urinary tract infections. Pediatr Nephrol 26(11):1967–1976. https://doi.org/10.1007/s00467-011-1801-5
Jakobsson B, Svensson L (1997) Transient pyelonephritic changes on 99mTechnetium-dimercaptosuccinic acid scan for at least five months after infection. Acta Paediatr 86(8):803–807. https://doi.org/10.1111/j.1651-2227.1997.tb08601.x
Lim R (2009) Vesicoureteral reflux and urinary tract infection: evolving practices and current controversies in pediatric imaging. AJR Am J Roentgenol 192(5):1197–1208. https://doi.org/10.2214/AJR.08.2187
Stein R, Dogan HS, Hoebeke P et al (2015) Urinary tract infections in children: EAU/ESPU guidelines. Eur Urol 67(3):546–558. https://doi.org/10.1016/j.eururo.2014.11.007
Siomou E, Giapros V, Fotopoulos A et al (2009) Implications of 99mTc-DMSA scintigraphy performed during urinary tract infection in neonates. Pediatrics 124(3):881–887. https://doi.org/10.1542/peds.2008-1963
Mantadakis E, Vouloumanou EK, Georgantzi GG, Tsalkidis A, Chatzimichael A, Falagas ME (2011) Acute Tc-99m DMSA scan for identifying dilating vesicoureteral reflux in children: a meta-analysis. Pediatrics 128(1):e169–e179. https://doi.org/10.1542/peds.2010-3460
Riccabona M (2016) Imaging in childhood urinary tract infection. Radiol Med 121(5):391–401. https://doi.org/10.1007/s11547-015-0594-1
Mandell GA (1997) Economic issue in pediatric nuclear medicine: cortical scanning of acute pyelonephritis. Q J Nucl Med 41(4):302–308 (PMID: 9542421)
Jakobsson B, Nolstedt L, Svensson L, Soderlundh S, Berg U (1992) 99mTechnetium-dimercaptosuccinic acid scan in the diagnosis of acute pyelonephritis in children: relation to clinical and radiological findings. Pediatr Nephrol 6(4):328–334. https://doi.org/10.1007/bf00869725
Moorthy I, Easty M, McHugh K, Ridout D, Biassoni L, Gordon I (2005) The presence of vesicoureteric reflux does not identify a population at risk for renal scarring following a first urinary tract infection. Arch Dis Child 90(7):733–736. https://doi.org/10.1136/adc.2004.057604
Montini G, Zucchetta P, Tomasi L et al (2009) Value of imaging studies after a first febrile urinary tract infection in young children: data from Italian renal infection study 1. Pediatrics 123(2):e239–e246. https://doi.org/10.1542/peds.2008-1003
Hansson S, Dhamey M, Sigstrom O et al (2004) Dimercapto-succinic acid scintigraphy instead of voiding cystourethrography for infants with urinary tract infection. J Urol 172(3):1071–1074. https://doi.org/10.1097/01.ju.0000135337.71154.60
Preda I, Jodal U, Sixt R, Stokland E, Hansson S (2007) Normal dimercaptosuccinic acid scintigraphy makes voiding cystourethrography unnecessary after urinary tract infection. J Pediatr 151(6):581–584. https://doi.org/10.1016/j.jpeds.2007.05.008
Tseng M-H, Lin W-J, Lo W-T, Wang S-R, Chu M-L, Wang C-C (2007) Does a normal DMSA obviate the performance of voiding cystourethrography in evaluation of young children after their first urinary tract infection? J Pediatr 150(1):96–99. https://doi.org/10.1016/j.jpeds.2006.09.028
Fouzas S, Krikelli E, Vassilakos P, Gkentzi D, Papanastasiou DA, Salakos C (2010) DMSA scan for revealing vesicoureteral reflux in young children with urinary tract infection. Pediatrics 126(3):e513–e519. https://doi.org/10.1542/peds.2009-3635
Balestracci A, Montecuco M, Serviddio C et al (2019) Role of Late DMSA Renal Scan in Detecting High-Grade Vesicoureteral Reflux. Indian J Pediatr 86(9):784–789. https://doi.org/10.1007/s12098-019-02917-4
Müller L-SO (2011) Imaging in urinary tract infection: top–down or down–up? Pediatr Radiol 41(1):96–98. https://doi.org/10.1007/s00247-011-2052-0
Jang KM, Lim MH, Park YH, Kim S (2017) Clinical efficacy of a top–down approach for children with a first febrile urinary tract infection. Child Kidney Dis 21(2):114–120. https://doi.org/10.3339/jkspn.2017.21.2.114
Hardy RD, Austin JC (2008) DMSA renal scans and the top–down approach to urinary tract infection. Pediatr Infect Dis J 27(5):476–477. https://doi.org/10.1097/INF.0b013e318168d26f
Prasad MM, Cheng EY (2012) Radiographic evaluation of children with febrile urinary tract infection: bottom–up, top-down, or none of the above.? Adv Urol 2012:1–8. https://doi.org/10.1155/2012/716739 (716739)
Pohl HG, Belman AB (2009) The “top–down” approach to the evaluation of children with febrile urinary tract infection. Adv Urol. https://doi.org/10.1155/2009/783409 (783409)
Dhull RS, Joshi A, Saha A (2018) Nuclear imaging in pediatric kidney diseases. Indian Pediatr 55(7):591–597 (PMID: 30129542)
Muller-Suur R, Gutsche HU (1995) Tubular reabsorption of technetium-99m-DMSA. J Nucl Med 36(9):1654–1658 (PMID: 7658227)
Willis KW, Martinez DA, Hedley-Whyte ET, Davis MA, Judy PF, Treves S (1977) Renal localization of 99mTc-stannous glucophetonate and 99mTc-stannous dimercaptosuccinate in the rat by frozen section autoradiography. The efficiency and resolution of technetium-99m. Radiat Res 69(3):475–488 (PMID: 322190)
Weyer K, Nielsen R, Petersen SV, Christensen EI, Rehling M, Birn H (2013) Renal uptake of 99mTc-dimercaptosuccinic acid is dependent on normal proximal tubule receptor-mediated endocytosis. J Nucl Med 54(1):159–165. https://doi.org/10.2967/jnumed.112.110528
Fragoso Costa P, Santos A, Testanera G (2017) An insight into the EANM technologist committee benchmark document on nuclear medicine technologists’ competencies. Eur J Nucl Med Mol Imaging 44(9):1604–1606. https://doi.org/10.1007/s00259-017-3741-1
(1998) Performance and responsibility guidelines for the nuclear medicine technologist: 1998 revision. Society of Nuclear Medicine-Technologists. J Nucl Med Technol 26(1):45–49 (PMID: 9549694)
Pintelon H, Dejonckheere M, Piepsz A (1997) Pediatric nuclear medicine: a practical approach. Q J Nucl Med 41(4):263–268 (PMID: 9542417)
Pintelon H, Jonckheer MH, Piepsz A (1994) Paediatric nuclear medicine procedures: routine sedation or management of anxiety? Nucl Med Commun 15(8):664–666. https://doi.org/10.1097/00006231-199408000-00012
Ljung B (1997) The child in diagnostic nuclear medicine. Eur J Nucl Med 24(6):683–690. https://doi.org/10.1007/bf00841410
Gordon I, Evans K, Peters AM et al (1987) The quantitation of 99Tcm-DMSA in paediatrics. Nucl Med Commun 8(8):661–670. https://doi.org/10.1097/00006231-198708000-00008
Cote CJ, Wilson S (2019) Guidelines for monitoring and management of pediatric patients before, during, and after sedation for diagnostic and therapeutic procedures. Pediatrics 143(6):e20191000. https://doi.org/10.1542/peds.2019-1000
Kohli ML, Vali R, Amirabadi A et al (2019) Procedural pain reduction strategies in paediatric nuclear medicine. Pediatr Radiol 49(10):1362–1367. https://doi.org/10.1007/s00247-019-04462-w
Jankovic DLJ, Djokic DDJ (2005) Alteration of the organ uptake of the (99m)Tc radiopharmaceuticals, (99m)Tc-DPD, (99m)Tc-DMSA, (99m)Tc-tin colloid and (99m)Tc MAA, induced by the applied cytotoxic drugs methotrexate sodium and cyclophosphamide. Nucl Med Commun 26:415–419. https://doi.org/10.1097/00006231-200505000-00004
Benador D, Benador N, Slosman DO, Nussle D, Mermillod B, Girardin E (1994) Cortical scintigraphy in the evaluation of renal parenchymal changes in children with pyelonephritis. J Pediatr 124(1):17–20. https://doi.org/10.1016/s0022-3476(94)70248-9
Taylor AJ, Lallone RL, Hagan PL (1980) Optimal handling of dimercaptosuccinic acid for quantitative renal scanning. J Nucl Med 21(12):1190–1193 (PMID: 6255114)
Tarkington MA, Fildes RD, Levin K, Ziessman H, Harkness B, Gibbons MD (1990) High resolution single photon emission computerized tomography (SPECT) 99mtechnetium-dimercapto-succinic acid renal imaging: a state-of-the-art technique. J Urol 144((2 Pt 2)):598–600. https://doi.org/10.1016/s0022-5347(17)39532-0 (discussion 606)
Treves ST, Gelfand MJ, Fahey FH, Parisi MT (2016) 2016 Update of the north American consensus guidelines for pediatric administered radiopharmaceutical activities. J Nucl Med 57(12):15N-18N (PMID: 27909182)
Lassmann M, Biassoni L, Monsieurs M, Franzius C, Jacobs F (2007) The new EANM paediatric dosage card. Eur J Nucl Med Mol Imaging 34(5):796–798. https://doi.org/10.1007/s00259-007-0370-0
Smith T, Evans K, Lythgoe MF, Anderson PJ, Gordon I (1996) Radiation dosimetry of technetium-99m-DMSA in children. J Nucl Med 37(8):1336–1342 (PMID: 8708767)
Smith T, Gordon I, Kelly JP (1998) Comparison of radiation dose from intravenous urography and 99Tcm DMSA scintigraphy in children. Br J Radiol 71(843):314–319. https://doi.org/10.1259/bjr.71.843.9616242
Mattsson S, Johansson L, Leide Svegborn S et al (2015) Radiation dose to patients from radiopharmaceuticals: a compendium of current information related to frequently used substances. Ann ICRP 44(2):7–321. https://doi.org/10.1177/0146645314558019
O’Reilly SE, Plyku D, Sgouros G et al (2016) A risk index for pediatric patients undergoing diagnostic imaging with (99m)Tc-dimercaptosuccinic acid that accounts for body habitus. Phys Med Biol 61(6):2319–2332. https://doi.org/10.1088/0031-9155/61/6/2319
Applegate KE, Connolly LP, Davis RT, Zurakowski D, Treves ST (1997) A prospective comparison of high-resolution planar, pinhole, and triple-detector SPECT for the detection of renal cortical defects. Clin Nucl Med 22(10):673–678. https://doi.org/10.1097/00003072-199710000-00002
Kim GE, Park JH, Kim JS, Won KS, Kim HW (2019) Comparison of Tc-99m DMSA renal planar scan and SPECT for detection of cortical defects in infants with suspected acute pyelonephritis. Indian J Pediatr 86(9):797–802. https://doi.org/10.1007/s12098-019-02969-6
van Luyk WH, Ensing GJ, Piers DA (1983) Low renal uptake of 99mTc-DMSA in patients with proximal tubular dysfunction. Eur J Nucl Med 8(9):404–405. https://doi.org/10.1007/bf00253217
Wehbi E, Salle A, Kanaroglou N et al (2016) Measurement of differential renal function by scintigraphy in hydronephrotic kidneys: importance of conjugate views for accurate evaluation. J Urol 195(2):471–475. https://doi.org/10.1016/j.juro.2015.09.085
Groshar D, Moskovitz B, Issaq E, Nativ O (1997) Quantitative SPECT of DMSA uptake by the kidneys: assessment of reproducibility. Kidney Int 52(3):817–820. https://doi.org/10.1038/ki.1997.399 (PMID: 9291204)
Demir F, Erselcan T, Turgut B et al (2017) Visuel and semiquantitative analysis of Tc-99m DMSA scintigraphy in children with pyelonephritis. J Clin Anal Med 8(6):515–518. https://doi.org/10.4328/JCAM.5282
Lythgoe MF, Gradwell MJ, Evans K, Gordon I (1998) Estimation and relevance of depth correction in paediatric renal studies. Eur J Nucl Med 25(2):115–119. https://doi.org/10.1007/s002590050202
Sheehy N, Tetrault TA, Zurakowski D, Vija AH, Fahey FH, Treves ST (2009) Pediatric 99mTc-DMSA SPECT performed by using iterative reconstruction with isotropic resolution recovery: improved image quality and reduced radiopharmaceutical activity. Radiology 251(2):511–516. https://doi.org/10.1148/radiol.2512081440
Biassoni L (2015) Pitfalls and limitations of radionuclide renal imaging in pediatrics. Semin Nucl Med 45(5):411–427. https://doi.org/10.1053/j.semnuclmed.2015.04.001
Agras K, Ortapamuk H, Naldöken S, Tuncel A, Atan A (2007) Resolution of cortical lesions on serial renal scans in children with acute pyelonephritis. Pediatr Radiol 37(2):153–158. https://doi.org/10.1007/s00247-006-0362-4
Iscaife A, Barbosa M, Ortiz V, Macedo AJ (2011) Segmental multicystic dysplastic kidney: a rare situation. J Pediatr Urol 7(4):491–494. https://doi.org/10.1016/j.jpurol.2010.12.005
Sarhan OM, Alghanbar M, Alsulaihim A, Alharbi B, Alotay A, Nakshabandi Z (2014) Multicystic dysplastic kidney: impact of imaging modality selection on the initial management and prognosis. J Pediatr Urol 10(4):645–649. https://doi.org/10.1016/j.jpurol.2014.03.004
Cooper CJ, Said S, Khalillullah S, Salameh HJ, Hernandez GT (2013) Multicystic dysplastic kidney complicated by pyelonephritis. Am J Case Rep 14:412–415. https://doi.org/10.12659/AJCR.889557
ESR paper on structured reporting in radiology (2018) Insights Imaging 9(1):1–7. https://doi.org/10.1007/s13244-017-0588-8
Varol S, Öktem F, Koçyiğit A, Doğan Demir A, Karataş E, Aydın M, Göknar N, İpekçi T (2021) The impact of Technetium-99m dimercapto-succinic acid scintigraphy on DNA damage and oxidative stress in children. Int J Clin Pract 75(11):e14810. https://doi.org/10.1111/ijcp.14810
Dantas FJ, de Mattos JC, Moraes MO et al (2002) Dna damage in peripheral blood nuclear cells assessed by comet assay from individuals submitted to scintigraphic examinations. Cell Mol Biol 48(7):789–791 (PMID: 12619977)
Acknowledgements
These guidelines were constructed with the help and feedback of the SNMMI Pediatric Imaging Council and EANM Pediatrics Committee. The comments, suggestions, and guidance from the members of these committees are enormously appreciated and have been incorporated into this guideline.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors (RV, ISA, ZBS, LB, LB, JB, FDG, GAM, MM, HRN, TSCN, IRB, TJR, AIS, VS, NS, STT, TZN, PZ, RL) declare that they have no conflict of interest.
Ethics approval
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vali, R., Armstrong, I.S., Bar-Sever, Z. et al. SNMMI procedure standard/EANM practice guideline on pediatric [99mTc]Tc-DMSA renal cortical scintigraphy: an update. Clin Transl Imaging 10, 173–184 (2022). https://doi.org/10.1007/s40336-022-00484-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-022-00484-x