Abstract
Objective
Globally, mood disorders are highly prevalent, and are associated with increased morbidity and mortalities. Magnetic resonance imaging is widely used in the study of mood disorders. However, bibliometric analyses of the state of this field are lacking.
Methods
A literature search in the web of science core collection (WoSCC) for the period between 1945 and 2020 returned 3073 results. Data extracted from these publications include, publication year, journal names, countries of origin, institutions, author names and research areas. The bibliometric method, CiteSpace V and key words analysis were used to visualize the collaboration network and identify research trends, respectively.
Results
Since it was first reported in 1999, the use of magnetic resonance imaging in studies on mood disorders has been increasing. Biological psychiatry is the core journal that has extensively published on this topic, while the UNIV PITTSBURGH, USA, has the highest published papers on this topic. Keyword analysis indicated that studies on depression, bipolar disorders, and schizophrenia, with a focus on specific brain regions, including amygdala, prefrontal cortex and anterior cingulate cortex are key research topics.
Conclusion
Brain structure and network, sex differences, and treatment-associated brain changes are key topics of future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mood disorders are a class of psychiatric conditions that alter moods, energy and motivation. This group of disorders include depression, bipolar disorder, premenstrual syndrome, premenstrual dysphoric disorder, and the autism spectrum of disorders among others. Globally, mood disorders affect > 300 million people with devastating consequences [1, 2]. Previous studies have reported the clinical prevalence of mood disorders [3, 4], with children, adolescents, elderly people and patients with neurological conditions being prone to depressive disorders [5, 6]. The pathophysiology of mood disorders is complex and not properly elucidated [7, 8]. Moreover, it is influenced by genetic and environmental factors that may disrupt neurotransmitter homeostasis [7, 8]. Therefore, mood disorders may result from negative feelings that leave a lasting influence on mental processes associated with perception, cognition and motor systems [9, 10]. In affective disorders, brain morphological alterations largely occur on the fronto-limbic cortex, hippocampus and amygdala. These structures modulate an individual’s emotional and cognitive function, and mood disorder manifestation [11]. Neuroimaging has revealed that brain networks that control emotional behaviors can also influence mood disorder pathophysiology [12]. Advances in in vivo neuroimaging techniques have, therefore, greatly improved our understanding of mood disorder pathophysiology [13].
There are various clinical imaging techniques, such as PET, DTI [14], ASL [15], and 1H-MRS [16]. However, magnetic resonance imaging (MRI), one of the neuroimaging techniques that are widely used in neuroscience to visualize neural activities, and to identify mental disease biomarkers [17] has unique advantages. In particular, MRI is now widely used to evaluate mood disorders [18, 19], such as depression [20] and premenstrual dysphoric disorder [21]. Advances in this technology will enable quantification of biochemical components of a functioning brain that are not detectable [22]. However, despite progress in the use of MRI to study mood disorders, accompanying bibliometric analysis is lacking.
Bibliometrics is a statistical analysis and quantitative tool for identifying research hotspots and frontiers in a particular field within a short time by extracting quantitative information on study distributions by country/region, institution, author, and journal [23]. Now, bibliometric methods in Citespace have been widely used in medical fields, such as acupuncture [24] and regenerative medicine [25]. The CiteSpace software was invented by Professor Chaomei Chen in early 2004. It is based on scientometrics and knowledge visualization, and is effective in mining scientific literature for critical information. It is used to establish co-occurrence network maps of authors, keywords, institutions, countries, and subject categories as well as co-citation networks of cited authors, cited references, and cited journals. For any discipline of interest, CiteSpace can greatly inform on basic knowledge, identify seminal studies in the area, uncover current research themes, and contextualize research advances [26].
Therefore, this study aimed at comprehensively analyzing the current status and developing trends of related references derived from Web of Science database from 1999 to 2020 in global research on mood disorders by magnetic resonance imaging through a bibliometric and visual analysis.
Materials and methods
Data collection and screening
Online literature search was performed in web of science core collection (WoSCC). To minimize bias from daily database updates, the search was done on the same day (April 29th, 2020) using the following search terms: (TS = (Disorder, Mood) OR TS = (Disorders, Mood) OR TS = (Mood Disorder) OR TS = (Affective Disorders) OR TS = (Affective Disorder) OR TS = (Disorder, Affective) OR TS = (Disorders, Affective)) AND ((Functional MRI) OR TS: (Functional MRIs) OR TS: (MRIs, Functional) OR TS: (Functional Magnetic Resonance Imaging) OR TS: (Magnetic Resonance Imaging, Functional) OR TS: (Spin Echo Imaging) OR TS: (Echo Imaging, Spin) OR TS: (Echo Imagings, Spin) OR TS: (Imaging, Spin Echo) OR TS: (Imagings, Spin Echo) OR TS: (Spin Echo Imagings) OR TS: (Imaging, Magnetic Resonance) OR TS: (NMR Imaging) OR TS: (Imaging, NMR) OR TS: (Tomography, NMR) OR TS: (Tomography, MR) OR TS: (MR Tomography) OR TS: (NMR Tomography) OR TS: (Steady-State Free Precession MRI) OR TS: (Steady-State Free Precession MRI) OR TS: (Zeugmatography) OR TS: (Imaging, Chemical Shift) OR TS: (Chemical Shift Imagings) OR TS: (Imagings, Chemical Shift) OR TS: (Shift Imaging, Chemical) OR TS: (Shift Imagings, Chemical) OR TS: (Chemical Shift Imaging) OR TS: (Tomography, Proton Spin) OR TS: (Proton Spin Tomography) OR TS: (Magnetization Transfer Contrast Imaging) OR TS: (MRI Scans) OR TS: (MRI Scan) OR TS: (Scan, MRI) OR TS: (Scans, MRI) OR TS: (fMRI) OR TS: (MRI, Functional)) AND Literature type: (Article), Indices = SCI-EXPANDED, SSCI, CCR-EXPANDED, IC time span = all years. Only published articles were selected, and publication language was unrestricted (Fig. 1).
Through descriptive analysis, we characterized the selected studies by publication year, country, journal, and authors and then constructed knowledge maps using the CiteSpace software (version 5.3.R4). Finally, citation growth rate or keywords were evaluated using burst in CiteSpace V.
Results and discussion
General information of publications
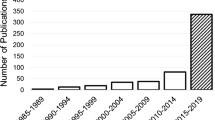
Due to its quality curation of research studies, WoS is a reliable source of studies for bibliometric analysis of scientific literature [27, 28]. Our first round of literature search found 54,346 and 331,162 reports on mood disorders and MRI, respectively. Among them, a total of 3073 original publications involving MRI in mood disorder studies were selected for further analysis. There was an increase in the number of publications on this topic between 1999 (28) and 2019 (236). Notably, in the last 4 months of 2020, 66 original studies were published (Fig. 2a). Citation scores of these studies for the 1999 (16) and 2019 (14,915) years exhibited a significant increase. An increase in citation scores by 4039 resulted in a total score of 142,188, with an h-index of 166 and on average, 46.27 references per item (Fig. 2b). These results indicate that MRI is increasingly becoming popular as a mood disorder research tool.
Funding analysis
Adequate research funding is crucial for scientific advancement and development of future researchers [29]. Research grant applications is critical in advancing one's academic career [30]. The 3073 published studies included in this study were supported by a total of 2976 grants. The top 10 funders were United States department of health human services (1000), NIH (999), NIH national institute of mental health (NIMH) (651), national natural science foundation of China (193), Narsad (151), German research foundation (DFG) (148), medical research council (MRC), UK (138), NIH national center for research resources NCRR (114), NIH national institute on drug abuse (NIDA) (76) and Wellcome trust (75) (Table 1). Among the top 10 funders, six are American. Prior to world war II, public research funding was scarce, and was mainly directed at aeronautical and agricultural research. Recently, improved government funding has accelerated basic research, including in China.
Journal analysis
Journal analysis simplifies identification, tracking, and focus on relevant research in topics of interest. The 3073 studies included in this study are published in 467 different journals. Among them, 185 studies are in biological psychiatry, 175 studies are in the journal of affective disorders, 169 studies are in psychiatry research, 169 studies are in neuroimaging, 103 studies are in neuroimage, 102 studies are in bipolar disorders, 76 studies are in psychological medicine, 72 studies are in human brain mapping, 72 studies are in PLos one, and 69 studies are in the American journal of psychiatry.
CiteSpace journal co-citation analysis identified 1029 highly cited journals and 10,270 network lines. Biological psychiatry was the most cited journal (Fig. 3). Moreover, Biological psychiatry, Neuroimage, American journal of psychiatry, Archives of General Psychiatry, and Journal of neuroscience published many groundbreaking studies that influenced research direction (Tables 2and3). Biological psychiatry is society of biological psychiatry’s official journal that is geared towards enhancing research excellence in areas studying the nature, causes, mechanisms, and management of thought, emotion, or behavioral disorders. Biological psychiatry is highly regarded in psychiatric neuroscience and was ranked 2nd among psychiatric journals in 2019 by google scholar, with an impact factor of 7.27.
Scientific Research Collaboration Analysis
Research collaboration is crucial in interdisciplinary research and helps overcome scientific challenges, leading to major research breakthroughs. Research collaboration network refers to the appearance of authors from different research institutions, or countries (regions) in the same paper.
Author analysis
CiteSpace analysis uncovered 919 nodes (corresponding to 919 prolific authors), and 1642 cooperative lines, indicating intense collaboration between authors (Fig. 4). Node size is directly proportional to the number of publications, while connecting line thickness is directly proportional to the level of collaboration. Phillips ML was the most productive author, with 59 publications, followed by Soares JC (54), Pine DS (48), Brambilla P (44), Drevets WC (42), Leibenluft E (40), Heinz A (33), Keshavan MS (33), Strakowski SM(32) and Birmaher B (31).
Co-author networks are used to analyze joint research in any field of interest. We found a total of 1029 highly cited authors and 1468 network lines, with Drevets WC being top, with 761 co-authorships (Fig. 5, Table 4).
Country analysis
CiteSpace analysis identified 57 countries and regions, with 70 collaboration links (Fig. 6), indicating high cross-country (region) research links. Top countries by publication numbers were USA, Germany, England, China, Canada, Italy, Netherlands, Australia, Brazil and Switzerland. Interestingly, while Germany is the 2nd (481 publications), no German institutions are in the top 10 list of institutions (Fig. 6, Table 5).
Institutional analysis
CiteSpace analysis identified 40 research institutions and nine collaborations in the co-institute network. Based on the number of publications, the top 10 institutions were University of Pittsburgh, Harvard University, NIMH, King's College London, University of California, Los Angeles, Stanford University, Yale University, University of California San Diego, University of Sao Paulo and McLean Hospital (Fig. 7, Table 5).
Research area analysis
The studies included covered a total of 50 research fields, including immunology (171), followed by cell biology (65), and biochemistry-molecular biology (60). The top 20 research fields involving MRI use in mood disorders are shown in Table 6. Neurosciences, neurology and psychiatry were the main research areas (Table 6).
Cited reference analysis
Analysis of cited reference co-citation identified 324 nodes and 555 links (Fig. 8). The top 10 cited publications on MRI use in mood disorders focused on depression, schizophrenia and post traumatic stress disorder. With a citation frequency of 123, “Brain Structural and Functional Abnormalities in Mood Disorders: Implications for Neurocircuitry Models of Depression”, ranked first (Table 7).
Research hotspots and frontiers
Within any given time period, knowledge maps of keywords co-occurrence reflect hot topics, while trending keywords indicate frontier topics. We used CiteSpace V to evaluate keywords in titles, abstracts, as well as article keyword sections, and to build keyword co-occurrence networks.
Research hotspots
Keyword visual knowledge map analysis revealed 130 nodes and 431 links (Fig. 9). With the strongest citation burst keywords being: f-MRI, depression, bipolar disorder, amygdala, mood disorder, prefrontal cortex, brain, major depression, schizophrenia, MRI, emotion, disorder, functional connectivity, meta-analysis, activation, abnormality, major depressive disorder, mood, anterior cingulate cortex, and magnetic resonance imaging (Table 8).
Key diseases of mood disorders
Individuals experience various emotions, such as sadness, irritation, happiness, and elation. However, people with mood disorders often experience strong emotions, for unusually long periods of time to the extent that emotions negatively impact their daily routines. Depression and bipolar disorders are the main mood disorders. Our analysis revealed 658 and 570 studies on depression and bipolar disorder, respectively. Depression is a significant clinical and public health concern [31] and its pathophysiology has not been clearly elucidated. Environmental as well as cellular and molecular factors trigger functional, and/or structural brain alterations [32] that may contribute to these disorders. Cognitive behavioral therapy is the best-studied psychotherapeutic approach, although its mechanisms of action are unknown [33]. Bipolar disorder is characterized by recurrent episodes of elevated moods and depression, along with changes in activity levels. Bipolar (affective) disorder, (previously manic depressive illness) is extremely difficult to manage [34]. Additionally, major depression and schizophrenia are major research topics. Schizophrenia is a heterogeneous psychiatric disorder with wide-ranging clinical and biological manifestations [35].
Key brain regions associated with mood disorders
Neuroimaging is increasingly becoming important in the study of the pathophysiology of mood disorders, with most studies focusing on the amygdala, prefrontal cortex and anterior cingulate cortex. The involvement of amygdala in major depression pathogenesis has been reported in previous studies [36]. While amygdala volume alterations have been implicated in mood disorders [37], Tomas et al. suggested that amygdala volume changes may reflect underlying illness or represent artifacts from medication or comorbidities [38]. The prefrontal cortex (PFC), which is involved in thinking and behavioral regulation has also been implicated in depression [39, 40]. Based on anatomical connectivity and functional specialization, the prefrontal cortex is divided into two subregions: ventromedial prefrontal cortex (vmPFC) and dorsolateral sectors (dlPFC) [41]. The human anterior cingulate cortex (ACC) is involved in response to pain affecting oneself, or others. However, its mechanisms of activity are poorly understood [42]. The mean gray matter volume of the "subgenual" ACC (sgACC) cortex is abnormally low in individuals with major depressive disorder (MDD) and bipolar disorder [43]. Psychopathic traits have been negatively correlated with amygdala-ventral anterior cingulate cortex connectivity for angry versus neutral faces [44]. The anterior cingulate cortex may influence initiation, motivation, and goal-directed behaviors [45].
Research frontiers
Keyword bursts provide a means of forecasting research direction. CiteSpace V analysis of burst keywords revealed 209 burst terms and 40 keywords by the end of 2020, and predicted the research hotspots shown in Fig. 10.
Discovering abnormal brain structure and network
In vivo neuroimaging of neural networks that putatively regulate normal emotions have shown that they are implicated in the pathogenesis of mood disorders [12]. Therefore, functional and structural brain pathology may contribute to mood disorders [46, 47]. Reduced gray matter volume has been reported in the posterior cingulate cortex and superior temporal gyrus in bipolar disorder [48], while white matter abnormalities have been associated with major depression [49]. Severe depression cases exhibit ventricular enlargement, sulcal widening, and reduced frontal lobe, hippocampus and caudate nucleus volumes [50]. Advances in brain imaging of mood disorders have been mainly due to studying regional brain abnormalities, and more recently, studying whole brain connectome. Various MRI strategies, including 'functional' MRI, which detects changes in blood flow to a specific area of the brain, blood-oxygen-level-dependent imaging (BOLD) fMRI, which examines changes in oxygenated or deoxygenated blood, and resting state fMRI have significantly improved our knowledge of neuronal activity. Mood disorder patients exhibit morphological abnormalities or morphometry in various visceromotor network structures [51]. Young MDD reported significant reduction in DRN-cingulate cortex connectivity relative to healthy controls and a correlation between DRN amygdala/hippocampus complex connectivity and depressive symptom severity [42]. Wayne C [46] proposed a neural model in which dysfunctions of MPFC and the circuits connecting it to other cortical and limbic structures account for mood disorder associated neural mechanisms.
Sex differences
Biological differences between sexes affect emotions and social behavior [52]. Lifetime depression and anxiety disorder rates are twice higher in women than men [53, 54]. Gender impacts mood and anxiety disorders and may, therefore, offer some insights into the mechanistic basis of affective disturbances in men and women [55,56,57]. Besides, women's moods are significantly affected by changes in menstrual cycle. Depression, anxiety and irritability are the three most studied symptoms of PMDD in women of childbearing age [58]. During the perinatal period, mood disturbance are commonly reported by women [59]. Depression is a common complication of pregnancy and the postpartum period [60]. Moreover, menopausal transition is correlated with mood changes ranging from distress to minor depression to major depressive disorders in women [61].The role of reproductive steroids in mood regulation among women may become the most potential research direction [62]. Given that sex differences affect various aspects of the brain, including its structure, function, and stress responses, studies should aim at establishing gender-associated differences that have an effect on mood disorders [63, 64].
Effect of treatment measures on brain activity
Effective therapies for emotional disorders are urgently needed. Although various pharmacological and non-pharmacological therapeutic approaches, including electroconvulsive therapy, cognitive behavioral therapy, ketogenic diets [65], circadian treatment [66], bright-light therapy [67] and drug naïve (ketamine, lithium salts) [68, 69] are available, their efficacies are widely varied between individuals.
Evidence-based medicine with meta-analysis
Meta-analysis may help discern important findings across disparate studies, thereby, providing actionable information to clinicians [70, 71]. For instance, multiple antidepressants are available for MDD, and their prescription should be informed by the best available data. A meta-analysis by Andrea Cipriani [72] on the relative efficacy and tolerability of 21 antidepressants used to treat major depressive disorders found that all antidepressants were more efficacious than placebo in adults. A meta-analysis study also showed that the relationship between creativity and mood disorders varied according to the research methodology used [73]. Low doses of partial dopamine agonist therapies represent a relatively safe and effective alternative therapies [74]. Additionally, a meta-analysis showed that lithium, which is commonly used to manage mood disorders, may elevate the risk of low urine concentrations, hypothyroidism, hyperparathyroidism, and weight gain [75].
Conclusions
We performed a bibliometric analysis of publications involving the use of MRI in mood disorder studies over the last 2 decades. Within this period, the number of such publications rose rapidly. The US, England, and Canada have high publication rates and centrality in this area. Additionally, research collaborations on this topic are very active. Our findings reveal Soares JC as the most prolific author, while the US emerged as the global leader in research investment. Mounting evidence shows that MRI is an effective tool for elucidating neuronal activity. The US department of human health services is the leading funding agency on this topic. We also found that depression, bipolar disorder and schizophrenia are the major focus areas when evaluating major brain regions, including the amygdala, prefrontal cortex and anterior cingulate cortex. Our findings indicate that in future, studies will likely focus on brain structure and network, sex differences, brain changes upon treatment and meta-analyses.
Data availability
The extracted data and statistical syntax are available from the first author upon reasonable request.
References
Rakofsky J, Rapaport M (2018) Mood disorders. Continuum (Minneap Minn) 24:804–827
Gordon-Lipkin E, Marvin AR, Law JK, Lipkin PH (2018) Anxiety and mood disorder in children with autism spectrum disorder and ADHD. Pediatrics 141:e20171377
Denton EJ et al (2018) Mood disorders are highly prevalent in patients investigated with a multiple sleep latency test. Sleep Breath 22:305–309
Uguz F, Yakut E, Aydogan S, Bayman MG, Gezginc K (2019) Prevalence of mood and anxiety disorders during pregnancy: a case-control study with a large sample size. Psychiatry Res 272:316–318
Tang MH, Pinsky EG (2015) Mood and affect disorders. Pediatr Rev 36:52–60 (quiz 61)
Deligianni F, Guo Y, Yang GZ (2019) From emotions to mood disorders: a survey on gait analysis methodology. IEEE J Biomed Health 23:2302–2316
Gruzdev SK, Yakovlev AA, Druzhkova TA, Guekht AB, Gulyaeva NV (2019) The missing link: how exosomes and miRNAs can help in bridging psychiatry and molecular biology in the context of depression, bipolar disorder and schizophrenia. Cell Mol Neurobiol 39:729–750
Lovheim H (2012) A new three-dimensional model for emotions and monoamine neurotransmitters. Med Hypotheses 78:341–348
Sanders RD, Gillig PM (2010) Gait and its assessment in psychiatry. Psychiatry (Edgmont) 7:38–43
Tarlacı S (2019) Quantum neurobiological view to mental health problems and biological psychiatry. J Psychopathol 25:70–84
Wilczynska K, Simonienko K, Konarzewska B, Szajda SD, Waszkiewicz N (2018) Morphological changes of the brain in mood disorders. Psychiatr Pol 52:797–805
Phillips ML, Drevets WC, Rauch SL, Lane R (2003) Neurobiology of emotion perception II: implications for major psychiatric disorders. Biol Psychiatry 54:515–528
Matsumoto K (2016) Development of magnetic resonance-based functional imaging: the past, the present, and the future. Yakugaku Zasshi 136:1075–1080
El-Serougy L, Abdel Razek AAK, Ezzat A, Eldawoody H, El-Morsy A (2016) Assessment of diffusion tensor imaging metrics in differentiating low-grade from high-grade gliomas. Neuroradiol J 29:400–407
Abdel Razek AAK, Talaat M, El-Serougy L, Gaballa G, Abdelsalam M (2019) Clinical applications of arterial spin labeling in brain tumors. J Comput Assist Tomogr. 43:525–532
Razek AAKA, Abdalla A, Ezzat A, Megahed A, Barakat T (2014) Minimal hepatic encephalopathy in children with liver cirrhosis: diffusion-weighted MR imaging and proton MR spectroscopy of the brain. Neuroradiology 56:885–891
Tulay EE, Metin B, Tarhan N, Arıkan MK (2019) Multimodal neuroimaging: basic concepts and classification of neuropsychiatric diseases. Clin EEG Neurosci 50:20–33
Ai T et al (2012) A historical overview of magnetic resonance imaging, focusing on technological innovations. Invest Radiol 47:725–741
Mathias LK, Monette PJ, Harper DG, Forester BP (2017) Application of magnetic resonance spectroscopy in geriatric mood disorders. Int Rev Psychiatry 29:597–617
Lai C-H (2019) The neural markers of MRI to differentiate depression and panic disorder. Prog Neuro-Psychoph 91:72–78
Petersen N, Ghahremani DG, Rapkin AJ et al (2019) Resting-state functional connectivity in women with PMDD. Transl Psychiatry 9(1):339
Budinger TF, Bird MD (2018) MRI and MRS of the human brain at magnetic fields of 14T to 20T: technical feasibility, safety, and neuroscience horizons. Neuroimage 168:509–531
Wang L, Xia E, Li H et al (2019) A bibliometric analysis of crowdsourcing in the field of public health. Int J Environ Res Public Health 16(20)
Liang YD et al (2017) Study of acupuncture for low back pain in recent 20 years: a bibliometric analysis via CiteSpace. J Pain Res 10:951–964
Chen CM, Hu ZG, Liu SB, Tseng H (2012) Emerging trends in regenerative medicine: a scientometric analysis in CiteSpace. Expert Opin Biol Ther 12:593–608
Chen C (2016) CiteSpace: a practical guide for mapping scientific literature
Bang CS, Lee JJ, Baik GH (2019) The most influential articles in Helicobacter pylori research: a bibliometric analysis. Helicobacter 24:e12589
Huang X, Fan X, Ying J, Chen S (2019) Emerging trends and research foci in gastrointestinal microbiome. J Transl Med 17:67
Farrokhyar F et al (2016) Impact of research investment on scientific productivity of junior researchers. Transl Behav Med 6:659–668
Squitieri L, Chung KC (2014) Funding research in the twenty-first century: current opinions and future directions. Hand clin 30(3):367–376
Wormser GP, Hassett AL (2019) Depression in the primary care setting. N Engl J Med 380:2278–2279
Krishnan V, Nestler EJ (2008) The molecular neurobiology of depression. Nature 455:894–902
Anthes E (2014) Depression: a change of mind. Nature 515:185–187
Anderson IM, Haddad PM, Scott J (2012) Bipolar disorder. BMJ 345:e8508
Tandon R et al (2013) Definition and description of schizophrenia in the DSM-5. Schizophr Res 150:3–10
Drevets WC (2003) Neuroimaging abnormalities in the amygdala in mood disorders. Ann N Y Acad Sci 985:420–444
Velakoulis D et al (2006) Hippocampal and amygdala volumes according to psychosis stage and diagnosis: a magnetic resonance imaging study of chronic schizophrenia, first-episode psychosis, and ultra-high-risk individuals. Arch Gen Psychiatry 63:139–149
Hajek T et al (2009) Amygdala volumes in mood disorders–meta-analysis of magnetic resonance volumetry studies. J Affect Disord 115:395–410
Treadway MT et al (2015) Illness progression, recent stress, and morphometry of hippocampal subfields and medial prefrontal cortex in major depression. Biol Psychiatry 77:285–294
Liu W et al (2017) The role of neural plasticity in depression: from hippocampus to prefrontal cortex. Neural Plast 2017:6871089
Koenigs M, Grafman J (2009) The functional neuroanatomy of depression: distinct roles for ventromedial and dorsolateral prefrontal cortex. Behav Brain Res 201:239–243
Carrillo M et al (2019) Emotional mirror neurons in the rat’s anterior cingulate cortex. Curr Biol 29:2104
Drevets WC, Savitz J, Trimble M (2008) The subgenual anterior cingulate cortex in mood disorders. CNS Spectr 13:663–681
Ewbank MP et al (2018) Psychopathic traits influence amygdala-anterior cingulate cortex connectivity during facial emotion processing. Soc Cogn Affect Neurosci 13:525–534
Devinsky O, Morrell MJ, Vogt BA (1995) Contributions of anterior cingulate cortex to behaviour. Brain 118(Pt 1):279–306
Drevets WC, Price JL, Furey ML (2008) Brain structural and functional abnormalities in mood disorders: implications for neurocircuitry models of depression. Brain Struct Funct 213:93–118
Anand A (2019) Editorial: functional and structural connectomics of mood disorders. Front Psychiatry 10:202
Nugent AC et al (2006) Cortical abnormalities in bipolar disorder investigated with MRI and voxel-based morphometry. Neuroimage 30:485–497
Tham MW, Woon PS, Sum MY, Lee TS, Sim K (2011) White matter abnormalities in major depression: evidence from post-mortem, neuroimaging and genetic studies. J Affect Disord 132:26–36
Schweitzer I, Tuckwell V, Ames D, O’Brien J (2001) Structural neuroimaging studies in late-life depression: a review. World J Biol Psychiatry 2:83–88
Drevets WC (2001) Neuroimaging and neuropathological studies of depression: implications for the cognitive-emotional features of mood disorders. Curr Opin Neurobiol 11:240–249
Choleris E, Galea LAM, Sohrabji F, Frick KM (2018) Sex differences in the brain: implications for behavioral and biomedical research. Neurosci Biobehav Rev 85:126–145
Weissman MM et al (1996) Cross-national epidemiology of major depression and bipolar disorder. JAMA 276:293–299
Gater R et al (1998) Sex differences in the prevalence and detection of depressive and anxiety disorders in general health care settings: report from the World Health Organization Collaborative Study on Psychological Problems in General Health Care. Arch Gen Psychiatry 55:405–413
Hirsh AT, Waxenberg LB, Atchison JW, Gremillion HA, Robinson ME (2006) Evidence for sex differences in the relationships of pain, mood, and disability. J Pain 7:592–601
Hankin BL (2009) Development of sex differences in depressive and co-occurring anxious symptoms during adolescence: descriptive trajectories and potential explanations in a multiwave prospective study. J Clin Child Adolesc Psychol 38:460–472
Rainville JR, Hodes GE (2019) Inflaming sex differences in mood disorders. Neuropsychopharmacology 44:184–199
Ko CH et al (2013) Depression, irritability, and anxiety in women with premenstrual dysphoric disorder. Int J Psychiatry Med 46:39–55
Bei B, Coo S, Trinder J (2015) Sleep and mood during pregnancy and the postpartum period. Sleep Med Clin 10:25–33
Becker M, Weinberger T, Chandy A, Schmukler S (2016) Depression during pregnancy and postpartum. Curr Psychiatry Rep 18:32
Alexander JL et al (2007) Neurobehavioral impact of menopause on mood. Expert Rev Neurother 7:S81–S91
McEvoy K, Osborne LM (2019) Allopregnanolone and reproductive psychiatry: an overview. Int Rev Psychiatry 31:237–244
Altemus M, Sarvaiya N, Neill Epperson C (2014) Sex differences in anxiety and depression clinical perspectives. Front Neuroendocrinol. 35:320–330
Rubinow DR, Schmidt PJ (2019) Sex differences and the neurobiology of affective disorders. Neuropsychopharmacology 44:111–128
Brietzke E et al (2018) Ketogenic diet as a metabolic therapy for mood disorders: Evidence and developments. Neurosci Biobehav Rev 94:11–16
Huhne A, Welsh DK, Landgraf D (2018) Prospects for circadian treatment of mood disorders. Ann Med 50:637–654
Pail G et al (2011) Bright-light therapy in the treatment of mood disorders. Neuropsychobiology 64:152–162
Haussmann R, Lewitzka U, Severus E, Bauer M (2017) Correct treatment of mood disorders with lithium. Nervenarzt 88:1323–1334
Sanacora G et al (2017) A consensus statement on the use of ketamine in the treatment of mood disorders. JAMA Psychiat 74:399–405
Paul M, Leibovici L (2014) Systematic review or meta-analysis? Their place in the evidence hierarchy. Clin Microbiol Infect 20:97–100
Lee YH (2018) An overview of meta-analysis for clinicians. Korean J Intern Med 33:277–283
Cipriani A et al (2018) Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet 391:1357–1366
Taylor CL (2017) Creativity and Mood disorder: a systematic review and meta-analysis. Perspect Psychol Sci 12:1040–1076
Romeo B, Blecha L, Locatelli K, Benyamina A, Martelli C (2018) Meta-analysis and review of dopamine agonists in acute episodes of mood disorder: efficacy and safety. J Psychopharmacol 32:385–396
McKnight RF et al (2012) Lithium toxicity profile: a systematic review and meta-analysis. Lancet 379:721–728
Acknowledgements
The authors would like to thank the Research and Innovation team of Emotional Diseases and Syndromes at Shandong University of Traditional Chinese Medicine for their support.
Funding
Prof. Mingqi Qiao received funding from National Science & Technology Major Project "Key New Drug Creation and Manufacturing Program" of China—NO. SQ2017ZX091064, while Prof. Dongmei Gao received funding from the National Natural Science Foundation of China—NO. 81001484 and 81473558.
Author information
Authors and Affiliations
Contributions
GM and SH conceived the study and wrote the manuscript. GM, SH and CX collected and analyzed the data, contributed materials/analysis tools, prepared figures and/or tables and read the final draft. GD and QM contributed to study conception and its coordination. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare no conflict of interest.
Ethical approval
This study is a literature review for which ethical approval was waived.
Informed consent
None required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gao, M., Sun, H., Cheng, X. et al. Magnetic resonance imaging in mood disorders: a bibliometric analysis from 1999 to 2020. Clin Transl Imaging 9, 241–254 (2021). https://doi.org/10.1007/s40336-021-00425-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-021-00425-0