Abstract
Introduction
Fluorine-18 (18F) Fluciclovine (anti-1-amino-3-18F-fluorocyclobutane- 1-carboxylic acid [FACBC]) is a synthetic amino acid labeled with 18F, currently used as PET radiopharmaceutical to investigating prostate cancer, namely in the recurrent setting.
Fluciclovine is transported to cell membranes by amino acid transporters, such as LAT1 and ASCT2. The upregulation of LAT-1 and ASCT2 activities is typical of prostate cancer but is also present in other pathological conditions such as non-prostatic neoplasms (e.g., lung cancer) and in benign inflammatory process (e.g., benign prostatic hyperplasia, chronic prostatitis, high-grade prostatic hyperplasia intraepithelial).
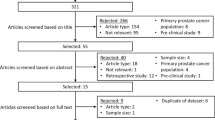
Methods
In this short essay we present a retrospective FACBC PET/CT analysis consisting of a selection of the five most relevant cases of patients referred in our centre to FACBC PET/CT for prostate cancer, with concomitant FACBC uptake in sites atyipical for prostate cancer.
Results
These five selected cases demonstrate FACBC uptake at the level of the pancreatic head, adrenal incidentalomas, pulmonary nodules, mediastinal lymph nodes and neoformative tissue of the rectal wall.
Discussion
Clinical cases selected in this pictorial essay have demonstrated that Fluciclovine is not an exclusive and specific radiotracer for prostate cancer and, therefore, can induce misdiagnosis. In fact, incidental benign and malignant uptake might occur and should be further evaluated with clinical correlation or other imaging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction/aim
Fluorine-18 (18F) Fluciclovine (anti-1-amino-3-18F-fluorocyclobutane- 1-carboxylic acid [FACBC]) is a synthetic amino acid, radiolabeled with 18F, available in Europe since 2018 and used as a new PET/CT tracer for the staging and restaging of patients with prostate cancer, also in recurrent disease [1]. Fluciclovine is internalized within cell membranes by amino acid transporters, such as LAT1 and ASCT2, but not metabolized or incorporated into newly synthesized proteins. The major route of elimination is renal but urinary excretion is slow and reaches approximately only 3% of the administered radioactivity within 4 h and 5% within 24 h [2]. Due to the body distribution of amino acid transporters, after intravenous administration of Fluciclovine this tracer is distributed to the liver (approximately 14% of the total administered activity), pancreas (3%), lungs (7%), to the medulla (12%) and to the heart wall (4%). Human L-type amino-acid transporter-1 (LAT1) and Human SLC1A5 (ASCT2) Amino acid transporter are overexpressed amino acid transporters especially in cancer cells of prostatic origin and higher levels of expression of LAT1 and ASCT2 are characteristic in the more aggressive phenotypes [3, 4]. For this reason, Fluciclovine (18F) is a highly specific radiotracer for investigating recurrent prostate cancer, even compared to Choline (18F). Fluciclovine seems to be slightly superior to the performance of Choline (11C) for patients radically treated for prostate cancer with biochemical relapse [5]. (68 Ga) Prostate-specific membrane antigen (PSMA) as well has demonstrated excellent results for the imaging of patients with prostate cancer relapse. When compared with Choline (18F) within the same patients, (68 Ga) PSMA was found to be superior to choline in detecting lesions and in increasing SUVmax [6]. In a recent study, 169 cases of diagnostic pitfalls were shown in 1000 patients undergoing PET/CT with 18F-choline during PCa staging or restaging. The most frequent sites of pitfalls were the lymph nodes, the adrenal glands and the lungs. Many patients (40%) showed mild absorption of 18F-choline in the lymph nodes. In most of these cases, absorption was confined to a single lymph node, generally located in the axillary, neck, mediastinal or inguinal regions. In all cases the absorption was considered inflammatory, except for two cases in which a lymphoma and a patient with bladder cancer were documented. In 13% of those patients, a slight absorption of the tracer into the adrenal glands, almost unilateral, was documented: the uptake was considered exclusively functional. The pulmonary district was the third most important district for prevalence of pitfalls (9%). Many patients have shown focal absorption at a solitary pulmonary node, usually with low SUVmax, suspected for benign pulmonary nodule. In one case a neuro-endocrine lung tumor was diagnosed in a large mass (SUVmax 4.5) and in two cases the diagnosis of sarcoidosis was made [7]. The term “diagnostic pitfall” was intended as a potentially pathological tracer uptake area, higher than the surrounding background, not related to the disease under study.
In patients with prostate cancer, Fluciclovine (18F) PET/CT was found to have a high sensitivity (92.5%) and specificity (90.1%) for the focus of primary disease, but the sensitivity for detecting recurrent disease varies with PSA values [1]. However, Fluciclovine is not a specific tracer due to the upregulation of LAT1 and ASCT2 activities also present in other neoplasms, in recent post-radiotherapy or cryotherapy and in benign inflammatory processes (such as benign prostatic hyperplasia, chronic prostatitis, high-grade intraepithelial prostatic hyperplasia) [8, 9]. Fluciclovine (18F) is FDA approved for restaging PCa and is broadly used in EU as well. Thus, the number of patients investigated with imaging procedure is increasing. [10,11,12]. Thus understanding potential source of errors in image interpretation is crucial.
Case reports
Five clinical cases were illustrated in our retrospective pictorial essay including a pancreatic head mass, adrenal incidentaloma, pulmonary nodules, mediastinal lymph nodes, neoformative rectal wall tissue. They were unexpected findings in patients with previous prostate cancer (PCa) or biochemical recurrence. As there is currently no evolutionary monitoring over time, these findings described in FACBC PET/CT imaging should be considered for interpretation purposes only.
Clinical case #1: pancreatic head mass
Clinical summary
An 86-year-old man with a history of chronic HCV hepatitis was diagnosed with PCa in 2014 (Gleason scale = 3 + 4), treated with androgen deprivation therapy (ADT). No curative therapy was administrated. From April 2018 he had a progressive increase experienced biochemical recurrence (BCR) with rising PSA levels (2.83) and then referred to 18F Choline PET/CT which showed high uptake of the prostate with no other signs of disease. However, for a further increase in PSA (3.05 ng/ml in March 2019) the patient performed 18F-FACBC PET/CT for further staging. FACBC PET/CT showed abnormal radiotracer uptake in the right prostatic lobe with standardized maximum uptake value (SUVmax 6.1), corresponding to the known primary tumor, without significant accumulation in the lymph nodes and bone. However, as a collateral finding, it showed a large area of inhomogeneous uptake, projecting at the level of the head of the pancreas, which appeared less intense (SUVmax 5.25) than the physiological distribution of the radiotracer in the remaining glandular parenchyma (SUVmax 11.2) (Fig. 1a, b). In the CT co-registration images, this finding corresponded to a 6.5 × 4.5 cm oval solid formation located posterior to the pancreatic head and second duodenal portion. For this reason, the patient subsequently underwent an MRI examination of the abdomen with contrast medium, which confirmed the presence of the coarse solid nodular formation at the level of the pancreatic head. This lesion showed significant post-contrast enhancement and displaced adjacent structures but without evident signs of infiltration of the same.
Pathology correlation
Considering data derived from PET images in April 2019, the patient underwent Echo-endoscopy with targeted biopsy. A macroscopic hypoechoic lesion of pancreatic relevance was detected, characterized by regular margins without signs of infiltration of the neighboring structures; the histological examination instead documented leukocyte-fibrin material with lymphocytes and fragments of necrotic tissue, suggestive for inflammatory process.
Clinical result
The case was discussed in a multidisciplinary tumor board with the indication of a rigorous diagnostic monitoring over time, which showed a modest reduction in the subsequent MRI control without any additional treatment. Currently the patient continues the nonsteroidal antiandrogen (NSAA) therapy (Leuprolide acetate) and the clinical-laboratory and instrumental follow-up with thoracic CT and abdominal MRI.
Take home message
In this case, 18F Fluciclovine showed an atypical distribution in the pancreatic site, generally physiological; therefore, any atypical distribution must be seriously considered to investigate and rule out the possible presence of further benign or malignant lesions.
Clinical case #2: adrenal incidentaloma
Clinical summary
An 82-year-old castration-resistant prostatic cancer (CRPC) patient has an increase in PSA (0.90 ng/ml). In July 2019 he performed an 18F-FACBC PET/CT scan showing inhomogeneous uptake in the prostate with focal areas in the right lobe (SUVmax 5.3): as expression of the PCa lesion. As a collateral finding, abnormal tracer uptake was detected in the right adrenal lodge (SUVmax 4.7), which in the CT co-registration images corresponded to a nodular formation of the right adrenal (size 35 × 32 × 25 mm) with density similar to lipid density (inhomogeneous with HU ranging from − 10 to 10), suggesting a possible adenoma (Fig. 2). The patient was asymptomatic and showed normal values in laboratory endocrinological tests (24 h urinary free cortisol, 24 h urinary metaneprines and cathecolamines, plasma aldosterone and plasma renin).
Adrenal tumor size greater than 4.0 cm has high sensitivity for adrenal cancer [13]. Adrenal lesions which exhibit less than 10 HU on non-contrast CT scan strongly suggest a benign adenoma [14]. Some benign adenomas may have higher than 10 HU. The patient was asymptomatic and showed normal values in laboratory endocrinological tests (24 h urinary free cortisol, 24 h urinary metaneprines and cathecolamines, plasma aldosterone and plasma renin).
Pathological correlation
In consideration of the diagnostic (MRI and CT), clinical and laboratory data, this incidentaloma was considered to be related to adrenal adenoma of the non-secreting type.
Clinical result
The CRPC patient is currently on androgen deprivation therapy (ADT) with careful clinical-laboratory monitoring of the PSA value.
Take home message
Several studies have shown the presence of increased FACBC uptake in adrenal adenoma [2]. It is, therefore, necessary to document atypical, non-physiological Fluciclovine concentrations in the adrenal site by comparing them with the Hounsfield unit scale (< 10 HU) and with information obtained from CT to rule out other adrenal pathologies. Hormonally inactive adenomas are initially managed by reimaging in 3–6 months, then annually for 1–2 years, and they should also have repeat hormonal assessment once a year for 5 years. If the mass grows more than 1 cm or becomes hormonally active, then adrenalectomy is recommended.
Clinical case #3: lung nodules
Clinical summary
An 85-year-old man with non-surgical prostate adenocarcinoma with a Gleason score of 7 (3 + 4) has been treated with NSAA (Enzalutamide) and gonadotropin-releasing hormone (GnRH) agonist (Triptorelin acetate) a since 2005. In January 2020 he showed a notable increase in PSA (6.67 ng/ml). A non-contrast CT of pelvis did not show significant abnormalities. In March 2020 he performed 18F-FACBC which showed an irregular and pathological uptake of the radiopharmaceutical in the right posterolateral prostate (SUVmax 6.68) site of known neoplasm, without significant lymph node and bone uptake. Collaterally, three subcentrimetric pulmonary nodules were appreciated, respectively, in the medial lateral segment of the middle lobe (SUVmax 2.9), in the apical segment of the right lower lobe (SUVmax 3.69) and in the basal lateral segment of the lower left lobe (SUVmax 3.01). The described nodules were of solid type, with regular margins and between 6 and 10 mm in size (Fig. 3a, b).
Pathological correlation
This case was discussed in the Prostate Oncology Department with the decision to monitor the growth of these pulmonary nodules with chest CT.
Clinical result
The patient is currently being treated with two different GnRH agonists (Triptorelin acetate and Enantone), in close clinical-diagnostic follow-up. The physical condition of the patient does not allow surgery, the PSA values remain high but stable over time under the therapy. Furthermore, pulmonary nodules appear unchanged in the last CT of the chest.
Take home message
The occasional finding of pulmonary nodules uptaking Fluciclovine even in the absence of other signs of metastatic prostatic disease, must always raise the diagnostic doubt of a possible synchronous lung cancer, since as is known, the amino acid transport systems (ASCT2 and LAT1) play an important role in the upregulation of cell proliferation in NSCL lung tumors [3]. However, especially when the uptake value is low, it cannot confirm or rule out metastatic lesions of prostate cancer or differentiate from other diseases. Metastatic lesions of the prostate can also occur in patients with no known metastatic disease and unfortunately the uptake values cannot suggest the different nature (NSCLC).
Clinical case #4: mediastinal lymph nodes
Clinical summary
A 76-year-old man who underwent radical prostatectomy and pelvic lymphadenectomy in May 2008 for mixed prostate adenocarcinoma (ductal and acinar, Gleason score: 3 + 4) underwent follow-up hormone therapy and adjuvant radiotherapy. For the biochemical recurrence the patient was treated with GnRH agonist (Triptorelin acetate) and then with NSAA (Enzalutamide) and radiotherapy until a new increase in PSA (1.2 ng/ml), even after hormonal deprivation. In December 2019 he performed 18F FACBC PET/CT revealing the presence of abnormal uptake in the spine at the level of the D1-D5 dorsal tract (Fig. 4a), corresponding to the co-registration CT images with osteoblastic area. Moreover, ilo-mediastinal lymphoadenopathies were also documented along the aortic arch and at the level of the aorto-pulmonary window (SUVmax 6.5) (Fig. 4b).
Pathological correlation
The case was discussed in the prostate oncology department with the decision to proceed with radiotherapy treatment on the D1–D5 dorsal spine for analgesic purposes, pending the possibility of investigating mediastinal lymphadenopathies.
Clinical result
Unfortunately, the patient died before further diagnostic tests could be performed.
Take home message
In this case, Fluciclovine showed uncommon uptake in the lymph nodes at the mediastinal site; this data seems to be of uncertain interpretation, suggesting a possible metastatic involvement, although it is known from studies that Fluciclovine can be localized both in inflammatory processes and in large B-cell and T-cell lymphomas. Indeed, some authors have reported a LAT1 overexpression in T-cell lymphoblastic lymphoma and T-cell acute lymphoblastic leukemia [8].
Clinical case #5: tissue thickening of the rectal wall
A 90-year-old man with a history of prostate adenocarcinoma diagnosed in 2002 was treated with radical prostatectomy followed by Luteinizing Hormone Releasing Hormone (LHRH) therapy for 1 year. In 2006 the patient underwent radiotherapy for locoregional relapse. A biochemical recurrence of the disease treated with GNRH agonist and NSAA has been documented since October 2016. In October 2019 for biochemical progression (PSA: 1.61 ng/ml), he performed PET/CT with (18F) Fluciclovine which detected abdominal and pelvic lymph nodes, (SUVmax 12.4) bone metastases of the right hemisome of L3 (SUVmax 7.1), but also an avid and uncommon uptake of FCABC (SUVmax 10.74) of the left rectal wall (Fig. 5) corresponding to the tissue thickening in the CT co-registration.
Pathological correlation
The patient was subsequently subjected to rectal sigmoidoscopy with biopsy which revealed a rectal ampulla with difficulty distensible with irregularities and eroded areas; histological examination documented hyperplastic glands with lymphoplasmacytic infiltrate of the wall.
Clinical result
The patient is currently being treated with two different GNRH agonists (Triptorelin acetate and Enantone), in close clinical-diagnostic follow-up.
Take home message
As it is known, since Fluciclovine is not a specific tumor tracer, it can also accumulate in inflammatory conditions in different parts of the body, simulating a possible rectal heteroplasia, but that instead turned out to be a hyperplasia of the wall with inflammatory infiltrates.
Discussion
In this illustrative test, five clinical cases were shown of patients with biochemical recurrence of prostate cancer, but who also had atypical tracer uptake at other anatomical sites on PET/CT 18F-FACBC. In particular, 5 clinical cases are described which, in addition to the known pathology, presented a mass of the pancreatic head, an adrenal incidentaloma, pulmonary nodules, mediastinal lymphadenopathy and neoformative/inflammatory tissue of the rectal wall. Our goal is to describe these variants of occasional findings with the aim of interpreting the images to lead to a correct diagnosis. In recent years, several authors have shown that the cellular uptake of Fluciclovine is mediated by some amino acid transporters, such as the alanine-serine-cysteine system (ASC), the N system and the L system (LAT1), which can be overexpressed in other pathological conditions (benign/malignant neoplasms or inflammatory/infectious processes) [15,16,17].
Although Fluciclovine has been approved by the FDA for the evaluation of biochemically recurrent prostate cancer, similarly to other radiopharmaceuticals (e.g., FDG) it can also be positive in other pathologies, showing a non-absolute specificity for prostate cancer.
Especially in recent years, a high uptake of Fluciclovine has been reported in the literature in other malignant tumor diseases such as glioma, breast cancer, lung cancer, renal cancer, colon cancer, myeloma, brain metastases and follicular lymphoma. Furthermore, a high tissue uptake of Fluciclovine can be present in non-tumor pathologies such as inflammatory or infectious forms, in chronic prostatic hyperplasia, nonspecific adenopathies, adrenal or pituitary adenomas and osteoid osteoma [16, 18,19,20]. In a recent prospective study, 27 women with invasive or locally advanced lobular or ductal carcinoma were studied; 14 of these patients showed pathological axillary lymph nodes with low FDG uptake but intense Fluciclovine fixation. Histological examination confirmed the presence of axillary lymph node metastases, showing that Fluciclovine is more specific than FDG especially in lobular breast cancer, which can generally have low levels of FDG uptake. From the data obtained, the authors hypothesized that there may be a genetic regulation that predisposes metastatic cells to overexpress amino acid transporters, reducing glucose metabolism [18]. Another study documented clinical cases of male breast cancer accidentally detected at PET/CT with Fluciclovine during the follow-up of prostate cancer. Male breast cancer is a rare tumor, but an increased incidence of prostate and breast cancer has been found in patients with mutated Breast Cancer Related Antigens (BRCA). Therefore, when identifying a breast mass in a patient with prostate cancer, genetic evaluation of family members is required for risk assessment [21].
The overexpression of ASCT2 and LAT1 is frequently found also in lung tumours, expecially in the non-small cell subtype, because the amino acid transport systems play a significant role in the upregulation of cell proliferation. A correlation between expression of LAT1 and tumour hypoxia was also found and probably represent a factor in resistance to platinum-based chemotherapy and a cause of an unfavourable prognosis in surgically non-resectable lung cancer [8, 22, 23]. Taking advantage of the absent renal excretion at the time of the scan, Schuster used Fluciclovine for the evaluation of renal masses; a focal uptake of the tracer in the renal site associated with morphological injury, must be considered suspect for malignant neoplasia. Besides the small number of patients, the study showed an increased uptake of FACBC in papillary tumours compared to the normal renal tissue. In comparison to brain parenchyma, a focal increased absorption of Fluciclovine was also demonstrated in brain metastases and brain tumours, such as gliomas and meningiomas [16, 24, 25]. However, the presence of Flucicovine uptake in a lesion or organ, while representing the presence of amino acid activity at that site, cannot always distinguish the nature of the benign/malignant tumor. In some glandular organs (adrenal, pancreas) it could represent the residual physiological absorption activity in the presence of structural alterations due to the lesion and a lower SUVmax value cannot always exclude a malignant lesion. Further investigations and adequate follow-up are required after some time.
Conclusions
In this pictorial essay some cases have been evaluated in which the FACBC is fixed to pathological lesions but different from those for which the drug is registered, namely the recurrence of prostate cancer. It is, therefore, advisable to always perform an acquisition according to the protocol, but extending the field of view as much as possible. Normal physiological distribution and variants knowledge is required for proper interpretation. Any non-physiological fixation of the tracer must be considered and evaluated on the basis of the patient's clinical condition, carrying out further morphological and laboratory evaluations.
References
Parent EE, Schuster DM (2018) Uptade on 18-F-fluciclovine PET for prostate cancer imaging. J Nucl Med 59:733–739
Gusman M, Aminsharifi JA, Peacock JG, Anderson SB, Clemenshaw MN, Banks KP (2019) Review of 18F-fluciclovine PET for detection of recurrent prostate cancer. Radiographics 39:822–841. https://doi.org/10.1148/rg.2019180139
Sakata T, Ferdous G, Tsuruda T, Satoh T, Baba S, Muto T, Ueno A, Endou KY, Okayasu HI (2009) L-type amino-acid transporte 1 as a novel biomarker for high-grade malignancy in prostate cancer. Pathol Int 59:7–18
Wang Q, Hardie RA, Hoy AJ et al (2015) Targeting ASCT2-mediated glutamine uptake block prostate cancer growth and tumour development. J Pathol 236:278–289
Nanni C, Zanoni L, Pultrone C et al (2016) (18)F-FACBC (anti1-amino-3-(18)F-fluorocyclobutane-1-carboxylic acid) versus (11)C-choline PET/CT in prostate cancer relapse: results of a perspective trial. Eur J Nucl Med Mol Imaging 43:1601–1610
Afshar-Oromieh A, Zechmann CM, Malcher A et al (2014) Comparison of PET imaging with (68)Ga-labelled PSMA ligand and (18)F-choline-based PET/CT for the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging 41:11–20
Calabria F, Chiaravalloti A, Cicciò C et al (2017) PET/CT with 18F–choline: Physiological whole bio-distribution in male and female subjects and diagnostic pitfalls on 1000 prostate cancer patients. 18F–choline PET/CT bio-distribution and pitfalls. A southern Italian experience. Nucl Med Biol 51:40–54
Robertson MS, Sakellis CG, Hyun H, Jacene HA (2020) Extraprostatic uptake of 18F-fluciclovine: differentiation of nonprostatic neoplasms from metastatic prostate cancer. Am J Roentgenol 214:641–648. https://doi.org/10.2214/AJR.19.21894
Nguyen NC, Muthukrishnan A, Mountz JM (2020) Differential 18F-FDG and 18F-fluciclovine uptake pattern in a patient with poorly differentiated adenocarcinoma of the lung and prostate cancer biochemical recurrence. Clin Nucl Med 45:e63–e64. https://doi.org/10.1097/rlu.0000000000002781
Schuster DM, Nanni C, Fanti S (2016) PET tracers beyond FDG in prostate cancer. Semin Nucl Med 46:507–521
Zanoni L, Bossert I, Matti A, Schiavina R, Pultrone C, Fanti S, Nanni C (2018) A rewiev discussing fluciclovine (18F) PET/CT imaging in the detection of recurrent prostate cancer. Future Oncol 14:1101–1115
Savir-Baruch B, Zanoni L, Schuster DM (2017) Imaging of prostate cancer using fluciclovine. PET Clin 12:145–157
Angeli A, Osella G, Alì A et al (1997) Adrenal incidentaloma: an overview of clinical and epidemiological data from the National Italian Study Group. Horm Res 47:279–283
Grumbach MM, Biller BM, Braunstein GD et al (2003) Management of the clinically inapparent adrenal mass (“incidentaloma”). Ann Intern Med 138:424–429
Oka S, Kanagawa M, Doi Y, Schuster DM, Goodman MM, Yoshimura H (2017) PET tracer 18F-fluciclovine can detect histologically proven bone metastatic lesions: a preclinical study in rat osteolytic and osteoblastic bone metastasis models. Theranostics 7:2048–2064
Schuster DM, Nanni C, Fanti S et al (2014) Anti-1-amino-3-18F-fluorocyclobutane-1-carboxylic acid: physiologic uptake patterns, incidental findings, and variants that may simulate disease. J Nucl Med 55:1986–1992
Nye JA, Schuster DM, Yu W, Camp DM, Goodman MM, Votaw JR (2007) Biodistribution and radiation dosimetry of the synthetic nonmetabolized amino acid analogue anti-18F-FACBC in humans. J Nucl Med 48:1017–1020
Ulaner GA, Goldman DA, Gonen M, Pham H, Castillo R, Lyashenko SK, Lewis JS, Dang C (2016) Initial results of a prospective clinical trial of 18F-fluciclovine PET/CT in newly diagnosed invasive ductal and invasive lobular breast cancers. J Nucl Med 57:1350–1356
Ulaner GA, Goldman DA, Corben A, Lyashenko SK, Gonen M, Lewis JS, Dickler M (2017) Prospective clinical trial of 18F-fluciclovine PET/CT for determining the response to neoadjuvant therapy in invasive ductal and invasive lobular breast cancers. J Nucl Med 58:1037–1042
Amzat R, Teleghani P, Miller DL et al (2013) Pilot study of the utility of the synthetic PET amino-acid radiotracer anti-1-amino-3-[(18)F] fluorocyclobutane-1-carboxylic acid for the noninvasive imaging of pulmonary lesions. Mol Imaging Biol 15:633–643
Gill HS, Tade F, Greenwald DT, Yonover PM, Savir-Baruch B (2018) Metastatic male breast cancer with increased uptake on 18F-fluciclovine PET/CT scan. Clin Nucl Med 43:23–24
Kaira K, Takahashi T, Murakami H et al (2011) Relationship between LAT1 expression and response to platinum-based chemioteraphy in non-small cell lung cancer patients with postoperative recurrence. Anticancer Res 31:3775–3782
Shimizu K, Kaira K, Tomizawa Y et al (2014) ASC amino-acid transporter2 (ASCT2) as a novel prognostic marker in non-small cell lung cancer. Br J Cancer 110:2030–2039
Schuster DM, Nye JA, Nieh PT et al (2009) Initial experience with the radiotracer anti-1-amino-3-[18F] fluorocyclobutane-1-carboxylic acid (anti-[18F]FACBC) with PET in renal carcinoma. Mol Imaging Biol 11:434–438
Kondo A, Ishii H, Aoki S et al (2016) Phase IIa clinical study of [18F] fluciclovine: efficacy and safety of a new PET tracer for brain tumors. Ann Nucl Med 30:608–618
Acknowledgements
We would like to thank all the Nuclear Medicine technical and nursing staff for their professional contribution.
Funding
Open Access funding provided by Università Politecnica delle Marche. There was no funding for this paper.
Author information
Authors and Affiliations
Contributions
CR, CC and LB contributed to the study conception and design. Data collections was done by CR. PET/CT analyses were done by CR, CC and AP. Images were created by GB and FMF. The first draft of the manuscript was written by CR and LB and all authors commented on previous version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Romagnolo, C., Cottignoli, C., Palucci, A. et al. Pictorial essay: incidental findings on 18F-Fluciclovine PET/CT scan. Clin Transl Imaging 9, 189–198 (2021). https://doi.org/10.1007/s40336-021-00412-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-021-00412-5