Abstract
The management of men with advanced prostate cancer has become a dynamic field due to the approval of several agents in the castration-resistant state of the disease (abiraterone acetate, enzalutamide, docetaxel, cabazitaxel, radium-223), the technical advances of radiation therapy (IMRT; stereotactic body radiation) and not at least due to significant innovations in the field of imaging modalities. Several distinct disease states of prostate cancer can be identified, with specific needs with regard to imaging modalities. The manuscript will discuss the following disease states: castration-naïve metastatic prostate cancer, oligometastatic prostate cancer, castration-resistant prostate cancer (non-metastatic M0 and metastatic M1). Imaging in advanced prostate cancer generally consists of bone scintigraphy and contrast enhanced-computed tomography (CT). Increasingly more sophisticated technologies including multiparametric MRI, PET/CT (with different tracers) and hybrid PET/CT-MRI techniques are discussed and in larger centres available also outside of clinical trials. Many questions, however, are unsolved and as of now it is unclear whether the increased diagnostic sensitivity/specificity of these imaging technologies translates into a relevant clinical benefit for men with advanced prostate cancer in the sense of improvement of clinical outcome or guiding treatment decision. This opinion piece will reflect some of the areas of unmet needs in the management of men with advanced prostate cancer that oncologists face in daily practice as perceived by the authors.

Similar content being viewed by others
References
Pezaro CJ, Omlin A, Lorente D et al (2014) Visceral disease in castration-resistant prostate cancer. Eur Urol 65:270–273
Schmid S, Omlin A, Blum D et al (2015) Assessment of anticancer-treatment outcome in patients with metastatic castration-resistant prostate cancer-going beyond PSA and imaging, a systematic literature review. Ann Oncol 26:2221–2247
Scher HI, Halabi S, Tannock I et al (2008) Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol 26:1148–1159
Gillessen S, Omlin A, Attard G et al (2015) Management of patients with advanced prostate cancer: recommendations of the St Gallen Advanced Prostate Cancer Consensus Conference (APCCC) 2015. Ann Oncol 26:1589–1604
Scher HI, Morris MJ, Stadler WM et al (2016) Trial design and objectives for castration-resistant prostate cancer: updated recommendations from the Prostate Cancer Clinical Trials Working Group 3. J Clin Oncol 34(12):1402–1418
Messiou C, Cook G, Reid AH et al (2011) The CT flare response of metastatic bone disease in prostate cancer. Acta Radiol 52:557–561
Ryan CJ, Shah S, Efstathiou E et al (2011) Phase II study of abiraterone acetate in chemotherapy-naive metastatic castration-resistant prostate cancer displaying bone flare discordant with serologic response. Clin Cancer Res 17:4854–4861
Sartor O, Eisenberger M, Kattan MW et al (2013) Unmet needs in the prediction and detection of metastases in prostate cancer. Oncologist 18:549–557
Tombal B, Lecouvet F (2012) Modern detection of prostate cancer’s bone metastasis: is the bone scan era over? Adv Urol 2012:893193
Shen G, Deng H, Hu S, Jia Z (2014) Comparison of choline-PET/CT, MRI, SPECT, and bone scintigraphy in the diagnosis of bone metastases in patients with prostate cancer: a meta-analysis. Skeletal Radiol 43:1503–1513
Hartman RP, Sundaram M, Okuno SH, Sim FH (2004) Effect of granulocyte-stimulating factors on marrow of adult patients with musculoskeletal malignancies: incidence and MRI findings. AJR Am J Roentgenol 183:645–653
Yu YS, Li WH, Li MH et al (2015) False-positive diagnosis of disease progression by magnetic resonance imaging for response assessment in prostate cancer with bone metastases: a case report and review of the pitfalls of images in the literature. Oncol Lett 10:3585–3590
James ND, Sydes MR, Clarke NW et al (2016) Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet 387(10024):1163–1177
Sweeney CJ, Chen YH, Carducci M et al (2015) Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med 373:737–746
Parker C, Gillessen S, Heidenreich A et al (2015) Cancer of the prostate: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 26(Suppl 5):v69–v77
Tannock IF, Sternberg CN (2016) Many men with castrate-sensitive metastatic prostate cancer should not receive chemotherapy. Ann Oncol 27:545–546
Lecouvet FE, Geukens D, Stainier A et al (2007) Magnetic resonance imaging of the axial skeleton for detecting bone metastases in patients with high-risk prostate cancer: diagnostic and cost-effectiveness and comparison with current detection strategies. J Clin Oncol 25:3281–3287
Venkitaraman R, Cook GJ, Dearnaley DP et al (2009) Does magnetic resonance imaging of the spine have a role in the staging of prostate cancer? Clin Oncol (R Coll Radiol) 21:39–42
Venkitaraman R, Cook GJ, Dearnaley DP et al (2009) Whole-body magnetic resonance imaging in the detection of skeletal metastases in patients with prostate cancer. J Med Imaging Radiat Oncol 53:241–247
Freitag MT, Bickelhaupt S, Ziener C et al (2016) Selected clinically established and scientific techniques of diffusion-weighted MRI: in the context of imaging in oncology. Radiologe 56:137–147
Lecouvet FE, El Mouedden J, Collette L et al (2012) Can whole-body magnetic resonance imaging with diffusion-weighted imaging replace Tc 99 m bone scanning and computed tomography for single-step detection of metastases in patients with high-risk prostate cancer? Eur Urol 62:68–75
Pasoglou V, Michoux N, Peeters F et al (2015) Whole-body 3D T1-weighted MR imaging in patients with prostate cancer: feasibility and evaluation in screening for metastatic disease. Radiology 275:155–166
Taouli B, Beer AJ, Chenevert T et al (2016) Diffusion-weighted imaging outside the brain: consensus statement from an ISMRM-sponsored workshop. J Magn Reson Imaging. doi:10.1002/jmri.25196
Beheshti M, Vali R, Waldenberger P et al (2009) The use of F-18 choline PET in the assessment of bone metastases in prostate cancer: correlation with morphological changes on CT. Mol Imaging Biol 11:446–454
Picchio M, Spinapolice EG, Fallanca F et al (2012) [11C]Choline PET/CT detection of bone metastases in patients with PSA progression after primary treatment for prostate cancer: comparison with bone scintigraphy. Eur J Nucl Med Mol Imaging 39:13–26
Evangelista L, Bertoldo F, Boccardo F et al (2016) Diagnostic imaging to detect and evaluate response to therapy in bone metastases from prostate cancer: current modalities and new horizons. Eur J Nucl Med Mol Imaging 43(8):1546–1562
Minamimoto R, Loening A, Jamali M et al (2015) Prospective comparison of 99mTc-MDP scintigraphy, combined 18F-NaF and 18F-FDG PET/CT, and whole-body MRI in patients with breast and prostate cancer. J Nucl Med 56:1862–1868
Morigi JJ, Stricker PD, van Leeuwen PJ et al (2015) Prospective comparison of 18F-fluoromethylcholine versus 68 Ga-PSMA PET/CT in prostate cancer patients who have rising PSA after curative treatment and are being considered for targeted therapy. J Nucl Med 56:1185–1190
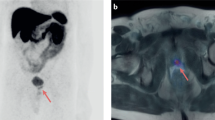
Freitag MT, Radtke JP, Hadaschik BA et al (2016) Comparison of hybrid (68)Ga-PSMA PET/MRI and (68)Ga-PSMA PET/CT in the evaluation of lymph node and bone metastases of prostate cancer. Eur J Nucl Med Mol Imaging 43:70–83
Ost P, Bossi A, Decaestecker K et al (2015) Metastasis-directed therapy of regional and distant recurrences after curative treatment of prostate cancer: a systematic review of the literature. Eur Urol 67:852–863
Gillessen S, Fanti S, Omlin A et al (2015) Reply to the letter to the editor ‘management of patients with advanced prostate cancer: recommendations of the St Gallen Advanced Prostate Cancer Consensus Conference (APCCC) 2015’ by Gillessen et al. Ann Oncol 26:2354–2355
Fanti S, Minozzi S, Castellucci P et al (2016) PET/CT with (11)C-choline for evaluation of prostate cancer patients with biochemical recurrence: meta-analysis and critical review of available data. Eur J Nucl Med Mol Imaging 43:55–69
Nanni C, Zanoni L, Pultrone C et al (2016) F-FACBC (anti1-amino-3-F-fluorocyclobutane-1-carboxylic acid) versus C-choline PET/CT in prostate cancer relapse: results of a prospective trial. Eur J Nucl Med Mol Imaging 43(9):1601–1610
Odewole OA, Tade FI, Nieh PT et al (2016) Recurrent prostate cancer detection with anti-3-[F]FACBC PET/CT: comparison with CT. Eur J Nucl Med Mol Imaging. doi:10.1007/s00259-016-3383-8
Panebianco V, Barchetti F, Grompone MD et al (2016) Magnetic resonance imaging for localization of prostate cancer in the setting of biochemical recurrence. Urol Oncol 34(7):303–310
Panebianco V, Barchetti F, Sciarra A et al (2015) Multiparametric magnetic resonance imaging vs. standard care in men being evaluated for prostate cancer: a randomized study. Urol Oncol 33(17):e11–e17
Kitajima K, Murphy RC, Nathan MA et al (2014) Detection of recurrent prostate cancer after radical prostatectomy: comparison of 11C-choline PET/CT with pelvic multiparametric MR imaging with endorectal coil. J Nucl Med 55:223–232
Souvatzoglou M, Eiber M, Takei T et al (2013) Comparison of integrated whole-body [11C]choline PET/MR with PET/CT in patients with prostate cancer. Eur J Nucl Med Mol Imaging 40:1486–1499
Schilling D, Schlemmer HP, Wagner PH et al (2008) Histological verification of 11C-choline-positron emission/computed tomography-positive lymph nodes in patients with biochemical failure after treatment for localized prostate cancer. BJU Int 102:446–451
Morand Piert M, El Naqa I, Davenport MS et al (2016) PET/MRI and prostate cancer. Clin Transl Imaging 1–13. doi:10.1007/s40336-016-0192-9
Beer TM, Armstrong AJ, Rathkopf DE et al (2014) Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med 371:424–433
Ryan CJ, Smith MR, de Bono JS et al (2013) Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med 368:138–148
Smith MR, Antonarakis ES, Ryan CJ et al (2016) Phase 2 study of the safety and antitumor activity of apalutamide (ARN-509), a potent androgen receptor antagonist, in the high-risk nonmetastatic castration-resistant prostate cancer cohort. Eur Urol. doi:10.1016/j.eururo.2016.04.023
Yu EY, Miller K, Nelson J et al (2012) Detection of previously unidentified metastatic disease as a leading cause of screening failure in a phase III trial of zibotentan versus placebo in patients with nonmetastatic, castration resistant prostate cancer. J Urol 188:103–109
Tombal B (2012) Non-metastatic CRPC and asymptomatic metastatic CRPC: which treatment for which patient? Ann Oncol 23(Suppl 10):x251–x258
Armstrong AJ, Eisenberger MA, Halabi S et al (2012) Biomarkers in the management and treatment of men with metastatic castration-resistant prostate cancer. Eur Urol 61:549–559
Morris MJ, Autio KA, Basch EM et al (2013) Monitoring the clinical outcomes in advanced prostate cancer: what imaging modalities and other markers are reliable? Semin Oncol 40:375–392
Caffo O, Palermo A, Veccia A et al (2013) Biochemical and objective response to abiraterone acetate withdrawal: incidence and clinical relevance of a new scenario for castration-resistant prostate cancer. Urology 82:1090–1093
Perez-Lopez R, Lorente D, Blackledge MD et al (2016) Volume of bone metastasis assessed with whole-body diffusion-weighted imaging is associated with overall survival in metastatic castration-resistant prostate cancer. Radiology 280(1):151–160
Blackledge MD, Collins DJ, Tunariu N et al (2014) Assessment of treatment response by total tumor volume and global apparent diffusion coefficient using diffusion-weighted MRI in patients with metastatic bone disease: a feasibility study. PLoS ONE 9:e91779
Padhani AR, Makris A, Gall P et al (2014) Therapy monitoring of skeletal metastases with whole-body diffusion MRI. J Magn Reson Imaging 39:1049–1078
Mateo J, Carreira S, Sandhu S et al (2015) DNA-repair defects and olaparib in metastatic prostate cancer. N Engl J Med 373:1697–1708
Balogova S, Zakoun JB, Michaud L et al (2014) Whole-body 18F-fluorocholine (FCH) PET/CT and MRI of the spine for monitoring patients with castration-resistant prostate cancer metastatic to bone: a pilot study. Clin Nucl Med 39:951–959
Ono M, Oka S, Okudaira H et al (2015) [(14)C]Fluciclovine (alias anti-[(14)C]FACBC) uptake and ASCT2 expression in castration-resistant prostate cancer cells. Nucl Med Biol 42:887–892
Simoncic U, Perlman S, Liu G et al (2015) Comparison of NaF and FDG PET/CT for assessment of treatment response in castration-resistant prostate cancers with osseous metastases. Clin Genitourin Cancer 13:e7–e17
Patchell RA, Tibbs PA, Regine WF et al (2005) Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet 366:643–648
Husband DJ, Grant KA, Romaniuk CS (2001) MRI in the diagnosis and treatment of suspected malignant spinal cord compression. Br J Radiol 74:15–23
Pezaro C, Omlin A, Perez-Lopez R et al (2015) Progressive computed tomography (CT) appearances preceding malignant spinal cord compression (MSCC) in men with castration-resistant prostate cancer. Clin Radiol 70:359–365
Sartor O, Coleman R, Nilsson S et al (2014) Effect of radium-223 dichloride on symptomatic skeletal events in patients with castration-resistant prostate cancer and bone metastases: results from a phase 3, double-blind, randomised trial. Lancet Oncol 15:738–746
Etchebehere EC, Araujo JC, Fox PS et al (2015) Prognostic factors in patients treated with 223Ra: the role of skeletal tumor burden on baseline 18F-fluoride PET/CT in predicting overall survival. J Nucl Med 56:1177–1184
Kwee SA, Lim J, Watanabe A et al (2014) Prognosis related to metastatic burden measured by (1)(8)F-fluorocholine PET/CT in castration-resistant prostate cancer. J Nucl Med 55:905–910
Garcia Garzon JR, Bassa P, Soler M et al (2015) Therapeutic algorithm guided by sequential 11C-choline PET/CT in a patient with metastatic castration-resistant prostate cancer. Clin Nucl Med 40:600–601
Yu EY, Duan F, Muzi M et al (2015) Castration-resistant prostate cancer bone metastasis response measured by 18F-fluoride PET after treatment with dasatinib and correlation with progression-free survival: results from American College of Radiology Imaging Network 6687. J Nucl Med 56:354–360
Gundem G, Van Loo P, Kremeyer B et al (2015) The evolutionary history of lethal metastatic prostate cancer. Nature 520:353–357
Lorente D, Omlin A, Zafeiriou Z, Nava-Rodrigues D, Pérez-López R, Pezaro C, Mehra N, Sheridan E, Figueiredo I, Riisnaes R, Miranda S, Crespo M, Flohr P, Mateo J, Altavilla A, Ferraldeschi R, Bianchini D, Attard G, Tunariu N, de Bono J (2016) Castration-resistant prostate cancer tissue acquisition from bone metastases for molecular analyses. Clin Genitourin Cancer. doi:10.1016/j.clgc.2016.04.016
McKay RR, Zukotynski KA, Werner L et al (2014) Imaging, procedural and clinical variables associated with tumor yield on bone biopsy in metastatic castration-resistant prostate cancer. Prostate Cancer Prostatic Dis 17:325–331
Kratochwil C, Giesel FL, Stefanova M et al (2016) PSMA-targeted radionuclide therapy of metastatic castration-resistant prostate cancer with Lu-177 labeled PSMA-617. J Nucl Med. doi:10.2967/jnumed.115.171397
Ceci F, Castellucci P, Graziani T et al (2016) (11)C-Choline PET/CT in castration-resistant prostate cancer patients treated with docetaxel. Eur J Nucl Med Mol Imaging 43:84–91
De Giorgi U, Caroli P, Burgio SL et al (2014) Early outcome prediction on 18F-fluorocholine PET/CT in metastatic castration-resistant prostate cancer patients treated with abiraterone. Oncotarget 5:12448–12458
De Giorgi U, Caroli P, Scarpi E et al (2015) (18)F-Fluorocholine PET/CT for early response assessment in patients with metastatic castration-resistant prostate cancer treated with enzalutamide. Eur J Nucl Med Mol Imaging 42:1276–1283
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The following conflicts of interest have to be reported: AO advisory boards (compensated, institutional): Bayer, Astellas, Janssen, Sanofi, Pfizer. Travel support: Bayer, Astellas, Janssen, Sanofi. JM: no conflicts of interest. SG: advisory boards (compensated institutional) Astellas, Bayer, Curevac, Dendreon, Janssen Cilag, Janssen Diagnostics, Millennium, Novartis, Orion Pharma, Pfizer, Sanofi Aventis. Advisory Boards (uncompensated): ProteoMediX, ESSA Pharmaceuticals Corp. Speakers Bureau (without honorarium): Amgen, Astellas, Bayer, Janssen Cilag, Sanofi Aventis. Patent: Pending patent application for a method for biomarker WO 2009138392 A1.
Rights and permissions
About this article
Cite this article
Omlin, A., Mueller, J. & Gillessen, S. The oncologists’ unmet clinical needs for imaging in advanced prostate cancer. Clin Transl Imaging 4, 423–431 (2016). https://doi.org/10.1007/s40336-016-0204-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-016-0204-9