Abstract
Introduction
Several observational studies have been conducted to assess the prevalence of cardiovascular risk factors in hypertensive patients; however, none has yet investigated prevalence, clustering, and current management of cardiovascular risk factors upon first referral to hypertension specialists, which is the aim of the present study.
Methods
Consecutive adult outpatients with essential/secondary hypertension were included at the time of their first referral to hypertension specialists at 13 Italian centers in the period April 2022–2023 if they had at least one additional major cardiovascular risk factor among LDL-hypercholesterolemia, type 2 diabetes, and cigarette smoking. Prevalence, degree of control, and current management strategies of cardiovascular risk factors were assessed.
Results
A total of 255 individuals were included, 40.2% women and 98.4% Caucasian. Mean age was 60.3±13.3 years and mean blood pressure [BP] was 140.3±17.9/84.8±12.3 mmHg). Most participants were smokers (55.3%), had a sedentary lifestyle (75.7%), suffered from overweight/obesity (51%) or high LDL-cholesterol (41.6%), had never adopted strategies to lose weight (55.7%), and were not on a low-salt diet (57.4%). Only a minority of patients reported receiving specialist counseling, and 27.9% had never received recommendations to correct unhealthy lifestyle habits. Nearly 90% of individuals with an estimated high/very high cardiovascular risk profile did not achieve recommended LDL-cholesterol targets.
Conclusions
In patients with hypertension, both pharmacological and lifestyle therapeutic advice are yet to improve before referral to hypertension specialists. This should be considered in the primary care setting in order to optimize cardiovascular risk management strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
With nearly 18 million deaths annually, cardiovascular disease (CVD) is the leading cause of premature mortality for non-communicable diseases (NCDs) worldwide, far exceeding the burden associated with the next most common NCDs, namely cancer, chronic lung disease, and diabetes [1]. In view of the heavy individual and socio- economic costs related to CVD and other NCDS, the 2030 Agenda for Sustainable Development included a target to reduce by one third premature mortality from these four major NCDs by 2030 through their prevention and treatment [2].
Several non-modifiable and modifiable traits and conditions contribute to the development of CVD, spanning from demographic features to lifestyle factors, environmental exposures, (epi)genetic determinants, and their clusters [3]. Unlike the increased risk load attributable to older age, male gender, or family history of premature CVD, the burden derived from major metabolic and behavioral risk factors—including hypertension [4], diabetes/insulin resistance, dyslipidemia, and tobacco smoking [3, 5]—could be prevented through timely identification and the adoption of effective strategies for their control. Educational campaigns on the importance of healthy lifestyles, including a balanced diet, regular physical exercise, and stress management, are acknowledged as important tools to increase awareness of risks related to uncontrolled cardiovascular risk factors and promote general well-being [6,7,8,9]. Indeed, failure to prescribe the necessary lifestyle modifications and appropriate pharmacological therapy, as well as poor therapeutic adherence/persistence represent additional physician- and patient-related risk factors that contribute substantially to failure in achieving the desired cardiovascular protection [10].
Cardiovascular risk factors prevalence, distribution, and treatment patterns have been investigated in several settings, including general practice physicians and cardiovascular specialists [10,11,12]. However, there are insufficient data among hypertensive individuals referred to hypertension specialists. In this study, we provide multicenter-generated data on the prevalence and clustering of major cardiovascular risk factors and their current management in adult hypertensive patients upon their first referral to hypertension Excellence Centers of the European Society of Hypertension (ESH) affiliated with the Italian Society of Hypertension (Società Italiana dell’Ipertensione Arteriosa, SIIA).
2 Methods
2.1 Study Design and Population
We conducted a cross-sectional, multicenter, observational study (Arterial blood PRessure, smOke, diAbetes, CHolesterol and their management in hypertensive outpatients referred to European Society of Hypertension (ESH) Excellence Centers in Italy—the APPROACH study) involving 13 Excellence Centers of the ESH affiliated with the SIIA over 9 Italian regions, with the primary aim of determining the prevalence and clustering of cardiovascular risk factors, as well as the current management strategies in patients referred for the first time to hypertension specialists during a period of 12 months. Adult (≥18 years) individuals with either essential or secondary hypertension who were willing to participate in the study were eligible for inclusion if they presented with at least one additional major cardiovascular risk factor (LDL hypercholesterolemia, type 2 diabetes mellitus and cigarette smoking). Active cancer and history of organ transplantation were exclusion criteria.
2.2 Ethical Clearance
The research was conducted in compliance with the Helsinki declaration and the European General Data Protection Regulation (EU GDPR), article 89. The study protocol was approved by the local ethics committees of the coordinating centers with ID numbers 4658/2021 (Brescia) and 0034276/21 (L’Aquila). Informed consent was obtained by all participants at enrollment.
2.3 Variables of Interest
Data of interest included major demographic, anthropometric, and clinical features, as follows: age; sex; race/ethnicity (White Caucasian; other); education (primary school or less; secondary school; college degree or above); body mass index (BMI, as Kg/m2); waist circumference (cm); usual body weight and any variation in body weight in the past year; office sitting and standing BP (mmHg); concomitant cardiovascular risk factors (LDL hypercholesterolemia; type 1 or 2 diabetes; smoking habits; alcohol use; obesity; hyperuricemia) and related treatments, including medications and any professional advice and assistance for lifestyle modification (verbal recommendations; brochures; nutritional counseling; personal trainer; cognitive-behavioral counseling for smoking/alcohol cessation; drug therapy for smoking/alcohol cessation; e-cigarettes; use of smartphone apps; lifestyle changes to lose weight; none); relevant family history (hypertension, diabetes; dyslipidemia; early atherosclerotic CVD); comorbidities (including established CVD, such as personal history of atrial fibrillation, TIA/stroke, ischemic heart disease, peripheral artery disease [PAD]; established chronic kidney disease [CKD]; chronic lung diseases; rheumatic diseases; liver steatosis; previous cancer; psychosocial stress); whether on a low-salt diet; degree of physical activity; and presence of any diagnosed hypertension-mediated organ damage (HMOD, including cardiovascular, renal, neurological, and ocular damage). When available, home and ambulatory BP recordings as well as relevant laboratory parameters obtained within the previous 6 months (total cholesterol, LDL-cholesterol, HDL-cholesterol, triglycerides, uric acid, serum glucose, glycosylated hemoglobin [HbA1c], creatinine, sodium, potassium) were also collected.
2.4 BP Measurement
Participants underwent three sitting and two standing (1-3 minutes) BP measurements with standard protocols, according to guidelines, using locally available, validated semi-automated BP monitors with properly sized bladder cuffs based on upper arm circumference. Interarm BP difference was investigated to detect any significant discrepancy (>15 mmHg). Mean sitting BP and heart rate (HR) were calculated as the average of the second and third measurements. Information on antihypertensive therapy (drug class, whether they were taken on the day of the visit, and whether any dosage changes had occurred in the previous month) was also collected.
2.5 Statistical Analysis
Data were anonymously collected at enrollment and transferred to a spreadsheet for analyses. Statistics were performed using R (v 4.0.2). Data were analyzed as recorded, without imputation for missing data. Stratification based on sex was performed.
Unpaired Student’s t-test and chi-squared test were used to detect differences in quantitative (mean ± standard deviation [SD]) and qualitative (N, %) data, respectively (statistical significance: p<0.05).
BP was treated as both a numeric value (mmHg) and a categorical variable (masked/white coat/sustained/controlled hypertension based on the combination of average office seated BP and ambulatory BP [13, 14]). Based on their night-day ratio, participants with available 24 hours ABPM were also classified as dippers (ratio ≥10% of the daytime average BP), non-dippers (ratio <10%), reverse dippers (lack of night-time BP reduction to higher night-time than daytime average BP), and extreme dippers (>20% nocturnal BP fall). The prevalence of orthostatic hypotension (a decrease in systolic BP ≥20 mmHg or in diastolic BP ≥10 mmHg after 1 or 3 minutes on standing) and hypertension (an increase in systolic BP ≥20 mmHg or in diastolic BP ≥10 mmHg after 1 or 3 minutes on standing) was also assessed.
SCORE2 and SCORE2-OP were used for calculation of cardiovascular risk according to literature [15], and the proportion of participants within the recommended range of serum LDL-c according to their estimated cardiovascular risk was calculated [16]. Similarly, the proportion of diabetic participants with HbA1c <7% was assessed [17].
3 Results
3.1 BP Profile and Patients’ Features
As of the date of study closure visit on December 31st, 2022, a total of 255 outpatients (59.8% men; mean age 60.3±13.4 years) from 13 SIIA-ESH excellence centers had been enrolled. Their demographic and clinical features are shown in Table 1. Almost 1 out of 10 individuals (7.9%) was diagnosed with secondary hypertension. Most outpatients were referred to hypertension specialists after 1–5 years (26.5%) or >5 years (47%) following initiation of antihypertensive treatment; only 1 in 4 patients reported being treated for hypertension for 1 year or less. Overall, about half participants (48.6%) had been on a stable dose of antihypertensive medications during the previous month. More than 1 in 10 participants declared not taking BP medications on the day of the visit. ABPM was available for about one in 3 participants (36.2%); among them, more than half participants had abnormal nocturnal BP fluctuations (36.4% non-dippers; 8% reverse dippers; 8% extreme dippers) (Table 2). On average, mean BP was in the range of grade I hypertension in all the examined settings (office sitting, home, and 24-hours ambulatory BP). By affecting about one in 6 individuals undergoing 1- or 3-minutes standing BP measurements (n. 31/203; 15.4%), orthostatic hypotension (n. 23/203; 11.3%), and hypertension (n. 29/203; n. 14.3%) were not uncommon.
Among the additional cardiovascular risk factors, LDL-hypercholesterolemia was the most common (41.6%), followed by cigarette smoking (20.8%) and type 2 diabetes (17.6%) (Table 1, Fig. 1). Obesity and mixed dyslipidemia were also common (26.3% and 25.9%, respectively). Nearly half participants (47.8%), mostly men (61.5% vs 38.4% of females), had established HMOD (Table 1).
Modifiable cardiovascular risk factors and lifestyle habits of the examined population. Overall prevalence (%) is reported, with the exclusion of missing data (smoking habits: n. 8 participants, 3.1%; alcohol use: n. 6 participants, 2.4%; physical activity: n. 5 participants, 2.0%; low-salt diet: n. 10 participants, 3.9%; body weight changes in the past year: n. 10 participants, 3.9%; any lifestyle changes to lose weight: n. 8 participants, 3.1%).
In terms of other modifiable cardiovascular risk factors, 66.3% of participants declared occasional to low alcohol use, 30.6% were non-drinkers, and only 0.8% reported high alcohol consumption (≥3 units/day) (Fig. 1). Only 24.3% declared adequate to intense physical exercise. As to their body weight, more than half of participants declared having always been (30.6%) or having become (20.4%) overweight/obese, while 1 in 10 (10.9%) was previously overweight/obese (Table 1).
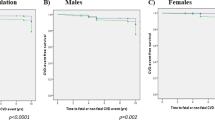
While mean age was similar between men and women, sex-based differences were observed in terms of estimated cardiovascular risk, with a larger proportion of men at very high risk compared with women (30.9% vs 18.4%, respectively). Accordingly, women had higher HDL-c and lower triglycerides and sitting office diastolic BP than men (Table 1).
3.2 Ongoing Management Strategies of Cardiovascular Risk Factors
Nearly one third of participants declared having never received recommendations to correct their lifestyle for cardiovascular prevention (Figure 2, panel A). Half of participants declared having received verbal recommendations, while one in 4 reported being referred to a nutrition specialist. Other forms of patients’ education (written recommendations, personal trainer, cognitive-behavioral counseling or drugs for smoke cessation, e-cigarette) were sparsely reported, showing limited use of the most appropriate strategies for each specific risk condition (S Table 1). No participant reported use of smartphone apps as an aid in lifestyle changes oriented towards cardiovascular benefit.
The majority of hypertensive patients (55.3%) were not on a low-salt diet (Fig. 1).
Most participants (53.7%) declared having never modified their lifestyle to lose weight: indeed, one in 5 (20.4%) declared weight gain during the previous year and 2.4% reported regaining the lost weight, while 19.2% declared weight loss (Fig. 1).
In terms of BP treatment, about 10% of participants were not taking any medications for hypertension at the time of their first visit; among treated participants, RAAS blockers were widely used (43.5% angiotensin II receptor blockers [ARBs], 29% angiotensin-converting-enzyme [ACE]-inhibitors), followed by calcium channels blockers (37.6%) and beta-blockers (35.3%) (Fig. 2, panel B).
As for medications for conditions other than hypertension, lipid-lowering drugs were the most frequently reported drugs (37.6% statin, 5.9% nutraceuticals), followed by antiplatelet agents (20.6%) (Fig. 2, panel B). All participants reporting hyperuricemia (7.9%) were taking uric acid lowering agents.
3.3 Risk Factors Control
As a result of the combination of clinical and 24-hour BP measurements, approximately half of the participants had uncontrolled (36.5%), masked (8.2%), or white coat (6.7%) hypertension (Table 2).
In parallel, LDL-c values were found above the desirable target in a wide proportion of participants. Specifically, based on their calculated cardiovascular risk score, 66.7%, 88.2%, and 89.4% of participants at low-moderate, high, and very high risk, respectively, were not at target (Table 3).
Among diabetic individuals with available HbA1c values, 6 in 10 individuals were above the target of 7% (Table 3).
3.4 Antihypertensive Treatment
Approximately half of the patients had been on a stable antihypertensive therapy for about 5 years (47%) and 26.5% for less than 1 year. Only 11% of patients referred for the first time to hypertension centers were not receiving any antihypertensive drugs. Among the others, the most represented pharmacological classes were ARB and calcium antagonists (43.7% e 37.8%, respectively), followed by beta-blockers (35.4%) and ACE-inhibitors (29.1%). As for diuretics, thiazide/thiazide-like diuretics and loop diuretics were reported in 22.8% and 4.7% of patients, respectively . A minority of patients were on mineralocorticoid receptor antagonists (3.5%) and alpha-1 blockers or centrally acting drugs (9.1%).
4 Discussion
In this study, we examined the prevalence, clustering, and ongoing management of key cardiovascular risk factors, beside hypertension, among adult patients at the time of their first referral to a hypertension specialized center. Our findings show substantial metabolic complexity in the examined population, but also concomitant significant undertreatment in terms of both pharmacological and non-pharmacological management strategies. Specifically, most hypertensive participants were smokers, had a sedentary lifestyle, were overweight/obese, suffered from high LDL-cholesterol, had never changed their habits to lose weight, and were not on a low-salt diet. Only a minority reported previous specialist counseling, and one in 3 individuals had never received recommendations to correct their unhealthy lifestyle habits. Not only hypertension, but also hypercholesterolemia and diabetes were poorly controlled. More importantly, nearly 90% of individuals with high/very high cardiovascular risk conditions did not achieve the recommended LDL-cholesterol targets.
With an age-standardized average prevalence of 34% in men and 32% in women in the age range of 30-79 years [5], hypertension is the most prevalent modifiable cardiovascular risk factor at a global scale [4], yet approximately 4 out of every 5 people with hypertension are not adequately treated [18] and less than 25% of treated patients achieve the recommended BP targets [3]. In parallel, and similar to our findings, recent data from more than 9000 high- and very high-risk adults from primary and secondary care settings enrolled in the multinational observational SANTORINI study indicate that failure to achieve LDL-cholesterol goals occurs in 80% of individuals [19, 20], which was attributed to cardiovascular risk underestimation and underutilization of combination lipid-lowering therapies.
The estimation of total cardiovascular risk is crucial in each hypertensive patient because it provides valuable information that can guide hypertension management through a personalized and individualized approach. Different patients may have varying degrees of risk based on a combination of factors such as age, gender, BP levels, cholesterol levels, smoking status, and existing comorbidities. The Systemic Coronary Risk Evaluation (SCORE) method, based on a large European database, estimates the risk of death from CVD over 10 years in either high-and low-risk European countries [21]. The more recent 2021 European Guidelines on CVD prevention updated and substituted the SCORE method with the SCORE2, which estimates the risk of fatal and nonfatal cardiovascular events over 10 years in apparently healthy individuals aged 40–69 years with stable/untreated risk factors, and the SCORE2-OP for older people (age 70–89 years) [15]. Strict control of risk factors is even more relevant in some high-risk categories, like individuals with masked hypertension and non-dipping/reverse dipping profiles, who are at increased risk of hypertension-mediated organ damage (HMOD) and cardiovascular events [4] and were not uncommon in the subset of individuals with complete BP profile in our study. Similarly, both orthostatic hypotension and hypertension are correlated with an increased risk of mortality and cardiovascular events [22, 23], and more than one in 10 individuals in our population suffered from either one of these conditions, in line with data from high-risk hypertensive populations [24]. The observation that a significant number of participants, particularly those at high and very high cardiovascular risk, did not meet the target LDL-cholesterol values highlights the need for more effective and targeted strategies for lipid management in these patients.
Regarding lifestyle behaviors, more than 30% of participants declared having never received recommendations to correct their lifestyle for cardiovascular prevention and 20.4% of participants declared having become overweight/obese. Lifestyle interventions play a pivotal role in reducing premature cardiovascular morbidity and mortality. Among all the established, effective lifestyle measures for cardiovascular well-being, weight loss in overweight or obese individuals is associated with improvements in BP, cholesterol levels, and overall cardiovascular health [25]. A regular physical activity, such as brisk walking, jogging, or cycling, has numerous cardiovascular benefits, including helping to lower BP, improve the cholesterol levels, and enhance overall cardiovascular fitness [26, 27]. However, in our population, only 24.7% declared adequate physical exercise. In parallel, consumption of fruits, vegetables, whole grains, lean proteins, and low-fat dairy products, together with reduced sodium and adequate potassium intake, has been shown to lower BP and reduce the risk of heart disease, leading to significant cardiovascular benefits [28,29,30]. Current evidence indicates that restriction of sodium intake leads to improved BP control, especially in hypertensive patients and in those at increased risk due to older age, diabetes, and metabolic syndrome [31,32,33], with the added value of a possible reduction in the number of drugs needed to achieve hypertension control [4]. The magnitude of BP benefits attributable to sodium intake restriction (< 5.8 g salt per day) was approximately 5/2 mmHg systolic/diastolic BP reductions in individuals with hypertension [34]. In agreement with this, current hypertension guidelines recommend not to exceed 2.0 g per day of sodium intake (approximately 5.0 g salt per day) [4, 13]. Still, a substantial portion of the examined hypertensive population—more than 4 in 10 individuals—reported not adhering to dietary measures to reduce sodium intake. Consuming alcohol in moderation and quit smoking are additional lifestyle measures associated with reduced risk of CVD [35, 36]. In our population, while only 0.8% reported high alcohol consumption, cigarette smoking represented the second most common risk factor, and nearly one in 4 smoker individuals had never received any recommendation to quit smoking.
With regard to antihypertensive treatments reported in our study, renin-angiotensin-system blockers, in particular ARBs, seem to represent the most frequently adopted antihypertensive strategy, in line with the most recent guidelines, followed by calcium antagonists. Unfortunately, the use of fixed-combination therapy compared to monotherapies was not investigated in our population.
Altogether, our findings highlight the need for greater integration of guidelines into clinical practice and increased patient-centeredness in the healthcare team, to ensure adequate patient understanding of the clinical benefit of a comprehensive cardiovascular prevention strategy and to identify and remove any potential barriers to virtuous lifestyle implementation. Physicians should measure office BP both in sitting and standing positions, especially in older individuals, in those with high-risk conditions, and during titration and changes of the antihypertensive treatment. This approach provides additional insights into the dynamics of BP regulation and helps healthcare providers take more informed decisions for a satisfactory management of hypertension.
This study has some limitations, including its observational nature, which does not allow any causal inferences, and the limited sample size, which should be considered in the interpretation of results and could limit their generalizability. Results could also not be generalizable to other healthcare systems. However, our study is the first to explore the degree and effectiveness of ongoing management strategies among hypertensive individuals upon their first referral to hypertension specialists, thereby providing valuable insights into hypertension management in general medicine settings that could help to overcome cultural barriers, and to tailor more targeted and effective interventions before referral to specialist care. As such, our findings may have broader implications for hypertension management.
In conclusion, this study underscores the ongoing challenges in achieving optimal BP management, emphasizing the need for greater integration of guidelines into clinical practice and implementation of a proactive patient-centered approach. Educating patients on the importance of therapeutic adherence/persistence and a healthy lifestyle, encouraging a heart-healthy diet, promoting regular physical activity, and performing periodic review and optimization of current medication regimens represent crucial points for an effective therapeutic alliance. In parallel, tailored strategies to address individual barriers to achieving risk factors control and continuous support and education through traditional and technology-based approaches can help improve cardiovascular outcomes. By addressing these issues, our study can contribute valuable data to inform healthcare policies, improve clinical practice, and enhance the overall cardiovascular health of hypertensive patients.
Data availability
The relevant data supporting the findings of this study are available upon reasonable request to the corresponding author.
References
Noncommunicable diseases. [cited 10 Feb 2024]. Available: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases#:~:text=Of%20all%20NCD%20deaths%2C%2077,disease%20deaths%20caused%20by%20diabetes
SDG Target 3.4. [cited 10 Feb 2024]. Available: https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/sdg-target-3.4-noncommunicable-diseases-and-mental-health#:~:text=Indicator%20Groups-,SDG%20Target%203.4%20%7C%20Noncommunicable%20diseases%20and%20mental%20health%3A%20By%202030,mental%20health%20and%20well%2Dbein
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the american heart association. Circulation. 2019;139:e56–528.
Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41:1874–2071.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from. to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 1990;2021(398):957–80.
Tocci G, Muiesan ML, Parati G, Agabiti Rosei E, Ferri C, Virdis A, et al. Trends in prevalence, awareness, treatment, and control of blood pressure recorded from 2004 to 2014 during world hypertension day in Italy. J Clin Hypertens. 2016;18:551–6.
Torlasco C, Faini A, Pengo MF, Borghi C, Grassi G, Ferri C, et al. May Measurement Month 2019: an analysis of blood pressure screening results from Italy. Eur Heart J Suppl. 2021;23:B77–81.
Del Pinto R, Grassi G, Muiesan ML, Borghi C, Carugo S, Cicero AFG, et al. World Hypertension Day 2021 in Italy: Results of a Nationwide Survey. High Blood Press Cardiovasc Prev. 2022;29:353–9.
Del Pinto R, Pagliacci S, De Feo M, Grassi D, Ferri C, Italian Society of Hypertension and Federfarma. Prevalence of hypertension and associated cardiovascular risk factors among pharmacies customers: an Italian nationwide epidemiological survey. Eur J Prev Cardiol. 2020;27: 1228–1230.
Del Pinto R, Desideri G, Ferri C, Agabiti RE. Real-world Antihypertensive treatment patterns, treatment adherence, and blood pressure control in the elderly: an italian awareness-raising campaign on hypertension by senior italia federanziani, the italian society of hypertension and the italian federation of general practitioners. High Blood Press Cardiovasc Prev. 2021;28:457–66.
Pokharel Y, Tang F, Jones PG, Nambi V, Bittner VA, Hira RS, et al. Adoption of the 2013 American College of Cardiology/American Heart Association Cholesterol Management Guideline in Cardiology Practices Nationwide. JAMA Cardiol. 2017;2:361–9.
Agabiti Rosei C, Del Pinto R, Grassi G, Muiesan ML, Ferri C. Prevalence of cardiovascular risk factors and related medical and lifestyle interventions among italian cardiovascular specialists: a proof-of-concept study. High Blood Press Cardiovasc Prev. 2023;30:255–64.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42:3227–337.
SCORE2 working group and ESC Cardiovascular risk collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42:2439–54.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111–88.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323.
Hypertension report. [cited 10 Feb 2024]. Available: https://www.who.int/teams/noncommunicable-diseases/hypertension-report
Ray KK, Haq I, Bilitou A, Manu MC, Burden A, Aguiar C, et al. Treatment gaps in the implementation of LDL cholesterol control among high- and very high-risk patients in Europe between 2020 and 2021: the multinational observational SANTORINI study. Lancet Reg Health Eur. 2023;29: 100624.
Dixon DL, Sharma G, Sandesara PB, Yang E, Braun LT, Mensah GA, et al. Therapeutic Inertia in cardiovascular disease prevention: time to move the bar. J Am Coll Cardiol. 2019;74:1728–31.
Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003.
Dani M, Dirksen A, Taraborrelli P, Panagopolous D, Torocastro M, Sutton R, et al. Orthostatic hypotension in older people: considerations, diagnosis and management. Clin Med. 2021;21:e275–82.
Hoshide S, Matsui Y, Shibasaki S, Eguchi K, Ishikawa J, Ishikawa S, et al. Orthostatic hypertension detected by self-measured home blood pressure monitoring: a new cardiovascular risk factor for elderly hypertensives. Hypertens Res. 2008;31:1509–16.
Townsend RR, Chang TI, Cohen DL, Cushman WC, Evans GW, Glasser SP, et al. Orthostatic changes in systolic blood pressure among SPRINT participants at baseline. J Am Soc Hypertens. 2016;10:847–56.
Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–84.
Cornelissen VA, Buys R, Smart NA. Endurance exercise beneficially affects ambulatory blood pressure: a systematic review and meta-analysis. J Hypertens. 2013;31:639–48.
Noone C, Leahy J, Morrissey EC, Newell J, Newell M, Dwyer CP, et al. Comparative efficacy of exercise and anti-hypertensive pharmacological interventions in reducing blood pressure in people with hypertension: a network meta-analysis. Eur J Prev Cardiol. 2020;27:247–55.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336: 1117–1124.
Filippini T, Malavolti M, Whelton PK, Naska A, Orsini N, Vinceti M. Blood pressure effects of sodium reduction: dose-response meta-analysis of experimental studies. Circulation. 2021;143:1542–67.
Binia A, Jaeger J, Hu Y, Singh A, Zimmermann D. Daily potassium intake and sodium-to-potassium ratio in the reduction of blood pressure: a meta-analysis of randomized controlled trials. J Hypertens. 2015;33:1509–20.
Chen J, Gu D, Huang J, Rao DC, Jaquish CE, Hixson JE, et al. Metabolic syndrome and salt sensitivity of blood pressure in non-diabetic people in China: a dietary intervention study. Lancet. 2009;373:829–35.
Suckling RJ, He FJ, Markandu ND, MacGregor GA. Modest salt reduction lowers blood pressure and albumin excretion in impaired glucose tolerance and type 2 diabetes mellitus: a randomized double-blind trial. Hypertension. 2016;67:1189–95.
Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell’Italia LJ, et al. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension. 2009;54:475–81.
Cutler JA, Follmann D, Allender PS. Randomized trials of sodium reduction: an overview. Am J Clin Nutr. 1997;65:643S-651S.
Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e108–20.
Saha SP, Bhalla DK, Whayne TF Jr, Gairola C. Cigarette smoke and adverse health effects: an overview of research trends and future needs. Int J Angiol. 2007;16:77–83.
Acknowledgements
RDP acknowledges the PROMOTE-BP grant from Eklund Foundation (2022), the NIH/ORWH (3R01DK042191-30S1, administrative supplement for Research on Sex/Gender Differences) and the Crohn’s & Colitis Foundation (882725, Clinical Research Investigator-Initiated Award (CRIA)-Senior Research Award (SRA)). RDP and CAR are Young Investigators of the Italian Society of Hypertension. MLM is President of the Italian Society of Hypertension. MV is supported by a grant of Italian Ministry of Health (ricercar corrente)
Funding
Open access funding provided by Università degli Studi dell’Aquila within the CRUI-CARE Agreement. None specific.
Author information
Authors and Affiliations
Contributions
RDP and CAR contributed equally to this work. CF conceived the study and interpreted the results. All authors participated to data collection. RDP performed statistics and data visualization. RDP and CAR drafted the first manuscript. RDP, CAR, MLM, CF, MV contributed to the interpretations of the findings and the critical revision of the manuscript. All authors agreed to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interests in relation to the current study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Del Pinto, R., Agabiti Rosei, C., Di Guardo, A. et al. Prevalence, Clustering, and Current Management of Cardiovascular Risk Factors Upon First Referral to Hypertension Specialists: the APPROACH Study. High Blood Press Cardiovasc Prev (2024). https://doi.org/10.1007/s40292-024-00650-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40292-024-00650-4