Abstract
Introduction
The number of Italian citizens unaware of their risk of cardiovascular disease it is still very high.
Aim
This study aimed to translate and preliminarily validate a brief Italian version of the Perception of Risk of Heart Disease Scale (PRHDS).
Methods
PRHDS was culturally adapted to the Italian context. Then, the scale was administered to 772 healthy adults. By randomly dividing the sample into two subsamples, we tested the scale dimensionality through Exploratory Factor Analysis (EFA) followed by Confirmatory Factor Analysis (CFA). Finally, we evaluated internal consistency.
Results
Psychometric properties of the scale were appropriate. EFA and CFA evidenced a unidimensional structure of a brief version of the scale, composed of six items. Internal consistency was adequate.
Conclusions
Italian version of the brief PRHDS is a promising self-report questionnaire to measure cardiovascular risk perception among Italian adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cardiovascular diseases (CVD) still represent the leading cause of death globally. The burden of CVD represented by the number of disability-adjusted life years (DALY) and deaths, continues to increase as well as the burden attributable to modifiable risk factors [1].
Despite efforts to increase the awareness of modifiable cardiovascular risk factors in primary and secondary prevention, the number of patients with unknown arterial hypertension, one of the most relevant risk factors for CVD, is still on the rise [2, 3]. Thus, there is room for further improvement in the awareness and knowledge of the subjects' cardiovascular risk profile to prevent the development of target organ damage and, ultimately, CVD.
Data from the REduction of Atherothrombosis for Continued Health Registry in Europe showed that the patients’ awareness of their risk factor profile is positively related to better control of their cardiovascular risk factors [4]. However, data on awareness are conflicting: some studies have highlighted that patient underestimate their risk profile [5, 6] but other studies did not confirm this evidence. For example, the Patient and Provider Assessment of Lipid Management Registry data showed that most patients overestimate their 10-year CV risk [7].
Using validated self-reported questionnaires would make it possible to record patients' perception of cardiovascular risk in a simple, fast, and reliable way however, the subjects' perceived cardiovascular risk is often self-assessed without adopting validated questionnaires. Several questionnaires are available in the literature: the Heart Disease Fact Questionnaire [8], a 25-item questionnaire to evaluate the respondents' knowledge of major risk factors for the development of heart disease; the Health Beliefs Related to Cardiovascular Disease, a 25-item designed to measure beliefs related to cardiovascular disease risk and diet and exercise in adults with diabetes and the Attitudes and Beliefs about Cardiovascular Disease Risk Questionnaire, a 26 items scale developed for Health Check programmes in United Kingdom [9].
We elected to evaluate a 20-item tool that estimates the subjects' perceived risk of developing CVD, the Perception of Risk of Heart Disease Scale (PRHDS) [10] that was preferred because of the lower number of items that could be more easily administered with a web-based platform.
As this scale was not validated in Italian, this study aimed at validating the PRHDS in the Italian language, administering its translation to a sample of healthy adults, and investigating its preliminary psychometric properties, thus making it available for Italian epidemiologic studies investigating CVD risk.
2 Materials and Methods
2.1 Participants
The data were collected via an anonymous online survey generated with the Google Form platform using a snowball sampling method between February and July 2022. The volunteers were recruited from the researchers' pool of acquaintances, word of mouth, and online social networks. All individuals with the following characteristics were eligible for enrollment: adults aged at least 18 years and individuals who could answer the online questionnaire independently. This second criterion translated into the ability to read and understand written Italian and the ability to use the computer to answer the questionnaire. Individuals diagnosed with cardiovascular disease were excluded from study participation for consistency with the original validation study [10].
People could access the questionnaire through an anonymous link without having to authenticate. The study was conducted following the American Psychological Association [11] ethical standards for treating human experimental volunteers and with the understanding and the written consent of each participant in compliance with the indications of the Declaration of Helsinki. Indeed, the participants were informed about the purposes of the study and gave informed consent electronically, and they could abandon completing the questionnaire without consequences. Privacy and anonymity were guaranteed to all participants. The data collected were stored electronically and managed only for scientific research, according to Italian Legislative Decree No. 101 of 10 August 2018, which regulates the protection of individuals concerning the processing of personal data.
2.2 Translation of the PRHDS Dread Risk
After obtaining the authors' written consent for the instrument's use and translation, PRHDS was culturally adapted to the Italian context. The adaptation of Brislin's model was used as a guide [12]. According to this methodology, a team approach was used during the retranslation process, which guaranteed high accuracy in the various stages of the cultural adaptation process. Two bilingual authors translated the text from English into Italian independently. A third investigator retranslated each version of the Italian text into the original (English) language.
Subsequently, all authors met in a consensus meeting to discuss the forward translation and find the best solution for the Italian context. A native speaker translated the final version of the instrument back into English. Finally, the instrument was submitted to the original author, who approved the new text formulation.
Following the recommendations of Polit and Beck [13], the face and content validity of the PRHDS were tested. Six panelists from outside the research group were involved: two nurses, two physicians, and two lay people. The panel of experts consisted of four women and two men. All experts had a university degree, and three had a Ph.D. Three open-ended questions were submitted to the panel to assess the instrument's face validity. We first asked these experts to rate each item's relevance to the conceptual definition. Then, we asked them to critique the clarity of each item in terms of content and style. Finally, we asked them to evaluate items' comprehensiveness on dichotomous and 4-point scales ranging from 1 (not relevant) to 4 (very relevant).
One of the most widely used measures to define content validity is the content validity index (CVI) [14]. The CVI includes the calculation of the Item Content Validity Index (I-CVI) and the Scale Validity Index (S-CVI).
The I-CVI is the index of inter-rater agreement [14] regarding the content validity of an individual scale item by simply expressing the proportion of agreement [15]. Content experts are asked to rate each item of the assessment instrument in terms of its relevance to the construct [15]. This is usually calculated by summing the number of experts who gave each item a rating of 3 or 4 on a 4-point Likert scale (1 = not relevant, 2 = somewhat relevant, 3 = fairly relevant, 4 = very relevant) [14] divided by the total number of experts involved in the rating [14, 15]. According to Lynn [16], the minimum acceptable value of I-CVI is closely related to the number of experts involved in the evaluation [14]. In fact, Lynn states that with a number of experts of six, the minimum acceptable I-CVI is 0.83 [14, 15], i.e. only one dissenting opinion (<4 on the Likert scale) [15]. Researchers have used the information on the I-CVI to guide them in the revision, deletion or replacement of items [15].
The S-CVI indicates the content validity of the overall scale [15]. To validate the PRHDS, the researchers used the Scale Validity Index Average (S-CVI/AVE), which is the average of the I-CVI for all items in the scale being assessed [15]. According to the literature, the standard criterion for acceptability when calculating the S-CVI/AVE is 0.80 [14]. This parameter has been calculated as the sum of the values of the individual I-CVIs divided by the number of items under analysis [14, 15].
2.3 Assessment of Other Indicators
In addition to the Italian version of the PRHDS, the online questionnaire collected demographic (i.e., age, gender, education, working status, marital status) and anthropometric (body mass index, BMI) information. Moreover, it collected clinical information (family history of cardiovascular diseases) and information about the presence of cardiovascular risk factors (hypertension, hypercholesterolemia, and diabetes). Age and BMI were treated as continuous variables. All the other variables were treated as dichotomous variables (Table 1).
Perceived Health was assessed through a single question. Participants had to complete the sentence “Would you say your health is” by marking an adjective on a 5-point Likert scale, where 1 was “bad”, and 5 was “excellent”.
2.4 Statistical Analysis
The items of the Brief PRHDS were preliminarily submitted to analyses to check the normal distribution by calculating mean, standard deviation, and indices of skewness and kurtosis; West and colleagues [17] recommend concern if skewness > |2| and kurtosis > |7|.
We used a brief version of the original scale. Therefore, using two different samples, we tested its dimensionality through Exploratory Factor Analysis (EFA) followed by Confirmatory Factor Analysis (CFA). This approach is the most common to scale development and validation [18]. Our sample size (772 individuals) was sufficient to use EFA in a random split-half of the sample and CFA in the second split-half. The minimum sample size for carrying out the factorial analysis was established following the indications of Nunnally [19], who suggested that the minimum ratio between the number of subjects and the number of variables is 10:1. In the case of the present study, the minimum number of subjects for conducting the analyses was 140. Therefore, the total sample was randomly divided into two samples of 386 individuals.
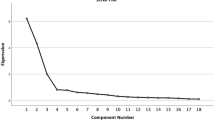
Regarding EFA, we ran the Kaiser Meyer Olkin (KMO) and Bartlett's test of sphericity to be sure that the correlation matrix could be subjected to analyses. KMO should be > 0.6, and Bartlett's test of sphericity should be significant. The criterion of eigenvalue greater than one, analysis of the scree plot, explained variance and theoretical sense determined the best-fitting factor solution. In the first stage, all items were included. Subsequent factor analyzes were conducted iteratively, eliminating one item at a time until a stable factor solution was found. Items with a factor loading < 0.32 were progressively excluded. After the first step, items loading at > 0.32 on more than one factor were excluded. Loadings in the 0.32 range or above are generally considered the cut-off on substantial loadings [20].
Regarding CFA, we used the Maximum Likelihood (ML) estimation method. A unidimensional factor model was tested to examine the factorial structure of the Brief PRHDS. The model loaded all items onto a single latent factor, assuming that all items tap into the same underlying latent construct (i.e., Cardiovascular Risk Perception). The model was initially run without specified error correlations. The potential modification of this model was based on the modification indices and content-based considerations. The goodness of fit of the model was evaluated using the χ2, the Tucker–Lewis incremental fit Index (TLI) [21], the Comparative Fit Index (CFI) [22], the standardized root-mean-square residual (SRMR; Pavlov et al., 2020), and the Root Mean Square Error of Approximation (RMSEA) [23]. Values close to 0.06 for the SRMR and RMSEA indicate a good fit; between 0.06 and 0.08 a moderate fit and values larger than 0.10 indicate a poor fit [24]. For the CFI and TLI, values of 0.95 or above indicate a good fit, whereas values of 0.90 and < 0.95 are taken as marginally acceptable fit [24].
The reliability of the Brief PRHDS was assessed based on internal consistency, calculating Cronbach’s alpha (1971), McDonald’s omega (1999), and the item’s inter-correlation coefficients. Cronbach’s alpha and McDonald’s omega above 0.60 are acceptable, and the item's inter-correlation coefficients higher than 0.30 are adequate [25].
Finally, we investigated the association of the Brief PRHDS scores with sociodemographic variables (i.e., age, gender, education, marital status), health status indicators (i.e., BMI, family history of cardiovascular diseases, hypertension, hypercholesterolemia, and diabetes) and the perceived health measure.
The association between the Brief PRHDS scores and continuous variables (i.e., age, BMI, and perceived health) was evaluated by correlations. Following guidelines by Cohen (1988), we interpreted correlations as measures of effect size. Correlations were considered weak (|0.10| < r < |0.29|), moderate (|0.30| < r < |0.49|), or strong (|0.50| < r < |1|). The association between the Brief PRHDS scores and categorical variables (i.e., gender, education, marital status, familiarity with cardiovascular diseases, hypertension, hypercholesterolemia, and diabetes) was evaluated by a series of independent sample t-tests. Assumption checks were performed before each t-test by evaluating skewness and kurtosis to check the normal distribution of the variables and Levene’s test to check the variances' homogeneity. Based on the assumption checks results, t-tests were performed using Welch's Test (unequal variances) or Student’s Test (equal variances).
All statistical tests were two-tailed, and a p ≤ 0.05 was considered statistically significant. Data analyses were performed using the IBM SPSS Statistics for Windows, version 26.0, and Jamovi, version 2.2.5.
3 Results
Participants were 772 native Italian adults ranging in age from 18 to 83 years (Mage = 40.7 years; SD = 13.7 years). They were equally distributed for gender, with 447 women (57.9%), and for education, with 429 participants (55.6%) who earned at least a bachelor’s degree. Most participants were workers (83.8%) and were married, civilly united, or in a stable relationship (62.2%). Regarding their health, their BMI ranged from 17 to 39 (MBMI = 23.93; SD = 3.90). About half of the participants had a family history of CVD (45%). The sample included subjects with low cardiovascular risk as only 12.6% had hypertension), 15.8% hypercholesterolemia, and 1% diabetes. The complete description of the participants concerning sociodemographic and health status characteristics is reported in Table 1.
3.1 Translation, Face and Content Validity of the PRHDS
The six panelists eliminated four items after the first round because they had a very similar meaning after translation into Italian (items 7 and 9 of the original scale had a similar meaning to item 1; items 15 and 16 had a similar meaning to item 11). Furthermore, the experts suggested rewriting the items that contained a negation (items 3, 10, 12, 14, 17, 19) to make them more understandable.
Once the requested changes had been made, the scale was sent to the experts. At the end of the second round, all I-CVI indices were above 0.70, except for items 14 and 19 (I-CVI = 0.66, see Table 2). After careful evaluation by the research team and the panelists, these items were removed from the Italian version of the scale due to their lack of representativeness with respect to the construct they were intended to measure in the Italian text. The final CVI for the overall scale was 0.97.
3.2 Descriptive Statistics and Preliminary Analyses
Table 3 illustrates descriptive statistics of the PRHDS items resulting from the content validity analysis. All items met the criteria to assume their normality (i.e., skewness < |2| and kurtosis < |7|).
The participants randomly assigned to EFA or CFA did not significantly differ in age [t(df = 770) = 0.13, p = 0.894], gender [χ2(1,772) = 2.57, p = 0.109], education [χ2(1,772) = 0.08, p = 0.772], working status [χ2(1,771) = 1.41, p = 0.235], and marital status [χ2(1,754) = 0.96, p = 0.328].
3.3 Factor Structure of the Brief PRHDS: Exploratory Factor Analysis
Data from the first sample were used in this analysis. The Bartlett’s sphericity test (χ2 = 1335.48, p < 0.001) and the KMO (equal to 0.80) ensured that the correlation matrix could be subjected to factor analysis. The analysis indicated that a single-factor solution was the most appropriate. After subsequent factor analyses were conducted stepwise, the initial pool of fourteen items was reduced to six (factor loadings of the initial 14 items are listed in the Appendix). Table 4 reports the pattern of factor loadings from the exploratory measurement model for the final six items. No item displays a loading lower than 0.32. The total variance explained by the factor extracted was 39.95%.
3.4 Factorial Validity of the Brief PRHDS: Confirmatory Factor Analysis
Confirmatory factor analysis was conducted separately on data from the second sample using the final six items of EFA. The model provided a not fully acceptable fit to the data [χ2(9, 386) = 89.26; p < 0.001; TLI = 0.795; CFI = 0.877, RMSEA = 0.152; SRMR = 0.060]. The magnitude of the modification index between items 4 and 5 was high, indicating additional covariance of item pair after controlling for cardiovascular risk perception. Therefore, a model with correlated residuals between items 4 and 5 was specified and tested against the first model. The resulting model provided a good fit to the data and fitted significantly better than a model without correlated residuals [χ2(8, 386) = 35.365; p < 0.001; TLI = 0.921; CFI = 0.958, RMSEA = 0.094; SRMR = 0.042]. All factor loadings were substantial. Table 4 presents the standardized factor loadings in the CFA sample.
3.5 Internal Consistency of the Brief PRHDS
The reliability analysis performed on the data collected from all 772 participants showed that the scale has adequate internal consistency. Cronbach’s alpha and McDonald’s omega were adequate: α = 0.788, ω = 0.796. Moreover, the inter-correlations coefficients of items were all larger than 0.39, indicating adequate internal consistency.
3.6 Associations Between the Brief PRHDS and Sociodemographic and Health Status Indicators
The Brief PRHDS score computed as average items' score met the criteria to assume their normality (i.e., skewness < |2| and kurtosis < |7|).
Regarding sociodemographic variables, the correlation between the Brief PRHDS and age was not significant (r = 0.066, p = 0.067). The group differences were not significant for gender [t(770) = 0.054, p = 0.957], education [t(770) = − 0.330, p = 0.741], and marital status [t(752) = 0.285, p = 0.776]. The group differences were significant for working status [t(769) = − 2.951, p = 0.003]. Working participants scored significantly higher on the Brief PRHDS (mean = 2.22, SD = 0.54) compared to not working participants (mean = 2.07, SD = 0.51), with a small effect size (Cohen’s d = − 0.29).
Regarding health status indicators, the correlation between the Brief PRHDS and BMI was positive but rather weak (r = 0.233, p < 0.001). The group differences were significant for family history of CDV [t(764) = − 4.798, p < 0.001]. Participants with family history of CDV scored significantly higher on the Brief PRHDS (mean = 2.30, SD = 0.52) than participants without family history of CDV (mean = 2.12, SD = 0.53), with a moderate effect size (Cohen’s d = − 0.35). The group differences were also significant for the presence of hypertension [Welch t(117) = − 3.888, p < 0.001]. Participants with hypertension scored significantly higher on the Brief PRHDS (mean = 2.42, SD = 0.60) than participants without hypertension (mean = 2.17, SD = 0.52), with a moderate effect size (Cohen’s d = − 0.45). The group differences were not significant for the presence of hypercholesterolemia [Welch t(159) = − 1.611, p = 0.109]. The group differences for the presence of diabetes were not calculated due to the low number of participants who reported having this risk factor (1.0%).
The correlation between the Brief PRHDS and the perceived health measure was negative and of moderate size (r = − 0.340, p < 0.001), indicating that higher cardiovascular risk perception scores were associated with lower scores on perceived health.
4 Discussion
In the present study, we translated the English version of the PRHDS into Italian and analyzed its preliminary psychometric properties by administering it to a sample of Italian adults. Overall, the results suggest that the brief PRHDS is a promising instrument for assessing cardiovascular risk perception among healthy Italian adults with a lower number of items compared to the original version of the scale. However, this scale deserves to be further evaluated in different cohorts, given the high variability of CV risk factor prevalence in different populations [26], and can represent a useful tool for Italian epidemiological studies evaluating the patient’s CVD risk perception.
An instrument that can assess the perception of the risk of heart disease is helpful for healthcare institutions to plan educational and awareness interventions on cardiovascular prevention, coherently with the evidence that people often underestimate their CV risk profile [5, 6, 27]. Nevertheless, adopting a tool developed for a different cultural and linguistic context can lead to misinterpretation [28]. Therefore, it is essential to check whether a tool is equivalent to the original in both semantic and cultural forms following appropriate methodology.
In our study, the content validation process showed some critical points concerning the adaptation of some items from English to Italian. In fact, during the CVI, the panel of experts pointed out that some items translated into Italian had a similar meaning. Therefore, such items were deleted by the authors, thus reducing the scale from 20 to 16 items. In addition, the panelists requested that the negative items be transformed into positive ones to have a better and unambiguous understanding of the scale. During this process two additional items were eliminated.
Exploratory and confirmative factor analyses revealed a good fit to a unidimensional model loading a reduced set of six items onto one latent factor. Cronbach's alpha and McDonald's omega were good and suggested that the Brief PRHDS has acceptable internal consistency.
The original scale consists of 20 items, measuring three dimensions: Dread Risk (7 items), Risk (6 items), and Unknown Risk (6 items) [10]. These three dimensions seem to be mainly an expression of how high or low the subjects' risk perception is. Therefore, in our opinion, the original items could be reduced to one dimension only, as found in the Italian version of the scale. Furthermore, the authors of the original scale were of the opinion that the dimensions of the scale had to be modified in order to be in line with the authors' choice of reference conceptual framework [29,30,31,32]. The original scale is based on the conceptual framework that adopts the psychometric paradigm of measuring perceived risk by asking people to make their own judgements or beliefs about the risk. In the psychometric paradigm, people make quantitative judgments about the riskiness of different hazards and the desired level of preventing them from occurring [32]. Interestingly, the six items of the Italian version describe the first dimension (dread risk) of the original scale. The PRHDS obtained after the validation process in Italian consists of six items. The brevity of the Italian version could be a point of strength in the administration of the scale. A high number of items to be administered through a questionnaire in a clinical setting is often unfeasible. Short questionnaires are more suitable than longer ones because they are less onerous and much quicker to complete. Prior research [33] showed that administering too-long tools could lead to a high non-response rate to questions. The latter can result in both difficulties in data analysis and a reduction in sample size. Nevertheless, such a relevant item reduction compared to the original scale can represent a limitation as shorter scale can have a limited accuracy in detecting risk perception compared to the original one.
The analysis of the association between the brief PRHDS and sociodemographic indicators showed that workers tend to have a higher risk perception compared to non-workers [2, 3]. This finding is of interest and, although potentially mediated by other confounders such as the socioeconomic status, of public health interest as non-workers, compared to workers employed by a company for instance, are not subject to regular and systematic CV screenings. In a cross-sectional study conducted in China among 692 subjects, individuals who were older, had a higher monthly income, and had diabetes were more prone to perceive higher CVD risk [3]. However in this study a different questionnaire was adopted for CVD risk perception (the Attitude and Beliefs about Cardiovascular Disease (ABCD) Risk Questionnaire) making it difficult to compare the findings with our results.
As expected, risk perception was significantly associated with BMI, family history for CVD and arterial hypertension. Interestingly, when examining the association between the brief PRHDS and health status indicators we found that the greater the CV risk perception, the lower the overall health perception suggesting an inverse correlation.
4.1 Limitations
We must acknowledge some limitations of the present study. Our data were primarily collected in a non-probabilistic sample of subjects living in one specific Italian region (Lombardy) in Italy. Thus, our results could be affected by this selection bias. Moreover, we did not collect test-retest data or evaluate convergent and discriminant validity. Future studies should investigate these specific reliability dimensions of the PRHDS. Nevertheless, our preliminary study offers encouraging results regarding the validity and reliability of a short and easy-to-administer version of the PRHDS in the Italian context but needs further confirmation.
5 Conclusion
In conclusion, our study suggests that the Italian version of the brief PRHDS is a promising self-report questionnaire to measure cardiovascular risk perception among Italian adults. These findings represent a starting point for overcoming some significant concerns of previous literature [5, 6] particularly the limited number of psychometrically sound questionnaires on cardiovascular risk perception. If further validated in other cohorts such tool can become a useful tool in both research and clinical settings to investigate the perceived CV risk and help tailoring CV screening programs.
Data Availability
The participants of this study did not give written consent for their data to be shared publicly, so due to the sensitive nature of the research supporting data is not available.
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V, GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group 1990–2019. J Am Coll Cardiol. 2020;76(25):2982–3021. https://doi.org/10.1016/j.jacc.2020.11.010.
Simione L, Gnagnarella C. Differences Between Health Workers and General Population in Risk Perception, Behaviors, and Psychological Distress Related to COVID-19 Spread in Italy. Front Psychol. 2020;11:2166. https://doi.org/10.3389/fpsyg.2020.02166.
Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, Tan KS, Wang DY, Yan Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7(1):11. https://doi.org/10.1186/s40779-020-00240-0.
Morrell J, Zeymer U, Baumgartner I, Limbourg T, Röther J, Bhatt DL, Bhatt DL, Steg PG. Differences in management and outcomes between male and female patients with atherothrombotic disease: results from the REACH Registry in Europe. Eur J Cardiovasc Prev Rehabil. 2011;18(2):270–7. https://doi.org/10.1097/HJR.0b013e32833cca34.
Conte M, Rozza F, Fucile I, D’Avino G, Sorvillo G, De Luca N, Mancusi C. Low awareness of cardiovascular risk factor among patients admitted in cardiac rehabilitation unit. High Blood Press Cardiovasc Prev. 2021;28(3):321–4. https://doi.org/10.1007/s40292-021-00444-y.
Maffei S, Meloni A, Deidda M, Sciomer S, Cugusi L, Cadeddu C, Gallina S, Franchini M, Scambia G, Mattioli AV, Surico N, Mercuro G, Igenda Study Group. Cardiovascular Risk Perception and Knowledge among Italian Women: lessons from IGENDA Protocol. J Clin Med. 2022;11(6):1695. https://doi.org/10.3390/jcm11061695.
Navar AM, Wang TY, Li S, Mi X, Li Z, Robinson JG, Virani SS, Peterson ED. Patient-perceived versus actual risk of cardiovascular disease and associated willingness to consider and use prevention therapy. Circ Cardiovasc Qual Outcomes. 2021;14(1): e006548. https://doi.org/10.1161/CIRCOUTCOMES.120.006548.
Wagner J, Lacey K, Chyun D, Abbott G. Development of a questionnaire to measure heart disease risk knowledge in people with diabetes: the Heart Disease Fact Questionnaire. Patient Educ Couns. 2005;58(1):82–7. https://doi.org/10.1016/j.pec.2004.07.004.
Woringer M, Nielsen JJ, Zibarras L, Evason J, Kassianos AP, Harris M, Majeed A, Soljak M. Development of a questionnaire to evaluate patients’ awareness of cardiovascular disease risk in England’s National Health Service Health Check preventive cardiovascular programme. BMJ Open. 2017;7(9): e014413. https://doi.org/10.1136/bmjopen-2016-014413.
Ammouri AA, Neuberger G. The perception of risk of heart disease scale: development and psychometric analysis. J Nurs Meas. 2008;16(2):83–97. https://doi.org/10.1891/1061-3749.16.2.83.
American Psycologist Association. Ethical principles of psychologists and Code of conduct. 1992.
Jones PS, Lee JW, Phillips LR, Zhang XE, Jaceldo KB. An Adaptation of Brislin’s Translation Model for Cross-cultural Research. Nurs Res. 2001;50(5):300–4. https://doi.org/10.1097/00006199-200109000-00008.
Polit DF, Beck CT. Essentials of nursing research: appraising evidence for nursing practice. 9th ed. Philadelphia: Wolters Kluwer Health; 2018. p. 442.
Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007;30(4):459–67. https://doi.org/10.1002/nur.20199.
Polit DF, Beck CT. The content validity index: are you sure you know what’s being reported? Critique and recommendations. Res Nurs Health ottobre. 2006;29(5):489–97. https://doi.org/10.1002/nur.20147.
Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;35(6):382–5.
Klem L. Structural equation modeling. In: Reading and understanding MORE multivariate statistics. Washington, DC, US: American Psychological Association; 2000. p. 227–60.
Worthington RL, Whittaker TA. Scale development research: a content analysis and recommendations for best practices. Couns Psychol. 2006;34(6):806–38. https://doi.org/10.1177/0011000006288127.
Nunnally JC. Psychometric theory, 2d edn. New York: McGraw-Hill; 1978. 701 p. (McGraw-Hill series in psychology).
Comrey AL, Lee HB. A first course in factor analysis. 2nd ed. New York: Psychology Press; 1992.
Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38(1):1–10. https://doi.org/10.1007/BF02291170.
Bentler PM. Fit Indexes, Lagrange multipliers, constraint changes and incomplete data in structural models. Multivar Behav Res. 1990;25(2):163–72. https://doi.org/10.1207/s15327906mbr2502_3.
Steiger JH. Notes on the Steiger-Lind (1980) Handout. Struct Equ Model Multidiscip J. 2016;23(6):777–81. https://doi.org/10.1080/10705511.2016.121748.
Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J gennaio. 1999;6(1):1–55. https://doi.org/10.1080/10705519909540118.
Nunnally JC, Bernstein IH. Psychometric theory. 3 edn, internat. stud. ed., [Nachdr.]. New Delhi: Tata McGraw Hill Education Private Ltd; 2010. 752 p. (McGraw-Hill series in psychology).
Bruno RM, Pucci G, Rosticci M, Guarino L, Guglielmo C, Agabiti Rosei C, Monticone S, Giavarini A, Lonati C, Torlasco C, Fedecostante M, Manzi MV, Pezzutto F, Di Pilla M, Artom N, Battistoni A, Pignatelli G, Sanga V, Pengo MF. Association Between Lifestyle and Systemic Arterial Hypertension in Young Adults: A National, Survey-Based, Cross-Sectional Study. High Blood Press Cardiovasc Prev. 2016;23(1):31–40. https://doi.org/10.1007/s40292-016-0135-6.
Gobbi P, Castoldi MG, Alagna RA, Brunoldi A, Pari C, Gallo A, Magri M, Marioni L, Muttillo G, Passoni C, La Torre A, Rosa D, Carnevale FA. Validity of the Italian Code of Ethics for everyday nursing practice. Nurs Ethics. 2018;25(7):906–17. https://doi.org/10.1177/0969733016677872.
Gjersing L, Caplehorn JR, Clausen T. Cross-cultural adaptation of research instruments: language, setting, time and statistical considerations. BMC Med Res Methodol. 2010;10(1):13. https://doi.org/10.1186/1471-2288-10-13.
Kendra MA, George VD. Defining Risk in Home Visiting. Public Health Nurs. 2001;18(2):128–37. https://doi.org/10.1046/j.1525-1446.2001.00128.x.
Lazarus RS, Folkman S. Stress, appraisal, and coping. 11. [print.]. New York: Springer; 20. 445 p.
Lupton D, curatore. Risk and Sociocultural Theory: New Directions and Perspectives [Internet]. 1a ed. Cambridge University Press; 1999 [citato 8 settembre 2023]. Disponibile su: https://www.cambridge.org/core/product/identifier/9780511520778/type/book
Slovic P. Perception of risk. Science. 1987;236(4799):280–5. https://doi.org/10.1126/science.3563507.
Sharma H. How short or long should be a questionnaire for any research? Researchers dilemma in deciding the appropriate questionnaire length. Saudi J Anaesth. 2022;16(1):65. https://doi.org/10.4103/sja.sja_163_21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with Ethical Standards
Written consent of each participant was obtained in compliance with the indications of the Declaration of Helsinki. The participants were informed about the purposes of the study and gave informed consent electronically. Privacy and anonymity were guaranteed to all participants. Participants could abandon completing the questionnaire without consequences.
Funding
Open access funding provided by Università degli Studi di Milano - Bicocca within the CRUI-CARE Agreement.
Conflict of interest
None.
Ethical approval
The Legal Department of the University of Milano-Bicocca states that participants must necessarily read the "data processing information" prepared based on the model provided by the University before completing a questionnaire and giving consent to participate. Therefore, a form on the “data processing information” and an informed consent form were prepared, administered, and made to sign by the participants before completing the online questionnaire. Since the data collection took place simply through an anonymous online questionnaire, with no possibility of identifying the respondents, no approval by the Ethics Committee was considered mandatory.
Appendix
Appendix
1.1 1. Pattern of Standardized Factor Loadings of the Initial 14 Items from AFE
Factor loading | |
|---|---|
Item 7 | 0.744 |
Item 5 | 0.674 |
Item 2 | 0.647 |
Item 4 | 0.645 |
Item 1 | 0.588 |
Item 6 | 0.461 |
Item 8 | − 0.365 |
Item 12 | − 0.257 |
Item 3 | 0.195 |
Item 10 | 0.174 |
Item 14 | 0.174 |
Item 13 | 0.095 |
Item 11 | 0.064 |
Item 9 | 0.052 |
1.2 2. Final Version of the Brief Italian Perception of Risk of Heart Disease Scale (PRHDS)
Fortemente in disaccordo (Strongly Disagree) | In disaccordo (Disagree) | D’accordo (Agree) | Fortemente d’accordo (Strongly Agree) | |
|---|---|---|---|---|
1. È possibile che io mi ammali di una malattia cardiaca | 1 | 2 | 3 | 4 |
2. C'è una buona possibilità che io abbia una malattia cardiaca nei prossimi 10 anni | 1 | 2 | 3 | 4 |
3. Ho un'alta probabilità di avere una malattia cardiaca a causa dei miei comportamenti passati | 1 | 2 | 3 | 4 |
4. Se mantengo il mio stile di vita avrò di sicuro una malattia cardiaca | 1 | 2 | 3 | 4 |
5. È difficile mantenere uno stile di vita sano | 1 | 2 | 3 | 4 |
6. Sono a rischio di avere una malattia cardiaca | 1 | 2 | 3 | 4 |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Rosa, D., Pengo, M.F., Adorni, R. et al. Psychometric Properties of a Brief Version of the Perception of Risk of Heart Disease Scale in an Italian Sample. High Blood Press Cardiovasc Prev 30, 475–484 (2023). https://doi.org/10.1007/s40292-023-00603-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-023-00603-3