Abstract
Introduction
Since sacubitril/valsartan (LCZ696) has neprilysin inhibition and angiotensin receptor-blocking properties, it is anticipated to have strong antihypertensive effects. However, there is not enough evidence to compare the safety and efficacy of sacubitril/valsartan to those of olmesartan in patients with hypertension.
Aim
To compare the efficacy and safety of sacubitril/valsartan versus olmesartan in patients with hypertension.
Methods
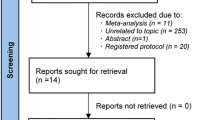
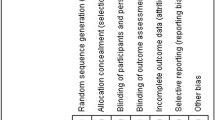
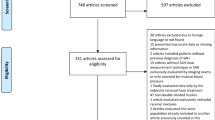
This study follows the guidelines of the Cochrane Handbook. We searched MEDLINE, Cochrane Central, Scopus, and Web of Science databases for relevant clinical trials. We extracted outcome endpoints regarding mean ambulatory systolic/diastolic blood pressure (maSBP/maDBP), mean sitting systolic/diastolic blood pressure (msSBP/msDBP), mean ambulatory/mean sitting pulse pressure (maPP/msPP), the proportion of patients achieving blood pressure control (< 140/90 mmHg), and adverse events. We used Review Manager Software for the conduction of the analysis of this study. The effect estimates of the studies were pooled as Mean difference or risk ratio and 95% confidence interval. We also conducted a subgroup analysis based on the dose of sacubitril/valsartan.
Results
A total of six clinical trials were included. The studies showed an overall low risk of bias. The pooled effect estimate revealed that sacubitril/valsartan significantly reduces maSBP, maDBP, maPP, msSBP, and msDBP measurements compared with olmesartan (p < 0.001). A significantly higher portion of patients achieved blood pressure control in the sacubitril/valsartan group (p < 0.001). The test of subgroup difference showed that 400 mg dose is significantly more effective than 200 mg dose in reducing maSBP. Regarding the safety profile, olmesartan was associated with more side effects due to drug discontinuation and more serious side effects.
Conclusion
Sacubitril/valsartan or LCZ696 is more effective and safer than olmesartan for controlling blood pressure in patients with hypertension.






Similar content being viewed by others
Change history
31 May 2023
A Correction to this paper has been published: https://doi.org/10.1007/s40292-023-00583-4
References
Lawes CMM, Vander Hoorn S, Law MR, Elliott P, MacMahon S, Rodgers A. Blood pressure and the global burden of disease 2000. Part 1: estimates of blood pressure levels. J Hypertens. 2006;24:413–22.
Mills KT, Bundy JD, Kelly TN, Reed J, Kearney PM, Reynolds K, et al. Abstract 16828: global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2015;132.
Cavalcante JL, Lima JAC, Redheuil A, Al-Mallah MH. Aortic stiffness. J Am Coll Cardiol. 2011;57:1511–22.
Bluemke DA, Kronmal RA, Lima JAC, Liu K, Olson J, Burke GL, et al. The relationship of left ventricular mass and geometry to incident cardiovascular events. J Am Coll Cardiol. 2008;52:2148–55.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension. Eur Heart J. 2013;34:2159–219.
Muiesan ML, Salvetti M, Monteduro C, Bonzi B, Paini A, Viola S, et al. Left ventricular concentric geometry during treatment adversely affects cardiovascular prognosis in hypertensive patients. Hypertension. 2004;43:731.
Sutton-Tyrrell K, Najjar SS, Boudreau RM, Venkitachalam L, Kupelian V, Simonsick EM, et al. Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation. 2005;111:3384–90.
Redheuil A, Wu CO, Kachenoura N, Ohyama Y, Yan RT, Bertoni AG, et al. Proximal aortic distensibility is an independent predictor of all-cause mortality and incident CV events: the MESA study. J Am Coll Cardiol. 2014;64:24.
Tsao CW, Gona PN, Salton CJ, Chuang ML, Levy D, Manning WJ, et al. Left ventricular structure and risk of cardiovascular events: a framingham heart study cardiac magnetic resonance study. J Am Heart Assoc. 2015;4:9.
Mitchell GF, Hwang S-J, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, et al. Arterial stiffness and cardiovascular events. Circulation. 2010;121:505–11.
Franklin SS, Wong ND. Hypertension and cardiovascular disease: contributions of the Framingham Heart Study. Glob Heart. 2013;8:59.
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, et al. Erratum: The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res. 2014;37:599–599.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Mori H, Ukai H, Yamamoto H, Saitou S, Hirao K, Yamuchi M, et al. Current status fo antihypertensive prescription and associated blood pressure control in Japan. Hypertens Res. 2006;29:143.
Habboush S, Sofy AA, Masoud AT, Cherfaoui O, Farhat AM, Abdelsattar AT, et al. Efficacy of single-pill, triple antihypertensive therapy in patients with uncontrolled hypertension: a systematic review and meta-analysis. High Blood Press Cardiovasc Prev [Internet]. 2022;29:245–52. https://doi.org/10.1007/s40292-022-00511-y.
Mostafa S, Shabana H, Khalil F, Mancy IM, Zedan HAM, Elmoursi A, et al. Evaluation of the safety and efficacy of dual therapy perindopril/amlodipine in the management of hypertension a systematic review and meta-analysis. High Blood Press Cardiovasc Prev [Internet]. 2022;29:565–76. https://doi.org/10.1007/s40292-022-00544-3.
Klingbeil AU, Schneider M, Martus P, Messerli FH, Schmieder RE. A meta-analysis of the effects of treatment on left ventricular mass in essential hypertension. Am J Med. 2003;115:41.
Sofy AA, Abdelsattar AT, Mohammed OM, Shareef MA, Alamodi AA, Nso N, et al. Amlodipine compared with benidipine in the management of hypertension: a systematic review and meta-analysis. High Blood Press Cardiovasc Prev. 2020;27:527.
Schiffrin EL. Circulatory therapeutics: Use of antihypertensive agents and their effects on the vasculature. J Cell Mol Med. 2010;14:1018–29.
Heeneman S, Sluimer JC, Daemen MJAP. Angiotensin-converting enzyme and vascular remodeling. Circ Res. 2007;101:441.
Ponikowski P, Voors AA, Anker DS, Bueno H, Cleland GFJ, Coats JSA, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Russ J Cardiol. 2017;7–81
Verdecchia P, Sleight P, Mancia G, Fagard R, Trimarco B, Schmieder RE, et al. Effects of telmisartan, ramipril, and their combination on left ventricular hypertrophy in individuals at high vascular risk in the ongoing telmisartan alone and in combination with ramipril global end point trial and the telmisartan randomized assessment. Circulation. 2009;120:1380–9.
Zannad F, Fay R. Blood pressure-lowering efficacy of olmesartan relative to other angiotensin II receptor antagonists: an overview of randomized controlled studies. Fundam Clin Pharmacol. 2007;21:181.
Nakajima T, Oh A, Saita S, Yoshida T, Ohishi M, Nishigaki N. Comparative effectiveness of angiotensin II receptor blockers in patients with hypertension in Japan—systematic review and network meta-analysis. Circ Rep. 2020;2:576.
Tsoi B, Akioyamen LE, Bonner A, Frankfurter C, Levine M, Pullenayegum E, et al. Comparative efficacy of angiotensin ii antagonists in essential hypertension: systematic review and network meta-analysis of randomised controlled trials. Hear Lung Circ. 2018;27:666.
Segura J, Ruilope LM. Dual-acting angiotensin receptor-neprilysin inhibition. Curr Hypertens Rep. 2011;13:74–8.
Cheung DG, Aizenberg D, Gorbunov V, Hafeez K, Chen C-W, Zhang J. Efficacy and safety of sacubitril/valsartan in patients with essential hypertension uncontrolled by olmesartan: a randomized, double-blind, 8-week study. J Clin Hypertens. 2018;20:150–8.
Supasyndh O, Wang J, Hafeez K, Zhang Y, Zhang J, Rakugi H. Efficacy and safety of sacubitril/valsartan (LCZ696) compared with olmesartan in elderly asian patients (≥65 years) with systolic hypertension. Am J Hypertens. 2017;30:1163–9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021.
Higgins JPT, S G. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated]. Cochrane Database Syst Rev. 2011.
De Vecchis R, Ariano C, Soreca S. Antihypertensive effect of sacubitril/valsartan: a meta-analysis. Minerva Cardioangiol. 2019;67:3.
Nixon RM, Müller E, Lowy A, Falvey H. Valsartan vs other angiotensin II receptor blockers in the treatment of hypertension: a meta-analytical approach. Int J Clin Pract. 2009;63:766–75.
Wang L, Zhao JW, Liu B, Shi D, Zou Z, Shi XY. Antihypertensive effects of olmesartan compared with other angiotensin receptor blockers: a meta-analysis. Am J Cardiovasc Drugs. 2012;12:335.
Cappuccio FP, Miller MA. Cardiovascular disease and hypertension in sub-Saharan Africa: burden, risk and interventions. Intern Emerg Med. 2016;11:299.
Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M. Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA. 2003;290:486.
Smith DHG, Dubiel R, Jones M. Use of 24-hour ambulatory blood pressure monitoring to assess antihypertensive efficacy. Am J Cardiovasc Drugs. 2005;5:41–50.
Baguet JP, Robitail S, Boyer L, Debensason D, Auquier P. A meta-analytical approach to the efficacy of antihypertensive drugs in reducing blood pressure. Am J Cardiovasc Drugs. 2005;5:131.
Gallo G, Tocci G, Fogacci F, Battistoni A, Rubattu S, Volpe M. Blockade of the neurohormonal systems in heart failure with preserved ejection fraction: a contemporary meta-analysis. Int J Cardiol. 2020;316:172.
Rakugi H, Kario K, Yamaguchi M, Sasajima T, Gotou H, Zhang J. Efficacy of sacubitril/valsartan versus olmesartan in Japanese patients with essential hypertension: a randomized, double-blind, multicenter study. Hypertens Res. 2022;45:824–33.
Supasyndh O, Sun N, Kario K, Hafeez K, Zhang J. Long-term (52-week) safety and efficacy of Sacubitril/valsartan in Asian patients with hypertension. Hypertens Res. 2017;40:472.
Kario K, Sun N, Chiang FT, Supasyndh O, Baek SH, Inubushi-Molessa A, et al. Efficacy and safety of LCZ696, a first-in-class angiotensin receptor neprilysin inhibitor, in asian patients with hypertension: a randomized, double-blind, placebo-controlled study. Hypertension. 2014;63:698.
Ruilope LM, Dukat A, Böhm M, Lacourcière Y, Gong J, Lefkowitz MP. Blood-pressure reduction with LCZ696, a novel dual-acting inhibitor of the angiotensin II receptor and neprilysin: a randomised, double-blind, placebo-controlled, active comparator study. Lancet. 2010;375:1255.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
The original article has been updated: Due to title change.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Almarjan, A.I., Almarjan, S.A. & Masoud, A.T. Different Doses of Sacubitril/Valsartan Compared with Olmesartan in Patients with Essential Hypertension: A Systematic Review and Meta-Analysis. High Blood Press Cardiovasc Prev 30, 207–218 (2023). https://doi.org/10.1007/s40292-023-00572-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-023-00572-7