Abstract
Arterial hypertension (AH) and periodontitis are among the most common non-communicable chronic diseases worldwide. Besides sharing common risk factors, an increasing body of evidence supports an independent association between the two conditions, with low-grade systemic inflammation acting as the plausible biological link with increased cardiovascular risk. In 2021, the Italian Society of Arterial Hypertension (SIIA) and the Italian Society of Periodontology and Implantology (SIdP) have joined forces and published a joint report on the relationships between AH and periodontitis, reviewing the existing scientific evidence and underlining the need to increase awareness of the strong connection between the two conditions and promote treatment strategies for the control of gums inflammation in patients with AH. The current document extends the previous joint report, providing clinical practical guidelines aimed to support clinicians in the management of patients who suffer from or are at risk of being affected by both conditions. These recommendations are based on careful consideration of the available evidence as well as of the current guidelines on the management of periodontitis and AH and are supported by SIIA and SIdP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Arterial hypertension (AH) and periodontitis are among the most common chronic diseases in the world, and they can significantly affect people’s health and well-being [1]. AH is the most relevant risk factor for cardiovascular diseases, which are still the main cause of death in the world and affects about 1 in 3 Italians, half of whom are unaware. Similarly, periodontitis, a chronic non-communicable disease of the supporting tissues of the teeth, affects up to 50% of the world’s population, with about 3 millions Italians suffering from severe forms and running an imminent risk of tooth loss [2].
In 2021, the Italian Society of Arterial Hypertension (SIIA) and the Italian Society of Periodontology and Implantology (SIdP) have joined forces and published a Joint report on the relationships between AH and periodontitis, reviewing the existing scientific evidence and underlining the need to promote strategies that aim to control gums inflammation in the management of patients suffering from AH [3].
The current document extends the previous joint report, providing clinical practical guidelines aimed to support clinicians in the management of patients affected or at risk of being affected by both conditions. These recommendations are based on careful consideration of the available evidence as well as of the current guidelines on the management of hypertension and periodontitis and are supported by SIIA and SIdP.
Practical Recommendations
-
1.
Measuring blood pressure and diagnosis of AH
-
2.
Diagnosis of gingivitis/periodontitis
-
3.
Assessing common risk factors
-
4.
Identifying patients with gingivitis/periodontitis at risk for AH
-
5.
Identifying patients with AH at risk of gingivitis/periodontitis
-
6.
Patient information to increase the level of awareness
-
7.
Identifying whom to refer patients at risk
-
8.
Step 1, 2 and 3 of periodontal therapy
-
9.
Follow-up and supportive care
-
10.
Integrated care pathways
-
11.
Recommendations for healthcare providers
-
12.
Essential bibliography
-
1.
Measuring blood pressure and diagnosis of AH
-
1.
A correct blood pressure (BP) measure is crucial to reach an accurate diagnosis of AH, define the severity of the condition, prescribe appropriate treatments, and plan the patient’s follow-up. The most widely used method to screen for AH is based on the measure of BP values in a health care setting (by a physician, a nurse, a pharmacist, or a dentist), referred to as Office Blood Pressure Monitoring (OBPM) [4]. A single BP recording is insufficient to reach a final diagnosis of AH, which instead should be made after repeated BP measurements [4]. These might be acquired:
-
(a)
in the same health care setting of the screening visit, if there is the experience in measuring BP or
-
(b)
through an ambulatory BP monitoring (ABPM), which records the BP values over 24 h (a minimum of 70% usable BP recordings are required for a valid ABPM measurement session) or
-
(c)
through home BP monitoring (HBPM), which represents the average of all BP readings performed with a semiautomatic, validated BP monitor, for at least 3 days (and preferably for 6–7 consecutive days) before each clinical visit.
When the HBPM is used to confirm the diagnosis of AH, patients should be instructed to acquire at least two BP measurements 1–2 min apart for each recording, and recordings should be performed in the morning and the evening [4]. The method used to confirm the diagnosis of AH should take into account the availability of ABPM devices, the individuals’ ability to acquire accurate BP values at home, the suspect of secondary forms of AH (i.e. obstructive sleep apnea syndrome) and the severity of BP elevation recorded during the first screening.
Independently of the method used to confirm the diagnosis of AH, all individuals with elevated BP values at a first screening should receive adequate training on the most appropriate method to measure BP at home.
-
1.1
BP measurements should be acquired in a quiet environment after 5 minutes of resting in a seated position.
-
1.2
Acquisitions should be carried out under conditions of mental and physical well-being, as measurements taken in the presence of symptoms (pain, anxiety, stress) are generally associated with increased BP values that do not represent the real BP control of the patient.
-
1.3
Measurements should be taken with a bladder cuff placed around the upper arm at the level of the heart. The cuff size should be appropriate for the size of the patient’s arm (obese individuals should use larger cuff sizes to avoid overestimation of BP values).
-
1.4
The acquisition of the first measurement should be followed by a second and third measurement, spaced at least 2–3 min apart.
-
1.5
A progressive decrease of BP in repeated measurements is often observed in individuals with a white coat effect or an alert reaction to BP measurement. In these cases, the patient’s final BP value should be considered as the average of at least 2 BP measurements taken consecutively and for which the difference in systolic BP should be <10 mm Hg.
-
1.6
At the first assessment, BP should be measured at both upper arms.
-
1.7
In older patients, a test for orthostatic hypotension should be performed at the first visit, including the measure of BP in supine position and after 1 and 3 minutes from the acquisition of the standing position. Repeated tests for orthostatic hypotension might be needed for older individuals, particularly when the BP-lowering treatment is modified.
-
1.8
A diagnosis of AH can be confirmed if:
-
Values of office BP in more than 1 visit are ≥ 140 and/or ≥ 90 mm Hg
-
Average values of HBPM are ≥ 135 and/or ≥ 85 mm Hg
-
The 24 h average BP values at the ABPM are ≥ 130 and/or ≥ 80 mm Hg, or the daytime (awake) mean BP values are ≥ 135 and/or ≥ 85 mm Hg, or night-time or asleep mean BP values are ≥ 120 and/or ≥ 70 mm Hg.
-
Take home messages
The diagnosis of AH is complex and should be made by healthcare professionals with experience in managing AH. |
A single BP measurement is not sufficient to reach a diagnosis of AH. |
HBPM and ABPM can be used to confirm the diagnosis of AH. |
Individuals with a suspected or confirmed diagnosis of AH should receive training on how to measure BP at home to ensure appropriate diagnosis, treatment and follow-up. |
-
2.
Diagnosis of gingivitis/periodontitis
The diagnosis of periodontal diseases is rather simple and accurate, even though it requires trained personnel and an equipped dental unit [5, 6]. Using the periodontal probe, the dentist may check the status of the periodontal tissue. Probing allows measuring the level of the clinical attachment (CAL), probing pocket depth (PD), soft tissue level (REC), and bleeding on probing (BOP). CAL is the distance between the tip of the probe inserted into the gingival sulcus and the cemento-enamel junction (CEJ). In physiologic conditions this distance is between 1 and 3 mm; greater measurements may be considered CAL loss and imply that the periodontal support has been compromised, even though a specific threshold to identify CAL loss has not been established. PD is the distance between the tip of the probe inserted into the gingival sulcus and the gingival margin. Sites with PD > 3 mm are defined as pockets, which in general present subgingival bacterial colonization and benefit from scaling, with CAL gain and PD reduction after treatment. REC is the distance between the CEJ and the gingival margin. BOP assessment consists of the recording of the presence of bleeding at a specific site after gentle probing with the periodontal probe. BOP is strictly correlated with the presence of inflammation in the periodontal tissues. Full-mouth assessment at 4- to 6-sites per tooth is required.
-
2.1
A patient with at least 10% of the sites with BOP is diagnosed with gingivitis. Gingivitis is then classified as localized (10% ≤ BOP ≤ 30%) or generalized (> 30%). This classification applies both to patients with intact periodontium and patients with a reduced periodontium (i.e. CAL loss).
-
2.2
The diagnosis of periodontitis is established if a patient presents with:
-
(a)
Interdental CAL loss at ≥2 non-adjacent teeth, or
-
(b)
Buccal or lingual CAL loss ≥3 mm with pocketing >3 mm detectable at ≥2 teeth.
-
(a)
-
2.3
It is important to exclude cases in which CAL loss is caused by other factors than periodontitis, such as traumatic REC, vertical root fractures, subgingival restorations or decay, impaction of third molars, or an endodontic lesion draining through the marginal periodontium.
-
2.4
The severity and the risk of progression of periodontitis are further classified according to stage and grade. Diagnostic process includes: a detailed medical and dental history and periodontal and intra-oral radiologic examinations.
-
2.5
Stage (I–IV) defines the severity of periodontitis and the complexity of treatment and depends on different parameters, including CAL, PD, radiologic bone loss, tooth loss, furcation involvement and impairment of masticatory function.
-
2.6
Grade (A to C) identifies the risk of progression of periodontitis and depends on previous evidence of progression and on local and systemic risk factors.
-
2.7
Extent is then classified as localized (< 30% of teeth involved), generalized, or molar/incisor pattern.
Take home messages
Dental professionals should check patients’ periodontal conditions during routine dental visits. |
Clinical and radiographic assessments are required to diagnose gingivitis and periodontitis. |
Staging and grading are useful tools to determine the severity of the disease and the complexity of treatment. |
-
3.
Assessing common risk factors
Evidence indicates that an independent association exists between periodontitis and AH, with common genetic denominators involving genes entailed in the immune function [7]. In parallel, these conditions share common unmodifiable and modifiable risk factors, such as older age, male sex, smoking habits, sedentary lifestyle, overweight/obesity, low socioeconomic status, and poor education, which concur, through intertwined mechanisms, to determine the clinical phenotype.
Therefore, when collecting medical history, attention should be paid to the burden represented by the exposure to such contributors, and the patient should be advised regarding the most updated approaches to the management of modifiable traits and how to persist over time in healthy lifestyle modifications. Even within the time constraints of clinical practice, very brief advice is encouraged, as recommended by cardiovascular prevention guidelines [8].
-
3.1
Patients with periodontitis and with AH should be screened for concomitant and shared modifiable cardiovascular risk factors.
-
3.2
Patients with periodontitis and with AH should be advised that they should actively manage all their cardiovascular risk factors for an effective reduction of their lifetime risk of related diseases.
-
3.3
Smoker individuals with AH and/or with periodontitis should be identified (“ASK”), advised on the best method of quitting (“ADVISE”), and offered help in their quitting attempts (“ACT”) at every visit.
-
3.4
Overweight and obese individuals with AH and/or with periodontitis should be informed of the BP benefit and the cardiovascular risk reduction associated with losing weight, and recommendations to adhere to healthy diet and engage in physical exercise should be given and reiterated over time.
-
3.5
According to guidelines, adults of all ages should be encouraged to stay active as their abilities and health condition allow, to increase their physical activity if sedentary, and, in the absence of specific limitations, to engage in at least 150-300 minutes of moderate-intensity exercise on a weekly basis, or in 75-150 minutes a week of vigorous-intensity aerobic exercise, or an equivalent combination thereof [8].
-
3.6
Individuals with AH and/or with periodontitis who also present with lipid and/or glucose metabolism disorders should be informed of the importance to control these concomitant risk factors to achieve a better control of their BP, improve periodontal outcomes, and reduce their lifetime cardiovascular risk.
Take home messages
Routine assessment and management of modifiable cardiovascular risk factors according to guidelines should be undertaken in individuals with periodontitis and in those with AH. |
-
4.
Identifying patient with gingivitis/periodontitis at risk for AH
An increased risk of incident AH exists in the presence of periodontal diseases [9]. Notably, observational evidence indicates an increased risk of uncontrolled AH in adults receiving antihypertensive treatment who also suffer from periodontitis [10]. In parallel, home and professional oral care are associated with improved BP profile [11,12,13].
For the multimodal connections between periodontal diseases and cardiovascular health status, in the light of the potential implications in terms of lifetime risk of cardiovascular diseases, early identification of individuals with gingivitis and periodontitis who are at risk of developing AH is desirable.
-
4.1
In patients with gingivitis/periodontitis, periodontal inflammation increases the risk of developing AH and might affect the achievement of adequate BP control during antihypertensive treatment.
-
4.2
Patients with gingivitis/periodontitis should regularly check their BP values.
-
4.3
In patients with gingivitis/periodontitis, family and personal history of risk factors and conditions that increase their risk for developing AH should be investigated:
-
4.3.1
Enquire on family history of AH, cardiovascular diseases, or renal disease, which, if present, poses an increased risk of developing AH;
-
4.3.2
Inform of the lifestyle factors that have a detrimental impact on cardiovascular health and increase the risk of AH, including sedentary habits, excessive body weight, high-salt diet, low vegetables consumption, smoking, alcohol use, recreational drug use, and poor sleep.
-
4.3.1
Take home messages
In individuals with gingivitis/periodontitis: |
– identify those with risk factors for developing AH |
– invite to regular BP checks also outside the health care setting. |
-
5.
Identifying patients with AH at risk of gingivitis/periodontitis
With the genetic component playing a role in the lifetime risk of periodontitis and AH, and in the light of the susceptibility of both conditions to common risk factors, it is important to identify individuals diagnosed with AH who might be at increased risk of periodontitis. Interestingly, a high-salt diet, which is a common environmental trigger for AH, was demonstrated to impair antibacterial response and to favor tissue inflammation [14, 15], both of which can have potential relevance for the risk and severity of periodontitis. Also, since the presence of gingival bleeding was found to increase the risk of high/uncontrolled BP, especially when occurring on top of an already established chronic periodontal disease [16], it is important that individuals with AH are made aware of the importance of a healthy periodontium.
-
5.1
Individuals with AH should be asked information on their family history of periodontal diseases.
-
5.2
Exposure to common risk factors should be investigated.
-
5.3
Individuals with AH and poor home oral hygiene practices (e.g. toothbrushing < 2times/day) should be identified.
-
5.4
Individuals with AH should be asked if they have experienced bleeding gums, teeth hypersensitivity, teeth mobility, halitosis or if they have lost teeth and for which reason.
-
5.5
Individuals with AH should be invited to visit the GengiveInforma App and take the test to assess their risk of having periodontitis.
-
5.6
Individuals with AH should be informed of the importance of regular dental visits to have their oral health needs assessed (i.e. every 6 months).
Take home messages
In individuals with AH: |
– ask about periodontal health status |
– investigate risk factors for the development of periodontal diseases |
– promote specific risk assessment and regular periodontal checks. |
-
6.
Patient information to increase the level of awareness
Despite the high prevalence of AH and periodontitis, with the former affecting over 1 billion people worldwide and the latter nearly 800 millions, the level of awareness, diagnosis and treatment remains unsatisfactory for both conditions. In Italy, recent data (2013) indicate that about 26% of adult patients followed by the family doctor had AH and about 61% had controlled BP levels [17]. Similarly, 50% of the Italian population suffers from some form of periodontal disease, with 3 out of 4 adults being affected by gingivitis. However, only 9% of the patients reports having been diagnosed with periodontitis. Therefore, it is essential to increase the level of awareness in the population and particularly on the link between these two diseases and on the positive effect that the treatment of periodontitis can have on BP.
-
6.1
Patients with gingivitis or those at risk or having periodontitis should be informed about the relationship between periodontitis and systemic diseases and more in general about the relationship between oral and systemic health.
-
6.2
Patients with or at risk of having AH should be specifically informed about the link between gingivitis/periodontitis and AH, and the SIdP-SIIA Recommendation decalogue should be provided.
-
6.3
This information should be delivered during first hypertensive/periodontal consultation and step 1 of periodontal therapy and should be reinforced at any reevaluation and any follow-up visit in the hypertension and dental clinic.
-
6.4
Patients should be encouraged to visit www.gengive.org for any further information and to use the app GengiveInforma to evaluate their own periodontal risk. In turn, patients with periodontitis should be encouraged to visit www.siia.it for any further information on AH, its screening, risk factors and complications.
Take home messages
Individuals with or at risk of AH should: |
– be informed about the correlation between AH and periodontal diseases |
– be encouraged to have a periodontal examination and a visit at an hypertension clinic. |
-
7.
Identifying whom to refer patients at risk
Once the patient at risk for periodontitis and AH has been identified, a multidisciplinary approach should be set up for the integrated management, prevention, and control of risk factors. This includes referring patients to the Specialist in the field, as summarized in the flowcharts (Figs. 1 and 2).
-
7.1
Individuals diagnosed with AH should undergo a questionnaire on their periodontal health status and risk factors (https://www.sidp.it/news/dettaglio-news/?id=129)
-
7.2
Individuals diagnosed with AH who are at moderate to high risk of periodontal diseases according to the questionnaire should be referred to the dental specialist (https://www.sidp.it/).
-
7.3
Individuals with periodontal diseases should be screened for their risk factors, including AH, and, in parallel to the appropriate periodontal treatment, should be referred to a center with expertise in the management of AH (https://siia.it/) for further assessment.
-
7.4
The recommendations at point 7.2 and 7.3 should be repeated in individuals with poor control of their cardiovascular risk factors and poor periodontal health status, respectively.
Take home messages
Patients at risk of periodontitis and AH should be referred to the specialists in the field (https://www.sidp.it/; https://siia.it/). |
-
8.
Step 1, 2 and 3 of periodontal therapy
Periodontitis can be treated in a simple and effective way, especially if the diagnosis is made early and in any case before the destruction of a large part of the attachment apparatus. The endpoint of treatment is to achieve no pockets ≥4 mm with BOP or no deep periodontal pockets (≥5 mm), as these conditions are associated with periodontitis progression over time.
According to the EFP Guidelines adopted in Italy by the SIdP, Periodontal Therapy is divided into 4 steps [18], each of which is fundamental to achieve oral health.
-
8.1
Step 1 focused on controlling risk factors and improving patient’s home oral hygiene and it includes:
-
8.1.1
patient’s instruction to correctly use the tools to remove the bacterial biofilm on a daily basis, such as toothbrush, interdental brush, dental floss, and mouthwash;
-
8.1.2
information on the nature and consequences of periodontitis both from an oral and general point of view, including systemic conditions such as AH, diabetes, and cardiovascular diseases;
-
8.1.3
the invitation to adopt healthy lifestyles (diet and exercise), to change incorrect habits (cigarette smoking), and to control concomitant diseases (Diabetes, AH, Cardiovascular Diseases, Rheumatoid Arthritis, etc);
-
8.1.4
the removal of the supragingival bacterial biofilm.
-
8.1.1
-
8.2
Step 2 aims to effectively remove the subgingival bacterial biofilm and any retentive factors such as calculus and /or inadequate restorations by means of professional procedures and instruments in a series of consecutive appointments.
-
8.3
Systemic antibiotics are not recommended on a routine basis but may be prescribed only in limited cases (severe cases and in young subjects). Their use must follow or be associated with mechanical removal of bacterial plaque during step 2.
-
8.4
Step 1 and 2 are performed by the dentist and the dental hygienist.
-
8.5
At the end of Step 1 and 2, a clinical re-evaluation of the patient is performed, and the clinical parameters recorded in the first visit are compared (PD, BOP, Plaque Index, Tooth Mobility etc.).
-
8.6
For Stage I–II periodontitis cases, step 1 and 2 may be adequate to restore oral health and achieve treatment goals.
-
8.7
In the more severe forms (Stage III-IV), Step 3, which includes non-surgical re-instrumentation of residual pockets and/or periodontal surgery, may be indicated. In order to handle Step 3 of treatment, a further periodontal training is necessary.
-
8.8
In stage IV, an interdisciplinary treatment involving different dental specialties may be necessary.
-
8.9
Once the disease and its possible sequelae are under control, it is essential to include the patient in a Supportive Periodontal Care (SPC) Program (step 4).
Take home messages
Treatment of periodontitis is recommended for individuals with or at risk of AH. |
The endpoint of treatment is to achieve no pockets ≥4 mm with BOP and no periodontal pockets ≥5 mm, and it is pursued through a step-by-step approach. |
-
9.
Follow-up and supportive care
Supportive Periodontal Care (SPC) system allows the monitoring of periodontal conditions over time [18]. At each appointment, the dentist and/or dental hygienist take care of the removal of bacterial plaque and calculus, verify the adequate execution of oral home care maneuvers and update the patient’s general health chart. Failure to adhere to this last phase is always associated with a high risk of disease recurrence, making treatments performed up to that moment ineffective. Furthermore, SPC is effective also in preventing the shift from gingivitis to periodontitis and in reducing the incidence of caries, thereby decreasing the risk of tooth loss.
-
9.1
Adult patients should be seen at least every 12 months for maintenance and periodontal and oral health assessment.
-
9.2
Adult patients with gingivitis or at risk of developing periodontitis should be seen at least every 6 months for maintenance and for periodontal and oral health assessment.
-
9.3
Periodontitis patients should be placed in a SPC program with a recall visit, every 3 to 6 months, according to their risk profile and disease severity.
-
9.4
Patients with risk factors for AH and periodontitis (smoking, diabetes, obesity, stress, unhealthy diet, inadequate physical activity) should be included in a SPC program with a frequency of recall visit based on a clinician decision.
Take home messages
Individuals with or at risk of periodontitis and AH should be included in a Supportive Periodontal Care (SPC) program tailored according to individual risk profile. |
-
10.
Integrated care pathways for the management of patients with or at risk for concomitant gingivitis/periodontitis and AH (Figs. 1 and 2 ).
Fig. 1
-
11.
Recommendations for healthcare providers.
-
(a)
Recommendations for Physicians managing Patients with AH
-
1.
AH and periodontitis are two very common chronic non-communicable diseases
-
2.
Periodontitis affects about 50% of the adult population, while gingivitis can reach up to 75%.
-
3.
There is evidence demonstrating the association of AH with periodontitis and gingivitis
-
4.
Failure to diagnose and treat periodontitis leads to loss of teeth and supporting tissues.
-
5.
Periodontitis is the main cause of tooth loss, with negative functional, aesthetic and psychological effects.
-
6.
AH and periodontitis share many risk factors: smoking, stress, obesity, diabetes, unhealthy diet, sedentary lifestyle.
-
7.
The presence of periodontal disease in a patient with AH should be suspected in the event of symptoms such as: spontaneous gums bleeding or bleeding on brushing, dental hypersensitivity, dental mobility, feeling of swollen gums (InForma Gums App)
-
8.
The check with the dentist/periodontist at least once a year is important to assess the oral health status and make early diagnosis of periodontal diseases.
-
9.
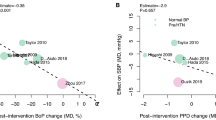
Professional oral hygiene and instrumentation of periodontal pockets show benefits on BP profile, particularly in terms of decrease in systolic BP.
-
10.
Proper home oral hygiene, with the use of toothbrush, brushes and thread, is an important element for the reduction of oral and systemic inflammation, with positive effects on the control of many systemic chronic diseases.
-
(b)
Recommendations for Dentists managing Patients with gingivitis/periodontitis
-
1.
AH and periodontitis are two very common chronic non-communicable diseases
-
2.
AH is defined when the BP values are ≥140/90 mmHg.
-
3.
AH affects about a third of the population in Italy and it is estimated that at least one in 10 hypertensive people are neither diagnosed nor aware.
-
4.
AH contributes to the development of cardiovascular diseases that are the leading cause of death in Italy.
-
5.
There is scientific evidence demonstrating the association of AH with periodontitis and gingivitis
-
6.
AH and periodontitis share many risk factors: smoking, stress, obesity, diabetes, unhealthy diet, sedentary lifestyle.
-
7.
Patients diagnosed with AH should be evaluated for the presence of periodontitis and gingivitis.
-
8.
BP assessment, according to guidelines, allows early detection of patients at risk of or with AH.
-
9.
Patients with BP values ≥140/90 mmHg and associated risk factors (smoking, diabetes, obesity, unhealthy diet, etc.) should be referred to their general practitioner or to a center with expertise in the management of AH (https://siia.it/)
-
10.
Besides improving oral health status, periodontal therapy can also help achieve a better control of systolic BP.
References
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;2021(398):957–80.
Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJL, Marcenes W. Global burden of severe periodontitis in 1990–2010: a systematic review and meta-regression. J Dent Res. 2014;93:1045–53.
Del Pinto R, Landi L, Grassi G, Sforza NM, Cairo F, Citterio F, et al. Hypertension and periodontitis: a joint report by the Italian Society of Hypertension (SIIA) and the Italian Society of Periodontology and Implantology (SIdP). High Blood Press Cardiovasc Prev. 2021;28:427–38.
Williams B, Mancia G, Spiering W, AgabitiRosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol. 2018;89(Suppl 1):S159–72.
Trombelli L, Farina R, Silva CO, Tatakis DN. Plaque-induced gingivitis: case definition and diagnostic considerations. J Periodontol. 2018;89(Suppl 1):S46–73.
Czesnikiewicz-Guzik M, Osmenda G, Siedlinski M, Nosalski R, Pelka P, Nowakowski D, et al. Causal association between periodontitis and hypertension: evidence from Mendelian randomization and a randomized controlled trial of non-surgical periodontal therapy. Eur Heart J. 2019;40:3459–70.
Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42:3227–337.
Carra MC, Fessi S, Detzen L, Darnaud C, Julia C, Hercberg S, et al. Self-reported periodontal health and incident hypertension: longitudinal evidence from the NutriNet-Santé e-cohort. J Hypertens. 2021;39:2422–30.
Pietropaoli D, Del Pinto R, Ferri C, Wright JT Jr, Giannoni M, Ortu E, et al. Poor oral health and blood pressure control among US hypertensive adults. Hypertension. 2018;72:1365–73.
Sharma S, Sridhar S, McIntosh A, Messow C-M, Aguilera EM, Del-Pinto R, et al. Periodontal therapy and treatment of hypertension-alternative to the pharmacological approach. A systematic review and meta-analysis. Pharmacol Res. 2021;166:105511.
Hwang S-Y, Oh H, Rhee M-Y, Kang S, Kim H-Y. Association of periodontitis, missing teeth, and oral hygiene behaviors with the incidence of hypertension in middle-aged and older adults in Korea: a 10-year follow-up study. J Periodontol. 2022;93:1283–93.
Del Pinto R, Pietropaoli D, Grassi G, Muiesan ML, Monaco A, Cossolo M, et al. Home oral hygiene is associated with blood pressure profiles: results of a nationwide survey in Italian pharmacies. J Clin Periodontol. 2022. https://doi.org/10.1111/jcpe.13720.
Wu C, Yosef N, Thalhamer T, Zhu C, Xiao S, Kishi Y, et al. Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature. 2013;496:513–7.
Jobin K, Stumpf NE, Schwab S, Eichler M, Neubert P, Rauh M, et al. A high-salt diet compromises antibacterial neutrophil responses through hormonal perturbation. Sci Transl Med. 2020;2020:12. https://doi.org/10.1126/scitranslmed.aay3850.
Pietropaoli D, Del Pinto R, Ferri C, Marzo G, Giannoni M, Ortu E, et al. Association between periodontal inflammation and hypertension using periodontal inflamed surface area and bleeding on probing. J Clin Periodontol. 2020;47:160–72.
Tocci G, Nati G, Cricelli C, Parretti D, Lapi F, Ferrucci A, et al. Prevalence and control of hypertension in the general practice in Italy: updated analysis of a large database. J Hum Hypertens. 2017;31:258–62.
Sanz M, Herrera D, Kebschull M, Chapple I, Jepsen S, Beglundh T, et al. Treatment of stage I-III periodontitis—the EFP S3 level clinical practice guideline. J Clin Periodontol. 2020;47(Suppl 22):4–60.
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Conflict of interest
The Authors declare no conflicts of interest.
Ethics approval
As a summary of existing evidence, ethical approval was not required.
Funding
No specific fundings were used for this work.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Pietropaoli, D., Cairo, F., Citterio, F. et al. Practical Guidelines for Patients with Hypertension and Periodontitis. High Blood Press Cardiovasc Prev 30, 7–16 (2023). https://doi.org/10.1007/s40292-022-00553-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-022-00553-2