Abstract
Background
Considering the finite time within a 24-h day, the distribution of time spent on movement behaviours has been found to be associated with health outcomes.
Objectives
This systematic review and meta-analysis aimed to summarise and evaluate the overflow effects of interventions targeting a single behaviour (physical activity, sedentary behaviour/screen time, or sleep) on other non-targeted behaviours among children and adolescents.
Methods
Six databases (MEDLINE [Ovid], PsycINFO [ProQuest], EMBASE [Ovid], PubMed, Web of Science and SPORTDiscus [EBSCO]) were searched for relevant studies published before 13 May, 2024. Randomised controlled trials and clustered randomised controlled trials that targeted a single behaviour and also assessed the effects on non-targeted behaviours, comprised of healthy children under the age of 18 years, were included. Movement behaviours can be measured either objectively or subjectively. The revised Cochrane risk-of-bias tool for randomised trials was adopted to evaluate the risk of bias.
Results
A total of 102 studies with 45,998 participants from 21 countries were identified, and 60 of them with 26,183 participants were incorporated into the meta-analysis. The meta-analysis demonstrated that physical activity interventions led to a reduction in the proportion of each day spent in sedentary behaviour (mean difference = − 0.95% of wear time, 95% confidence interval − 1.44, − 0.45, I2 = 39%). Sedentary behaviour interventions resulted in increased standing time (mean difference = 3.87%, 95% confidence interval 1.99, 5.75, I2 = 0%). Interventions targeting screen time did not yield changes in physical activity or sleep. The findings on the effectiveness of sleep interventions on non-targeted behaviours and of physical activity interventions on sleep were inconclusive.
Conclusions
Overall, the findings suggested that interventions aimed at increasing physical activity or reducing sedentary behaviour had overflow effects on non-targeted behaviours, but the effect sizes were small. Additional evidence is needed to reach definitive conclusions regarding the impact of behaviour change interventions on sleep and of the overflow effects of sleep interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This systematic review represents the first attempt to synthesise evidence on the overflow effects of single movement behaviour interventions on non-targeted behaviours among children and adolescents. |
An overflow effect on non-targeted behaviours was found in interventions targeting physical activity and sedentary behaviour. |
Because of the risk of bias present in the included studies, cautious interpretation of the findings is needed. |
1 Introduction
The development of healthy movement behaviours (such as physical activity, sedentary behaviour, screen time, sleep) during childhood and adolescence has a strong association with a diverse array of health indicators [1,2,3]. Specifically, physical activity and sleep are positively associated with both physical (e.g. bone health, body weight status) and mental health among children and adolescents [4,5,6], and prolonged sedentary behaviour and screen time are associated with a higher risk of being overweight/obese and worse mental health among children and adolescents [7, 8]. Despite the importance of adopting healthy movement behaviours, previous systematic reviews have shown that children and adolescents worldwide engage in unhealthy lifestyles, characterised by low physical activity, high sedentary behaviour and/or screen time, and insufficient sleep [1, 3].
Given that the time in a 24-h day is finite and fixed, these component behaviours are co-dependent. The 24-h movement guidelines, which provide recommendations for the integration of physical activity, sedentary behaviour, and sleep within a 24-h period, have been proposed to recognise the interrelationships among these behaviours [9, 10]. The 24-Hour Activity Cycle, a holistic approach that treats all behaviours engaged in within a day as integrated, aligns with this framework [11]. Embedding the 24-Hour Activity Cycle in health promotion, previous studies using isotemporal substitution analyses have illustrated the relationships between time substitution and health outcomes. For instance, a meta-analysis covering 17,390 adults found that reallocating 30 min of sedentary behaviour to any intensity of physical activity was associated with lower levels of waist circumference, fasting insulin and the risk of all-cause mortality [12]. A systematic review of studies of children and adolescents revealed that substituting sedentary behaviour with moderate-to-vigorous intensity physical activity (MVPA) was associated with a lower risk of adiposity [13]. Furthermore, isotemporal substitution of physical activity, sedentary behaviour and sleep in a 24-h day has been found to be associated with improved physical fitness [14], motor skills [15], inflammatory markers [16], cognitive function [17] and mental health [18] in cross-sectional and longitudinal studies of children and adolescents.
Interventions targeting the improvement of all three behaviours across a 24-h day are still in their infancy, and most interventions are designed to change a single behaviour. The only intervention study that aimed to change adolescents’ physical activity, sedentary behaviour and sleep simultaneously adopted a quasi-experimental design in a school setting [19]. It was found that the intervention group had higher physical activity (both light-intensity physical activity and MVPA), lower sedentary behaviour and longer sleep duration after 1 academic year than the control group [19]. However, interventions designed to target a single behaviour have also been found to impact non-targeted behaviours. This phenomenon has been described as the overflow effect [20]. For instance, a systematic review summarising behavioural interventions for children under 5 years of age reported that a physical activity intervention had an overflow effect of decreasing sedentary behaviour [21]. Interventions aimed at reducing sedentary behaviour have reported improvement in physical activity (e.g. frequency of exercise and participation in sports, MVPA, steps per day) and sleep [22,23,24]. Regarding sleep, which constitutes a considerable portion of the 24-h cycle, the evidence for an overflow effect of sleep interventions is sparse and mixed. For example, an intervention targeting sleep routines among young children found an increased MVPA of 11 min per day in the intervention group compared with the control group, although the difference was not significant [25]; another family-based sleep intervention among infants and toddlers found no significant effect on light-to-vigorous physical activity [26]. Another intervention reported that adolescents spent less time in sedentary behaviour when they were instructed to increase sleep duration [27]. Given these mixed findings, it is imperative to conduct a review covering a wide age range (< 18 years) to systematically summarise the evidence of overflow effects in behavioural interventions. This review offers crucial evidence to better understand how behaviours interact in a 24-h day, which in turn can inform future interventions.
This systematic review examined the overflow effects of interventions targeting a single movement behaviour on other non-targeted movement behaviours in children and adolescents aged under 18 years. The secondary purpose was to investigate whether the overflow effects vary across different characteristics of the intervention (e.g. age group, setting, duration of intervention).
2 Methods
2.1 Protocol and Registration
The protocol of this review was registered in the International Prospective Register of Systematic Reviews (PROSPERO; CRD42022315153). This report follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [28].
2.2 Information Sources and Search Strategy
A systematic search was conducted on 7 March, 2022 and updated on 13 May, 2024, using the databases MEDLINE (Ovid), PsycINFO (ProQuest), EMBASE (Ovid), PubMed, Web of Science and SPORTDiscus (EBSCO). Details of the search strategy are available in Table S1 of the Electronic Supplementary Material (ESM).
2.3 Eligibility Criteria
The search had no limitations on publication date, but was limited to studies published in English in peer-reviewed journals. Only randomised controlled trials and clustered randomised controlled trials were included. Studies that included apparently healthy children aged under 18 years were eligible. Studies that targeted a single movement behaviour (physical activity of any intensity, sedentary behaviour, screen time or sleep) but also assessed the effects of the intervention on non-targeted behaviours were included in the review, for example studies that targeted physical activity but assessed the effects of the intervention on sedentary behaviour, screen time and/or sleep. Physical activity, sedentary behaviour and sleep can be evaluated using either device-based measures (e.g. accelerometers, pedometers) or subjective measures (e.g. questionnaires, interviews, diaries); screen time can be assessed through subjective measures such as questionnaires, interviews or diaries. Studies had to include a control group that did not receive any intervention or received an intervention that was not related to the content of the intervention group. For inclusion in the review, studies had to measure the outcomes of at least one non-targeted movement behaviour (physical activity, sedentary behaviour, screen time or sleep) at both baseline and post-intervention. Studies were excluded if they were (1) non-randomised controlled experimental studies; (2) qualitative studies; (3) case studies and case series; (4) grey literature; (5) comments/editorials; (6) reviews; or (7) studies targeting population with clinical diagnoses (with the exception of obesity/overweight).
2.4 Study Selection and Data Extraction
After removing duplicates, two independent reviewers (JF, CZ) screened the titles and abstracts in the initial sample, followed by full-text screening of papers identified in the previous step. Any discrepancies were resolved by discussion or by consulting a third independent reviewer (WH). Data extraction (e.g. author, publication year, country, study design, population, setting, targeted behaviour, non-targeted behaviour, measurement of non-targeted behaviour, main findings, intervention duration) was conducted by two reviewers (JF, MN) and checked by a third reviewer (CZ). The targeted behaviour was determined by the purpose claimed by the authors and strategies of the intervention. The corresponding authors of potentially relevant studies were contacted to provide supplementary data. For example, for interventions targeting physical activity that used accelerometers, sedentary behaviour data expressed as minutes per day were requested, as it was expected that such data were collected; 52 e-mails were sent requesting such information, and 20 replies were received.
2.5 Risk of Bias and Publication Bias
The revised Cochrane risk-of-bias tool for randomised trials (RoB 2) was used to assess the risk of bias in the included studies [29]. The assessment was conducted by JF and checked by JJ. This tool evaluated five domains, namely randomisation, deviations from intended interventions, missing outcome data, measurement and selection of reported results [29]. Discrepancies, if any, were resolved through consensus discussions or involvement of a third reviewer (WH) when necessary. Moreover, publication bias was visualised using funnel plots for meta-analyses that included a minimum of ten studies.
2.6 Data Synthesis
Meta-analyses were performed for the post-intervention outcomes for non-targeted behaviours, using Review Manager version 5.4 [30]. Mean values and standard deviations were determined to estimate the effect of the intervention, and standard errors and 95% confidence intervals (CIs) were converted to standard deviations [31]. The pooled effect sizes were presented as the mean difference (MD; intervention group vs control group) with 95% CI. Random-effect models were performed, and a series of sensitivity analyses were conducted by removing studies one by one. Sub-group analyses were conducted based on various factors, including age groups (preschoolers, school-aged children, adolescents), settings, duration of intervention, effectiveness on the target behaviour (based on the statistical analysis results), whether the design of the intervention was based on a theoretical framework, wear time of accelerometers and risk of bias. Subgroup analyses were conducted if there were at least two studies examining the overflow effect on the same non-targeted behaviour within the subgroup. Heterogeneity was presented as I-square (I2) values and was categorised as low (< 25%), moderate (26–50%) or high (> 50%) [32].
3 Results
3.1 Study Selection
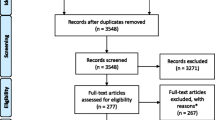
After removing duplicates, 12,704 studies were included in the sample for title and abstract screening. Among these, 393 studies underwent full-text screening, 102 studies were included in the final sample, and 60 of them were included for the meta-analysis. A flow diagram of the selection process is presented in Fig. 1.
3.2 Descriptive Characteristics of Included Studies
Table S2 of the ESM provides an overview of the studies in the final sample. A total of 102 studies covering 45,998 participants were included in this study. The average age of the participants in the studies ranged from 3 months to 17.9 years, representing a diverse group from 21 countries. Among the 87 physical activity (i.e. physical activity as the targeted behaviour) interventions, 68 measured sedentary behaviour, 16 measured screen time and seven measured sleep duration as non-targeted behaviours. All of the sedentary behaviour interventions (sedentary behaviour as the targeted behaviour; n = 6) measured physical activity as one of the outcomes, and eight interventions targeting screen time measured physical activity; three of the latter also measured sleep. Two sleep (targeted behaviour) interventions measured physical activity, one of which also reported sedentary behaviour.
3.3 Overflow Effects of Physical Activity Interventions on Sedentary Behaviour/Screen Time and Sleep
The results of the 68 physical activity interventions that also measured the effects on sedentary behaviour [33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100] are summarised in Table S2 of the ESM. Nineteen studies reported significantly lower sedentary behaviour in the intervention groups than in the control groups at post-intervention [73,74,75,76,77, 79,80,81,82,83,84,85,86,87,88, 90, 91, 95, 96]; no significant difference was found between the intervention and control group in 46 studies [33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72, 78, 89, 97,98,99,100]. The remaining three studies solely reported within-group differences and did not examine the differences between groups [92,93,94].
Thirty-seven studies examined the effect of physical activity interventions on sedentary behaviour measured as a percentage of wear time (Fig. 2) [33,34,35, 37, 41, 42, 45, 48, 49, 51, 52, 54, 56,57,58, 61, 65,66,67, 71,72,73,74,75,76,77,78,79,80, 83, 84, 86, 88, 89, 92, 97, 98]. All studies except one [88] used device-based measurement. The intervention groups reported less sedentary behaviour than the control groups (MD = − 0.95%, 95% CI − 1.44, − 0.45, I2 = 39%). Subgroup analyses (Table 1) were performed based on participants’ age, setting, intervention duration, the effectiveness of the intervention on the target behaviour (physical activity), whether the study was theory based, wear time of accelerometers and level of risk of bias. The results indicated that physical activity interventions were effective in reducing sedentary behaviour among school-aged children and adolescents (school-aged children: MD = − 0.88%, 95% CI − 1.53, − 0.24, I2 = 52%; adolescents: MD = − 1.64%, 95% CI − 2.61, − 0.68, I2 = 0%), but were not effective among preschoolers (MD = − 0.82%, 95% CI = − 1.90, 0.26, I2 = 0%). Interventions conducted in schools and childcare centres observed significantly reduced sedentary behaviour (MD = − 1.03%, 95% CI − 1.58, − 0.47, I2 = 44%). The pooled results indicated that the physical activity interventions led to a decrease in sedentary behaviour regardless of their effectiveness in improving the target behaviour. However, a larger effect was observed when the interventions effectively changed the target behaviour than those did not (effective: MD = − 2.05%, 95% CI − 3.10, − 1.01, I2 = 49%; not effective: MD = − 0.43%, 95% CI − 0.75, − 0.10, I2 = 0%). Regarding the use of a theoretical framework (theory based, no theory), intervention duration (less than 12 weeks, at least 12 weeks), wear time of accelerometers (whole day, segmented time) and the risk of bias (some concerns, high risk), significant decreases in sedentary behaviour were observed in all subgroups.
Among the 68 physical activity interventions that also measured the effects on sedentary behaviour, 11 examined the pooled results of physical activity interventions on sedentary behaviour measured as minutes per day, and their meta-analyses results are presented in Fig. 3a [40, 43, 44, 47, 50, 59, 62, 63, 82, 90, 95]. There was no significant difference between the intervention and control groups (MD = − 5.26 min, 95% CI − 10.61, 0.09, I2 = 45%), for both school-aged children (MD = − 5.35 min, 95% CI − 12.19, 1.48, I2 = 58%) and adolescents (MD = − 5.08 min, 95% CI = − 16.23, 6.08, I2 = 34%). A sub-group analysis indicated that physical activity interventions were effective in reducing sedentary behaviour when measured subjectively (MD = − 11.09 min, 95% CI − 19.05, − 3.13, I2 = 0%), but were not effective when adopting device-based measurement (MD = − 3.84 min, 95% CI − 10.20, 2.53, I2 = 56%). Of the 16 studies that examined the effect of physical activity intervention on screen time [48, 101,102,103,104,105,106,107,108,109,110,111,112,113,114,115], nine reported decreased screen time in the intervention group [101, 106,107,108,109,110,111,112,113] compared with the control group, and seven did not find significant differences [48, 102,103,104,105, 114, 115]. Six studies met the meta-analysis criteria, and all of them utilised subjective measurement to assess screen time [48, 103, 105, 107, 111, 114] (Fig. 3b). No significant differences in screen time were found between the intervention and control groups in the meta-analysis (MD = − 6.46 min, 95% CI = − 16.38, 3.46, I2 = 0%).
Seven studies examined the effect of physical activity interventions on sleep duration [46, 49, 103, 116,117,118]; six of them did not find significant differences in sleep duration between the intervention and control groups [46, 49, 103, 116, 118, 119], while one reported significantly longer sleep duration in the intervention group than in the control group [117]. As shown in Fig. 3c, the meta-analysis showed no significant difference between the intervention and control groups (MD = 0.78 min, 95% CI − 11.95, 13.51, I2 = 0%), based on three studies that used both device-based [49, 119] and subjective measures [103].
3.4 Overflow Effects of Sedentary Behaviour Interventions on Physical Activity and Sleep
Of the six studies examining the effect of sedentary behaviour interventions on physical activity [94, 120,121,122,123,124], three reported favourable changes in physical activity in the intervention group [120, 121, 124] relative to the control group; two did not observe any significant differences [122, 123] and one did not examine between-group differences [94]. Based on three included studies that implemented standing desks as a primary intervention strategy and used accelerometers to measure physical activity [120, 122, 124], a meta-analysis of the effect of sedentary behaviour interventions on standing (percent of wear time) reported positive changes (MD = 3.87%, 95% CI 1.99, 5.75, I2 = 0%) [Fig. 4a]. The same three studies also investigated the effect of sedentary behaviour interventions on stepping [120, 122, 124], but no significant effect was found (Fig. 4b).
Pooled analysis on the effect of a sedentary behaviour intervention on standing (% of wear time), b sedentary behaviour intervention on stepping (% of wear time) and c screen time intervention on moderate-to-vigorous intensity physical activity (min/day). CI confidence interval, IV inverse variance, SD standard deviation
3.5 Overflow Effect of Screen Time Interventions on Physical Activity and Sleep
Of the eight studies investigating the effect of screen time interventions on physical activity [22,23,24, 87, 125,126,127,128], six found no difference at post-intervention [22, 23, 87, 125,126,127], and the remaining two reported increased physical activity in the intervention group compared with the control group [24, 128]. Based on both device-based [23, 128] and subjective measures [127], three studies on the effect of screen time interventions on MVPA (min/day) revealed no significant changes (Fig. 4c). Regarding the effects of screen time interventions on sleep, no significant changes were reported in any of the three studies [22, 127, 128].
3.6 Overflow Effect of Sleep Interventions on Physical Activity and Sedentary Behaviour
Two studies examining the overflow effects of sleep interventions did not find significant changes in physical activity or sedentary behaviour [25, 26]. Both studies were conducted in family-based settings and targeted children below the age of 5 years (i.e. infants, toddlers and preschoolers) [25, 26]. In these studies, parents received educational interventions, and physical activity and sedentary behaviour were measured using accelerometers [25, 26].
3.7 Risk of Bias
Overall, 62 studies were determined to raise some concerns of risk bias, 36 studies were determined to have a high risk of bias, and four studies demonstrated a low risk of bias (Fig. S1 of the ESM) [39, 94, 106, 125]. The main factors contributing to high risk bias were deviations from the intended interventions (e.g. absence of blinding for participants and intervention deliverers, inappropriate analytical methods that failed to address missing data from excluded participants) and measurement of the outcomes (e.g. use of invalid or unreliable measurement tools).
3.8 Sensitivity Analyses and Publication Bias
A series of sensitivity analyses were performed by removing each study one by one from the meta-analysis. The results showed that the pooled effect of physical activity interventions on sedentary behaviour (in minutes per day) in the intervention group became significant, compared with the control group, when either of the two studies was excluded [63, 82]. The findings of the subgroup analyses of the effect of physical activity interventions on sedentary behaviour (percent of wear time) were less robust. Specifically, when one study was removed [45], the previously observed effect was no longer significant in the analysis of the ‘school-aged children’ subsample in the child age subgroup or in the ‘theory-based intervention’ subsample in the theory-based subgroup. Regarding the duration of the interventions, excluding any of the five studies [41, 48, 67, 86, 97] led to non-significant differences between the intervention and control groups in the subsample of interventions that lasted for less than 12 weeks. After removing one study [37], the statistical significance of the overflow effect of physical activity interventions on sedentary behaviour was no longer observed in the ‘ineffective’ interventions subsample. In the sensitivity analyses of the risk of bias findings, removing any of the three studies [41, 48, 61] categorised as ‘high risk of bias’ led to the observed statistical significance of the effect becoming non-significant. Regarding the subgroup analysis examining the effect of physical activity intervention on sedentary behaviour (min/day), based on the measurement, the previously observed effect was no longer significant in the analysis of the ‘subjective measurement’ subsample when one study was removed [95]. The funnel plots did not show any indication of publication bias (Figs. S2 and S3 of the ESM).
4 Discussion
This is the first attempt to synthesise evidence on the overflow effects of single movement behaviour interventions on non-targeted behaviours among children aged under 18 years. The findings indicate that physical activity interventions entailed concomitant, albeit small, reductions in sedentary behaviour, as measured by the percentage of wear time using devices, but they had no significant effect on screen time. The impacts may vary across age groups, settings and the effectiveness of the intervention on the target behaviour. Interventions aimed at reducing sedentary behaviour led to increases in standing time but not in stepping time. Interventions designed to reduce screen time did not yield concomitant changes in physical activity or sleep. Findings on the overflow effects of sleep interventions on non-targeted behaviours and of physical activity interventions on sleep outcomes were inconclusive.
Although sedentary behaviour was not targeted in the physical activity interventions in this review, a small decrease in sedentary behaviour was observed, indicating an approximate reduction of 6 min (0.95% of wear time, assuming the accelerometers were worn for 10 h a day). This finding of a decrease in sedentary behaviour is consistent with findings from a previous review [21]. However, that review reported a larger effect size, i.e. a decrease of 32 min in sedentary behaviour, in interventions targeting physical activity in the early years in a sub-group analysis of three studies [21]. This discrepancy in effect size may be attributable to the different inclusion criteria used in the two reviews. Specifically, all three studies included in the latter review compared a specific type of physical activity intervention (i.e. structured lessons, participatory intervention) with control groups that received other physical activity interventions (i.e. free playtime, gym class) [129,130,131]. However, those studies did not meet the inclusion criteria of this review, specifically that the control group should not receive any intervention.
Our subgroup meta-analyses revealed some trends in studies reporting the effect of physical activity interventions on sedentary behaviour (% of wear time) by age group, setting and the effectiveness of the intervention in changing the target behaviour. The finding that school-aged children and adolescents benefited more from physical activity interventions than preschoolers was consistent with a previous systematic review, which found that older children were more likely to benefit from physical activity in the form of decreasing screen time [132]. The age-related increase in sedentary behaviour among children may explain these differences, as there is more room for improvement among older children [133]. Regarding setting, interventions conducted in schools and childcare centres were more effective in decreasing sedentary behaviour than those conducted in family and community settings. Previous systematic reviews have also observed the favourable effectiveness of school-based interventions on physical activity levels [134], physical activity enjoyment [135] and both physical and mental health [136,137,138]. Unsurprisingly, although both effective and ineffective physical activity interventions resulted in a decrease in sedentary behaviour, interventions that effectively improved physical activity decreased sedentary behaviour more than interventions that did not effectively improve physical activity. This is plausible because within a fixed 24-h day, an increase in one behaviour (physical activity) is likely to be accompanied by a decrease in other behaviours, such as sedentary behaviour. However, because of the lack of systematic reviews summarising the overflow effects of behaviour change interventions, it was difficult to make comparisons between previous evidence and the present findings.
When sedentary behaviour was expressed as minutes per day, physical activity interventions did not have a significant effect on sedentary behaviour, for both school-aged children and adolescents. However, a subgroup analysis revealed a significant reduction in sedentary behaviour when it was measured subjectively, while the effect was not significant when device-based measurement was used. Importantly, no statistically significant subgroup difference was found between the subjective and device-based measurement approaches. It is noteworthy that a small number of studies (n = 4) were included in the ‘subjective measurement’ subsample. Additionally, the risk of bias was rated as ‘some concerns’ or ‘high’ across all the included studies (n = 11). Given these limitations, the heterogeneity of measurement should be further explored in future higher quality studies.
With only a limited number of studies (n = 7) included in this review and three studies included in the meta-analysis, findings on the effect of physical activity interventions on sleep were inconclusive, with both null findings and favourable changes reported. Unlike sedentary behaviour, the effect of physical activity interventions on sleep may involve various physiological mechanisms in addition to the time allocation due to the fixed total time of a 24-h day. A certain amount of physical activity could modify the functioning of the central nervous system and somatic physiology, and thereby affect the overall mechanisms of sleep [139]. A systematic review and meta-analysis of 66 studies including adult participants observed a small and positive effect size of both acute and regular exercise interventions on sleep duration [140]. The differences between our findings and those of that review may be due to differences in the target population (adults vs children), measurements of sleep outcomes or intervention duration. It is worth noting that all of the interventions included in this review had a duration of less than 24 weeks, and it is plausible that interventions with a longer duration may be necessary to induce changes in sleep patterns. However, there has been no consensus on the minimum duration of interventions required to achieve significant improvements in sleep among both children and adults [141, 142].
Favourable changes in standing time were observed in sedentary behaviour interventions, while no changes were observed in stepping time. It is noteworthy that all three studies included in the meta-analysis of this subgroup implemented standing desks as a primary intervention strategy [120, 122, 124]. A previous systematic review summarising the effect of school-based standing desk interventions among school-aged children and youth aged 5–18 years also reported consistent improvement in standing time [143]. In another systematic review examining the effect of standing desks on step counts among children and adolescents, no significant differences were reported between the intervention and control groups at post-intervention [144]. This could be attributed to the characteristics of standing desks and the context in which they are used (e.g. in a classroom), which primarily substituted standing time for sitting time but may limit opportunities for increasing stepping. To generate an overflow effect on physical activity of other intensities, future sedentary behaviour interventions for children should consider strategies both during and outside classes.
The screen time interventions did not have any significant effect on MVPA. The findings of our meta-analysis were supported by the findings of another intervention involving a large sample (1520 children aged 12–17 years), which did not observe significant changes in the self-reported quantity and frequency of physical activity following an intervention aimed at reducing media use [22]. The strategies used in the various interventions may point to potential reasons for these findings. The included studies aimed to reduce screen time through educational approaches or restrictions on device use [22, 23, 127, 128], rather than by providing alternative activities. As a result, the change in screen time did not necessarily translate into an increase in physical activity, particularly MVPA. However, robust conclusions cannot be made because of the limited number of studies. Regarding the effect of screen time interventions on sleep, no significant effect was observed in this review, but there were a limited number of relevant studies. Our findings were inconsistent with a previous systematic review of 11 studies that reported an approximate 10-min increase in sleep duration among children aged 2–13 years following screen time intervention [145]. The discrepancy between our findings and those of the previous review can be attributed to the different inclusion criteria. Specifically, this review focused exclusively on single-behaviour interventions targeting screen time, whereas the previous review also included multi-behaviour interventions (7/11 studies) and interventions that incorporated strategies to improve sleep (6/11 studies) [145]. Moreover, intervention characteristics are crucial when investigating the effects of regulating children’s screen time on sleep [145]. More specifically, previous interventions have used the strategy of limiting screen use before bedtime to improve sleep [146, 147], whereas all three screen time interventions included in this review focused on reducing total screen time through plans for media use or environmental modifications [22, 127, 128]. Further screen time interventions, especially those focused on evening or pre-bed screen time, are warranted to establish robust conclusions regarding their overflow effect on sleep.
The findings on the overflow effects of sleep interventions, which were based on the narrative analysis of a limited number of studies (n = 2), were inconclusive. The overflow effect of sleep interventions for children and adolescents has received limited attention. In a previous systematic review of studies of the effect of sleep interventions on children under the age of 18 years, only one study examined the effect on physical activity, and a sleep component was included as a part of a broader multi-behaviour intervention [148]. Among the two sleep interventions examined in this review [25, 26], one that targeted young children observed an 11-min increase in MVPA within the intervention group, but this was not significantly different from the control group [25]. The second intervention focused on antenatal and early postnatal education, and did not observe significant changes in light-to-vigorous physical activity [26]. This suggests that changes in sleep may not necessarily lead to changes in other types of behaviours. The aims of these sleep interventions should be taken into account, as they usually focus on sleep problems [26] or sleep hygiene [25], rather than sleep duration. Another potential reason for the different findings could be the absence of comprehensive measurement tools for all of the behaviours engaged in during a 24-h day. For instance, one study reported an increase of 54 min in sleep duration and a 2.7-min increase in total physical activity [25]. While not explicitly reported, it is reasonable to anticipate that there was a concomitant decrease in sedentary behaviour among the participants in the same study [25]. In summary, drawing definitive conclusions is challenging because of the limited number of studies.
To the best of our knowledge, this review represents the first attempt to comprehensively summarise the effects of single-movement behaviour interventions on non-targeted behaviours among participants from early childhood to adolescence. Nevertheless, some limitations should be acknowledged. First, in terms of the overflow effects of single-behaviour interventions on sleep and the overflow effects of sleep interventions, a concern arises from the limited number of studies. Second, a discrepancy was found in inclusion criteria for wear time of device-based measurements of the movement behaviours, which may potentially undermine the overall conclusions. Hence, it is critical to reach a consensus on the optimal inclusion criteria for wear time, so that future research can generate more robust evidence. Third, the majority of studies in this review (98/102 studies) were classified as having ‘some concerns’ or a ‘high risk of bias’, which may have contributed to less robust findings. Future high-quality studies with a low risk of bias are needed to strengthen the evidence. Interventions focusing on physical activity among school-aged children and adolescents, and that are implemented in schools and childcare centres appear to yield greater benefits in reducing sedentary behaviour than their counterparts. However, sleep patterns are relatively stable and challenging to modify [149]. More interventions with long durations and objective measurements are needed to examine the effects of behaviour change interventions on sleep. Future interventions are recommended to take holistic 24-h measurements of movement behaviours, regardless of the intervention target, whenever a device-based continuous measurement approach is possible.
Exploring the overflow effects of single-behaviour interventions has multi-faceted clinical and economic implications. Substantial decreases in physical activity and increases in sedentary behaviour are often observed in children and adolescents [150], and movement behaviours such as physical activity and sedentary behaviour have been found to be associated with various health outcomes in this period [151, 152]. While the effect size observed in this review was small, its related clinically important outcomes were supported by previous studies [153, 154]. A study on preschoolers found that replacing 5 min of sedentary behaviour with vigorous-intensity physical activity was linked to higher fat-free mass index, cardiorespiratory fitness and motor fitness [153]. Similarly, a study of school-aged children reported that substituting 10 min of sedentary behaviour with vigorous-intensity physical activity was associated with lower waist circumference and body mass index [154]. Implementing behaviour change interventions during this critical stage may have a positive influence on an individual’s health across the lifespan [155, 156]. The overflow effects of single-behaviour interventions indicate co-dependencies among behaviours, emphasising the need to consider all behaviours holistically. Taking advantage of potential overflow effects may maximise intervention effects. For example, interventions designed to improve physical activity could serve as a strategy to combat both physical inactivity and sedentary behaviour; promoting standing could be a practical alternative for reducing prolonged sedentary time. In the long term, taking advantage of a potential overflow effect can help alleviate economic burdens for both individuals and society. Furthermore, there are emerging efforts to develop interventions that target the three movement behaviours within a 24-h timeframe [157, 158], offering an integrated and flexible approach to achieve similar health outcomes. Nevertheless, it is crucial to acknowledge the complexity of the interplay and trade-offs among these behaviours. It has been argued that different movement behaviours may have unique barriers and facilitators that require tailored intervention strategies [159]. Further studies should help to understand how to optimise health by incorporating multiple target behaviours into an intervention.
5 Conclusions
Overflow effects on non-targeted behaviours were observed in interventions aimed at increasing physical activity or reducing sedentary behaviour although the effect size was small. Physical activity interventions effectively reduced sedentary behaviour, with those that improved physical activity showing a greater reduction compared with those that did not. Interventions targeting sedentary behaviour resulted in a concomitant increase in standing time. Overflow effects in other movement behaviours were not observed. These findings shed light on the importance of holistic consideration of a 24-h framework for evaluating movement behaviours. Further multiple-behaviour interventions are needed to explore strategies to obtain optimal health outcomes.
References
Rollo S, Antsygina O, Tremblay MS. The whole day matters: understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J Sport Health Sci. 2020;9:493–510.
Kuzik N, Poitras VJ, Tremblay MS, Lee E-Y, Hunter S, Carson V. Systematic review of the relationships between combinations of movement behaviours and health indicators in the early years (0–4 years). BMC Public Health. 2017;17:849.
Feng J, Zheng C, Sit CH-P, Reilly JJ, Huang WY. Associations between meeting 24-hour movement guidelines and health in the early years: a systematic review and meta-analysis. J Sports Sci. 2021;39:2545–57.
Biddle SJH, Ciaccioni S, Thomas G, Vergeer I. Physical activity and mental health in children and adolescents: an updated review of reviews and an analysis of causality. Psychol Sport Exerc. 2019;42:146–55.
Pate RR, Hillman C, Janz K, Katzmarzyk PT, Powell KE, Torres A, et al. Physical activity and health in children under 6 years of age: a systematic review. Med Sci Sport Exerc. 2019;51:1282–91.
Matricciani L, Paquet C, Galland B, Short M, Olds T. Children’s sleep and health: a meta-review. Sleep Med Rev. 2019;46:136–50.
Haghjoo P, Siri G, Soleimani E, Farhangi MA, Alesaeidi S. Screen time increases overweight and obesity risk among adolescents: a systematic review and dose-response meta-analysis. BMC Prim Care. 2022;23:161.
Stanczykiewicz B, Banik A, Knoll N, Keller J, Hohl DH, Rosińczuk J, et al. Sedentary behaviors and anxiety among children, adolescents and adults: a systematic review and meta-analysis. BMC Public Health. 2019;19:459.
Tremblay MS, Carson V, Chaput J-P, Gorber SC, Dinh T, Duggan M, et al. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016;41:S311–27.
Tremblay MS, Chaput J-P, Adamo KB, Aubert S, Barnes JD, Choquette L, et al. Canadian 24-hour movement guidelines for the early years (0–4 years): an integration of physical activity, sedentary behaviour, and sleep. BMC Public Health. 2017;17:874.
Rosenberger ME, Fulton JE, Buman MP, Troiano RP, Grandner MA, Buchner DM, et al. The 24-hour activity cycle: a new paradigm for physical activity. Med Sci Sports Exerc. 2019;51:454.
del Pozo-Cruz J, García-Hermoso A, Alfonso-Rosa RM, Alvarez-Barbosa F, Owen N, Chastin S, et al. Replacing sedentary time: meta-analysis of objective-assessment studies. Am J Prev Med. 2018;55:395–402.
Wilhite K, Booker B, Huang B-H, Antczak D, Corbett L, Parker P, et al. Combinations of physical activity, sedentary behavior, and sleep duration and their associations with physical, psychological, and educational outcomes in children and adolescents: a systematic review. Am J Epidemiol. 2023;192:665–79.
Lemos L, Clark C, Brand C, Pessoa ML, Gaya A, Mota J, et al. 24-hour movement behaviors and fitness in preschoolers: a compositional and isotemporal reallocation analysis. Scand J Med Sci Sports. 2021;31:1371–9.
Mota JG, Clark CCT, Bezerra TA, Lemos L, Reuter CP, Mota JAPS, et al. Twenty-four-hour movement behaviours and fundamental movement skills in preschool children: a compositional and isotemporal substitution analysis. J Sports Sci. 2020;38:2071–9.
Segura-Jiménez V, Pedišić Ž, Gába A, Dumuid D, Olds T, Štefelová N, et al. Longitudinal reallocations of time between 24-h movement behaviours and their associations with inflammation in children and adolescents: the UP&DOWN study. Int J Behav Nutr Phys Act. 2023;20:72.
Lau PWC, Song H, Song D, Wang J-J, Zhen S, Shi L, et al. 24-Hour movement behaviors and executive functions in preschoolers: a compositional and isotemporal reallocation analysis. Child Dev. 2023;00:1–12.
Fairclough SJ, Tyler R, Dainty JR, Dumuid D, Richardson C, Shepstone L, et al. Cross-sectional associations between 24-hour activity behaviours and mental health indicators in children and adolescents: a compositional data analysis. J Sports Sci. 2021;39:1602–14.
Sevil J, García-González L, Abós Á, Generelo E, Aibar A. Can high schools be an effective setting to promote healthy lifestyles? Effects of a multiple behavior change intervention in adolescents. J Adolesc Health. 2019;64:478–86.
Rhodes RE, Guerrero MD, Vanderloo LM, Barbeau K, Birken CS, Chaput J-P, et al. Development of a consensus statement on the role of the family in the physical activity, sedentary, and sleep behaviours of children and youth. Int J Behav Nutr Phys Act. 2020;17:74.
Downing KL, Hnatiuk JA, Hinkley T, Salmon J, Hesketh KD. Interventions to reduce sedentary behaviour in 0–5-year-olds: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2018;52:314–21.
Moreno MA, Binger KS, Zhao Q, Eickhoff JC. Effect of a family media use plan on media rule engagement among adolescents: a randomized clinical trial. JAMA Pediatr. 2021;175:351–8.
Babic MJ, Smith JJ, Morgan PJ, Lonsdale C, Plotnikoff RC, Eather N, et al. Intervention to reduce recreational screen-time in adolescents: outcomes and mediators from the ‘Switch-Off 4 Healthy Minds’ (S4HM) cluster randomized controlled trial. Prev Med. 2016;91:50–7.
Todd MK, Reis-Bergan MJ, Sidman CL, Flohr JA, Jameson-Walker K, Spicer-Bartolau T, et al. Effect of a family-based intervention on electronic media use and body composition among boys aged 8–11 years: a pilot study. J Child Health Care. 2008;12:344–58.
Yoong SL, Grady A, Stacey F, Polimeni M, Clayton O, Jones J, et al. A pilot randomized controlled trial examining the impact of a sleep intervention targeting home routines on young children’s (3–6 years) physical activity. Pediatr Obes. 2019;14: e12481.
Moir C, Meredith-Jones K, Taylor B, Gray A, Heath A, Dale K, et al. Early intervention to encourage physical activity in infants and toddlers: a randomized controlled trial. Med Sci Sport Exerc. 2016;48:2446–53.
Van Dyk TR, Krietsch KN, Saelens BE, Whitacre C, McAlister S, Beebe DW. Inducing more sleep on school nights reduces sedentary behavior without affecting physical activity in short-sleeping adolescents. Sleep Med. 2018;47:7–10.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10:89.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366: l4898.
Cochrane Collaboration. Review Manager (version 5.3) [computer software]. Copenhagen: The Nordic Cochrane Centre; 2014.
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane handbook for systematic reviews of interventions version 6.3. Hoboken: Wiley; 2022. Available from: www.training.cochrane.org/handbook. [Accessed 10 Sep 2024].
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Adamo KB, Wasenius NS, Grattan KP, Harvey ALJ, Naylor PJ, Barrowman NJ, et al. Effects of a preschool intervention on physical activity and body composition. J Pediatr. 2017;188:42-9.e2.
Baquet G, Aucouturier J, Gamelin FX, Berthoin S. Longitudinal follow-up of physical activity during school recess: impact of playground markings. Front Public Health. 2018;6:1–7.
Graves LEF, Ridgers ND, Atkinson G, Stratton G. The effect of active video gaming on children’s physical activity, behavior preferences and body composition. Pediatr Exerc Sci. 2010;22:535–46.
Gross RS, Mendelsohn AL, Yin HS, Tomopoulos S, Gross MB, Scheinmann R, et al. Randomized controlled trial of an early child obesity prevention intervention: impacts on infant tummy time. Obesity. 2017;25:920–7.
Hall A, Wolfenden L, Shoesmith A, McCarthy N, Wiggers J, Bauman AE, et al. The impact of an implementation intervention that increased school’s delivery of a mandatory physical activity policy on student outcomes: a cluster-randomised controlled trial. J Sci Med Sport. 2022;25:321–6.
Hands B, Larkin D, Rose E, Parker H, Smith A. Can young children make active choices? Outcomes of a feasibility trial in seven-year-old children. Early Child Dev Care. 2011;181:625–37.
Harrington DM, Davies MJ, Bodicoat DH, Charles JM, Chudasama YV, Gorely T, et al. Effectiveness of the “Girls Active” school-based physical activity programme: a cluster randomised controlled trial. Int J Behav Nutr Phys Act. 2018;15:40.
Jauho AM, Pyky R, Ahola R, Kangas M, Virtanen P, Korpelainen R, et al. Effect of wrist-worn activity monitor feedback on physical activity behavior: a randomized controlled trial in Finnish young men. Prev Med Rep. 2015;2:628–34.
Johnstone A, Hughes AR, Bonnar L, Booth JN, Reilly JJ. An active play intervention to improve physical activity and fundamental movement skills in children of low socio-economic status: feasibility cluster randomised controlled trial. Pilot Feasibility Stud. 2019;5:45.
Kolle E, Solberg RB, Säfvenbom R, Dyrstad SM, Berntsen S, Resaland GK, et al. The effect of a school-based intervention on physical activity, cardiorespiratory fitness and muscle strength: the School in Motion cluster randomized trial. Int J Behav Nutr Phys Act. 2020;17:1–14.
Laukkanen A, Juhani Pesola A, Heikkinen R, Kaarina Sääkslahti A, Finni T. Family-based cluster randomized controlled trial enhancing physical activity and motor competence in 4-7-year-old children. PLoS One. 2015;10:1–17.
Li B, Pallan M, Liu WJ, Hemming K, Frew E, Lin R, et al. The CHIRPY DRAGON intervention in preventing obesity in Chinese primaryschool-aged children: a cluster-randomised controlled trial. PLoS Med. 2019;16: e1002971.
Beets MW, Weaver RG, Turner-McGrievy G, Huberty J, Ward DS, Pate RR, et al. Making policy practice in afterschool programs: a randomized controlled trial on physical activity changes. Am J Prev Med. 2015;48:694–706.
Likhitweerawong N, Boonchooduang N, Kittisakmontri K, Chonchaiya W, Louthrenoo O. Short-term outcomes of tablet/smartphone-based (OBEST) application among obese Thai school-aged children and adolescents: a randomized controlled trial. Obes Med. 2020;20: 100287.
Madsen K, Linchey J, Gerstein D, Ross M, Myers E, Brown K, et al. Energy balance 4 kids with play: results from a two-year cluster-randomized trial. Child Obes. 2015;11:375–83.
Maloney AE, Bethea TC, Kelsey KS, Marks JT, Paez S, Rosenberg AM, et al. A pilot of a video game (DDR) to promote physical activity and decrease sedentary screen time. Obesity. 2008;16:2074–80.
Morell-Azanza L, Ojeda-Rodríguez A, Ochotorena-Elicegui A, Martín-Calvo N, Chueca M, Marti A, et al. Changes in objectively measured physical activity after a multidisciplinary lifestyle intervention in children with abdominal obesity: a randomized control trial. BMC Pediatr. 2019;19:6–13.
Morris JL, Daly-Smith A, Defeyter MA, McKenna J, Zwolinsky S, Lloyd S, et al. A pedometer-based physically active learning intervention: the importance of using preintervention physical activity categories to assess effectiveness. Pediatr Exerc Sci. 2019;31:356–62.
Morrison R, Reilly JJ, Penpraze V, Westgarth C, Ward DS, Mutrie N, et al. Children, parents and pets exercising together (CPET): exploratory randomised controlled trial. BMC Public Health. 2013;13:1096.
Nathan N, McCarthy N, Hope K, Sutherland R, Lecathelinais C, Hall A, et al. The impact of school uniforms on primary school student’s physical activity at school: outcomes of a cluster randomized controlled trial. Int J Behav Nutr Phys Act. 2021;18:1–9.
O’Dwyer MV, Fairclough SJ, Ridgers ND, Knowles ZR, Foweather L, Stratton G. Effect of a school-based active play intervention on sedentary time and physical activity in preschool children. Health Educ Res. 2013;28:931–42.
Okely AD, Stanley RM, Jones RA, Cliff DP, Trost SG, Berthelsen D, et al. ‘Jump start’ childcare-based intervention to promote physical activity in pre-schoolers: six-month findings from a cluster randomised trial. Int J Behav Nutr Phys Act. 2020;17:6.
Pate RR, Brown WH, Pfeiffer KA, Howie EK, Saunders RP, Addy CL, et al. An intervention to increase physical activity in children: a randomized controlled trial with 4-year-olds in preschools. Am J Prev Med. 2016;51:12–22.
Bundy A, Engelen L, Wyver S, Tranter P, Ragen J, Bauman A, et al. Sydney playground project: a cluster-randomized trial to increase physical activity, play, and social skills. J Sch Health. 2017;87:751–9.
Resaland GK, Moe VF, Bartholomew JB, Andersen LB, McKay HA, Anderssen SA, et al. Gender-specific effects of physical activity on children’s academic performance: the Active Smarter Kids cluster randomized controlled trial. Prev Med. 2018;106:171–6.
Riiser K, Richardsen KR, Haugen ALH, Lund S, Løndal K. Active play in ASP: a matched-pair cluster-randomized trial investigating the effectiveness of an intervention in after-school programs for supporting children’s physical activity. BMC Public Health. 2020;20:1–12.
Saelens BE, Sallis JF, Wilfley DE, Patrick K, Cella JA, Buchta R. Behavioral weight control for overweight adolescents initiated in primary care. Obes Res. 2002;10:22–32.
Sahota P, Rudolf MCJ, Dixey R, Hill AJ, Barth JH, Cade J. Evaluation of implementation and effect of primary school based intervention to reduce risk factors for obesity. Br Med J. 2001;323:1027–9.
Staiano AE, Beyl RA, Hsia DS, Katzmarzyk PT, Newton RL. Twelve weeks of dance exergaming in overweight and obese adolescent girls: transfer effects on physical activity, screen time, and self-efficacy. J Sport Health Sci. 2017;6:4–10.
Suchert V, Isensee B, Sargent J, Weisser B, Hanewinkel R. Prospective effects of pedometer use and class competitions on physical activity in youth: a cluster-randomized controlled trial. Prev Med. 2015;81:399–404.
Toftager M, Christiansen LB, Ersbøll AK, Kristensen PL, Due P, Troelsen J. Intervention effects on adolescent physical activity in the multicomponent SPACE study: a cluster randomized controlled trial. PLoS One. 2014;9: e99369.
Tuominen PPA, Husu P, Raitanen J, Kujala UM, Luoto RM. The effect of a movement-to-music video program on the objectively measured sedentary time and physical activity of preschool-aged children and their mothers: a randomized controlled trial. PLoS One. 2017;12:1–21.
Vazou S, Saint-Maurice PF, Skrade M, Welk G. Effect of integrated physical activities with mathematics on objectively assessed physical activity. Children. 2018;5:140.
Weigensberg MJ, Àvila Q, Spruijt-Metz D, Davis JN, Wen CKF, Goodman K, et al. Imagine HEALTH: randomized controlled trial of a guided imagery lifestyle intervention to improve obesity-related lifestyle behaviors in predominantly Latinx adolescents. J Altern Complement Med. 2021;27:738–49.
Cardon G, Labarque V, Smits D, De BI. Promoting physical activity at the pre-school playground: the effects of providing markings and play equipment. Prev Med. 2009;48:335–40.
Wells NM, Myers BM, Henderson CR. School gardens and physical activity: a randomized controlled trial of low-income elementary schools. Prev Med. 2014;69:S27-33.
Alhassan S, Sudarsky L, Dangol G, Zhou W, Turley A, Sylvia AM, et al. Feasibility and preliminary efficacy of a childcare provider-led activity intervention on toddlers’ physical activity levels: a pilot randomized controlled study. Child Care Pract. 2022. https://doi.org/10.1080/13575279.2022.2082381.
Moore JB, Weaver RG, Levine BJ, Singletary CR, Carson RL, Beets MW, et al. A pilot study of a comprehensive school physical activity program in elementary schools: be a champion! Health Behav Policy Rev. 2021;8:110–8.
Strugnell C, Crooks N, Gaskin CJ, Becker D, Orellana L, Bolton KA, et al. Four-year accelerometry outcomes from a cluster randomized whole of systems trial of prevention strategies for childhood obesity. Child Obes. 2022;19:332–40.
Wolfenden L, Jones J, Parmenter B, Razak LA, Wiggers J, Morgan PJ, et al. Efficacy of a free-play intervention to increase physical activity during childcare: a randomized controlled trial. Health Educ Res. 2019;34:84–97.
Andersen E, Øvreås S, Jørgensen KA, Borch-Jenssen J, Moser T. Children’s physical activity level and sedentary behaviour in Norwegian early childhood education and care: effects of a staff-led cluster-randomised controlled trial. BMC Public Health. 2020;20:1651.
Blaes A, Ridgers ND, Aucouturier J, Van Praagh E, Berthoin S, Baquet G. Effects of a playground marking intervention on school recess physical activity in French children. Prev Med. 2013;57:580–4.
Crouter SE, De Ferranti SD, Whiteley J, Steltz SK, Osganian SK, Feldman HA, et al. Effect on physical activity of a randomized afterschool intervention for inner city children in 3rd to 5th grade. PLoS One. 2015;10:1–18.
Engelen L, Bundy AC, Naughton G, Simpson JM, Bauman A, Ragen J, et al. Increasing physical activity in young primary school children - it’s child’s play: a cluster randomised controlled trial. Prev Med. 2013;56:319–25.
Fetter DS, Scherr RE, Linnell JD, Dharmar M, Schaefer SE, Zidenberg-Cherr S. Effect of the shaping healthy choices program, a multicomponent, school-based nutrition intervention, on physical activity intensity. J Am Coll Nutr. 2018;37:472–8.
Carlin A, Murphy MH, Nevill A, Gallagher AM. Effects of a peer-led Walking In ScHools intervention (the WISH study) on physical activity levels of adolescent girls: a cluster randomised pilot study. Trials. 2018;19:1–12.
Goldfield GS, Harvey ALJ, Grattan KP, Temple V, Naylor PJ, Alberga AS, et al. Effects of child care intervention on physical activity and body composition. Am J Prev Med. 2016;51:225–31.
Gutiérrez-Martínez L, Martínez RG, González SA, Bolívar MA, Estupiñan OV, Sarmiento OL. Effects of a strategy for the promotion of physical activity in students from Bogotá. Rev Saude Publica. 2018;52:1–11.
McLellan G, Arthur R, Donnelly S, Bakshi A, Fairclough SJ, Taylor SL, et al. Feasibility and acceptability of a classroom-based active breaks intervention for 8–12-year-old children. Res Q Exerc Sport. 2022;93:813–24.
Nathan NK, Sutherland RL, Hope K, McCarthy NJ, Pettett M, Elton B, et al. Implementation of a school physical activity policy improves student physical activity levels: outcomes of a cluster-randomized controlled trial. J Phys Act Health. 2020;17:1009–18.
Norris E, Dunsmuir S, Duke-Williams O, Stamatakis E, Shelton N. Physically active lessons improve lesson activity and on-task behavior: a cluster-randomized controlled trial of the “Virtual Traveller” intervention. Health Educ Behav. 2018;45:945–56.
Norris E, Shelton N, Dunsmuir S, Duke-Williams O, Stamatakis E. Virtual field trips as physically active lessons for children: a pilot study. BMC Public Health. 2015;15:1–9.
O’Dwyer MV, Fairclough SJ, Knowles Z, Stratton G. Effect of a family focused active play intervention on sedentary time and physical activity in preschool children. Int J Behav Nutr Phys Act. 2012;9:117.
Riley N, Lubans DR, Holmes K, Morgan PJ. Findings from the EASY minds cluster randomized controlled trial: evaluation of a physical activity integration program for mathematics in primary schools. J Phys Act Health. 2016;13:198–206.
Riley N, Lubans DR, Morgan PJ, Young M. Outcomes and process evaluation of a programme integrating physical activity into the primary school mathematics curriculum: the EASY Minds pilot randomised controlled trial. J Sci Med Sport. 2015;18:656–61.
Sacher PM, Kolotourou M, Chadwick PM, Cole TJ, Lawson MS, Lucas A, et al. Randomized controlled trial of the MEND program: a family-based community intervention for childhood obesty. Obesity. 2010;18:S62–8.
Cradock AL, Barrett JL, Giles CM, Lee RM, Kenney EL, DeBlois ME, et al. Promoting physical activity with the Out of School Nutrition and Physical Activity (OSNAP) initiative: a cluster-randomized controlled trial. JAMA Pediatr. 2016;170:155–62.
Sebire SJ, Jago R, Banfield K, Edwards MJ, Campbell R, Kipping R, et al. Results of a feasibility cluster randomised controlled trial of a peer-led school-based intervention to increase the physical activity of adolescent girls (PLAN-A). Int J Behav Nutr Phys Act. 2018;15:1–13.
Taylor SL, Noonan RJ, Knowles ZR, Owen MB, McGrane B, Curry WB, et al. Evaluation of a pilot school-based physical activity clustered randomised controlled trial—active schools: Skelmersdale. Int J Environ Res Public Health. 2018;15:1011.
Comeras-Chueca C, Villalba-Heredia L, Perez-Lasierra JL, Marín-Puyalto J, Lozano-Berges G, Matute-Llorente Á, et al. Active video games improve muscular fitness and motor skills in children with overweight or obesity. Int J Environ Res Public Health. 2022;19:2642.
Guo H, Zeng X, Zhuang Q, Zheng Y, Chen S. Intervention of childhood and adolescents obesity in Shantou city. Obes Res Clin Pract. 2015;9:357–64.
Verswijveren SJJM, Ridgers ND, Martín-Fernández JA, Chastin S, Cerin E, Chinapaw MJM, et al. Intervention effects on children’s movement behaviour accumulation as a result of the Transform-Us! School- and home-based cluster randomised controlled trial. Int J Behav Nutr Phys Act. 2022;19:76.
Polo-Recuero B, Ordóñez-Dios A, Rojo-Tirado MÁ, Lorenzo A. Do you want to increase physical activity in adolescents? A school-based physical activity program could be an efficient way. Children. 2023;10:1641.
Grendstad H, Hallén J. Effects of adding high-intensity training during an 8-week period on maximal oxygen uptake in 12-year-old youth athletes. Scand J Med Sci Sports. 2024;34: e14489.
Suksong N, Maphong R, Sriramatr S. A walking intervention for enhancing self-efficacy, physical activity, and cardiovascular endurance in overweight children: a randomized controlled trial. Ann Appl Sport Sci. 2024;12: e1291.
Direito A, Jiang Y, Whittaker R, Maddison R. Apps for IMproving FITness and increasing physical activity among young people: the AIMFIT pragmatic randomized controlled trial. J Med Internet Res. 2015;17:1–13.
Evans EW, Wing RR, Pierre DF, Howie WC, Brinker M, Jelalian E. Testing the effect of summer camp on excess summer weight gain in youth from low-income households: a randomized controlled trial. BMC Public Health. 2020;20:1–10.
Gill M, Roth SE, Chan-Golston AM, Rice LN, Crespi CM, Koniak-Griffin D, et al. Evaluation of an intervention to increase physical activity in low-income, urban middle schools. J Sch Health. 2019;89:705–14.
Leme ACB, Lubans DR, Guerra PH, Dewar D, Toassa EC, Philippi ST. Preventing obesity among Brazilian adolescent girls: six-month outcomes of the Healthy Habits, Healthy Girls-Brazil school-based randomized controlled trial. Prev Med. 2016;86:77–83.
Essery EV, DiMarco NM, Rich SS, Nichols DL. Mothers of preschoolers report using less pressure in child feeding situations following a newsletter intervention. J Nutr Educ Behav. 2008;40:110–5.
Lerner-Geva L, Bar-Zvi E, Levitan G, Boyko V, Reichman B, Pinhas-Hamiel O. An intervention for improving the lifestyle habits of kindergarten children in Israel: a cluster-randomised controlled trial investigation. Public Health Nutr. 2015;18:1537–44.
Mahajan A, Negi PC, Gandhi S, Sharma D, Grover N. Impact of school-based health behavioral intervention on awareness, practice pattern of healthy lifestyle, and cardiometabolic risk factors among school children of Shimla: a cluster-randomized, intervention study. Indian J Pediatr. 2022;89:343–50.
Weintraub DL, Tirumalai EC, Haydel KF, Fujimoto M, Fulton JE, Robinson TN. Team sports for overweight children. Arch Pediatr Adolesc Med. 2008;162:232.
Ni Mhurchu C, Maddison R, Jiang Y, Jull A, Prapavessis H, Rodgers A. Couch potatoes to jumping beans: a pilot study of the effect of active video games on physical activity in children. Int J Behav Nutr Phys Act. 2008;5:1–5.
Ling J, Suriyawong W, Robbins LB, Zhang N, Kerver JM. FirstStep2Health: a cluster randomised trial to promote healthy behaviours and prevent obesity amongst low-income preschoolers. Pediatr Obes. 2024;19: e13122.
Morgan PJ, Young MD, Barnes AT, Eather N, Pollock ER, Lubans DR. Engaging fathers to increase physical activity in girls: the “Dads And Daughters Exercising and Empowered” (DADEE) randomized controlled trial. Ann Behav Med. 2019;53:39–52.
Simon C, Kellou N, Dugas J, Platat C, Copin N, Schweitzer B, et al. A socio-ecological approach promoting physical activity and limiting sedentary behavior in adolescence showed weight benefits maintained 2.5 years after intervention cessation. Int J Obes. 2014;38:936–43.
Tarro L, Llauradó E, Aceves-Martins M, Moriña D, Papell-Garcia I, Arola L, et al. Impact of a youth-led social marketing intervention run by adolescents to encourage healthy lifestyles among younger school peers (EYTO-Kids project): a parallel-cluster randomised controlled pilot study. J Epidemiol Community Health. 2019;73:324–33.
Trost SG, Tang R, Loprinzi PD. Feasibility and efficacy of a church-based intervention to promote physical activity in children. J Phys Act Health. 2009;6:741–9.
Morgan PJ, Rayward AT, Young MD, Pollock ER, Eather N, Barnes AT, et al. Establishing effectiveness of a community-based, physical activity program for fathers and daughters: a randomized controlled trial. Ann Behav Med. 2022;56:698–711.
Zhou HR, Wang WW, Yang HF, Qi SX, Wang CC, Hong X. The effects of a one year school-based comprehensive lifestyle intervention among Chinese kids against obesity (CLICK-obesity) in Nanjing, China. J Public Health. 2023;31:1071–9.
Amini M, Djazayery A, Majdzadeh R, Taghdisi MH, Sadrzadeh-Yeganeh H, Abdollahi Z, et al. A school-based intervention to reduce excess weight in overweight and obese primary school students. Biol Res Nurs. 2016;18:531–40.
Efstathiou NT, Risvas GS, Theodoraki EMM, Galanaki EP, Zampelas AD. Health education: effects on classroom climate and physical activity. Health Educ J. 2016;75:799–810.
Davis CL, Tkacz J, Gregoski M, Boyle CA, Lovrekovic G. Aerobic exercise and snoring in overweight children: a randomized controlled trial. Obesity. 2006;14:1985–91.
Sundgot-Borgen C, Friborg O, Kolle E, Torstveit MK, Sundgot-Borgen J, Engen KME, et al. Does the Healthy Body Image program improve lifestyle habits among high school students? A randomized controlled trial with 12-month follow-up. J Int Med Res. 2019;48:300060519889453.
Fantini L, Gostoli S, Artin MG, Rafanelli C. An intervention based on Well-Being Therapy to prevent alcohol use and other unhealthy lifestyle behaviors among students: a three-arm cluster randomized controlled trial. Psychol Health Med. 2024;29:930–50.
Torres-Lopez LV, Migueles JH, Cadenas-Sanchez C, Bendtsen M, Henriksson P, Mora-Gonzalez J, et al. Effects of exercise on sleep in children with overweight/obesity: a randomized clinical trial. Obesity. 2024;32:281–90.
Clemes SA, Barber SE, Bingham DD, Ridgers ND, Fletcher E, Pearson N, et al. Reducing children’s classroom sitting time using sit-to-stand desks: findings from pilot studies in UK and Australian primary schools. J Public Health. 2016;38:526–33.
Ee J, Parry S, de Oliveira BIR, McVeigh JA, Howie E, Straker L. Does a classroom standing desk intervention modify standing and sitting behaviour and musculoskeletal symptoms during school time and physical activity during waking time? Int J Environ Res Public Health. 2018;15:1–13.
Ellis YG, Cliff DP, Howard SJ, Okely AD. Feasibility, acceptability, and potential efficacy of a childcare-based intervention to reduce sitting time among pre-schoolers: a pilot randomised controlled trial. J Sports Sci. 2019;37:146–55.
Parrish A, Trost SG, Howard SJ, Batterham M, Cliff D, Salmon J, et al. Evaluation of an intervention to reduce adolescent sitting time during the school day: the ‘Stand Up for Health’ randomised controlled trial. J Sci Med Sport. 2018;21:1244–9.
Verloigne M, Ridgers ND, De Bourdeaudhuij I, Cardon G. Effect and process evaluation of implementing standing desks in primary and secondary schools in Belgium: a cluster-randomised controlled trial. Int J Behav Nutr Phys Act. 2018;15:94.
Epstein LH, Roemmich JN, Robinson JL, Paluch RA, Winiewicz DD, Fuerch JH, et al. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Arch Pediatr Adolesc Med. 2008;162:239–45.
Lumeng JC, Miller AL, Horodynski MA, Brophy-Herb HE, Contreras A, Lee H, et al. Improving self-regulation for obesity prevention in head start: a randomized controlled trial. Pediatrics. 2017;139: e20162047.
Maddison R, Marsh S, Foley L, Epstein LH, Olds T, Dewes O, et al. Screen-Time Weight-loss Intervention Targeting Children at Home (SWITCH): a randomized controlled trial. Int J Behav Nutr Phys Act. 2014;11:111.
Pedersen J, Rasmussen MGB, Sørensen SO, Mortensen SR, Olesen LG, Brønd JC, et al. Effects of limiting recreational screen media use on physical activity and sleep in families with children: a cluster randomized clinical trial. JAMA Pediatr. 2022;176:741–9.
Alhassan S, Nwaokelemeh O, Ghazarian M, Roberts J, Mendoza A, Shitole S. Effects of locomotor skill program on minority preschoolers’ physical activity levels. Pediatr Exerc Sci. 2012;24:435–49.
Alhassan S, Nwaokelemeh O, Lyden K, Goldsby T, Mendoza A. A pilot study to examine the effect of additional structured outdoor playtime on preschoolers’ physical activity levels. Child Care Pract. 2013;19:23–35.
De Bock F, Genser B, Raat H, Fischer JE, Renz-Polster H. A participatory physical activity intervention in preschools: a cluster randomized controlled trial. Am J Prev Med. 2013;45:64–74.
Maniccia DM, Davison KK, Marshall SJ, Manganello JA, Dennison BA. A meta-analysis of interventions that target children’s screen time for reduction. Pediatrics. 2011;128:e193-210.
Kontostoli E, Jones AP, Pearson N, Foley L, Biddle SJH, Atkin AJ. Age-related change in sedentary behavior during childhood and adolescence: a systematic review and meta-analysis. Obes Rev. 2021;22: e13263.
Hartwig TB, Sanders T, Vasconcellos D, Noetel M, Parker PD, Lubans DR, et al. School-based interventions modestly increase physical activity and cardiorespiratory fitness but are least effective for youth who need them most: an individual participant pooled analysis of 20 controlled trials. Br J Sports Med. 2021;55:721–9.
Burns RD, Fu Y, Podlog LW. School-based physical activity interventions and physical activity enjoyment: a meta-analysis. Prev Med. 2017;103:84–90.
Pozuelo-Carrascosa DP, García-Hermoso A, Álvarez-Bueno C, Sánchez-López M, Martinez-Vizcaino V. Effectiveness of school-based physical activity programmes on cardiorespiratory fitness in children: a meta-analysis of randomised controlled trials. Br J Sports Med. 2018;52:1234–40.
Mei H, Xiong Y, Xie S, Guo S, Li Y, Guo B, et al. The impact of long-term school-based physical activity interventions on body mass index of primary school children: a meta-analysis of randomized controlled trials. BMC Public Health. 2016;16:205.
Andermo S, Hallgren M, Nguyen T-T-D, Jonsson S, Petersen S, Friberg M, et al. School-related physical activity interventions and mental health among children: a systematic review and meta-analysis. Sport Med Open. 2020;6:25.
Uchida S, Shioda K, Morita Y, Kubota C, Ganeko M, Takeda N. Exercise effects on sleep physiology. Front Neurol. 2012;3:48.
Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: a meta-analytic review. J Behav Med. 2015;38:427–49.
Fangupo LJ, Haszard JJ, Reynolds AN, Lucas AW, McIntosh DR, Richards R, et al. Do sleep interventions change sleep duration in children aged 0–5 years? A systematic review and meta-analysis of randomised controlled trials. Sleep Med Rev. 2021;59: 101498.
Murawski B, Wade L, Plotnikoff RC, Lubans DR, Duncan MJ. A systematic review and meta-analysis of cognitive and behavioral interventions to improve sleep health in adults without sleep disorders. Sleep Med Rev. 2018;40:160–9.
Minges KE, Chao AM, Irwin ML, Owen N, Park C, Whittemore R, et al. Classroom standing desks and sedentary behavior: a systematic review. Pediatrics. 2016;137: e20153087.
Sherry AP, Pearson N, Clemes SA. The effects of standing desks within the school classroom: a systematic review. Prev Med Rep. 2016;3:338–47.
Martin KB, Bednarz JM, Aromataris EC. Interventions to control children’s screen use and their effect on sleep: a systematic review and meta-analysis. J Sleep Res. 2020;30: e13130.
Tamura N, Tanaka H. Effects of sleep education with self-help treatment for elementary schoolchild with nocturnal lifestyle and irritability. Sleep Biol Rhythms. 2014;12:169–79.
Wolfson AR, Harkins E, Johnson M, Marco C. Effects of the Young Adolescent Sleep Smart Program on sleep hygiene practices, sleep health efficacy, and behavioral well-being. Sleep Health. 2015;1:197–204.
Yoong SL, Chai LK, Williams CM, Wiggers J, Finch M, Wolfenden L. Systematic review and meta-analysis of interventions targeting sleep and their impact on child body mass index, diet, and physical activity. Obesity. 2016;24:1140–7.
Gregory AM, O’Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child Adolesc Psychiatry. 2002;41:964–71.
Husøy A, Kolle E, Steene-Johannessen J, Dalene KE, Andersen LB, Ekelund U, et al. Longitudinal changes in device-measured physical activity from childhood to young adulthood: the PANCS follow-up study. Int J Behav Nutr Phys Act. 2024;21:29.
Agbaje AO, Perng W, Tuomainen T-P. Effects of accelerometer-based sedentary time and physical activity on DEXA-measured fat mass in 6059 children. Nat Commun. 2023;14:8232.
Agbaje AO. The interactive effects of sedentary time, physical activity, and fat mass on insulin resistance in the young population. J Clin Endocrinol Metab. 2024. https://doi.org/10.1210/clinem/dgae135.
Leppänen MH, Nyström CD, Henriksson P, Pomeroy J, Ruiz JR, Ortega FB, et al. Physical activity intensity, sedentary behavior, body composition and physical fitness in 4-year-old children: results from the ministop trial. Int J Obes. 2016;40:1126–33.
Dalene KE, Anderssen SA, Andersen LB, Steene-Johannessen J, Ekelund U, Hansen BH, et al. Cross-sectional and prospective associations between physical activity, body mass index and waist circumference in children and adolescents. Obes Sci Pract. 2017;3:249–57.
Hassan MA, Zhou W, Ye M, He H, Gao Z. The effectiveness of physical activity interventions on blood pressure in children and adolescents: a systematic review and network meta-analysis. J Sport Health Sci. 2024;13:699–708.
Kwon S, Janz KF, Letuchy EM, Burns TL, Levy SM. Active lifestyle in childhood and adolescence prevents obesity development in young adulthood. Obesity. 2015;23:2462–9.
Feng J, Huang WY, Sit CH-P. Effectiveness of a parent-focused intervention targeting 24-h movement behaviors in preschool-aged children: study protocol for a randomized controlled trial. Front Public Health. 2022;10: 870281.
Flood SM, Thompson B, Faulkner G, Vanderloo LM, Blackett B, Dolf M, et al. Development of a participACTION app-based intervention for improving postsecondary students’ 24-hour movement guideline behaviors: protocol for the application of intervention mapping. JMIR Res Protoc. 2023;12: e39977.
Hesketh KR, Lakshman R, van Sluijs EMF. Barriers and facilitators to young children’s physical activity and sedentary behaviour: a systematic review and synthesis of qualitative literature. Obes Rev. 2017;18:987–1017.
Acknowledgements
We express our gratitude to all the contributing authors for providing the data.
Funding
Open access funding provided by Hong Kong Baptist University Library.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest/Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
All data have been included in the article or included as supplementary information.
Code Availability
Not applicable.
Authors’ Contributions
JF and WH conceived the idea for the review. JF and CZ searched and screened the studies. JF, MN and CZ completed the data extraction. JF and JJ carried out the risk of bias assessment. JF performed the data analysis and drafted the initial manuscript. All authors edited the paper and gave the final approval of the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Feng, J., Huang, W.Y., Zheng, C. et al. The Overflow Effects of Movement Behaviour Change Interventions for Children and Adolescents: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Sports Med (2024). https://doi.org/10.1007/s40279-024-02113-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s40279-024-02113-1