Abstract
Objective
Concussions are common among youth athletes and could disrupt critical neurodevelopment. This study examined the association between age of first concussion (AFC) and neurocognitive performance, psychological distress, postural stability, and symptoms commonly associated with concussion in healthy collegiate men and women student athletes.
Methods
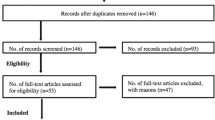
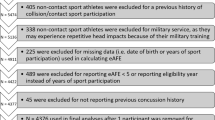
Participants included 4267 collegiate athletes from various contact, limited-contact, and non-contact sports (1818 women and 2449 men) who completed baseline assessments as part of the Concussion Assessment, Research and Education (CARE) Consortium. Psychological distress was assessed with the Brief Symptom Inventory 18; neurocognitive performance was assessed with the Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT); symptoms commonly associated with concussion were assessed with the ImPACT Post-Concussion Symptom Scale; postural stability was assessed with the Balance Error Scoring System. Generalized linear models were used to examine the effects of AFC on clinical outcomes separately in men and women.
Results
Later AFC was associated with lower global (Exp(B) = 0.96, P = 0.001) and somatic (Exp(B) = 0.96, P = 0.002) psychological distress on the Brief Symptom Inventory 18 and faster ImPACT reaction time (B = − 0.003, P = 0.001) in women. AFC was not associated with any clinical outcomes in men.
Conclusion
Younger AFC was associated with some differences in psychological distress and reaction time among women but not men; however, these results are likely not clinically meaningful. Sociodemographic disparities, pre-existing conditions, and sport type may impact clinical and cognitive outcomes in collegiate athletes more than concussion history. Future work should examine the relationship between AFC and lifespan-related outcomes.


Similar content being viewed by others
References
McCrory P, Meeuwisse W, Dvorak J, Aubry M, Bailes J, Broglio S, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51:838–47.
Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21:375–8.
Centers for Disease Control and Prevention, USA. Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged ≤19 years --- United States, 2001--2009. MMWR Morb Mortal Wkly Rep. 2011;60:1337–42.
Alosco ML, Stern RA. Youth exposure to repetitive head impacts from tackle football and long-term neurologic outcomes: a review of the literature, knowledge gaps and future directions, and societal and clinical implications. Semin Pediatr Neurol. 2019;30:107–16.
Anderson V, Moore C. Age at injury as a predictor of outcome following pediatric head injury: a longitudinal perspective. Child Neuropsychol. 1995;1:187–202.
McKinlay A. Long-term outcomes of traumatic brain injury in early childhood. Aust Psychol. 2014;49:323–7.
Risen SR, Reesman J, Yenokyan G, Slomine BS, Suskauer SJ. The course of concussion recovery in children 6–12 years of age: experience from an interdisciplinary rehabilitation clinic. PM&R. 2017;9:874–83.
Bernard CO, Ponsford JA, McKinlay A, McKenzie D, Krieser D. Predictors of post-concussive symptoms in young children: injury versus non-injury related factors. J Int Neuropsychol Soc. 2016;22:793–803.
Zemek R, Barrowman N, Freedman SB, Gravel J, Gagnon I, McGahern C, et al. Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA. 2016;315:1014–25.
Neidecker JM, Gealt DB, Luksch JR, Weaver MD. First-time sports-related concussion recovery: the role of sex, age, and sport. J Osteopath Med. 2017;117:635–42.
Dufour SC, Adams RS, Brody DL, Puente AN, Gray JC. Prevalence and correlates of concussion in children: data from the Adolescent Brain Cognitive Development study. Cortex. 2020;131:237–50.
De Bellis MD, Keshavan MS, Beers SR, Hall J, Frustaci K, Masalehdan A, et al. Sex differences in brain maturation during childhood and adolescence. Cereb Cortex. 2001;11:552–7.
Gur RE, Gur RC. Sex differences in brain and behavior in adolescence: findings from the Philadelphia Neurodevelopmental Cohort. Neurosci Biobehav Rev. 2016;70:159–70.
Broglio SP, McCrea M, McAllister T, Harezlak J, Katz B, Hack D, et al. A national study on the effects of concussion in collegiate athletes and US military service academy members: the NCAA–DoD concussion assessment, research and education (CARE) consortium structure and methods. Sports Med. 2017;47:1437–51.
Rice SG. Medical conditions affecting sports participation. Pediatrics. 2008;121:841–8.
Carney N, Ghajar J, Jagoda A, Bedrick S, Davis-O’Reilly C, du Coudray H, et al. Concussion guidelines step 1: systematic review of prevalent indicators. Neurosurgery. 2014;75:S3-15.
Schmidt JD, Rizzone K, Hoffman NL, Weber ML, Jones C, Bazarian J, et al. Age at first concussion influences the number of subsequent concussions. Pediatr Neurol. 2018;81:19–24.
Hollingshead AB. Four factor index of social status. New Haven, CT: Yale University; 1975. https://sociology.yale.edu/sites/default/files/files/yjs_fall_2011.pdf#page=21
Meachen S-J, Hanks RA, Millis SR, Rapport LJ. The reliability and validity of the Brief Symptom Inventory—18 in persons with traumatic brain injury. Arch Phys Med Rehabil. 2008;89:958–65.
Lancaster MA, McCrea MA, Nelson LD. Psychometric properties and normative data for the Brief Symptom Inventory-18 (BSI-18) in high school and collegiate athletes. Clin Neuropsychol. 2016;30:321–33.
Derogatis L. BSI 18, Brief Symptom Inventory 18: administration, scoring and procedures manual. Minneapolis: NCS Pearson Inc.; 2001.
Schatz P, Pardini JE, Lovell MR, Collins MW, Podell K. Sensitivity and specificity of the ImPACT Test Battery for concussion in athletes. Arch Clin Neuropsychol. 2006;21:91–9.
Caccese JB, Bodt BA, Iverson GL, Kaminski TW, Bryk K, Oldham J, et al. Estimated age of first exposure to contact sports and neurocognitive, psychological, and physical outcomes in healthy NCAA collegiate athletes: a cohort study. Sports Med. 2020;50:1377–92.
Buckley TA, Oldham JR, Caccese JB. Postural control deficits identify lingering post-concussion neurological deficits. J Sport Health Sci. 2016;5:61–9.
Houck Z, Asken B, Clugston J, Perlstein W, Bauer R. Socioeconomic status and race outperform concussion history and sport participation in predicting collegiate athlete baseline neurocognitive scores. J Int Neuropsychol Soc. 2018;24:1–10.
Taranto E, Fishman M, Garvey K, Perlman M, Benjamin HJ, Ross LF. Public attitudes and knowledge about youth sports participation and concussion risk in an urban area. J Natl Med Assoc. 2018;110:635–43.
Fishman M, Taranto E, Perlman M, Quinlan K, Benjamin HJ, Ross LF. Attitudes and counseling practices of pediatricians regarding youth sports participation and concussion risks. J Pediatr. 2017;184:19–25.
Fraser-Thomas J, Côté J. Youth sports: Implementing findings and moving forward with research. Athl Insight J. 2006;8:12–27.
Johnson LSM. Return to play guidelines cannot solve the football-related concussion problem. J Sch Health. 2012;82:180–5.
Tsushima WT, Geling O, Arnold M, Oshiro R. Are there subconcussive neuropsychological effects in youth sports? An exploratory study of high-and low-contact sports. Appl Neuropsychol Child. 2016;5:149–55.
Thomas DJ, Coxe K, Li H, Pommering TL, Young JA, Smith GA, et al. Length of recovery from sports-related concussions in pediatric patients treated at concussion clinics. Clin J Sport Med. 2018;28:56–63.
Benson BW, McIntosh AS, Maddocks D, Herring SA, Raftery M, Dvořák J. What are the most effective risk-reduction strategies in sport concussion? Br J Sports Med. 2013;47:321–6.
Asken BM, McCrea MA, Clugston JR, Snyder AR, Houck ZM, Bauer RM. “Playing through it”: delayed reporting and removal from athletic activity after concussion predicts prolonged recovery. J Athl Train. 2016;51:329–35.
Asken BM, Bauer RM, Guskiewicz KM, McCrea MA, Schmidt JD, Giza CC, et al. Immediate removal from activity after sport-related concussion is associated with shorter clinical recovery and less severe symptoms in collegiate student-athletes. Am J Sports Med. 2018;46:1465–74.
Guskiewicz KM, Marshall SW, Bailes J, McCrea M, Cantu RC, Randolph C, et al. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery. 2005;57:719–26.
Kiraly MA, Kiraly SJ. Traumatic brain injury and delayed sequelae: a review—traumatic brain injury and mild traumatic brain injury (concussion) are precursors to later-onset brain disorders, including early-onset dementia. Sci World J. 2007;7:1768–76.
McAllister T, McCrea M. Long-term cognitive and neuropsychiatric consequences of repetitive concussion and head-impact exposure. J Athl Train. 2017;52:309–17.
Sariaslan A, Sharp DJ, D’Onofrio BM, Larsson H, Fazel S. Long-term outcomes associated with traumatic brain injury in childhood and adolescence: a nationwide Swedish cohort study of a wide range of medical and social outcomes. PLoS Med. 2016;13:e1002103.
Broshek DK, Kaushik T, Freeman JR, Erlanger D, Webbe F, Barth JT. Sex differences in outcome following sports-related concussion. J Neurosurg. 2005;102:856–63.
Covassin T, Elbin RJ, Harris W, Parker T, Kontos A. The role of age and sex in symptoms, neurocognitive performance, and postural stability in athletes after concussion. Am J Sports Med. 2012;40:1303–12.
Master CL, Katz BP, Arbogast KB, McCrea MA, McAllister TW, Pasquina PF, et al. Differences in sport-related concussion for female and male athletes in comparable collegiate sports: a study from the NCAA-DoD Concussion Assessment, Research and Education (CARE) Consortium. Br J Sports Med [Internet]. 2020 [cited 2021 Aug 9]; https://bjsm.bmj.com/content/early/2020/12/20/bjsports-2020-103316
Caccese JB, Eckner JT, Franco-MacKendrick L, Hazzard JB, Ni M, Broglio SP, et al. Clinical reaction-time performance factors in healthy collegiate athletes. J Athl Train. 2020;55:601–7.
Collins MW, Grindel SH, Lovell MR, Dede DE, Moser DJ, Phalin BR, et al. Relationship between concussion and neuropsychological performance in college football players. JAMA. 1999;282:964–70.
Boyd RW, Lindo EG, Weeks LD, McLemore MR. On racism: a new standard for publishing on racial health inequities [Internet]. 2020 [cited 2021 Aug 9]. https://www.healthaffairs.org/do/https://doi.org/10.1377/hblog20200630.939347/full/
Iverson GL, Silverberg ND, Mannix R, Maxwell BA, Atkins JE, Zafonte R, et al. Factors associated with concussion-like symptom reporting in high school athletes. JAMA Pediatr. 2015;169:1132–40.
Caccese JB, Iverson GL, Hunzinger KJ, Asken BM, Clugston JR, Cameron KL, et al. Factors associated with symptom reporting in US Service Academy cadets and NCAA student athletes without concussion: findings from the CARE Consortium. Sports Med. 2021;51:1087–105.
Elbin RJ, Kontos AP, Kegel N, Johnson E, Burkhart S, Schatz P. Individual and combined effects of LD and ADHD on computerized neurocognitive concussion test performance: evidence for separate norms. Arch Clin Neuropsychol. 2013;28:476–84.
Brinkley A, McDermott H, Munir F. What benefits does team sport hold for the workplace? A systematic review. J Sports Sci Routledge. 2017;35:136–48.
Nixdorf I, Frank R, Hautzinger M, Beckmann J. Prevalence of Depressive Symptoms and Correlating Variables Among German Elite Athletes. J Clin Sport Psychol. Human Kinetics, Inc.; 2013;7:313–26.
Stone AA, Bachrach CA, Jobe JB, Kurtzman HS, Cain VS. The science of self-report: implications for research and practice. Psychology Press; 1999.
Zuckerman SL, Lee YM, Odom MJ, Solomon GS, Forbes JA, Sills AK. Recovery from sports-related concussion: days to return to neurocognitive baseline in adolescents versus young adults. Surg Neurol Int. 2012;3:130.
Crowe LM, Catroppa C, Babl FE, Rosenfeld JV, Anderson V. Timing of traumatic brain injury in childhood and intellectual outcome. J Pediatr Psychol. 2012;37:745–54.
Babcock L, Byczkowski T, Wade SL, Ho M, Mookerjee S, Bazarian JJ. Predicting postconcussion syndrome after mild traumatic brain injury in children and adolescents who present to the emergency department. JAMA Pediatr. 2013;167:156–61.
Moser RS, Davis GA, Schatz P. The age variable in childhood concussion management: a systematic review. Arch Clin Neuropsychol. 2018;33:417–26.
Acknowledgements
Contributing CARE Consortium Investigators Include: April Marie (Reed) Hoy, MS, ATC (Azusa Pacific University); Darren Campbell, MD (Brigham Young University); Louise A. Kelly, PhD (California Lutheran University); John DiFiori, MD (Hospital for Special Surgery, National Basketball Association); Justus D. Ortega, PhD (Humboldt State University); Nicholas Port, PhD (Indiana University); Margot Putukian MD (Major League Soccer); T. Dianne Langford, PhD and Jane McDevitt, PhD, ATC, CSCS (Temple University); Christopher C. Giza, MD (University of California, Los Angeles); Holly J. Benjamin MD (University of Chicago); Thomas W. Kaminski, PhD, ATC (University of Delaware); James R. Clugston, MD, MS (University of Florida); Joseph B. Hazzard, Jr., ATC (University of Houston-Clear Lake); Patrick G. O’Donnell, MHA (University of Massachusetts Memorial Medical Center); Luis A Feigenbaum, PT, DPT, ATC (University of Miami); James T. Eckner, MD, MS (University of Michigan); Jason P. Mihalik, PhD, CAT(C), ATC (University of North Carolina at Chapel Hill); Christina L. Master, MD (University of Pennsylvania); Anthony P. Kontos, PhD and Michael Collins, PhD (University of Pittsburgh Medical Center); Sara P.O. Chrisman, MD, MPH (University of Washington); Alison Brooks, MD, MPH (University of Wisconsin-Madison); Jonathan Jackson, MD and Gerald McGinty, PT, DPT (United States Air Force Academy); Carlos Estevez, DPT, OCS, ECS (United States Coast Guard Academy); Kenneth L. Cameron, PhD, MPH, ATC (United States Military Academy); Adam Susmarski, DO (United States Naval Academy); Christopher M. Miles, MD (Wake Forest University); Laura Lintner DO (Winston-Salem University).
Author information
Authors and Affiliations
Consortia
Contributions
JNM carried out analyses and interpretation of data, drafted the initial manuscript, reviewed and revised the manuscript for important intellectual content, approved the final version of the manuscript, and agrees to be accountable for all aspects of the work. JPH conceptualized and designed the study, interpreted the data, reviewed and revised the manuscript for important intellectual content, approved the final version of the manuscript, and agrees to be accountable for all aspects of the work. TAB and JDS conceptualized and designed the study, reviewed and revised the manuscript for important intellectual content, approved the final version of the manuscript, and agree to be accountable for all aspects of the work. SPB, TWM, MM, and PFP conceptualized and designed the CARE Consortium, received funding for the CARE Consortium, reviewed and revised the manuscript for important intellectual content, approved the final version of the manuscript, and agree to be accountable for all aspects of the work. JBC conceptualized and designed the study, interpreted the data, reviewed and revised the manuscript for important intellectual content, approved the final version of the manuscript, and agrees to be accountable for all aspects of the work. Named authors and CARE Consortium Investigators contributed to data acquisition, reviewed and revised the manuscript for important intellectual content, approved the final manuscript, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
All of the authors declare that they have no conflicts of interest to disclose.
Funding
Data collection and sharing for this project was conducted with support from the National Collegiate Athletic Association (NCAA) and the Department of Defense (DOD). The US Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702–5014 is the awarding and administering acquisition office. This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs, through the Combat Casualty Care Research Program, endorsed by the Department of Defense, through the Joint Program Committee 6/ Combat Casualty Care Research Program – Psychological Health and Traumatic Brain Injury Program under Award No. W81XWH1420151. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the Department of Defense. This work was supported by the National Institute on Aging (NIA) of the National Institutes of Health (NIH) R01AG058822 (to JPH), and The Ohio State University Discovery Themes Chronic Brain Injury Initiative (JPH and JBC). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Availability of data
The CARE Consortium dataset used in the present study is available in the FITBIR repository (https://fitbir.nih.gov/).
Ethics approval
The local IRB at each performance site, as well as the US Army Medical Research and Materiel Command Human Research Protection Office, reviewed and approved all study procedures. This study was performed in accordance with the Declaration of Helsinki.
Consent to participate
All participants provided written informed consent prior to participation in this study.
Rights and permissions
About this article
Cite this article
Moody, J.N., Hayes, J.P., Buckley, T.A. et al. Age of First Concussion and Cognitive, Psychological, and Physical Outcomes in NCAA Collegiate Student Athletes. Sports Med 52, 2759–2773 (2022). https://doi.org/10.1007/s40279-022-01719-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-022-01719-7