Abstract
Background
The availability of increasingly advanced and expensive new health technologies puts considerable pressure on publicly financed healthcare systems. Decisions to not—or no longer—reimburse a health technology from public funding may become inevitable. Nonetheless, policymakers are often pressured to amend or revoke negative reimbursement decisions due to the public disagreement that typically follows such decisions. Public disagreement may be reinforced by the publication of pictures of individual patients in the media. Our aim was to assess the effect of depicting a patient affected by a negative reimbursement decision on public disagreement with the decision.
Methods
We conducted a discrete choice experiment in a representative sample of the public (n = 1008) in the Netherlands and assessed the likelihood of respondents’ disagreement with policymakers’ decision to not reimburse a new pharmaceutical for one of two patient groups. We presented a picture of one of the patients affected by the decision for one patient group and “no picture available” for the other group. The groups were described on the basis of patients’ age, health-related quality of life (HRQOL) and life expectancy (LE) before treatment, and HRQOL and LE gains from treatment. We applied random-intercept logit regression models to analyze the data.
Results
Our results indicate that respondents were more likely to disagree with the negative reimbursement decision when a picture of an affected patient was presented. Consistent with findings from other empirical studies, respondents were also more likely to disagree with the decision when patients were relatively young, had high levels of HRQOL and LE before treatment, and large LE gains from treatment.
Conclusions
This study provides evidence for the effect of depicting individual, affected patients on public disagreement with negative reimbursement decisions in healthcare. Policymakers would do well to be aware of this effect so that they can anticipate it and implement policies to mitigate associated risks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Decisions to not—or no longer—reimburse a health technology from public funding are sensitive and often followed by public disagreement, which may be influenced by the depiction of individual patients affected by such negative decisions in the media. |
This study shows that members of the public are indeed more likely to disagree with a negative reimbursement decision when seeing a picture of an affected patient, particularly when the patient is relatively young and healthy, and can gain many life years from treatment. |
Policymakers would do well to anticipate the effect of patient depiction in the media on public disagreement to avoid amending or revoking negative reimbursement decisions and mitigate the risk of inequalities in access to new health technologies between patient groups. |
1 Introduction
The demand for healthcare continues to rise because of aging populations, increased numbers of chronically ill in societies, and the availability of increasingly advanced and expensive new health technologies [1]. The rising demand for healthcare and resulting pressure on limited budgets jeopardizes the sustainability of publicly financed healthcare systems and risks the crowding out of other public expenditures, e.g., on education and public order and safety [2,3,4,5]. To curb expenditures, policymakers are increasingly confronted with the need to set priorities in the allocation of healthcare resources and the inevitability of decisions to not—or no longer—reimburse a health technology from public funding [6, 7].
In many countries, reimbursement decisions are informed on the basis of criteria relating to the necessity (e.g., specified in terms of the disease severity of patients [8,9,10]), effectiveness, cost-effectiveness, and budget effect of a health technology [11]. In the case that a health technology does not meet such predefined criteria (e.g., the incremental cost-effectiveness ratio of a pharmaceutical does not fall below the applied monetary threshold), or in the arguably less common case that a health technology does meet the criteria, the outcome of a reimbursement decision may be negative. In such a case, policymakers decide to not (yet) or no longer reimburse a health technology from public funding for all patients or to reimburse the technology only for a subgroup of patients for whom the technology is indicated [12].
To facilitate consistent and fair decision making, the outcomes of reimbursement decisions are commonly made public by policymakers alongside information on characteristics of the patient population and on the effectiveness, cost-effectiveness, and budget effect of the health technology [13]. Even though negative reimbursement decisions may increasingly be considered necessary and made by policymakers [14], such reimbursement decisions remain politically and societally sensitive and are often met with opposition from members of the public [15, 16]. Public opposition to such decision may be strengthened when the media report on these decisions by publishing the pictures and stories of—oftentimes—individual patients who are affected by the decision [15, 17]. While such opposition is understandable, it puts pressure on policymakers to amend or revoke a negative reimbursement decision [15, 16]. This would be in the interest of the patient (group) for whom the health technology is indicated. However, this could be detrimental to other patients bearing the (health) opportunity costs of reimbursement, and in the long term, pose a risk for the sustainability of the healthcare system and public at large.
Evidence indicates that members of the public have a stronger emotional response and urge to help someone in need when they can identify and mentally visualize that individual as compared with when that individual cannot be identified, and hence remains “statistical” [15, 18,19,20,21]. This relates to the well-established concept of the Rule of Rescue, which illustrates the tendency of the public to come to the aid of identifiable individuals in immediate peril [22, 23]. Evidence further indicates that members of the public prefer reimbursing health technologies for younger and more severely ill patients, and for patients who are expected to gain more health from treatment [24,25,26,27,28]. From this it can be inferred that public disagreement may be influenced by the publication of pictures of individual patients in the media who are not or no longer granted access to a health technology, and that disagreement may be even stronger when those patients are relatively young, more severely ill, and their health gains from treatment are large. While such evidence is currently lacking, gaining a better understanding of the role of pictures in shaping public opinion—especially in this era of social media and visual communication—may become increasingly important. Therefore, the aim of this study was to address this gap in the literature and examine the effect of depicting an individual patient, and of the age, disease severity, and health gains from treatment of the patients affected by a negative reimbursement decision in healthcare on public disagreement with the decision. The results of this study are of interest to those seeking to better understand public disagreement with negative reimbursement decisions in healthcare and to obtain insight into the effect of depicting an individual patient affected by the decision on this disagreement.
2 Methods
2.1 Sample
To meet the aim of our study, we designed a discrete choice experiment (DCE) that was administered online by Motivaction, a professional sampling agency located in the Netherlands, in June 2022. This agency recruited respondents from their online panel and quota sampled them to be representative of the public in terms of age (18–80 years), sex, and education level.
Respondents received a participation fee of 2.30 euros upon completion of the questionnaire, which they could save in a personal account or donate to charity. The Research Ethics Review Committee of the Erasmus School of Health Policy & Management assessed and waived ethical approval for this study (reference: ETH2122-0605).
2.2 Discrete Choice Experiment
We constructed a Bayesian D-efficient DCE with informed priors using Spotlight software [29]. We based the priors of the design for the pilot study on the empirical findings discussed in the Introduction section [15, 18, 19, 25], indicating that respondents were more likely to disagree with a negative reimbursement decision when one of the patients affected by the decision was depicted (by means of presenting a picture of an individual patient) and when patients were younger, more severely ill, and gained more health from. We optimized the design for the main study using priors based on the results of the pilot study. Table S1.1 (Supplementary Material S1) presents an overview of the applied priors.
The DCE design consisted of 120 choice tasks, divided into 10 blocks, to one of which respondents were randomly assigned. Respondents completed a series of 12 choice tasks (in random order) in which we explained that two new pharmaceuticals had become available for two groups of 100 patients (labeled patient group A and B). We (randomly) presented a picture of one of the patients for either group A or B and the text “no picture available” for the other group. The picture was consistently positioned left or right (i.e., for patient group A or B, respectively) for individual respondents to reduce the cognitive burden of completing the choice tasks for respondents. The pictures were selected from Microsoft 365 Free Stock Images on the basis of the criteria that they were as similar (e.g., in terms of the facial expressions of the patients) and neutral (e.g., patients were not depicted in a hospital setting) as deemed possible, within as well as between the different age groups of the patients. The age of the patient in the picture corresponded with the age of the respective patient group (i.e., 10, 40, or 70 years) and was randomly selected from a group of 18 pictures (6 pictures per age group) that were equally distributed across sex and ethnicities. Table S1.2 (Supplementary Material S1) presents an overview of the pictures. Note that we did not obtain ethical approval for examining the effect of the sex and ethnicity of the depicted patients on respondents’ disagreement with the negative reimbursement decisions.
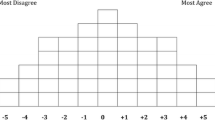
The patient groups were further described (in writing) on the basis of their age, disease severity [i.e., health-related quality of life (HRQOL) and life expectancy (LE) before treatment], HRQOL and LE gains from treatment, and the costs of their treatment. The latter amounted to a total of 200,000 euros per patient, which we used to calculate and present the cost-effectiveness (i.e., defined as “costs per healthy life year gained”) of the new pharmaceuticals and the opportunity costs of their reimbursement (i.e., defined as “expenditure avoided, the euros saved can be spent for treating other patients” in accordance with the definition used in a summary report on reimbursement decisions published by the National Health Care Institute (ZIN) in the Netherlands [30]). We explained to respondents that the healthcare budget was insufficient for reimbursing the new pharmaceutical for both patient groups and that policymakers had decided to not reimburse the pharmaceutical for patient group A (or B, randomly selected). We then asked respondents to indicate whether they agreed with the decision of policymakers to not reimburse the pharmaceutical for patient group A (or B) or whether they believed that the pharmaceutical should not be reimbursed for patient group B (or A)—forcing respondents to clearly express their disagreement. Figure 1 presents an example choice task as presented in version A of the questionnaire.
Before conducting the analyses, we formulated the hypotheses that respondents would be more likely to disagree with the policymakers’ decision to not reimburse the pharmaceutical for a specific patient group in case we presented a picture of a patient from that patient group and—in line with related empirical research (e.g., [25, 26, 28]—when the patients were relatively young, had low levels of HRQOL and LE before treatment, and large HRQOL and LE gains from treatment. Furthermore, we formulated the hypothesis that the effect of depicting an affected patient would be stronger when the patients were younger, had lower levels of HRQOL and LE before treatment, and larger HRQOL and LE gains from treatment. To our knowledge, evidence on the effect of respondents’ characteristics on their disagreement with negative reimbursement decisions is not yet available, which is why we explored the data without formulating any a priori hypothesis on this association.
We anticipated that (at least some) respondents might disagree with the negative reimbursement decision—regardless of whether this concerned patient group A or B—and would in fact prefer to reimburse the pharmaceuticals for both patient groups. To reduce the likelihood that such preferences influenced our results (e.g., by way of protest answers), we explained to respondents that we appreciated this preference and that they could leave a comment (on this or anything else) after completing the choice tasks in which they were forced to make a choice for not reimbursing the new pharmaceutical for one of the patient groups.
2.3 Attributes and Levels
We selected attributes concerning patients’ age, HRQOL and LE before treatment, and HRQOL and LE gains from treatment. This selection was based on the results of an informal review of the empirical literature on public preferences for reimbursing health technologies on the basis of patients’ age, disease severity, and the size and type of health gains discussed in the Introduction section [24,25,26,27,28]. HRQOL was measured on a visual analogue scale (VAS) ranging from 0 “worst health you can imagine” to 100 “best health you can imagine” and LE was measured in years. We determined the range and levels of the attributes on the basis of the criteria [31]: (i) that the differences in levels could be distinguished by respondents and (ii) that the levels aligned with those commonly used in related empirical studies. The latter would enable us to compare our results with those of (at least some of) the reviewed studies. For reasons of clarity, we also presented the healthy life years gained from treatment and the costs of treatment as attributes in the choice tasks, which we calculated on the basis of the levels of the relevant attributes. In Fig. 1, the 12 healthy life years from treatment gained by patients in group A was, for example, calculated as ((20 points HRQOL gains from treatment × 10 LE gains from treatment) + ((20 points HRQOL gains from treatment + 80 points HRQOL before treatment) × 10 LE gains from treatment)) / 100. The costs of 333,000 euros per healthy life year gained was calculated as ((200,000 euros × 100 patients × 10 LE before treatment) + 10 LE gains from treatment) / (12 healthy life years × 100 patients), rounded to the nearest 1000 euros. Note that we excluded these attributes from the analysis to avoid multicollinearity (Table 1).
2.4 Questionnaire
The questionnaire consisted of three parts. In part one, we informed respondents about the aim of the study and asked them to give consent for using their data for research purposes. We explained that they could withdraw from the study at any moment, at which time their data would be discarded. We then asked respondents about their age, sex, and education level for sampling purposes and about their health insurance premium, HRQOL “today,” and about what they considered best for themselves and the public in the Netherlands in terms of the coverage and premium of the mandatory health insurance (answer options: they should stay the same, increase, or decrease) for sensitizing purposes. We then explicated the task instruction to respondents and introduced them in three steps to the attributes (including the healthy life years gains and opportunity costs of reimbursement), levels, and choice tasks used in the second part of the questionnaire, the clarity of which we assessed on a 7-point Likert scale (ranging from 1 “very unclear” to 7 “very clear”). We included a practice choice task in each step that built up in complexity to the choice tasks that respondents would complete in the DCE.
In part two, we randomly assigned respondents to one of four DCE versions (labelled A–D). The data obtained in versions A and B was used to meet the aim of the current study. The data obtained in versions C and D was used to meet a different aim, on which we report elsewhere [32]. Versions A and B of the questionnaire were identical, except for the way in which we specified the costs of treatment in the choice tasks. In version A, we presented the costs in terms of the cost-effectiveness of the pharmaceuticals (e.g., specified as “330,000 euros per healthy life year gained” for patient group A in Fig. 1). In version B, we presented the costs in terms of the opportunity costs associated with reimbursement (e.g., specified as “costs of 330,000 euros avoided, this amount can be spent on other patients” for patient group A, assuming the same costs as in Fig. 1). In each version, we asked respondents to complete 12 choice tasks, and subsequently, to leave a comment if so desired. In part three, respondents were asked about their sociodemographic characteristics.
2.5 Data Collection
Prior to conducting the main study, we conducted a pilot study to pretest the questionnaire [31, 33]. More specifically, we collected pilot data (n = 406) to assess the clarity of the task instruction and of the attributes and levels, and choice tasks on a 7-point Likert scale (ranging from 1 “very unclear” to 7 “very clear”) as presented in the four (i.e., A–D) versions of the questionnaire. Table S1.1 (Supplementary Material S1) presents the number of respondents per questionnaire version. The mean (SD) clarity scores were 5.8 (1.1) for the instruction and 5.5 (1.3) for the attributes, levels, and choice tasks, which was considered satisfactory. As such, we did not modify the questionnaire for the main data collection (n = 1628) and merged the pilot and main data (total sample n = 2034) before conducting the analyses. Note that we used data obtained from a subsample (n = 1008) to meet the aim of the current study (see Sect. 2.4).
2.6 Data Analysis
Before assessing the effect of depicting one of the patients affected by policymakers’ decision to not reimburse a new pharmaceutical for patient group A or B on respondents’ disagreement with the decision, we calculated the proportions of (in total 12,096) choice tasks in which respondents (dis)agreed with the decision and of respondents who consistently (dis)agreed with the decision in all choice tasks. We used random-intercept logit regression models to analyze the choice data. These models accounted for the likelihood that choices were nested and that some respondents could be more inclined to (dis)agree with negative reimbursement decisions than others, independent of the picture, attributes, and levels presented in the choice tasks. Note that random-intercept models are a specific type of random-effect models where only the intercept is modeled as a random effect, while the coefficients of the predictor variables are modeled as fixed effects. We used a normal distribution for the random intercept and categorical variables for coding the attribute levels and respondent characteristics.
We first ran six models to examine the main and interaction effects of the choice–task characteristics on respondents’ disagreement with policymakers’ decision to not reimburse the new pharmaceutical for one of the patient groups. By running model 1, we estimated the main effects of depicting one of the patients affected by the negative reimbursement decision by means of presenting their picture (0, no; 1, yes) and of the attributes (i.e., patients’ age, their HRQOL and LE before treatment, and their HRQOL and LE gains from treatment) and levels on respondents’ disagreement. By running models 2–6, we successively estimated the interaction effects of depicting one of the affected patients and patients’ age, their HRQOL and LE before treatment, and their HRQOL and LE gains from treatment on respondents’ disagreement. We then ran 7 models to examine the main and interaction effects of the choice–task and respondents’ characteristics on their disagreement with the negative reimbursement decision. By running model 7, we estimated the main effects of depicting one of the patients, the attributes and levels, and respondents’ age, sex, education level, household income (per month, before tax), having children (no/yes), and HRQOL on their disagreement. Finally, by running models 8–13, we successively estimated the interaction effects between depicting an affected patient and the abovementioned respondents’ characteristics on their disagreement, while controlling for the attributes and levels. We furthermore controlled for the presentation of the picture (i.e., positioned left or right for patient group A or B, respectively) and the treatment costs (i.e., presented as cost-effectiveness or opportunity costs in version A or B of the questionnaire, respectively) in all models.
After running models 1–13, we further explored the choice data by estimating the main and interaction effects of depicting one of the affected patients and patients’ age and their HRQOL and LE endpoint after treatment (calculated as ‘HRQOL before treatment + HRQOL gains from treatment’ and ‘patients’ age + LE before treatment + LE gains from treatment’, respectively), as well as the interaction effect between HRQOL and LE gains from treatment on respondents’ disagreement. We assessed the robustness of our results by repeating the analyses excluding respondents who (i) reported a clarity score < 4 for the introduction to the attributes, levels, and choice tasks; (ii) completed the 12 choice tasks in less than 34 s or more than 17.3 min (i.e., the completion times of the quickest and slowest 5.0% of respondents, respectively) on the basis of the distribution of completion times; and (iii) left a comment saying that the pharmaceuticals should actually be reimbursed for neither or both patient groups, which we identified and clustered using inductive coding methods.
We conducted the analyses using Stata 18.0 (Stata Corp LP, College station, Texas).
3 Results
Table 2 presents the descriptive statistics of the sample (n = 1008) and of the public in the Netherlands for age, sex, and education level. The statistics indicate that the distribution of age, sex, and education level differed slightly between our sample and the public as members of the public who were 31–64 years old, female, and lower educated were overrepresented.
Of the respondents, 502 (49.8%) completed version A and 506 (50.2%) completed version B of the questionnaire. The mean (SD) clarity score for the task instruction was 5.8 (1.1) on the 7-point Likert scale and 24 (2.4%) reported a score < 4. For the introduction to the attributes, levels, and choice tasks, the mean (SD) clarity score was 5.5 (1.2) and 59 (5.9%) reported a score < 4 on the 7-point Likert scale. On average, respondents completed the 12 choice tasks in 13.6 min. Of the respondents, 303 (30.2%) left a comment after completing the choice tasks. A total of 61 respondents (6.0%) left a comment saying that the pharmaceuticals should be reimbursed for both (n = 50) or for neither (n = 11) of the patient groups. Table S2.1 (Supplementary Material S2) presents an overview and description of the clusters of comments left by respondents. Respondents disagreed with the negative reimbursement decision of policymakers in 73.2% of the choice tasks and agreed with the decision in the remaining 26.8%. Of the respondents, 8 (0.8%) disagreed and 0 (0.0%) agreed consistently with policymakers’ decision in all 12 choice tasks (equally distributed between versions A and B).
Table 3 presents the results of regression model 1–6 on the basis of which we examined the effect of choice–task characteristics on respondents’ disagreement with policymakers’ decision to not reimburse the new pharmaceutical for one of the two patient groups. The results of model 1 indicate that respondents were more likely to disagree with policymakers’ decision when we presented a picture of one of the patients affected by the decision as compared with being shown the text “no picture available” for that patient group. The results of model 1 further indicate that respondents were more likely to disagree when patients were 10 years old as compared with being 40 or 70 years old, had a HRQOL before treatment of 60 or 80 points as compared with 20 or 40 points, had a LE before treatment of 5, 10, or 15 years as compared with 1 year, and had a LE gain from treatment of 5, 10, or 15 years as compared with 1 year. The results of models 2–6 further indicate that the effect of depicting an affected patient on respondents’ likelihood to disagree with policymakers’ decision was dependent on the LE that patients gained from treatment (model 6). The effect of depicting an affected patient was greater when the patients gained 5 or 15 life years from treatment as compared with gaining 1 or 10 life years. The results from models 1–6 support the hypotheses that respondents would be more likely to disagree with the negative reimbursement decision in the case that a picture of one of the patients affected by the decision was presented and when patients were relatively young and LE gains from treatment were relatively large. However, they do not support the hypotheses that respondents would be more likely to disagree with the decision when HRQOL and LE before treatment were relatively low and HRQOL gains from treatment large.
Table 4 presents the results of regression model 7–13 on the basis of which we examined the effect of choice–task and respondents’ characteristics on their disagreement with policymakers’ decision. The results of model 7 indicate that respondents’ age, sex, education level, household income, whether they had children, and their HRQOL did not affect the likelihood of their disagreement with the decision. The results of models 8–13 provide insight into the interaction between being the presentation of a picture of one of the patients affected by the decision and respondents’ characteristics. The results of these models indicate that the effect of depicting an individual patient on respondents’ disagreement with the negative reimbursement decision was dependent on each of these characteristics. Respondents were more likely to disagree with the negative reimbursement decision in the case that a picture of an affected patient was presented when they were 31–64 or 65–80 years old as compared with 18–30 years old (model 8), female as compared with male (model 9), had a high education level as compared with a low or medium education level (model 10), had children as compared with having no children (model 11), had not specified their household income as compared with having a low, medium, or high income level (model 12), and had a HRQOL of 26–50, 51–75, or 76–100 points as compared with 0–25 points on the VAS (model 13).
Figure S3.1 (Supplementary Material S3) shows that respondents are more likely to disagree with the negative reimbursement decision when patients’ HRQOL and LE end point after treatment is relatively higher. The latter effect is greatest when patients’ are 10 years old. Figure S3.2 further shows that the effect of 20 points HRQOL from treatment is greater when patients’ LE gains from treatment are larger. The sensitivity analyses indicted that our results were robust. Tables S3.1 and S3.2 (Supplementary Material S3) presents the respective regression results. Note that for convenience only the main effects of choice–task and respondents’ characteristics on their disagreement with the negative reimbursement decision are presented.
4 Discussion
Our aim was to examine the effect of depicting an individual patient, and of the age, disease severity, and health gains from treatment of the patients affected by a negative reimbursement decision in healthcare on public disagreement with the decision. The main findings of this study indicate that respondents were more likely to disagree with the decision in case a picture of an affected patient was presented and that they were more likely to disagree with the decision when the affected patients were relatively young, had relatively high levels of HRQOL and LE before treatment, and relatively large LE gains from treatment. While this combination of patient characteristics and treatment outcomes may not seem realistic at first glance, it is, unfortunately, not uncommon. This is the case, for example, in early-stage cancer or rare genetic disorders in young patients who, apart from their condition, are otherwise healthy. We further found that the effect of presenting a picture on the likelihood of disagreement with the decision was stronger when respondents were 31 years or older, female, higher educated, had children, did not specify their household income, and a HRQOL of 26 points or more on the 0–100 VAS.
These findings generally support the predetermined hypotheses. However, it seems fair to note that the finding that respondents were more likely to disagree when patients’ HRQOL and LE before treatment were relatively high was counterintuitive, especially because evidence indicates that members of the public have a stronger emotional response and urge to help someone in need [18, 19], and someone’s need for health(care) may logically depend on the severity of their disease, and hence on their HRQOL and LE before treatment. This dependency is increasingly incorporated in decision-making frameworks used for informing reimbursement decisions in healthcare. For example, the decision criterion ‘necessity of care’ is defined in terms of disease severity and operationalized as patients’ proportional shortfall of quality-adjusted life-years (QALYs) in the Netherlands [9, 34].
The main strength of this study lies in the innovative approach to include pictures of patients in a DCE. To our knowledge, this is the first study to apply such a design to examine the effect of depicting individual, affected patients on public disagreement with negative reimbursement decisions in healthcare. As a result, we are limited in our ability to directly compare our findings with those of others. Nonetheless, we can compare our findings with those of other studies who examined the effect of identifiability on healthcare decision-making more broadly. For example, our findings are generally in line with those of Kogut and Ritov who found that people were more willing to help a victim (i.e., “a child whose life is in danger”) who could be identified on the basis of a picture than a similar victim who could not be identified [35, 36]. Our findings are furthermore in line with those of Västfjäll et al. who found that financial donations to a humanitarian aid organization were higher in the case that charity requests included a picture of a child threatened by severe hunger or even starvation [37]. Here, we would also like to highlight the findings of Wiss et al., who found that people were less willing to reimburse treatment for a child with a rare disease than for a child with a common disease, both of whom could be identified on the basis of a picture [38]. We appreciate that the findings of Wiss et al. [38] are of a different order than our findings. Nonetheless, we deemed it relevant to mention their study considering that they, like us, provide insight into the potential interaction between depicting a patient by means of a picture and information on other factors, e.g., relating to characteristics of the disease (such as it being common or rare) or treatment (such as the type of health gains).
Another strength of this study lies in the selection of pictures of individuals with a neutral expression against a neutral background to reduce the potential bias of influencing factors related to characteristics of the patients, disease, or treatment that were not included in the choice tasks. Note, however, that pictures of individual patients in the media may not always be neutral representations. For example, patients could be depicted who are in a hospital setting or visibly suffering from some disease. Further research is warranted to examine the additional effect of depicting patients in different ways on public disagreement. We further reduced the potential bias of influencing factors related to the sex and race of the patients by balancing these characteristics among the selected pictures and presenting a random selection from the set of age-specific pictures in the choice tasks.
Despite these strengths, some limitations must be mentioned. A first limitation concerns the hypothetical context in which we asked respondents to indicate whether they (dis)agreed with the negative reimbursement decisions. We acknowledge that this limits us in our ability to generalize the finding that respondents disagreed with the decision in the majority of choice tasks (i.e., 72.3%) to real-life situations. Nonetheless, on the basis of our findings it seems evident that depicting a patient affected by the decision may increase that likelihood. A second limitation that is also concerned with the generalisability of our findings results from the limited representativeness of our sample in terms of age, sex, and education level of the public in the Netherlands. Notably, members of the public aged 18–30 years, those who were male, and those who had a higher level of education were underrepresented in our sample. As compared with respondents with a low or medium education level, those with a high education level were less likely to disagree with the negative reimbursement decision when the 5% of respondents with the slowest and fastest completion times were excluded (see Table S3.2 in Supplementary Material S3). As such, further research is warranted to examine the relationship between respondents’ education level and their influenceability by the depiction of affected patients in the media. A final limitation concerns the relatively simple choice tasks applied to examine respondents’ (dis)agreement with negative reimbursement decisions. The choice tasks enabled us to meet the aim of our study while keeping the cognitive burden limited for respondents. Further research is warranted to examine the relationship between depicting a patient and public disagreement with negative reimbursement scenarios in more complex choice tasks that include information on, for example, risks of adverse events and uncertainty about the effectiveness of the technology that is denied reimbursement. In addition, the low McFadden pseudo R-squared statistic and the high Akaike information criterion (AIC) and Bayesian information criterion (BIC) statistics suggest that the goodness of fit of our models is low. Although this may be considered a limitation of our study, we would like to mention that this is not uncommon in DCE studies and could be explained by the complexity of modeling individual choice behavior [39]. We furthermore like to mention that, despite these statistics, our models successfully aided in achieving the aims of our study. Specifically, they provided evidence of the statistically significant effect of depicting a patient affected by a negative reimbursement decision on public disagreement with that decision.
Our study provides evidence on the effect of depicting a patient affected by a negative reimbursement decision on public disagreement with such decisions in healthcare. Public disagreement puts pressure on policymakers to amend or revoke negative reimbursement decisions [15, 16]. This would be in the interest of the patients affected by the decision; however, it could be detrimental to the patients bearing the (health) opportunity costs of reimbursement and the public at large. Indeed, amending or revoking a negative reimbursement decisions may pose a risk to the sustainability of the healthcare system and make negative reimbursement decisions inevitable for future generations. This may further increase inequalities in access to new health technologies between different patient groups; for example, in the case that health technologies are reimbursed for patient groups that receive media attention and not for patient groups that are not noticed by the public. Therefore, it is important that policymakers in healthcare recognize these dynamics. By doing so, they can proactively devise and implement strategies that balance the short-term needs of patients with the long-term sustainability of the healthcare system, thereby mitigating the risks of increased inequalities and ensuring a more equitable allocation of healthcare resources.
5 Conclusions
The results of this study indicate that depicting an individual patient who is affected by a negative reimbursement decision may increase the disagreement with the decision among members of the public in the Netherlands. Their disagreement may even be more likely when the depicted patient gains much LE from treatment, and when the patient group affected by the negative reimbursement decision is relatively young and healthy. Policymakers would do well to be aware of this effect so that they can anticipate it and implement policies to mitigate associated risks.
References
Paulden M. A framework for the fair pricing of medicines. Pharmacoeconomics. 2024;42(2):145–64.
Reckers-Droog VT, van Exel NJA, Brouwer WBF. Looking back and moving forward: on the application of proportional shortfall in healthcare priority setting in the Netherlands. Health Policy (New York). 2018;122(6):621–9.
Hicks LL. Making hard choices. J Leg Med. 2011;32(1):27–50.
Pammolli F, Riccaboni M, Magazzini L. The sustainability of European health care systems: beyond income and aging. Eur J Health Econ. 2012;13(5):623–34.
Tran LD, Zimmerman FJ, Fielding JE. Public health and the economy could be served by reallocating medical expenditures to social programs. SSM Population Health. 2017;1(3):185–91.
Stadhouders N, Koolman X, Tanke M, Maarse H, Jeurissen P. Policy options to contain healthcare costs: a review and classification. Health Policy (New York). 2016;120(5):486–94. https://doi.org/10.1016/j.healthpol.2016.03.007.
Makady A, van Acker S, Nijmeijer H, de Boer A, Hillege H, Klungel O, et al. Conditional financing of drugs in the Netherlands: past, present, and future—results from stakeholder interviews. Value Health. 2019;22(4):399–407.
Norwegian Ministry of Health and Care Services. Principles for priority setting in health care. 2017;1–69. Available from: https://www.regjeringen.no/contentassets/439a420e01914a18b21f351143ccc6af/en-gb/pdfs/stm201520160034000engpdfs.pdf
Zorginstituut Nederland. Ziektelast in de praktijk. Diemen; 2018.
Institute for Health N, Excellence C. NICE health technology evaluations: the manual Process and methods. 2022. Available from: www.nice.org.uk/process/pmg36
Chugh Y, De Francesco M, Prinja S. Systematic literature review of guidelines on budget impact analysis for health technology assessment. Appl Health Econ Health Policy. 2021;19(6):825–38.
Parkinson B, Sermet C, Clement F, Crausaz S, Godman B, Sarah Garner kise, et al. Disinvestment and value-based purchasing strategies for pharmaceuticals: an international review.
Daniels N. Just health: meeting health needs fairly. Cambridge University Press; 2007.
Schurer M, Matthijsse SM, Vossen CY, van Keep M, Horscroft J, Chapman AM, et al. Varying willingness to pay based on severity of illness: impact on health technology assessment outcomes of inpatient and outpatient drug therapies in the Netherlands. Value Health. 2022;25(1):91–103. https://doi.org/10.1016/j.jval.2021.08.003.
Pinho M, Dias CE. Can mass media be an obstacle to rationing decisions? A case report from Portugal. Int J Health Govern. 2020;25(1):3–11.
Wang DL. Courts and health care rationing: the case of the Brazilian Federal Supreme Court. Health Econ Policy Law. 2013;8(1):75–93.
Burgoyne CB. Distributive justice and rationing in the NHS: framing effects in press coverage of a controversial decision. J Community Appl Soc Psychol. 1997;7(2):119–36.
Hope T. Rationing and life-saving treatments: should identifiable patients have higher priority? J Med Ethics. 2001;27(3):179–85.
Small DA, Loewenstein G. Helping a victim or helping the victim: altruism and identifiability. J Risk Uncertainty. 2003; 26.
Mechanic D. Muddling through elegantly: finding the proper balance in rationing. Health Aff. 1997;16(5):83–92.
Schelling TC. The life you save may be your own. In: Chase Samuel B, editor. Problems in Public Expenditure Analysis Studies of Government Finance. Washington: Brookings Institution; 1968. p. 127–62.
Jonsen AR. III. THE HEALTH CARE SYSTEM 3. Bentham in a box: technology assessment and health care allocation.
Cookson R, McCabe C, Tsuchiya A. Public healthcare resource allocation and the Rule of Rescue. J Med Ethics. 2008;34:540–4.
Reckers-Droog V, van Exel J, Brouwer W. Willingness to pay for health-related quality of life gains in relation to disease severity and the age of patients. Value Health. 2021;24(8):1182–92.
Reckers-Droog V, van Exel J, Brouwer W. Equity weights for priority setting in healthcare: severity, age, or both? Value Health. 2019;22(12):1441–9.
Attema AE, Brouwer WBF, Pinto-Prades JL. Reference-dependent age weighting of quality-adjusted life years. Health Econ (United Kingdom). 2022;31(12):2515–36.
Lancsar E, Gu Y, Gyrd-Hansen D, Butler J, Ratcliffe J, Bulfone L, et al. The relative value of different QALY types. J Health Econ. 2020;1:70.
van de Wetering L, van Exel J, Bobinac A, Brouwer WBF. Valuing QALYs in relation to equity considerations using a discrete choice experiment. Pharmacoeconomics. 2015;33(12):1289–300.
Jonker M. Spotlight. 2022 [cited 2024 Jan 19]. Available from: www.spotlight-software.com
Zorginstituut Nederland. Werken aan kwaliteit, toegankelijkheid en betaalbaarheid: Een overzicht van de adviezen en standpunten van Zorginstituut Nederland - 2018 en 2019. Diemen; 2020. Available from: www.zorginstituutnederland.nl
Mühlbacher AC, de Bekker-Grob EW, Rivero-Arias O, Levitan B, Vass C. How to present a decision object in health preference research: attributes and levels, the decision model, and the descriptive framework. Patient. 2024. https://doi.org/10.1007/s40271-024-00673-y.
van Don M, de Bruijn A, Knies S, Brouwer W, Reckers-Droog V. How do economic arguments influence public disagreement with negative reimbursement decisions in healthcare. 2024.
Campoamor NB, Guerrini CJ, Brooks WB, Bridges JFP, Crossnohere NL. Pretesting discrete-choice experiments: a guide for researchers. Patient. 2024;17(2):109–20.
Zorginstituut Nederland. Cost-effectiveness in practice. Diemen; 2015.
Kogut T, Ritov I. The “identified victim” effect: an identified group, or just a single individual? J Behav Decis Making. 2005;18:157–67 (John Wiley and Sons Ltd).
Kogut T, Ritov I. The singularity effect of identified victims in separate and joint evaluations. Organ Behav Hum Decis Process. 2005;97(2):106–16.
Västfjäll D, Slovic P, Mayorga M, Peters E. Compassion fade: Affect and charity are greatest for a single child in need. PLoS ONE. 2014;9(6): e100115.
Wiss J, Levin LÅ, Andersson D, Tinghög G. Prioritizing rare diseases: psychological effects influencing medical decision making. Value Health. 2014;17(7):A325–6.
Hauber AB, González JM, Groothuis-Oudshoorn CGM, Prior T, Marshall DA, Cunningham C, et al. Statistical methods for the analysis of discrete choice experiments: a report of the ISPOR Conjoint Analysis Good Research Practices Task Force. Value Health. 2016;19(4):300–15.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author Contributions
Anne de Bruijn, Mats van Don, Saskia Knies, Werner Brouwer, and Vivian Reckers-Droog were responsible for conceptualization; Anne de Bruijn and Vivian Reckers-Droog for formal analysis; Werner Brouwer and Vivian Reckers-Droog for funding acquisition; Anne de Bruijn, Mats van Don, and Vivian Reckers-Droogfor methodology; Vivian Reckers-Droog for project administration; Vivian Reckers-Droog for supervision; Anne de Bruijn, Mats van Don, Saskia Knies, Werner Brouwer, and Vivian Reckers-Droog for validation; Anne de Bruijn and Vivian Reckers-Droog for visualization; Anne de Bruijn and Vivian Reckers-Droog for writing—original draft preparation; and Anne de Bruijn, Mats van Don, Saskia Knies, Werner Brouwer, and Vivian Reckers-Droog for writing—review and editing.
Competing Interests
Ms. de Bruijn has nothing to disclose. Mr. van Don has nothing to disclose. Dr. Knies reports other from National Health Care Institute (ZIN) in the Netherlands during the conduct of the study. Dr. Brouwer reports grants from National Health Care Institute (ZIN) in the Netherlands during the conduct of the study and grants from National Health Care Institute (ZIN) in the Netherlands outside the submitted work. Dr. Reckers-Droog reports grants from National Health Care Institute (ZIN) in the Netherlands during the conduct of the study and grants from National Health Care Institute (ZIN) in the Netherlands outside the submitted work.
Funding
This study is part of a larger project examining public opposition to negative reimbursement decisions in healthcare and was funded by the National Health Care Institute (ZIN) in the Netherlands. The views expressed in this article are those of the authors.
Ethics Approval
The Research Ethics Review Committee of the Erasmus School of Health Policy & Management assessed and waived ethical approval for this study (reference: ETH2122-0605).
Data Availability
The dataset generated during and/or analyzed during the current study is available from the corresponding author on reasonable request.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
de Bruijn, A., van Don, M., Knies, S. et al. Examining the Effect of Depicting a Patient Affected by a Negative Reimbursement Decision in Healthcare on Public Disagreement with the Decision. PharmacoEconomics 42, 879–894 (2024). https://doi.org/10.1007/s40273-024-01386-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-024-01386-8