Abstract
Objective
Cabotegravir long-acting (CAB–LA) administered every 2 months was approved in the USA as pre-exposure prophylaxis (PrEP) for individuals at risk of acquiring human immunodeficiency virus (HIV)-1 infection based on the HIV Prevention Trials Network (HPTN) 083 and HPTN 084 clinical trials, which demonstrated superior reduction in HIV-1 acquisition compared with daily oral emtricitabine/tenofovir disoproxil fumarate (FTC/TDF) in men who have sex with men (MSM), transgender women (TGW), and cisgender women. A decision-analytic model was developed to assess the lifetime cost-effectiveness of initiating CAB–LA versus generic oral FTC/TDF for HIV PrEP in the USA from a healthcare sector perspective.
Methods
PrEP-eligible adults entered the Markov model receiving CAB–LA or FTC/TDF and could continue initial PrEP, transition to a second PrEP option, or discontinue PrEP over time. Efficacy was taken from the HPTN 083 and HPTN 084 clinical trials. Individuals who acquired HIV-1 infection incurred lifetime HIV-related costs, could transmit HIV onwards, and could develop PrEP-related resistance mutations. Input parameter values were obtained from public and published sources. Model outcomes were discounted at 3%.
Results
The model estimated that the CAB–LA pathway prevented 4.5 more primary and secondary HIV-1 infections per 100 PrEP users than the oral PrEP pathway, which yielded 0.2 fewer quality-adjusted life-years (QALYs) lost per person. Additional per-person lifetime costs were $9476 (2022 US dollars), resulting in an incremental cost-effectiveness ratio of $46,843 per QALY gained. Results remained consistent in sensitivity and scenario analyses, including in underserved populations with low oral PrEP usage.
Conclusions
Our analysis suggests that initiating CAB–LA for PrEP is cost-effective versus generic daily oral FTC/TDF for individuals at risk of acquiring HIV-1 infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This analysis found that initiating cabotegravir long-acting (CAB–LA) for pre-exposure prophylaxis (PrEP) represents a cost-effective approach to reducing primary and onward HIV-1 infections compared with initiating generic daily oral emtricitabine/tenofovir disoproxil fumarate (FTC/TDF) for adult men who have sex with men (MSM), transgender women, and cisgender women at risk of acquiring HIV-1 infection in the USA. |
Among cisgender women, African American/Black MSM, and individuals with low oral PrEP adherence or no current PrEP use, the CAB–LA pathway resulted in cost savings. |
CAB–LA may be an important tool to reduce new HIV-1 infections in the USA overall and in specific communities aligned with the Ending the HIV Epidemic initiative. |
1 Introduction
The human immunodeficiency virus (HIV) epidemic remains a persistent public health problem in the USA, particularly in underserved populations and regions. In 2019,Footnote 1 nearly 37,000 individuals were newly diagnosed with HIV in the USA, with 37% occurring among African American/Black individuals and 52% occurring in the Southern USA [1]. The US Department of Health and Human Services launched the Ending the HIV Epidemic (EHE) initiative in 2019 to reduce new HIV infections in the USA overall and in specific racial, ethnic, and geographic communities with the highest burden of new HIV infections via increased resources and support [2]. The EHE initiative has identified pre-exposure prophylaxis (PrEP) as a powerful tool to reduce HIV-1 infections among individuals at increased risk. Oral PrEP has been available in the USA since 2012, with two options currently approved [emtricitabine/tenofovir disoproxil fumarate (FTC/TDF) and emtricitabine/tenofovir alafenamide (FTC/TAF)]. Notably, FTC/TAF is not approved for individuals at risk of HIV acquisition from receptive vaginal sex [3]. For cisgender women, this leaves only FTC/TDF approved for use, but very high levels of adherence are required for effectiveness in preventing HIV acquisition [4, 5] and associated clinical findings have been inconsistent [6]. In general, oral PrEP requires a high level of adherence to be effective [6], and real-world evidence suggests this level of adherence is achieved by only a fraction of PrEP users [7]. Oral PrEP is also highly underutilized in the USA, with the Centers for Disease Control and Prevention (CDC) estimating that only 23% of eligible individuals were using PrEP in 2019 overall and that utilization was even more disparate in underserved populations, at only 8% of eligible African American/Black individuals, 14% of eligible Hispanic/Latino individuals, and 10% of eligible cisgender women [8].
Cabotegravir long-acting (CAB–LA) is an injectable PrEP option for administration every 2 months. Two large-scale, multinationalFootnote 2 studies, the HIV Prevention Trials Network (HPTN) 083 clinical trial in men who have sex with men (MSM) and transgender women (TGW) and the HPTN 084 clinical trial in cisgender women, assessed the efficacy and safety of CAB–LA. Notably, the HPTN 083 clinical trial included substantial representation of key populations disproportionately affected by HIV and currently underutilizing, and therefore receiving less benefit from, daily oral PrEP (50% African American/Black individuals among participating US sites, 12.5% TGW, and 67.5% individuals under the age of 30 years) [9]. The primary analyses of these trials found that CAB–LA reduced the occurrence of new HIV-1 infections by 66% among MSM and TGW (with similar results in key subgroups) and by 88% among cisgender women when compared with daily oral FTC/TDF, with both studies meeting a priori criteria for the establishment of superiority [9,10,11]. As a result of these findings, the blinded, randomized portions of both studies were stopped early for efficacy on the recommendation of independent Data Safety Monitoring Boards. Further testing revealed that 1 HIV-1 infection in the CAB–LA arm of each clinical trial was prevalent at baseline. In post hoc analyses that excluded these baseline infections, CAB–LA exhibited a 69% relative reduction in HIV acquisition compared with FTC/TDF in MSM and TGW and a 92% relative reduction in cisgender women [9,10,11]. CAB–LA for PrEP was approved in December 2021 in the USA for adults and adolescents weighing at least 35 kg and at risk of sexually acquired HIV-1 infection [11].
Because of the key role of PrEP in the EHE campaign, it is critical for decision-makers to understand the potential long-term health and economic outcomes associated with the available PrEP options. Branded FTC/TDF and FTC/TAF have both shown mixed cost-effectiveness results [12,13,14], while generic FTC/TDF has demonstrated cost-effectiveness versus no PrEP among MSM and TGW at risk in the USA [15]. CAB–LA demonstrated superior efficacy compared with FTC/TDF and extends effective PrEP access to cisgender women and individuals for whom optimal utilization of oral PrEP may be difficult. The potential cost-effectiveness of CAB–LA was examined in a limited analysis before its approval [15], and a full assessment is now needed. The objective of this analysis was to comprehensively estimate the costs, health outcomes, and cost-effectiveness of CAB–LA versus other PrEP options among eligible individuals in the USA.
2 Methods
2.1 Model Overview
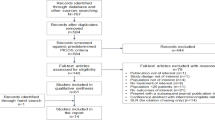
A decision-analytic model with a Markov structure and a 1-month cycle length was developed in Microsoft Excel to assess initiating PrEP with CAB–LA versus generic daily oral FTC/TDF (Fig. 1). The model used a lifetime time horizon to fully capture all costs and effects, as HIV-1 infection requires lifelong management. The modeled population included MSM, TGW, and cisgender women aged 18 years and older who are at an increased risk of acquiring HIV-1 infection. At the initiation of the model, individuals were assumed to experience this increased level of risk for a total of 5 years. This duration of increased risk was estimated by calibrating modeled lifetime risk of HIV acquisition without PrEP against US lifetime HIV-acquisition estimates [16]. Longer and shorter durations of risk were tested in the scenario analysis.
Individuals entered the model by initiating CAB–LA or generic daily oral FTC/TDF. Over time, individuals could continue receiving their initial PrEP option, transition to a second PrEP option, or discontinue PrEP. In the CAB–LA pathway, the second PrEP option for all individuals was generic daily oral FTC/TDF. In the oral PrEP pathway, the second PrEP option for MSM and TGW was daily oral FTC/TAF; cisgender women in the oral PrEP pathway did not have a second PrEP option because FTC/TAF is not approved for individuals at risk of HIV acquisition from receptive vaginal sex. While receiving PrEP, individuals were at a lower risk of acquiring HIV-1 infection than those not receiving PrEP, with protection levels dependent on their selected PrEP option and their PrEP adherence and persistence. Individuals receiving PrEP also completed ongoing monitoring visits and testing in accordance with CDC guidelines [6, 17,18,19], and those receiving CAB–LA could experience injection site reactions (ISRs) [9, 10, 20].
Individuals who acquired HIV-1 infection discontinued use of PrEP and transitioned to HIV-related care, including multiclass antiretroviral (ARV) treatment regimens, ongoing monitoring, and other related care, for the remainder of their lifetimes. Individuals with unsuppressed HIV-1 infection could also transmit HIV onwards or develop PrEP-related resistance mutations. Individuals who did not acquire HIV-1 infection during the 5-year duration of risk were assumed to incur no additional costs for the remainder of their lifetimes.
The analysis took a healthcare sector perspective and assessed costs and health outcomes for the eligible cohort over time. Input parameter values were obtained via a targeted review of public and published sources. The most recent relevant source was selected when multiple sources for an input were available. Modeled cost outcomes in 2022 US dollars included PrEP-related costs (e.g., drug acquisition, administration, monitoring, and adverse event management costs) and lifetime costs associated with new HIV-1 infections. Health outcomes included new primary and secondary HIV-1 infections and the associated losses in life expectancy and quality-adjusted life-years (QALYs). Average per-person costs and health outcomes were discounted at 3% per year, according to established US cost-effectiveness practice recommendations [21], and various incremental cost-effectiveness ratios (ICERs), such as the incremental cost per QALY gained, were then calculated to compare PrEP scenarios.
2.2 Modeled Population
The population entering the model included adults with increased risk of acquiring HIV-1 infection and eligible to receive PrEP [1]. The base-case analysis focused on PrEP-eligible populations aligned with the HPTN 083 and HPTN 084 study populations. The modeled distribution of MSM and TGW (HPTN 083) and cisgender women (HPTN 084) is presented in Table 1. In the scenario analysis, the cost-effectiveness of CAB–LA was assessed for specific population subgroups, including MSM and TGW, African American/Black MSM, Hispanic MSM, White MSM, and cisgender women.
2.3 PrEP Use
The model accounted for PrEP adherence, persistence, and switching, with parameter values specific to each PrEP option. All PrEP-use parameters and assumptions for the base-case analysis are provided in Table 1.
2.3.1 PrEP Adherence
Adherence is a critical factor in PrEP efficacy, and many individuals receiving oral PrEP have documented adherence issues due to known barriers such as daily pill burden, stigma, and concerns about potential side effects [22, 23]. Nevertheless, oral PrEP requires a high level of adherence to be effective (ideally 4+ doses per week for MSM and TGW [6] and 6+ doses per week for cisgender women [4, 5]). CAB–LA injections are directly administered by a healthcare provider and may address adherence barriers associated with oral PrEP [22, 23]. In the HPTN 083 clinical trial, 70.0% of a random sample of participants in the FTC/TDF arm had laboratory evidence via dried blood spot testing consistent with four or more doses per week [24]. In contrast, 91.5% of person-years (PY) were covered in either arm of the trial by CAB–LA or placebo injections, defined as injections received with a delay of less than 2 weeks [9] [note that the dosing schedule approved by the Food and Drug Administration (FDA) states that CAB–LA may be given up to 7 days before or after the date the individual is scheduled to receive their injection [11].] To account for the observed adherence, the base-case analysis adjusted acquisition costs downward for oral PrEP (assuming less frequent prescription refills; see Online Resource for more information) and, conservatively, used full, unadjusted costs for CAB–LA based on indicated dosing. For both CAB–LA and oral PrEP, efficacy did not require adjustment in the base-case analysis, as it was already aligned with observed clinical trial adherence. In the sensitivity and scenario analyses, adherence to oral PrEP was varied using uncertainty information and real-world adherence data [7]; these changes were allowed to affect PrEP costs and efficacy (see Online Resource for more information). A similar analysis has not yet been conducted for CAB–LA due to a lack of data on the impact of changes in CAB–LA adherence on efficacy.
2.3.2 PrEP Persistence and Switching
Persistence on PrEP was defined as the percentage of modeled individuals remaining on PrEP over time. Oral PrEP persistence was taken from a study assessing real-world PrEP persistence in the USA over a 12-month period [7]. As expected, a higher rate of PrEP discontinuation was observed during the initial 6 months of use than in months 6–12. Accordingly, the model assumed a higher rate of PrEP discontinuation in the first 6 months followed by a lower rate from that point onward, with a consistent value based on discontinuation observed between 6 months and 12 months in the real-world study [7]. CAB–LA persistence in the real world had not yet been assessed at the time this model was developed. As CAB–LA provides an additional modality that addresses barriers to both adherence and persistence [22, 23], it may improve PrEP continuation rates. This trend would be consistent with the experience in contraception, where matching women’s preferred modality increased persistence [25]. Therefore, CAB–LA was assumed to have a 20% relative improvement in persistence compared with oral PrEP at all time points. Equal persistence was tested in the scenario analysis. In all cases, individuals who discontinued their initial PrEP could switch to another option (Table 1). Conservatively, the model did not account for any residual CAB–LA efficacy after discontinuation. This assumption is consistent with guidelines that recommend initiation of daily oral PrEP within 8 weeks after the last injection of CAB–LA for individuals at continued risk of HIV-1 acquisition [6].
2.4 Clinical Data
While receiving PrEP, individuals were at a reduced risk of acquiring HIV-1 infection and those receiving CAB–LA could experience ISRs. Individuals who acquired HIV-1 infection incurred lifetime losses in life expectancy and QALYs and could potentially transmit HIV onwards. They could also acquire PrEP-related resistance mutations. Information on the clinical data used in the model to characterize these events is provided in the following sections.
2.4.1 HIV Incidence and PrEP Efficacy
HIV incidence varied depending on the PrEP option (if any) an individual received. Base HIV incidence for MSM and TGW not receiving PrEP was taken from Mera et al. [26], as the HPTN 083 clinical trial did not include a placebo arm for ethical reasons. HIV incidence for MSM and TGW receiving CAB–LA or oral PrEP in the base-case analysis was taken from the HPTN 083 clinical trial [9]. In the sensitivity analyses, HIV incidence was adjusted to account for varying oral PrEP adherence rates [9, 24, 27] (see Online Resource for more information).
Base HIV incidence for cisgender women at risk has not been studied extensively in the USA, and the HPTN 084 clinical trial did not include a placebo arm for ethical reasons. Therefore, base HIV incidence was estimated from the number of cisgender women in the USA with and without a PrEP indication and available HIV-1 diagnosis rates (Online Resource Table S-1). HIV incidence for cisgender women receiving CAB–LA or FTC/TDF was taken from the HPTN 084 clinical trial [10]. All HIV incidence values used in the model are summarized in Table 2.
2.4.2 Adverse Event Incidence
Modeled individuals receiving CAB–LA could experience ISRs. Rates of ISR by severity were taken from the HPTN 083 (MSM and TGW) and HPTN 084 (cisgender women) clinical trials (Table 2). The model applied ISR events in the first year of the analysis, as ISRs that require management tend to occur early in CAB–LA use.
All other short-term adverse events were assumed to have similar, low incidence rates across all PrEP options, and long-term adverse events were assumed to be rare given the relatively short exposure to PrEP. Thus, adverse events beyond ISRs were not included in the model.
2.4.3 PrEP-Related Resistance Mutations
Individuals who acquired HIV-1 infection while receiving PrEP could develop PrEP-related resistance mutations and require different ARV treatment regimens than individuals without resistance. The incidence of PrEP-related resistance, measured as events per PY receiving PrEP, was 0.16% for individuals receiving CAB–LA [integrase strand transfer inhibitor (INSTI) resistance] and 0.19% for individuals receiving oral PrEP [nucleoside reverse transcriptase inhibitor (NRTI) resistance] [9, 28]. Data for all modeled individuals were taken from the HPTN 083 clinical trial because resistance data were not yet available from the HPTN 084 trial. Non-nucleoside reverse transcriptase inhibitor (NNRTI) resistance was not included in the model because none of the PrEP options include NNRTIs, so any observed NNRTI resistance after HIV acquisition must be transmitted rather than resistance associated with PrEP. Similarly, NRTI resistance was not included in the model for CAB–LA.
2.4.4 Secondary HIV Infections
By avoiding HIV-1 infection, individuals on PrEP avoid potential onward HIV transmission. On average, individuals who acquired HIV-1 infection in the model were estimated to transmit HIV to 0.80 others [29]. These secondary infections were generally assumed to occur in the acute phase of HIV disease progression, when viral load and risk of transmission are high before viral suppression is achieved via multiclass ARV treatment. This timing informed the discounting of associated costs, losses in life expectancy, and QALYs.
2.5 Costs
Over time, modeled individuals incurred PrEP-related costs, including acquisition, administration, and monitoring costs, and could incur ISR management costs, lifetime HIV-related care costs, and PrEP-related resistance costs. Information about these costs is provided in the sections below.
2.5.1 PrEP-Related Costs
PrEP acquisition costs were based on indicated dosing and unit costs (Table 3). Dosing was taken from the relevant product labels [3, 11, 30]. Unit costs were taken from Redbook using 2022 wholesale acquisition costs [31]. The cost of FTC/TDF was based on the lowest cost among the available generic options. The cost of CAB–LA was based on individuals receiving seven injections in year 1, according to the initiation dosing schedule, and six injections every year thereafter, based on every-2-month maintenance dosing [11]. Oral PrEP acquisition costs were adjusted to account for adherence observed in the HPTN 083 clinical trial, where the base-case analysis estimated an average of 3.95 doses taken each week by individuals receiving oral PrEP (Online Resource Table S-2). Conservatively, CAB–LA costs were based on indicated dosing and were not adjusted for adherence.
Administration costs for PrEP included the costs associated with injection administrations (CAB–LA) and routine physician visits (all PrEP) (Table 3). Monitoring costs for PrEP included the costs associated with laboratory tests recommended for individuals receiving PrEP in the clinical monitoring guidelines published by the CDC in 2021 [6] (Table 3 and Online Resource Table S-3).
2.5.2 ISR Management Costs
Management costs for ISRs were estimated by severity. Mild ISRs were assumed to require no medical management. Moderate ISRs were assumed to be managed with 800 mg of over-the-counter ibuprofen three times per day for 3 days after each injection in the first year of CAB–LA use, with a total cost per event of $4.51 [31]. Severe ISRs were assumed to require a physician visit [Current Procedural Terminology (CPT) code 99213] and the same ibuprofen regimen, with a total cost per event of $187.58 [32].
2.5.3 Lifetime HIV Management Costs
Individuals who acquired HIV-1 infection in the model incurred the cost of lifetime HIV-related care, including the cost of ARV treatment and ongoing monitoring. The total discounted lifetime cost of HIV-related care was taken from a study of incremental healthcare costs for commercially insured individuals living with HIV compared with individuals without HIV [33]. The cost reported in 2017 US dollars was inflated to $939,946 in 2022 US dollars [34] and was applied to all modeled primary and secondary infections at the time of HIV acquisition.
2.5.4 PrEP-Related Resistance Mutation Costs
In the model, individuals with PrEP-related resistance mutations were assumed to require different ARV treatment regimens than individuals without resistance for a period of time (Table 3). Individuals who acquired HIV-1 infection without PrEP-related resistance mutations were assumed to receive dolutegravir/lamivudine ($32,290 per year), the lowest cost INSTI-based single-tablet regimen currently recommended as an initial regimen for most people with HIV [31, 35]. Individuals with PrEP-related resistance mutations required more expensive first-line regimens. Specifically, individuals with INSTI resistance were assumed to receive darunavir/cobicistat/emtricitabine/tenofovir alafenamide ($49,489 per year) and individuals with NRTI resistance were assumed to receive dolutegravir + darunavir/cobicistat ($50,166 per year) [31]. Individuals with PrEP-related resistance mutations were assumed to remain on their more expensive regimens for the entirety of their first-line treatment. The average duration of first-line treatment was conservatively estimated to be 16.2 years, based on a 2011 study by Beck et al. [36]. Realistically, durations may now be shorter due to the availability of additional ARV options and the possibility of regimen optimization in the setting of viral suppression. Furthermore, PrEP-related resistance mutations may occur less frequently as HIV testing options continue to evolve.
2.6 Life Expectancy and QALY Losses Due to HIV
Individuals who acquired HIV-1 infection experienced losses in life expectancy and QALYs, with values estimated from published literature and publicly available life-expectancy data (Table 1). These losses were applied to all modeled primary and secondary infections. Individuals who did not acquire HIV-1 infection were assumed to have no losses in life expectancy or QALYs. Additionally, no utility or QALY decrements were applied while receiving PrEP because it was assumed that individuals choosing to receive PrEP view the choice positively, as benefits like decreased anxiety about acquiring HIV-1 infection may outweigh potential negative feelings on issues such as ISRs.
2.7 Validation
Various validation processes were conducted to support confidence in the model and its outcomes. Specifically, the model structure, input parameter values, programming, and outcomes were validated according to the Assessment of the Validation Status of Health-Economic decision models (AdViSHE) tool [37]. Face-validity testing of the model structure, inputs, and outcomes was conducted by the authors and by clinical and health economic modeling experts external to the project team. Cross-validity testing was conducted by comparing the structure, inputs, and results of our model with those of several other models, as described in the Discussion section. The computer model in Excel was subjected to a predefined quality-check process that included extreme-value and other scenario testing as well as validation of all equations, code, input data, and results. The computer model was also independently assessed by a health economic modeling expert external to the project team and extensively reviewed and pressure tested by the authors. Finally, comprehensive sensitivity and scenario analyses were conducted to assess the impact of parameter uncertainty and alternate modeling assumptions and input parameter values on the model results, as described in the following sections.
2.8 Analyses
2.8.1 Base-Case Analysis
The base-case analysis assessed lifetime costs and health outcomes for individuals in the CAB–LA pathway versus the oral PrEP pathway (Fig. 1), assuming a 5-year duration of risk during which PrEP use could help prevent HIV-1 infection. Model outcomes included total costs by cost category, number of primary and secondary HIV-1 infections, life-years and QALYs lost due to HIV acquisition, and various ICERs (Table 4). All costs and health outcomes were discounted at 3% per year [21]. Willingness-to-pay thresholds in the USA commonly range between $50,000 and $300,000 per QALY gained [38, 39]. For this analysis, the CAB–LA pathway was considered cost-effective if the incremental cost per QALY gained was at or below $100,000 per QALY gained [38].
2.8.2 Sensitivity Analyses
Sensitivity analyses were conducted to assess the impact of parameter uncertainty on the cost-effectiveness results. In the one-way sensitivity analysis, input parameters were individually varied over their 95% confidence intervals (CIs). In the probabilistic sensitivity analysis, 10,000 iterations were conducted, where input parameter values were varied simultaneously and sampled from probability distributions via Monte Carlo simulation. The ranges and distributions used in these analyses were derived from published sources whenever possible and are described in additional detail in Online Resource Table S-4.
2.8.3 Scenario Analysis
A scenario analysis was conducted to assess the impact on the cost-effectiveness results of variations in PrEP use, the modeled population, and other key assumptions. Two real-world PrEP-use scenarios were examined to compare the CAB–LA pathway with no PrEP, as PrEP is still highly underutilized in the USA, and to test oral PrEP adherence observed in a real-world setting rather than in a clinical trial setting. Additional scenarios were conducted to assess the cost-effectiveness of the CAB–LA pathway in individual population subgroups that experience a disproportionate burden of new HIV-1 infections (i.e., MSM and TGW, African American/Black MSM, Hispanic MSM, White MSM, and cisgender women). For these subgroup analyses, HIV incidence for PrEP users was taken from HPTN 083 or HPTN 084 and, like the base-case analysis, base HIV incidence for MSM and TGW not receiving PrEP was taken from Mera et al. [26] and base HIV incidence for cisgender women was estimated from the number of cisgender women in the USA with and without a PrEP indication and available HIV-1 diagnosis rates (Online Resource Table S-1). The duration of HIV risk was varied in two scenarios to test the impact of shorter (2-year) and longer (10-year) durations of risk. Finally, scenarios were conducted to compare the CAB–LA pathway with a FTC/TAF pathway (where approved for use) and to assess variations in important PrEP use parameters, including persistence, switching, and monitoring. Specific scenarios tested are summarized in Table 5.
3 Results
3.1 Base-Case Analysis Results
For individuals eligible for PrEP, the base-case analysis compared the CAB–LA pathway versus the oral PrEP pathway beginning with the lowest cost generic FTC/TDF option. In these pathways, individuals could continue receiving their initial PrEP option, transition to a second PrEP option (CAB–LA pathway: FTC/TDF; oral PrEP pathway: FTC/TAF, if indicated), or discontinue PrEP over time (Fig. 1). Model results showed that, over the 5-year duration of risk, the CAB–LA pathway prevented a total of 4.5 more primary and secondary HIV-1 infections per 100 PrEP users than the oral PrEP pathway. Average per-person PrEP-related costs were $51,993 higher for the CAB–LA pathway than for the oral PrEP pathway, but these increased PrEP-related costs were largely offset by a $42,517 reduction in lifetime HIV management costs. The CAB–LA pathway also resulted in 0.202 fewer QALYs lost than the oral PrEP pathway. Overall, the CAB–LA pathway was cost-effective when compared with the oral PrEP pathway beginning with the lowest cost generic FTC/TDF option, with an incremental cost per QALY gained of $46,843 (Table 4).
3.2 Sensitivity Analysis Results
The one-way sensitivity analysis showed that model results were most sensitive to changes in HIV incidence for MSM and TGW while receiving FTC/TDF or CAB–LA and to changes in adherence to oral PrEP (Online Resource Fig. S-2). Overall, ICERs generally remained below $100,000 per QALY gained when parameters were varied across their 95% CIs, suggesting the stability of the predicted results.
The probabilistic sensitivity analysis showed that the CAB–LA pathway was cost-effective compared with the oral PrEP pathway in 85% of the 10,000 Monte Carlo simulations (Online Resource Fig. S-3). In 9% of the simulations, the CAB–LA pathway was dominant (i.e., the CAB–LA pathway was less costly and more effective, as shown in quadrant IV of Online Resource Fig. S-4).
3.3 Scenario Analysis Results
Table 5 summarizes the scenario analysis results. The CAB–LA pathway was dominant in several of the scenarios that examined PrEP use assumptions, including the two real-world PrEP-use scenarios, the scenario comparing the CAB–LA pathway with a pathway beginning with FTC/TAF, and the scenario with more individuals consistently receiving FTC/TDF to cover the CAB–LA pharmacokinetic (PK) tail. The CAB–LA pathway was cost-effective or dominant compared with the oral PrEP pathway for most population subgroups, including MSM and TGW, MSM of color, and cisgender women. The CAB–LA pathway was also found to be cost-effective in scenarios testing longer or shorter durations of HIV risk, equivalent persistence for all PrEP options, no PK tail coverage after CAB–LA discontinuation, and alternative monitoring costs. The CAB–LA pathway slightly exceeded $100,000 per QALY gained in the scenario focused on the White MSM population.
4 Discussion
This analysis comprehensively evaluated the costs, health outcomes, and cost-effectiveness of initiating PrEP with CAB–LA versus existing oral PrEP options among MSM, TGW, and cisgender women aged 18 years or older in the USA who are eligible for PrEP due to increased risk of acquiring HIV-1 infection. Our analysis showed that the CAB–LA pathway prevented more primary and secondary HIV-1 infections than the daily oral PrEP pathway beginning with generic FTC/TDF and yielded fewer QALYs lost. The CAB–LA pathway increased PrEP-related costs but reduced downstream HIV-related care costs. Overall, the CAB–LA pathway was shown to be cost-effective. A range of sensitivity and scenario analyses were conducted, and ICERs generally remained below $100,000 per QALY gained when parameters and modeling assumptions were varied broadly, suggesting stability of the predicted cost-effectiveness results. The CAB–LA pathway also resulted in cost savings in several key scenarios, including those examining real-world PrEP use and subgroup analyses among African American/Black MSM and cisgender women.
An earlier study by Neilan and colleagues [15] examined the potential cost-effectiveness of long-acting injectable PrEP in a limited analysis conducted before CAB–LA was approved by the FDA. This study provides an important comparison with our results. The Neilan study showed that CAB–LA may reduce transmissions and increase QALYs compared with generic daily oral FTC/TDF over a 10-year time horizon, with an incremental cost of $1,582,000 per QALY gained for MSM and TGW similar to those enrolled in the HPTN 083 clinical trial. Our study also found that initiating PrEP with CAB–LA may substantially improve health outcomes and estimated a lifetime incremental cost of $46,843 per QALY gained for MSM, TGW, and cisgender women eligible for PrEP. The two studies both consider similar interventions, costs and health outcomes, and primary and secondary HIV-1 infections. Key differences between the Neilan study [15] and ours include the model structure (microsimulation versus Markov model), analysis time horizon (10 years versus lifetime), modeled population (MSM and TGW only versus MSM, TGW, and cisgender women), comparator structure (individual comparators versus PrEP pathways), structure of costs and health outcomes for individuals who acquire HIV-1 infection (annual versus lifetime), and various differences in specific input parameter values. Access to both models would be required to conduct a formal assessment of the impact of the differences. However, in an informal assessment conducted by adapting our model to match the Neilan study as much as possible, model results were found to be most sensitive to changes in the model time horizon, with shorter time horizons like 10 years yielding very high ICERs similar to those reported in the Neilan study [15]. This result is not surprising because, for shorter time horizons, the model captures the upfront cost of PrEP but omits most of the cost associated with lifelong HIV management and the long-term effects of HIV acquisition on quality of life and survival, especially for individuals who acquire HIV later in the model time horizon. This comparison demonstrates that, as the good modeling practice recommendations specify [21], the choice of a sufficiently long model time horizon is critical to ensuring an accurate cost-effectiveness assessment, particularly for preventive interventions such as HIV PrEP that have upfront costs and long-term benefits.
More recently, another study assessed the cost-effectiveness of CAB–LA in South Africa using a 20-year model that also included MSM, TGW, and cisgender women [40]. While cost comparisons with this study are difficult due to health system differences, the study reported that CAB–LA could prevent 11–22% more HIV-1 infections than FTC/TDF over a 20-year period, depending on PrEP coverage and persistence [40]. A modeling study among MSM in Atlanta that evaluated the impact of CAB–LA on EHE goals similarly showed that switching from FTC/TDF to CAB–LA could decrease new HIV-1 infections by 12% (with current PrEP use) to 30% (with PrEP use increased 20%) between 2022 and 2026 [41]. Our model showed consistent results, with a 25% reduction in total new primary and secondary HIV-1 infections for the CAB–LA pathway compared with the oral PrEP pathway in which individuals initiated daily oral FTC/TDF, and extended the work of these studies by assessing lifetime costs and cost-effectiveness among MSM, TGW, and cisgender women using PrEP.
Our analysis also had limitations that should be considered when interpreting the results. First, the static model structure held HIV incidence constant over the 5-year duration of HIV risk. As such, our analysis assessed the cost-effectiveness of the CAB–LA pathway within the current epidemic conditions, but the EHE initiative or other factors may result in variation in HIV incidence in the future. Second, HIV incidence estimates for individuals receiving PrEP were taken from relevant clinical trials [9, 10], which may not mirror real-world outcomes. However, the scenario analysis showed that model results for the CAB–LA pathway were generally more favorable in real-world scenarios, such as scenarios with real-world oral PrEP adherence or no PrEP as a comparator, as PrEP is still highly underutilized in the USA. Further, the HPTN 084 clinical trial was conducted in sub-Saharan Africa, where cisgender women at increased risk of acquiring HIV-1 infection may have different base HIV incidence and PrEP use patterns than in the USA. Importantly, while the HPTN 084 clinical trial did not include a placebo arm for ethical reasons, a counterfactual study estimated that, had a placebo arm been included, HIV incidence (2.2 events per 100 PY) [42] would have been similar to our estimate of base HIV incidence among cisgender women at increased risk of acquiring HIV-1 infection in the USA (2.73 events per 100 PY). To examine variation in HIV incidence and oral PrEP adherence, a scenario testing lower HIV incidence and a hypothetical adherence improvement that yields a 20% improvement in oral PrEP efficacy was included in the scenario analysis, and the CAB–LA pathway remained cost-effective. Further study of PrEP efficacy among cisgender women in alternate geographical locations is warranted, but health equity considerations suggest that inclusion of cisgender women in economic analyses is essential now to help estimate the value of the available PrEP options for this underserved and understudied population [4,5,6, 8, 43, 44].
In addition to limitations related to HIV incidence, our analysis had limitations in data availability. First, because long-term and real-world adherence and persistence data for CAB–LA are not yet available, the model used conservative assumptions for adherence and included only a modest improvement in persistence for CAB–LA versus oral PrEP over time. A scenario that excluded this persistence improvement was tested in the scenario analysis, and the CAB–LA pathway remained cost-effective. Second, our analysis used the PrEP administration guidelines published by the CDC in 2021 [6], but guidelines will continue to evolve. Recent [35] and future changes could affect costs for all individuals receiving PrEP (e.g., costs for monitoring tests) and for those individuals who receive PrEP and acquire HIV (e.g., costs for resistance testing and selection of initial ARV treatment regimens). In the scenario analysis, model results remained consistent when alternate monitoring costs were examined, and any changes in resistance testing guidelines are expected to have an even smaller impact, as only individuals who acquire HIV receive resistance testing and the cost of this testing is a small fraction of the total lifetime cost of HIV-related care [35]. Finally, recent data for several model input parameters were not available in published studies. Thus, lifetime QALY losses for individuals who acquired HIV-1 infection (calculated to include only individuals diagnosed with CD4 cell counts above 350 cells/μL) and the duration of first-line ARV treatment differentiation for individuals with PrEP-related resistance mutations were taken from somewhat dated studies by Farnham et al. [29] and Beck et al. [36], respectively. Data on HIV incidence among TGW and cisgender women eligible for PrEP were also not available, as most studies have focused on MSM [43]. Thus, base HIV incidence for TGW was assumed equal to that of MSM, and base HIV incidence for cisgender women at risk was calculated based on available published data (Online Resource Table S-1). For all of these parameters, conservative estimates were used in the base-case analysis, and the model results were found to be consistent in the sensitivity analyses.
5 Conclusions
This analysis suggests that CAB–LA for PrEP represents a cost-effective approach to reducing primary and onward HIV-1 infections compared with all options assessed, including generic daily oral FTC/TDF, for individuals in the USA who are eligible for PrEP due to increased risk of acquiring HIV-1 infection. The CAB–LA pathway was predicted to be cost-effective overall and potentially cost-saving among specific subgroups disproportionately affected by HIV and currently receiving less benefit from daily oral PrEP, such as cisgender women and MSM of color. As a result, CAB–LA may be an important tool to reduce new HIV-1 infections in the USA overall and in specific communities aligned with the EHE initiative.
Notes
While 2020 data are available, 2019 estimates are provided here due to the impact of the COVID-19 pandemic on access to HIV testing, care-related services, and case surveillance activities in state and local jurisdictions.
References
CDC. Diagnoses of HIV infection in the United States and dependent areas, 2019. May 2021. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Accessed 1 Nov 2022.
CDC. Ending the HIV epidemic. April 1, 2021. https://www.cdc.gov/endhiv/index.html. Accessed 1 Nov 2022.
DESCOVY PI. DESCOVY® (emtricitabine and tenofovir alafenamide) tablets, for oral use. Gilead Sciences; January 2022. https://www.gilead.com/~/media/files/pdfs/medicines/hiv/descovy/descovy_pi.pdf?la=en. Accessed 1 Nov 2022.
Marrazzo JM, Ramjee G, Richardson BA, Gomez K, Mgodi N, Nair G, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2015;372(6):509–18.
Celum C, Hosek S, Tsholwana M, Kassim S, Mukaka S, Dye BJ, et al. PrEP uptake, persistence, adherence, and effect of retrospective drug level feedback on PrEP adherence among young women in southern Africa: results from HPTN 082, a randomized controlled trial. PLoS Med. 2021;18(6): e1003670.
CDC. US Public Health Service: preexposure prophylaxis for the prevention of HIV infection in the United States—2021 update: a clinical practice guideline. Centers for Disease Control and Prevention; December 2021. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf. Accessed 1 Nov 2022.
Oglesby A, Germain G, Laliberte F, Bush S, Swygard H, MacKnight S, et al. Real-world persistency of patients receiving tenofovir-based pre-exposure prophylaxis for the prevention of HIV infection in the US. In: Presented at the Infectious Disease Week (IDWeek) Conference, Virtual. 29 Sep-3 Oct, 2021.
CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2019. May 2021. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-vol-26-no-2.pdf. Accessed 1 Nov 2022.
Landovitz RJ, Donnell D, Clement ME, Hanscom B, Cottle L, Coelho L, et al. Cabotegravir for HIV prevention in cisgender men and transgender women. N Engl J Med. 2021;385(7):595–608.
Delany-Moretlwe S, Hughes JP, Bock P, Ouma SG, Hunidzarira P, Kalonji D, et al. Cabotegravir for the prevention of HIV-1 in women: results from HPTN 084, a phase 3, randomised clinical trial. Lancet. 2022;399(10337):1779–89.
APRETUDE PI. APRETUDE (cabotegravir extended-release injectable suspension), for intramuscular use. ViiV Healthcare; December 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/215499s000lbl.pdf. Accessed 1 Nov 2022.
Chen A, Dowdy DW. Clinical effectiveness and cost-effectiveness of HIV pre-exposure prophylaxis in men who have sex with men: risk calculators for real-world decision-making. PLoS ONE. 2014;9(10): e108742.
Paltiel AD, Freedberg KA, Scott CA, Schackman BR, Losina E, Wang B, et al. HIV preexposure prophylaxis in the United States: impact on lifetime infection risk, clinical outcomes, and cost-effectiveness. Clin Infect Dis. 2009;48(6):806–15.
Walensky RP, Horn T, McCann NC, Freedberg KA, Paltiel AD. Comparative pricing of branded tenofovir alafenamide-emtricitabine relative to generic tenofovir disoproxil fumarate-emtricitabine for HIV preexposure prophylaxis: a cost-effectiveness analysis. Ann Intern Med. 2020;172(9):583–90.
Neilan AM, Landovitz RJ, Le MH, Grinsztejn B, Freedberg KA, McCauley M, et al. Cost-effectiveness of long-acting injectable HIV preexposure prophylaxis in the United States: a cost-effectiveness analysis. Ann Intern Med. 2022;175(4):479–89.
Hess KL, Hu X, Lansky A, Mermin J, Hall HI. Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol. 2017;27(4):238–43.
Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I, et al. Sexually transmitted infection treatment guidelines, 2021. MMWRR Recomm Rep. 2021;70(4):39.
CDC. Interpretation of hepatitis B serologic test results. https://www.cdc.gov/hepatitis/HBV/PDFs/SerologicChartv8.pdf. Accessed 1 Nov 2022.
Schillie S, Wester C, Osburne M, Wesolowski L, Ryerson AB. CDC recommendations for hepatitis C screening among adults—United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(2):1–17.
Landovitz RJ, Donnell D, Clement M, Hanscom B, Cottle L, Coelho L. HPTN 083 final results: pre-exposure prophylaxis containing long-acting injectable cabotegravir is safe and highly effective for cisgender men and transgender women who have sex with men. In: Presented at the AIDS 2020 Conference, Virtual. 6–10 July, 2020.
Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016;316(10):1093–103.
Serota DP, Rosenberg ES, Sullivan PS, Thorne AL, Rolle CM, Del Rio C, et al. Pre-exposure prophylaxis uptake and discontinuation among young black men who have sex with men in Atlanta, Georgia: a prospective cohort study. Clin Infect Dis. 2020;71(3):574–82.
Kelley CF, Kahle E, Siegler A, Sanchez T, Del Rio C, Sullivan PS, Rosenberg ES. Applying a PrEP continuum of care for men who have sex with men in Atlanta. Georgia Clin Infect Dis. 2015;61(10):1590–7.
Grinsztejn B, Donnell D, Clement M, Hanscom B, Cottle L, Coelho L. HPTN 083: efficacy of pre-exposure prophylaxis (PrEP) containing long-acting injectable cabotegravir (CAB-LA) is maintained across regions and key populations. In: Presented at the AIDS 2020 Conference, Virtual. 6–10 July, 2020.
Ross J, Stover J. Use of modern contraception increases when more methods become available: analysis of evidence from 1982–2009. Glob Health Sci Pract. 2013;1(2):203–12.
Mera R, Scheer S, Carter C, Das M, Asubonteng J, McCallister S, Baeten J. Estimation of new HIV diagnosis rates among high-risk, PrEP-eligible individuals using HIV surveillance data at the metropolitan statistical area level in the United States. J Int AIDS Soc. 2019;22(12): e25433.
Grant RM, Anderson PL, McMahan V, Liu A, Amico KR, Mehrotra M, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14(9):820–9.
Marzinke M, Grinsztejn B, Fogel J, Piwowar EM, Hanscom B, Coelho L. Laboratory analysis of HIV infections in HPTN 083: injectable CAB for PrEP [oral abstract]. In: Presented at the Conference on Retroviruses and Opportunistic Infections, Boston, Massachusetts. 6–10 March, 2021.
Farnham PG, Gopalappa C, Sansom SL, Hutchinson AB, Brooks JT, Weidle PJ, et al. Updates of lifetime costs of care and quality-of-life estimates for HIV-infected persons in the United States: late versus early diagnosis and entry into care. J Acquir Immune Defic Syndr. 2013Oct;64(2):183–9.
TRUVADA PI. TRUVADA® (emtricitabine and tenofovir disoproxil fumarate) tablets, for oral use. Gilead Sciences; June 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/021752s061lbl.pdf. Accessed 1 Nov 2022.
Merative Micromedex Solutions. Red Book. 2022. https://www.micromedexsolutions.com/home/dispatch/ssl/true. Accessed 15 Apr 2021.
CMS.gov. Physician fee schedule. 1 July 2022. https://www.cms.gov/medicare/physician-fee-schedule/search/overview. Accessed 23 Aug 2022.
Cohen JP, Beaubrun A, Ding Y, Wade RL, Hines DM. Estimation of the incremental cumulative cost of HIV compared with a non-HIV population. Pharmacoecon Open. 2020;4(4):687–96.
US Bureau of Labor Statistics. Consumer price index for Medical Care. 2022. https://data.bls.gov/cgi-bin/surveymost?cu. Accessed Jan 2022.
Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV. Department of Health and Human Services; 21 September 2022. https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/adult-adolescent-arv/guidelines-adult-adolescent-arv.pdf. Accessed 1 Nov 2022.
Beck EJ, Mandalia S, Lo G, Sharott P, Youle M, Anderson J, et al. Cost-effectiveness of early treatment with first-line NNRTI-based HAART regimens in the UK, 1996–2006. PLoS ONE. 2011;6(5): e20200.
Vemer P, Corro Ramos I, van Voorn GA, Al MJ, Feenstra TL. AdViSHE: a validation-assessment tool of health-economic models for decision makers and model users. Pharmacoeconomics. 2016;34(4):349–61.
Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796–7.
Braithwaite RS, Meltzer DO, King JT Jr, Leslie D, Roberts MS. What does the value of modern medicine say about the $50,000 per quality-adjusted life-year decision rule? Med Care. 2008;46(4):349–56.
Jamieson L, Johnson LF, Nichols BE, Delany-Moretlwe S, Hosseinipour MC, Russell C, Meyer-Rath G. The relative cost-effectiveness of long-acting injectable cabotegravir versus oral pre-exposure prophylaxis. In: Presented at the AIDS Conference, Montreal, Canada and virtual. 29 July–2 August, 2022.
Mitchell KM, Boily MC, Hanscom B, Moore M, Todd J, Paz-Bailey G, et al. Estimating the impact of HIV PrEP regimens containing long-acting injectable cabotegravir or daily oral tenofovir disoproxil fumarate/emtricitabine among men who have sex with men in the United States: a mathematical modelling study for HPTN 083. Lancet Reg Health Am. 2023Feb;18: 100416.
Moore M, Donnell DJ, Boily MC, Mitchell KM, Delany-Moretlwe S, Hosseinipour M, et al. Estimated long-acting PrEP effectiveness in the HPTN 084 cohort using a model-based HIV incidence in the absence of PrEP. Presented at the The International AIDS Society (IAS), Virtual. 18–21 July, 2021. Available at: https://theprogramme.ias2021.org/Abstract/Abstract/1303. Accessed 25 Aug 2023.
Torres-Rueda S, Terris-Prestholt F, Gafos M, Indravudh PP, Giddings R, Bozzani F, et al. Health economics research on non-surgical biomedical HIV prevention: identifying gaps and proposing a way forward. Pharmacoeconomics. 2023Jul;41(7):787–802.
Sarri G, Soriano Gabarro M, Cheng R, Jhutti-Johal J. Gender and health equity in health care decision-making: how women’s issues continue to be neglected. In: Presented at: ISPOR Europe. Copenhagen, Denmark; 12–15 November 2023.
CDC. Core indicators for monitoring the Ending the HIV Epidemic initiative (preliminary data): National HIV Surveillance System data reported through March 2021; and preexposure prophylaxis (PrEP) data reported through December 2020. July 2021. https://www.cdc.gov/hiv/pdf/library/reports/surveillance-data-tables/vol-2-no-3/cdc-hiv-surveillance-tables-vol-2-no-3.pdf. Accessed 1 Nov 2022.
Xu J, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2018. NCHS data brief no 355. Hyattsville, MD: National Center for Health Statistics; January 2020. https://www.cdc.gov/nchs/data/databriefs/db355-h.pdf. Accessed 1 Nov 2022.
Mayer K, Molina JM, Thompson MA, Anderson PL, Mounzer KC, De Wet JJ, et al. Emtricitabine and tenofovir alafenamide vs emtricitabine and tenofovir disoproxil fumarate for HIV pre-exposure prophylaxis (DISCOVER): primary results from a randomised, double-blind, multicentre, active-controlled, phase 3, non-inferiority trial. Lancet. 2020;396(10246):239–54.
CDC. US Public Health Service: Preexposure prophylaxis for the prevention of HIV infection in the United States—2021 update: a clinical practice guideline [Draft]. Centers for Disease Control and Prevention; 2021.
Acknowledgements
The authors wish to thank Sarah-Jane Anderson, PhD, of GSK and Heidi Swygard, MD, MPH, of ViiV Healthcare for their contributions in the identification of appropriate input parameter values and validation of the model. The authors also wish to thank John Forbes of RTI Health Solutions for providing copyediting and formatting support for the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding for this study was provided by ViiV Healthcare Inc. Authors maintained independent scientific control of the study design and analyses.
Conflicts of Interest
AB, AD, and CM are employees of RTI Health Solutions, an independent research organization that received funding from ViiV Healthcare Inc. to support the conduct of the study. JF, AM, and AO are employees of ViiV Healthcare Inc.
Availability of Data
Data used in this analysis were taken from published or publicly available sources. A minority of data were taken from unpublished clinical study reports and are presented in this article.
Ethics Approval
Not applicable.
Informed Consent
Not applicable.
Authors’ Contributions
The manuscript has been read and approved by all authors, each of whom has met the requirements for authorship. AB, AD, and CM contributed to the design and programming of the economic model, identification and final selection of the input parameter values, interpretation of the study results, and preparation of the manuscript. JF and AO contributed to the design of the economic model, identification of input parameter values, interpretation of study results, and the preparation of the manuscript. AM contributed to the interpretation of study results and the preparation of the manuscript.
Meetings
Portions of the methods and results reported in this manuscript were presented at ISPOR 2022 in Washington DC, USA (presentation title: Cost-Effectiveness of Every Two Month Cabotegravir Long-Acting (CAB–LA) Compared with Daily Oral Emtricitabine (FTC)/Tenofovir Disoproxil Fumarate (TDF) for Pre-Exposure Prophylaxis (PrEP) to Prevent HIV-1 Infection in the United States).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Brogan, A.J., Davis, A.E., Mellott, C.E. et al. Cost-effectiveness of Cabotegravir Long-Acting for HIV Pre-exposure Prophylaxis in the United States. PharmacoEconomics 42, 447–461 (2024). https://doi.org/10.1007/s40273-023-01342-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-023-01342-y