Abstract
Background
Atrial fibrillation (AF) remains the most common form of cardiac arrhythmia. Management of AF aims to reduce the risk of stroke, heart failure and premature mortality via rate or rhythm control. This study aimed to review the literature on the cost effectiveness of treatment strategies to manage AF among adults living in low-, middle- and high-income countries.
Methods
We searched MEDLINE (OvidSp), Embase, Web of Science, Cochrane Library, EconLit and Google Scholar for relevant studies between September 2022 and November 2022. The search strategy involved medical subject headings or related text words. Data management and selection was performed using EndNote library. The titles and abstracts were screened followed by eligibility assessment of full texts. Selection, assessment of the risk of bias within the studies, and data extraction were conducted by two independent reviewers. The cost-effectiveness results were synthesised narratively. The analysis was performed using Microsoft Excel 365. The incremental cost effectiveness ratio for each study was adjusted to 2021 USD values.
Results
Fifty studies were included in the analysis after selection and risk of bias assessment. In high-income countries, apixaban was predominantly cost effective for stroke prevention in patients at low and moderate risk of stroke, while left atrial appendage closure (LAAC) was cost effective in patients at high risk of stroke. Propranolol was the cost-effective choice for rate control, while catheter ablation and the convergent procedure were cost-effective strategies in patients with paroxysmal and persistent AF, respectively. Among the anti-arrhythmic drugs, sotalol was the cost-effective strategy for rhythm control. In middle-income countries, apixaban was the cost-effective choice for stroke prevention in patients at low and moderate risk of stroke while high-dose edoxaban was cost effective in patients at high risk of stroke. Radiofrequency catheter ablation was the cost-effective option in rhythm control. No data were available for low-income countries.
Conclusion
This systematic review has shown that there are several cost-effective strategies to manage AF in different resource settings. However, the decision to use any strategy should be guided by objective clinical and economic evidence supported by sound clinical judgement.
Registration
CRD42022360590.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Apixaban, left atrial appendage closure, propranolol, catheter ablation and convergent procedures are potentially efficient to manage atrial fibrillation in high-income countries. Apixaban, warfarin and radiofrequency catheter ablation are potentially efficient to manage atrial fibrillation in middle-income countries. |
More population-specific clinical trials, head-to-head trials and other relevant population-specific studies are needed to provide more robust data for economic evaluation, which will in turn support decision making. |
The decision to use any treatment strategy should always be individualised and guided by strong objective clinical and economic evidence and sound clinical judgement. |
1 Introduction
Among the cardiac arrhythmias, atrial fibrillation (AF) remains the most common from a public health to clinical perspective [1]. In 2019, approximately 57.9 million people worldwide had AF, twice the number in 1990 [2], representing about 1% of the general population aged 18 years and above. Over 30% of hospital admissions for cardiac rhythm problems were due to AF [3]. AF independently confers a significant long-term risk for ischaemic stroke (fivefold), acute coronary events (including myocardial infarction) and the syndrome heart failure (HF) [1]. Independent of these deadly and disabling conditions, AF is associated with impaired quality of life and premature mortality [3, 4]. Within the progressively ageing populations of high-income countries in whom the antecedents for AF remain high (particularly hypertension), the burden AF is progressively increasing [1]. Although incident AF is closely related to older age, in low- and middle-income countries (LMIC) where hypertension remains largely undetected and uncontrolled, the future burden of AF is also likely to rise [5]. The management of this disease is also abysmal in LMIC due to poor access to healthcare [5].
The management of AF is usually individualised and dependent on several factors including patient factors (e.g. risk of a particular therapy for a patient, patient’s overall risk of stroke and other emboli-related problems) and diagnostic factors (e.g. severity of symptoms and the cause or duration of AF). In general, the short-term goals for the management of AF include symptom relief, and prevention of AF-associated complications including acute decompensated heart failure (HF) in those with impaired systolic function [1]. In the longer-term, key goals include the prevention of stroke, symptom relief, heart rate control, rhythm control and aggressive risk factors management [1]. Prevention of (ischaemic) stroke remains the principal goal in the management of most AF patients, although there is increasing focus on the prevention of chronic HF; particularly as HF begets AF and vice versa [6]. To date, randomised controlled trials (RCTs) do not suggest the superiority of rate control over rhythm control to achieve a normal rhythm. However, if the ultimate goal is restoration and maintenance of sinus rhythm, rate control medication is usually continued throughout the follow-up, unless continuous sinus rhythm is present. Managing AF-related abnormal heart rate may also control abnormal rhythm, but in some cases, cardioversion or ablation procedures are required to control the abnormal rhythm. There are different management strategies for AF, so it is important to stratify the risk profile of each patient, as some patients may require earlier and different intervention from others. This led to the establishment of the CHADS2 [congestive heart failure, hypertension, age ≥ 75 years, diabetes, stroke (doubled)] score. Recently, a new and updated version known as CHA2DS2-VASc [congestive heart failure, hypertension, age ≥ 75 years (doubled), diabetes, stroke (doubled), vascular disease, age 65–74 years and sex category (female)] has taken over as the most accurate risk stratification tool, offering more accurate results for low-risk patients [1].
The prevention of AF-related (ischaemic) stroke can be achieved by different intervention strategies. Anti-coagulants including Vitamin K antagonists (VKA) and Factor Xa inhibitors are the most commonly used interventions. Types of VKA that can be administered to prevent AR-related stroke include warfarin, acenocoumarol, phenprocoumon and fluindione. Historically, warfarin is the most used VKA and the mainstay of therapy when anti-coagulation is required. Modern alternatives to warfarin [due to the need for routine international normalized ratio (INR) therapeutic monitoring and high-risk of haemorrhagic strokes/other major bleeding events] are the Factor Xa inhibitors or the direct oral anticoagulants (DOAC). These include apixaban, dabigatran, edoxaban and rivaroxaban. Anti-platelets such as aspirin (a cyclooxygenase inhibitor) and, more latterly, clopidogrel (a selective adenosine diphosphate receptor inhibitor) are also used in AF but often in combination with anti-coagulants. In patients with AF from mechanical heart valves, low molecular weight heparin (LMWH) or unfractionated heparin (UFH) can be used for ‘bridging’ anti-coagulation. Direct thrombin inhibitors such as argatroban and bivalirudin can be used as alternatives for heparin. Studies have shown that DOACs are as effective as the VKAs in preventing AF-related stroke, but in terms of cost effectiveness, VKAs still appears as an attractive strategy in resource-limited settings [7] due to the high cost of DOACs. In high-income countries, however, DOACs seem to be the new conventional strategies [8]. Anti-coagulant treatment is likely unnecessary in males with CHA2DS2-VASc score of 0 and females with a score of 1. Scores ≥ 1 for males and ≥ 2 for females would require anti-coagulants.
Alternatively, strategies to control heart rate associated with AF include beta-blockers (metoprolol, bisoprolol, atenolol, esmolol, propranolol, carvedilol), non-dihydropyridine calcium channel antagonists (verapamil, diltiazem), digitalis glycosides (digoxin and digitoxin) and some class 3 anti-arrhythmic drugs (amiodarone and dronedarone) [1]. The use of any of these strategies for heart rate control depends on the treatment objectives such as acute rate control or long-term rate control, and factors such as left ventricular dysfunction and failed rhythm control. Anti-arrhythmic strategies (if required) include electric cardioversion, pharmacological cardioversion (flecainide, amiodarone, sotalol, ibutilide, propafenone and vernakalant), ablation procedures which could be catheter ablation (e.g. radiofrequency, cryoballoon or hybrid ablation—convergent procedure), or surgical ablation. As mentioned earlier, the use of any strategy for rhythm control depends on several factors including the symptoms, severity of AF (according to duration and class), ventricular dysfunction and haemodynamic stability. Studies have shown that rate and rhythm control strategies can reduce cardiovascular morbidities and mortality [9, 10].
In the long term, the key goal of any AF management strategy is to improve modifiable risk factors associated with the condition including lifestyle modification, monitoring and any potential triggers of paroxysmal AF (e.g. excessive alcohol intake). However, these strategies are often considered as secondary or tertiary and are used in combination with other strategies described above [11].
While some cases of AF are paroxysmal or persistent and self-terminate in less than a year with appropriate management, most cases transit to a life-long/permanent condition. This necessitates lifetime management and monitoring of rate control to reduce the increased risk of tachycardia-induced cardiomyopathy and stroke. Although both are very costly, this raise concerns around the cost effectiveness of applied management strategies. As the cost of managing AF is becoming as important as the health outcomes, economic evaluation of treatment strategies to manage AF has become an indispensable tool to inform decision making. This systematic review answers the following research question: What strategies to manage atrial fibrillation among people aged 18 years and above were cost effective in low-, middle- and high-income countries between 2012 and 2022? The outcome of this study will guide decision making in the management of AF amidst several strategies used in different settings to manage the disease.
2 Methods
2.1 Protocol and Registration
The design of this systematic review was in accordance with the recommendation in the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) 2020 statement [12]. Details of the PRISMA checklist are provided in Electronic Supplementary Material (ESM) 1. This review has been registered in the International Prospective Register of Systematic Reviews (PROSPERO), CRD42022360590.
To aid the development of the study design, we did a preliminary assessment of literature using PubMed and Google Scholar to identify studies’ characteristics and methodologies. This helped to define the final inclusion and exclusion criteria used for the search.
2.2 Eligibility Criteria
Studies included in this review were original research on the economic evaluation of AF management strategies. The studies presented cost data and health outcome measure(s) for patients aged 18 years and above. There was no restriction on comorbidities or co-treatment strategies. Full-text articles were included. The studies were limited to humans only, in English language and published between January 2012 and November 2022.
Economic evaluations of other arrhythmias (other than atrial fibrillation) or other cardiac diseases, reviews and commentaries, opinion papers, conference abstracts or proceedings and qualitative reports were excluded. Studies whose costs and health outcomes were estimated using proxied data were also excluded. Studies with incomplete information needed for economic evaluation, and studies that evaluated one DOAC for stroke prevention were excluded, except in the case of mixed treatment strategies. The reason for excluding studies that evaluated a single DOAC was because the four novel DOACs (apixaban, dabigatran, edoxaban and rivaroxaban) were under patency in year 2022. Hence, to eliminate analytical bias of the included studies, we included only studies that evaluated the relative efficiency of at least two DOACs in head-to-head comparisons.
2.3 Information Sources
Based on expert librarians’ recommendations [13] and after an assessment of the health economic core library recommendations by the US National Library of Medicine [14], we searched MEDLINE (OvidSp), Embase, Web of Science, Cochrane Library, EconLit (EBSCOhost) and Google Scholar to identify relevant studies.
2.4 Search Strategy
The search was performed in September 2022. Related ‘search terms’ which include related relevant medical subject headings (MeSH), or related text words (title, abstract and keywords) were combined to form a union (concept cluster). For example, if A, B and C represent related search terms, the union was formed as ‘A or B or C’. Several relevant concept clusters were created. The concept clusters were combined to form an intersection cluster. For example, if D, E and F are concept clusters, they were combined as ‘D and E and F’. The results were then reviewed by looking at the MeSH, subheadings, titles and abstract to check if there are terms that could improve our search. For instance, in our preliminary search, we searched for ‘atrial fibrillation’ and ‘arrhythmia’ which present results with all related headings and subheadings and were combined to form a related MeSH ‘search term’. We then searched for text words like ‘arrhythmia’, ‘dysrhythmia’, and ‘abnormal heart rhythm’ appearing in the title, abstract or keywords, which were combined to form related text words, (search term). Both related ‘search terms’ (MeSH and text words) were combined to form a concept cluster. Details of the search strategies are shown in ESM 2. The MEDLINE search strategy was adapted for search in other databases. Auto-alert systems was set up to provide literature updates while the data extraction and analyses are ongoing. The auto-alert systems were stopped 2 months after the data extraction (November 2022).
2.5 Data Management and Selection Process
All searched results from the six databases were exported into a single EndNote library. A union group was created to contain all the articles from the different databases. De-duplication of studies was performed with EndNote. From the union group, different subgroups to represent exclusion criteria were created. Excluded studies were exported to different exclusion ‘group set’ based on the criteria for exclusion. A study that does not meet the inclusion criteria for multiple reasons was exported to the relevant exclusion ‘group set’ in the order of priority: ‘subject area’, ‘originality’, ‘economic evaluation’ and ‘clarity’ completeness, ‘study from 2012 and beyond’, and more than one DOAC evaluated (in the case of stroke prevention) (see ESM 2).
Selection was performed independently by two reviewers (C.O. and C.A.). A third reviewer (J.B.) overviewed the selections by the first two reviewers and resolved any selection disagreement among the first two reviewers. First, titles were screened followed by the abstracts of original research articles that involve the economic evaluation of atrial fibrillation management strategies. Next, an auto search for the full text of the articles whose abstracts were eligible was initiated. The full text of the potential articles was assessed for costs, health outcomes and clarity of reporting.
2.6 Data Collection Process
An electronic data extraction form was used. Two reviewers (C.O. and C.A.) independently extracted and managed the data from the included studies. Disagreement with the extraction results from the two reviewers that cannot be resolved by them was resolved by the third reviewer (J.B.). The data was collected based on the 2022 International Society for Pharmacoeconomics and Outcome Research (ISPOR) Consolidated Health Economic Evaluation Reporting Standards (CHEERS) guideline [15] (see ESM 2).
2.7 Data Items, Outcomes and Prioritisation
Data was extracted based on the following:
-
(a)
Publication: title, authors, year, study objectives, sample size, gender, setting/country the study was conducted, etc.
-
(b)
Study design: randomised-control trials, cohort studies, case-control studies, cross-sectional studies, type of economic evaluation, time horizon, type of atrial fibrillation, comparators, risk of stroke based on the CHA2DS2-VASc score, etc. A CHA2DS2-VASc score of 0 is ‘low’ risk of stroke, 1 is ‘moderate’ and any score above 1 is a ‘high’ risk.
-
(c)
Cost and outcome measures: cost perspective, quality-adjusted life-years (QALY), discount rate, willingness-to-pay threshold, price year and currency, etc.
-
(d)
Other relevant information, e.g. study assumptions.
2.8 Risk of Bias Assessment
Risk of bias assessment of the individual studies was done at the outcome level using the Consensus Health Economic Criteria (CHEC) checklist designed for conducting economic evaluation-based systematic reviews [16]. This checklist has 19 reporting standards for economic model characteristics, identification and valuation of costs and outcomes, discussion section, conclusions as well as funding and conflicts of interest statement. As the risk of bias tool did not provide thresholds to include or exclude studies for data synthesis, an internally created conservative classification system was used to ensure that only studies with low risk to moderate risk of bias were included in the synthesis. The risk of bias in this scenario was defined as the inappropriateness or failure of a study to conduct or report the applicable items indicated on the risk of bias tool. The risk of bias was measured as a percentage of the failure or inappropriateness. Studies were classified as ‘low risk’ (0–10%), ‘moderate risk’ (11–30%), or ‘high risk’ (> 30%) based on the percentage of applicable items for each study which were not reported or inappropriately reported. Studies with high risk of bias were excluded from the data synthesis. The checklist was completed in duplicate by two members of the review team (C.O. and C.A.). Differences were resolved with the third author (J.B.). Details of the risk of bias assessment is available in the supplementary file 3 (ESM 3).
2.9 Data Synthesis
A narrative synthesis and summary of answers to the research question was performed due to heterogeneities in the identified studies. Such heterogenies emanated from either difference in country’s economic development or treatment goals for managing AF. Hence, the grouping of studies for narrative synthesis was first based on the income level classification by the World Bank [high-income countries (HIC), middle-income countries (MIC) and low-income countries (LIC)]. Studies were then grouped as per the treatment goals including stroke prevention, rate control and rhythm control. The analysis was performed using Microsoft Excel 365 (Microsoft, Seattle, USA). The ICER for each study was adjusted to 2021 USD value following the guidelines of the Campbell and Cochrane Economics Methods Group (CCEGM) and the Evidence for Policy and Practice Information and Coordinating Centre (EPPI-Centre) [17].
3 Results
3.1 Screening and Selection of Studies
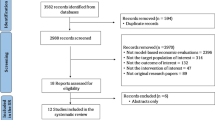
A total of 2019 articles were identified from five databases (Medline, 221; Embase, 1108; Web of Science, 518; Cochrane, 102 and EconLit, 9) and Google Scholar (61 articles). Two potential articles from Medline were identified through the auto alert system but were duplicates. After de-duplication, 1803 articles were available for screening. The studies excluded at the screening phase were moved to exclusion ‘group sets’ based on the reason for exclusion in a hierarchy order described in the methodology. A total of 230 potential articles were available for eligibility check after phase 1 screening. Conference abstracts and studies which had multiple, relevant missing information for economic evaluation were excluded as ‘incomplete information’ studies, while studies with unspecific methodology or analytical approach were excluded as ‘not specific’ studies. At the end of the eligibility assessment, a total of 50 studies met the inclusion criteria. Figure 1 describes the flow diagram of the selection process. The EndNote library (available upon request) summarises the reasons for exclusion of studies.
3.2 Characteristics of the Included Studies
Data were extracted from the included studies as per the data items described in the methodology. All studies were for patients with non-valvular AF. No study was found to evaluate the management strategies of AF in LIC setting. For stroke prevention strategies, 32 studies evaluated the cost effectiveness in HIC [8, 18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48], while seven studies evaluated the cost effectiveness in MIC [49,50,51,52,53,54,55]. Ten studies in HIC [10, 28, 29, 56,57,58,59,60,61,62] and three studies in MIC [63,64,65] evaluated the cost effectiveness of rhythm control strategies. Only one study [10] evaluated the cost effectiveness of rate control strategies in AF management in HIC. Of the 32 studies that evaluated strategies for stroke prevention in HIC, 14 were from North America [8, 25, 26, 28, 29, 31, 32, 37,38,39, 44, 46,47,48], 13 from Europe [18, 19, 22,23,24, 27, 30, 33,34,35, 40, 42, 45], 4 from Asia [21, 29, 43, 47] and 1 from Oceania [28]. The proportion of male sex (52–77%) was higher than the female sex in most of the studies. Five studies from Asia [10, 29, 63,64,65], four from North America [56,57,58,59], two from Oceania [28, 61] and two from Europe [60, 62], respectively evaluated management strategies for rhythm control.
All the studies were cost-utility analyses with QALY as the main outcome measure. All studies were cohort studies with most studies designed using a lifetime horizon. Few studies had a 5-year and 10-year time horizon [28, 29, 45, 52, 57, 61, 65]. Markov models were the principal type of model employed in the assessment of included studies. The design of the model varied across the studies with health states range from 8 to 17 health states. The payer perspective was the most applied costing perspective (68% of the studies), while 24% and 12% of the studies were performed from the provider perspective [20, 23, 25, 33, 34, 36, 43, 47, 55, 58, 61, 64] and societal perspective [10, 19, 23, 31, 51, 53], respectively. Most of the studies (59%) applied an annual discount rate of 3% for both costs and outcomes. Twenty-four per cent of studies applied 3.5% discount rate for both costs and outcomes. Twelve per cent of the studies applied 5% as discount rate for both costs and outcomes, while the remaining studies applied a discount rate of 1.5% for outcomes, and 4% or 4.5% for costs. The willingness-to-pay threshold also varied across the studies. Studies from the USA used a threshold of either $50,000 [25, 28, 38, 39, 46, 47] or $100,000 [8, 19, 26, 39, 58] per QALY gained. Studies from the UK used the National Institute of Health and Clinical Excellence (NICE) recommended threshold between £20,000 and £30,000 per QALY [40, 60, 62]. Other studies in Europe adopted the NICE recommendation but expressed values in Euros or US$ [18, 19, 22,23,24, 27, 30, 34, 35, 40, 42, 45]. Some other studies used government-led guidelines [22, 34, 44], or one to three times the gross domestic product per capita (GDP) of the country citing the World Health Organization [10, 21, 43, 47, 56]. The sample size was hypothetical for most studies, between 1000 and 10,000 patients, while some studies used the sample size from observational data repository or randomised-control trials, with sample sizes ranging from 231 to 212,459 patients [10, 21, 34, 42, 50, 54, 56, 58, 61, 65]. The patients average age was 67 (55–78) years (see Table 1).
Identifying the optimal stroke prevention strategy was the predominant objective of most of the included studies. Evaluated interventions for stroke prevention include warfarin, aspirin, clopidogrel, LMWH, the DOACs (apixaban, dabigatran, rivaroxaban and edoxaban) and left atrial appendage closure (LAAC). Strategies for rhythm control identified in the studies include anti-arrhythmic drugs (atenolol, sotalol, pilsicainide, flecainide, propafenone, dronedarone and amiodarone); catheter ablation, including cryoballoon ablation, radiofrequency catheter ablation (RFCA) and hybrid procedure (convergent procedure). The only study that evaluated a rate control strategy assessed atenolol, propranolol, betaxolol, bevantolol, bisoprolol, diltiazem and verapamil.
3.3 Risk of Bias Assessment
The risk of bias assessment performed using the CHEC list (available in ESM 3) showed that the included studies had low to moderate risk of bias. This was partly due to preliminary assessment done during the studies selection with EndNote library.
3.4 Cost Effectiveness of Treatment Strategies
3.4.1 Stroke Prevention Strategies in High-Income Countries
In patients at low risk of stroke, three out of six studies showed that apixaban was the optimal choice to prevent stroke [30, 37, 40]. These three studies compared warfarin with different DOACs only. Only one study compared warfarin with DOACs, LAAC, clopidogrel and aspirin, and it showed that LAAC was the optimal strategy [33]. Dabigatran was the optimal choice specifically from one study [40], likewise rivaroxaban [43]. Pharmacogenomic-guided warfarin (PG-warfarin) was cost effective when compared with standard warfarin care [41].
In those at moderate risk of stroke, apixaban was the optimal strategy in 11 of 18 included studies [8, 18, 26, 27, 29, 35, 37, 41, 43, 45, 47]. These studies either compared warfarin with DOACs or compared between DOACs, but 1 of the 11 studies compared LAAC with warfarin and DOACs [34]. Dabigatran was the optimal choice in three studies [22, 37, 48], while rivaroxaban [20], edoxaban [39], PG-warfarin [27] and LAAC [24], were the optimal strategies in four different studies.
In those at high risk of stroke, LAAC was the optimal strategy in three of nine studies [31, 36, 38]. Two studies provided evidence that apixaban was the optimal studies, but LAAC was not a comparator in any of the two studies [32, 37]. PG-warfarin and PG-DOAC were the cost-effective choice in two different studies, but were not compared with LAAC [26, 46] (see Table 2).
3.4.2 Rate Control Strategies in High-Income Countries
Only one study was identified to evaluate interventions for rate control [10]. Propranolol was the optimal strategy to control abnormal heart rate due to AF when compared with betaxolol, bevantolol, bisoprolol, diltiazem and verapamil.
3.4.3 Rhythm Control Strategies in High-Income Countries
In patients at low risk of stroke, catheter ablation was the optimal strategy to control heart rhythm in patients with paroxysmal AF when compared with anti-arrhythmic drugs (AADs) alone [56, 62]. Convergent procedure was a more efficient strategy in patients with persistent AF when compared with AAD and catheter ablation [57]. A comparison of AADs alone showed that sotalol was the optimal choice when compared with atenolol, pilsicainide, flecainide, propafenone, dronedarone and amiodarone [10]. Risk factor management (RFM) was cost effective in controlling heart rhythm when compared with no RFM [61].
In patients at moderate risk of stroke, catheter ablation was the optimal strategy to control heart rhythm in patients with paroxysmal or persistent AF when compared with AADs alone [59]. Convergent procedure was the optimal intervention in patients with persistent AF when compared with AADs and catheter ablation [57].
In patients at high risk of stroke, catheter ablation was the optimal strategy to control heart rhythm in patients with paroxysmal, persistent or permanent AF when compared with AADs alone [58, 60]. Convergent procedure was the optimal intervention in patients with persistent AF when compared with AADs and catheter ablation [57] (see Table 2).
3.4.4 Stroke Prevention Strategies in Middle-Income Countries
In patients at low to moderate risk of stroke, apixaban was the optimal choice in three studies [49, 50, 52], which compared it with warfarin, dabigatran, edoxaban and rivaroxaban. Rivaroxaban was the optimal choice in two studies [54, 55] which compared it with apixaban, dabigatran, warfarin and LMWH, while warfarin was the cost-effective strategy in a single study [51].
In patients at high risk of stroke, one study showed that high dose edoxaban (60mg) was the optimal choice [53] (see Table 3).
3.4.5 Rhythm Control Strategies in Middle-Income Countries
In patients at moderate or high risk of stroke with paroxysmal AF, a study which compared AAD with CA showed that CA was the optimal strategy [63]. A study which compared AADs with RFCA and cryoballoon catheter ablation [64], and another study which compared cryoballoon catheter ablation with RFCA [65], both showed that RFCA was the optimal strategy for rhythm control (see Table 3).
A summary of the evidence is provided in Table 4.
4 Discussion
This systematic review evaluated the contemporary available evidence around the optimal management of all subtypes of AF. Data were collected and synthesised from studies conducted over the last decade (2012–2022) in both high- and middle-income countries. Treatment strategies were identified for stroke prevention, rate control and rhythm control. All included studies evaluated non-valvular atrial fibrillation. From this review, apixaban is suggested as the optimal strategy in HIC for stroke prevention in patients with low or moderate risk of stroke, while dabigatran is suggested as a next optimal strategy. In patients at high risk of stroke, LAAC is suggested as an optimal strategy, except where an occlusion procedure is contraindicated in the patients, while PG-guided warfarin is considered as second-line therapy. There is limited evidence to inform the decision to apply rate control. However, based on the available evidence, propranolol was the optimal choice in patients without bronchial asthma, peripheral vascular disease, diabetes mellitus or any other contraindications. In respect to rhythm control, for patients at low to moderate risk of stroke in HIC, catheter ablation is suggested for paroxysmal or persistent AF, while convergent procedure is reserved for persistent to permanent AF. Where catheter ablation or hybrid procedure is contraindicated and AAD is recommended, sotalol is the suggested option. In MICs, there are limited evidence to inform decision making. Available evidence lends priority to the use of apixaban for stroke prevention in patients at low and moderate risk of stroke, followed by rivaroxaban. Where there is substantial financial constraint, warfarin is suggested as the optimal choice. High dose edoxaban is suggested for patients at high risk of stroke, but this recommendation needs to be strengthened with additional evidence. In rhythm control in MICs, radiofrequency catheter ablation is suggested in patients at moderate to high risk of stroke.
This systematic review is the first to holistically evaluate stroke prevention, cardiac rate and cardiac rhythm control strategies in AF management while considering the difference in economic development (whether low-, middle- or high-income country) where management is being applied. We ensured that included studies on stroke prevention evaluated the relative efficiency of two or more DOACs in head-to-head comparisons. The included studies were also recently (within the last decade) conducted economic evaluations.
Previously conducted systematic reviews have shown that for stroke prevention, the DOACs are cost effective, but it is unclear which of the DOAC is most cost effective [66,67,68]. Although, some systematic reviews have indicated that apixaban was the optimal strategy when compared with other DOACs [69, 70]. The findings are similar to the European guideline on AF management which recommends the use of DOACs in patients with one major risk factor or ≥ 2 clinically relevant non-major risk factors; the use DOAC or aspirin in patients with one clinically relevant non-major risk factor with preference for DOAC; and the use of aspirin in patients without risk factors [1]. In rate control, the guideline recommend the use of beta blockers, calcium-channel blockers, digitalis or a combination; also recommending that the choice of medication should be individualized and the dose monitored to avoid bradycardia [1]. The guideline also recommends that catheter ablation be reserved in patients with AF who remain symptomatic despite optimal medical therapy [1]. In MICs, a meta-analysis showed that DOACs were not cost effective compared with VKA [71], but in HICs, DOACs were cost effective. In cardiac rhythm control, a systematic review showed that catheter ablation was not cost effective as a first line compared with AAD as there was insufficient evidence to support the superiority of catheter ablation over AAD [72]. Our systematic review provides additional evidence to the cost effectiveness of DOACs in stroke prevention, with the likelihood of apixaban being the most optimal intervention. Our systematic review also provided supporting evidence that VKA is still potentially cost effective in MICs. However, it provided new evidence that catheter ablation can be cost effective and considered as first line compared with AAD, as opposed to a previous systematic review [72].
The studies included in this review have some important limitations. Most used data from the same clinical trials, which may not be ideal for the population for which the economic evaluation was performed. The trials itself lack head-to-head comparison of interventions. A comparison of one intervention to the standard of care may not provide the optimal treatment strategy because other interventions were not compared. A comparison of multiple treatment strategies is more reliable as it provides evidence on the relative efficiency between the different strategies. Generally, population-specific data were lacking in most studies included in the review. There were very limited studies in the literature that evaluated rate and rhythm control treatment strategies. All these limitations underscore the need for more population-specific clinical trials, head-to-head trials and other relevant population-specific studies to provide more robust data for economic evaluation. The value of information analysis may be pertinent in understanding the value that trials may offer and potentially help to inform their design.
This systematic review, likewise, has some limitations. Based on the available evidence, the recommendations provided here are only suggestive and do not necessarily apply to all settings. Due to limited head-to-head trials, the results from this systematic review indicate the need for more RCTs or potentially real-world evidence approaches on the interventions indicated for AF management to provide stronger evidence, which will in turn be used to conduct new economic evaluations to support decision making. Thus, the results of this review should be interpreted with caution, and treatment should always be individualised and guided by sound clinical evidence. Also, with the varying structure and funding of health systems across the world, heterogeneity in the studies’ characteristics and the limited evidence, a quantitative synthesis of evidence was not considered. The limited number of available studies, especially for cardiac rate and rhythm control, makes it difficult for generalisability of findings. More economic evaluations on rate and rhythm control strategies would provide stronger evidence. Hence, future economic evaluations especially on rate control strategies are necessary. The thresholds for risk of bias classification of the CHEC checklist developed by the authors may not be the best approach and may have some limitations. Hence, caution is needed when using our developed check list as well as the interpretation of our findings. The grouping of studies by income-level classification is not ideal to adequately control for heterogeneity. While grouping by income-level classification may control for heterogeneity in the cost component of the ICER, it does not control for potential heterogeneity in the effectiveness of the interventions which is dependent on several covariates including race, pharmacogenetics, comorbidities, lifestyle, environment, etc. Future studies should also consider a regression analysis to test for the effect of these covariates on the ICER, which may inform the need for subgroup analysis in the future.
5 Conclusions
Based on the available evidence, in high-income countries, the review suggests the use of apixaban in patients at low and moderate risk of stroke, and LAAC in patients at high risk. Propranolol should be considered for rate control in patients without contraindication due to cardioselectivity. Catheter ablation and convergent procedure are suggested in paroxysmal and persistent AF, respectively. In middle-income countries, apixaban is suggested for stroke prevention while warfarin should be considered in the case of financial constraint. Radiofrequency catheter ablation is suggested in rhythm control.
Due to limited clinical trials on AF management strategies, the lack of head-to-head trials (especially on the new oral anti-coagulants), the heterogeneity in clinical characteristic of the trials from which the data used in most of the included studies in this review were derived from, and the variations in the modelling methods amongst the studies, the decision to use any treatment strategy should always be individualised and guided by strong objective and subjective clinical and economic evidence in a multi-disciplinary team setting.
References
Society E, Task A, Members F, Camm AJ, Uk C, Kirchhof P, et al. Guidelines for the management of atrial fibrillation: the task force for the management of atrial fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010;31:2369–429.
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021.
Ball J, Carrington MJ, McMurray JJV, Stewart S. Atrial fibrillation: profile and burden of an evolving epidemic in the 21st century. Int J Cardiol. 2013;167:1807–24.
Soliman EZ, Safford MM, Muntner P, Khodneva Y, Dawood FZ, Zakai NA, et al. Atrial fibrillation and the risk of myocardial infarction. JAMA. 2014. https://doi.org/10.1001/jamainternmed.2013.11912.
Agbor VN, Aminde LN, Tianyi F-L, Mbanga CM, Petnga S-JN, Ditah C, et al. Atrial fibrillation among adults with heart failure in sub-Saharan Africa—prevalence, incidence and all-cause mortality: a systematic review and meta-analysis protocol. BMJ Open. 2019;9:e022320. https://doi.org/10.1136/bmjopen-2018-022320.
Mulder BA, Rienstra M, Van Gelder IC, Blaauw Y. Update on management of atrial fibrillation in heart failure: a focus on ablation. Heart. 2022;108:422–8. https://doi.org/10.1136/heartjnl-2020-318081.
Wu B, Kun L, Liu X, He B. Cost-effectiveness of different strategies for stroke prevention in patients with atrial fibrillation in a health resource-limited setting. Cardiovasc Drug Ther. 2014;28:87–98.
Shah A, Shewale A, Hayes CJ, Martin BC. Cost-effectiveness of oral anticoagulants for ischemic stroke prophylaxis among nonvalvular atrial fibrillation patients. Stroke J. 2016;47:1555–61.
Hagens VE, Vermeulen KM, Tenvergert EM, Van Veldhuisen DJ, Bosker HA, Kamp O, et al. Rate control is more cost-effective than rhythm control for patients with persistent atrial fibrillation—results from the RAte Control versus Electrical cardioversion (RACE) study. Eur Heart J. 2004;25:1542–9.
Kim M, Kim W, Kim C, Joung B. Cost-effectiveness of rate- and rhythm-control drugs for treating atrial fibrillation in Korea. Yonsei Med J. 2019;60:1157. https://doi.org/10.3349/ymj.2019.60.12.1157.
Gao L, Scuffham P, Ball J, Stewart S, Byrnes J. Long-term cost-effectiveness of a disease management program for patients with atrial fibrillation compared to standard care—a multi- state survival model based on a randomized controlled trial. J Med Econ. 2021;24:87–95. https://doi.org/10.1080/13696998.2020.1860371.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. http://www.bmj.com/content/372/bmj.n71.abstract. Accessed 5 Sept 2022.
Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. 2017;6:1–12.
AcademyHealth. Health economics core library recommendations, 2011. 2011. https://www.nlm.nih.gov/nichsr/corelib/hecon-2011.html. Accessed 15 Aug 2022.
Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, et al. Consolidated health economic evaluation reporting standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Pharmacoeconomics. 2022;40:601–9. https://doi.org/10.1007/s40273-021-01112-8.
Evers S, Goossens M, de Vet H, van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: consensus on health economic criteria. Int J Technol Assess Health Care. 2005;21:240–5.
CCEMG and EPPI-Centre. CCEMG—EPPI-Centre Cost Converter v.1.6. 2019 [cited 2020 Mar 15]. https://eppi.ioe.ac.uk/costconversion/default.aspx. Accessed 18 Oct 2022.
Athanasakis K, Karampli E, Tsounis D, Bilitou A, Kyriopoulos J. Cost-effectiveness of apixaban vs. other new oral anticoagulants for the prevention of stroke: an analysis on patients with non-valvular atrial fibrillation in the Greek healthcare setting. Clin Drug Investig. 2015;35:693–705. https://doi.org/10.1007/s40261-015-0321-7.
Canestaro WJ, Patrick AR, Avorn J, Ito K, Matlin OS, Brennan TA, et al. Cost-effectiveness of oral anticoagulants for treatment of atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2013;6:724–31. https://doi.org/10.1161/CIRCOUTCOMES.113.000661.
Escobar Cervantes C, Martí-Almor J, Cabeza AIP, Bowrin K, Llorac Moix A, Genís Gironès M, et al. Real-world cost-effectiveness analysis of NOACs versus VKA for stroke prevention in Spain. PLoS ONE. 2022;17: e0266658. https://doi.org/10.1371/journal.pone.0266658.
Choi JH, Kim W, Kim YT, Cho J, Shin SY, Kim C, et al. Cost-effectiveness of direct oral anticoagulant vs. warfarin among atrial fibrillation patients with intermediate stroke risk. Front Cardiovasc Med. 2022. https://doi.org/10.3389/fcvm.2022.849474/full.
Coyle D, Coyle K, Cameron C, Lee K, Kelly S, Steiner S, et al. Cost-effectiveness of new oral anticoagulants compared with warfarin in preventing stroke and other cardiovascular events in patients with atrial fibrillation. Value Heal. 2013;16:498–506.
de Jong LA, Groeneveld J, Stevanovic J, Rila H, Tieleman RG, Huisman MV, et al. Cost-effectiveness of apixaban compared to other anticoagulants in patients with atrial fibrillation in the real-world and trial settings. PLoS ONE. 2019;14:e0222658. https://doi.org/10.1371/journal.pone.0222658.
Freeman JV, Hutton DW, Barnes GD, Zhu RP, Owens DK, Garber AM, et al. Cost-effectiveness of percutaneous closure of the left atrial appendage in atrial fibrillation based on results from PROTECT AF Versus PREVAIL. Circ Arrhythmia Electrophysiol. 2016. https://doi.org/10.1161/CIRCEP.115.003407.
Harrington AR, Armstrong EP, Nolan PE, Malone DC. Cost-effectiveness of apixaban, dabigatran, rivaroxaban, and warfarin for stroke prevention in atrial fibrillation. Stroke. 2013;44:1676–81. https://doi.org/10.1161/STROKEAHA.111.000402.
Hospodar AR, Smith KJ, Zhang Y, Hernandez I. Comparing the cost effectiveness of non-vitamin k antagonist oral anticoagulants with well-managed warfarin for stroke prevention in atrial fibrillation patients at high risk of bleeding. Am J Cardiovasc Drugs. 2018;18:317–25. https://doi.org/10.1007/s40256-018-0279-y.
Janzic A, Kos M. Cost effectiveness of novel oral anticoagulants for stroke prevention in atrial fibrillation depending on the quality of warfarin anticoagulation control. Pharmacoeconomics. 2015;33:395–408. https://doi.org/10.1007/s40273-014-0246-7.
Kawakami H, Nolan MT, Phillips K, Scuffham PA, Marwick TH. Cost-effectiveness of combined catheter ablation and left atrial appendage closure for symptomatic atrial fibrillation in patients with high stroke and bleeding risk. Am Heart J. 2021;231:110–20.
Kimura T, Igarashi A, Ikeda S, Nakajima K, Kashimura S, Kunitomi A, et al. A cost-utility analysis for catheter ablation of atrial fibrillation in combination with warfarin and dabigatran based on the CHADS 2 score in Japan. J Cardiol. 2017;69:89–97.
Kongnakorn T, Lanitis T, Annemans L, Thijs V, Goethals M, Marbaix S, et al. Stroke and systemic embolism prevention in patients with atrial fibrillation in Belgium: comparative cost effectiveness of new oral anticoagulants and warfarin. Clin Drug Investig. 2015;35:109–19. https://doi.org/10.1007/s40261-014-0253-7.
Labori F, Persson J, Bonander C, Jood K, Svensson M. Cost-effectiveness analysis of left atrial appendage occlusion in patients with atrial fibrillation and contraindication to oral anticoagulation. Eur Heart J. 2022;43:1348–56. https://academic.oup.com/eurheartj/article/43/13/1348/6468857. Accessed 21 Sept 2022.
Lanitis T, Cotté FE, Gaudin AF, Kachaner I, Kongnakorn T, Durand-Zaleski I. Stroke prevention in patients with atrial fibrillation in France: comparative cost-effectiveness of new oral anticoagulants (apixaban, dabigatran, and rivaroxaban), warfarin, and aspirin. J Med Econ. 2014;17:587–98. https://doi.org/10.3111/13696998.2014.923891.
Lee VW-Y, Tsai RB-C, Chow IH-I, Yan BP-Y, Kaya MG, Park J-W, et al. Cost-effectiveness analysis of left atrial appendage occlusion compared with pharmacological strategies for stroke prevention in atrial fibrillation. BMC Cardiovasc Disord. 2016;16:167. https://doi.org/10.1186/s12872-016-0351-y.
Micieli A, Wijeysundera HC, Qiu F, Atzema CL, Singh SM. A decision analysis of percutaneous left atrial appendage occlusion relative to novel and traditional oral anticoagulation for stroke prevention in patients with new-onset atrial fibrillation. Med Decis Mak. 2016;36:366–74. https://doi.org/10.1177/0272989X15593083.
Pradelli L, Calandriello M, Di Virgilio R, Bellone M, Tubaro M. Cost‑effectiveness analysis of apixaban versus other NOACs for the prevention of stroke in Italian atrial fibrillation patients. Farmecon Heal Econ Ther Pathways. 2014;15:101–12. https://journals.seedmedicalpublishers.com/index.php/FE/article/view/971. Accessed 21 Sept 2022.
Reddy VY, Akehurst RL, Amorosi SL, Gavaghan MB, Hertz DS, Holmes DR. Cost-effectiveness of left atrial appendage closure with the WATCHMAN device compared with warfarin or non-vitamin k antagonist oral anticoagulants for secondary prevention in nonvalvular atrial fibrillation. Stroke. 2018;49:1464–70. https://doi.org/10.1161/STROKEAHA.117.018825.
Rognoni C, Marchetti M, Quaglini S, Liberato NL. Apixaban, dabigatran, and rivaroxaban versus warfarin for stroke prevention in non-valvular atrial fibrillation: a cost-effectiveness analysis. Clin Drug Investig. 2014;34:9–17. https://doi.org/10.1007/s40261-013-0144-3.
Saw J, Bennell MC, Singh SM, Wijeysundera HC. Cost-effectiveness of left atrial appendage closure for stroke prevention in atrial fibrillation patients with contraindications to anticoagulation. Can J Cardiol. 2016;32:1355.e9-1355.e14.
Ruiz Vargas E, Sposato LA, Lee SAW, Hachinski V, Cipriano LE. Anticoagulation therapy for atrial fibrillation in patients with Alzheimer’s disease. Stroke. 2018;49:2844–50. https://doi.org/10.1161/STROKEAHA.118.022596.
Verhoef TI, Redekop WK, Hasrat F, de Boer A, Maitland-van der Zee AH. Cost effectiveness of new oral anticoagulants for stroke prevention in patients with atrial fibrillation in two different European healthcare settings. Am J Cardiovasc Drugs. 2014;14:451–62. https://doi.org/10.1007/s40256-014-0092-1.
Verhoef TI, Redekop WK, Langenskiold S, Kamali F, Wadelius M, Burnside G, et al. Cost-effectiveness of pharmacogenetic-guided dosing of warfarin in the United Kingdom and Sweden. Pharmacogenom J. 2016;16:478–84. https://www.nature.com/articles/tpj201641. Accessed 21 Sept 2022.
Walter E, Voit M, Eichhober G. Cost-effectiveness analysis of apixaban compared to other direct oral anticoagulants for prevention of stroke in Austrian atrial fibrillation patients. Expert Rev Pharmacoecon Outcomes Res. 2021;21:265–75. https://doi.org/10.1080/14737167.2020.1798233.
Wang Y, Xie F, Kong MC, Lee LH, Ng HJ, Ko Y. Cost-effectiveness of dabigatran and rivaroxaban compared with warfarin for stroke prevention in patients with atrial fibrillation. Cardiovasc Drugs Ther. 2014;28:575–85. https://doi.org/10.1007/s10557-014-6558-1.
Wong EKC, Belza C, Naimark DMJ, Straus SE, Wijeysundera HC. Cost-effectiveness of antithrombotic agents for atrial fibrillation in older adults at risk for falls: a mathematical modelling study. C Open. 2020;8:E706–14. https://doi.org/10.9778/cmajo.20200107.
Wu Y, Zhang C, Gu Z-C. Cost-effectiveness analysis of direct oral anticoagulants vs. vitamin k antagonists in the elderly with atrial fibrillation: insights from the evidence in a real-world setting. Front Cardiovasc Med. 2021. https://doi.org/10.3389/fcvm.2021.675200/full.
You JH. Universal versus genotype-guided use of direct oral anticoagulants in atrial fibrillation patients: a decision analysis. Pharmacogenomics. 2015;16:1089–100. https://doi.org/10.2217/pgs.15.64.
Zhao YJ, Lin L, Zhou HJ, Tan KT, Chew AP, Foo CG, et al. Cost-effectiveness modelling of novel oral anticoagulants incorporating real-world elderly patients with atrial fibrillation. Int J Cardiol. 2016;220:794–801.
Zheng Y, Sorensen SV, Gonschior A-K, Noack H, Heinrich-Nols J, Sunderland T, et al. Comparison of the cost-effectiveness of new oral anticoagulants for the prevention of stroke and systemic embolism in atrial fibrillation in a UK setting. Clin Ther. 2014;36:2015-2028.e2.
Liao C-T, Lee M-C, Chen Z-C, Ku L-JE, Wang J-D, Toh HS. Cost-effectiveness analysis of oral anticoagulants in stroke prevention among patients with atrial fibrillation in Taiwan. Acta Cardiol Sin. 2020;36:50–61.
Liu C-Y, Chen H-C. Cost-effectiveness analysis of apixaban, dabigatran, rivaroxaban, and warfarin for stroke prevention in atrial fibrillation in Taiwan. Clin Drug Investig. 2017;37:285–93. https://doi.org/10.1007/s40261-016-0487-7.
Dilokthornsakul P, Nathisuwan S, Krittayaphong R, Chutinet A, Permsuwan U. Cost-effectiveness analysis of non-vitamin k antagonist oral anticoagulants versus warfarin in Thai patients with non-valvular atrial fibrillation. Hear Lung Circ. 2020;29:390–400.
Mendoza JA, Silva FA, Rangel LM. Cost-effectiveness of new oral anticoagulants and warfarin in atrial fibrillation from adverse events perspective. Rev Colomb Cardiol. 2019;26:70–7. https://rccardiologia.com/previos/RCC2019Vol.26/RCC_2019_26_2_MAR-ABR/RCC_2019_26_2_70-77.pdf. Accessed 21 Sept 2022.
Rattanachotphanit T, Limwattananon C, Waleekhachonloet O, Limwattananon P, Sawanyawisuth K. Cost-effectiveness analysis of direct-acting oral anticoagulants for stroke prevention in Thai patients with non-valvular atrial fibrillation and a high risk of bleeding. Pharmacoeconomics. 2019;37:279–89. https://doi.org/10.1007/s40273-018-0741-3.
Sun K-X, Cui B, Cao S-S, Huang Q-X, Xia R-Y, Wang W-J, et al. Cost-effectiveness analysis of direct oral anticoagulants versus vitamin K antagonists for venous thromboembolism in China. Front Pharmacol. 2021. https://doi.org/10.3389/fphar.2021.716224/full.
Zhou H, Nie X, Jiang M, Dong W. Cost-effectiveness of anticoagulants for preventing stroke in patients with non-valvular atrial fibrillation in mainland China. J Clin Pharm Ther. 2022;47:523–30. https://doi.org/10.1111/jcpt.13575.
Khaykin Y, Mallow PJ, Rizzo JA, Verma A, Chun L, Olesovsky S, et al. Cost-effectiveness of catheter ablation versus antiarrhythmic drug therapy for the treatment of atrial fibrillation: a Canadian perspective. J Heal Econ Outcomes Res. 2016;3:1–12. http://jheor.org/article/9837
Anderson LH, Black EJ, Civello KC, Martinson MS, Kress DC. Cost-effectiveness of the convergent procedure and catheter ablation for non-paroxysmal atrial fibrillation. J Med Econ. 2014;17:481–91. https://doi.org/10.3111/13696998.2014.911185.
Chew DS, Li Y, Cowper PA, Anstrom KJ, Piccini JP, Poole JE, et al. Cost-effectiveness of catheter ablation versus antiarrhythmic drug therapy in atrial fibrillation: the CABANA randomized clinical trial. Circulation. 2022;146:535–47. https://doi.org/10.1161/CIRCULATIONAHA.122.058575.
Lau D, Sandhu RK, Andrade JG, Ezekowitz J, So H, Klarenbach S. Cost-utility of catheter ablation for atrial fibrillation in patients with heart failure: an economic evaluation. J Am Heart Assoc. 2021. https://doi.org/10.1161/JAHA.120.019599.
Leung LWM, Imhoff RJ, Marshall HJ, Frame D, Mallow PJ, Goldstein L, et al. Cost-effectiveness of catheter ablation versus medical therapy for the treatment of atrial fibrillation in the United Kingdom. J Cardiovasc Electrophysiol. 2022;33:164–75. https://doi.org/10.1111/jce.15317.
Pathak RK, Evans M, Middeldorp ME, Mahajan R, Mehta AB, Meredith M, et al. Cost-effectiveness and clinical effectiveness of the risk factor management clinic in atrial fibrillation. JACC Clin Electrophysiol. 2017;3:436–47.
Reynolds MR, Lamotte M, Todd D, Khaykin Y, Eggington S, Tsintzos S, et al. Cost-effectiveness of cryoballoon ablation for the management of paroxysmal atrial fibrillation. EP Eur. 2014;16:652–9. https://doi.org/10.1093/europace/eut380.
Du X, He X, Jia Y, Wu J, Long D, Yu R, et al. A long-term cost-effectiveness analysis comparing radiofrequency catheter ablation with antiarrhythmic drugs in treatment of Chinese patients with atrial fibrillation. Am J Cardiovasc Drugs. 2019;19:569–77. https://doi.org/10.1007/s40256-019-00349-1.
Hu M, Han Y, Zhao W, Chen W. Long-term cost-effectiveness comparison of catheter ablation and antiarrhythmic drugs in atrial fibrillation treatment using discrete event simulation. Value Heal. 2022;25:975–83.
Sun X-R, He S-N, Lin Z-Y, Zhang L, Wang Y-J, Zeng L-J, et al. Radiofrequency catheter ablation versus cryoballoon ablation in the treatment of paroxysmal atrial fibrillation: a cost-effectiveness analysis in China. Clin Ther. 2019;41:78–91.
Coleman CI, Baker WL, Limone BL. Cost-effectiveness of newer anticoagulants for stroke prevention in atrial fibrillation: a systematic literature review. Value Heal. 2013;16:A287.
Costa S, Ramos JC, Braga AC, Pereira J. Stroke prevention in non-valvular atrial fibrillation: systematic review of cost-effectiveness studies. Value Heal. 2013;16:A531.
Ferreira J, Mirco A. Revisão sistemática das análises custo-efetividade dos novos anticoagulantes orais na prevenção do acidente vascular cerebral na fibrilhação auricular. Rev Port Cardiol. 2015;34:179–91.
Al Mukdad M, Al-Badriyeh D, Elewa HF. Cost-effectiveness evaluations among the direct oral anticoagulants for the prevention and treatment of venous thromboembolism: systematic review. Clin Appl Thromb. 2019;25:107602961984910. https://doi.org/10.1177/1076029619849103.
Pinyol C, Cepeda JM, Roldan I, Roldan V, Jimenez S, Gonzalez P, et al. A systematic literature review on the cost-effectiveness of apixaban for stroke prevention in non-valvular atrial fibrillation. Cardiol Ther. 2016;5:171–86. https://doi.org/10.1007/s40119-016-0066-2.
Noviyani R, Youngkong S, Nathisuwan S, Bagepally BS, Chaikledkaew U, Chaiyakunapruk N, et al. Economic evaluation of direct oral anticoagulants (DOACs) versus vitamin K antagonists (VKAs) for stroke prevention in patients with atrial fibrillation: a systematic review and meta-analysis. BMJ Evid-Based Med. 2022;27:215–23. https://doi.org/10.1136/bmjebm-2020-111634.
Neyt M, Van Brabandt H, Devos C. The cost-utility of catheter ablation of atrial fibrillation: a systematic review and critical appraisal of economic evaluations. BMC Cardiovasc Disord. 2013;13:78. https://doi.org/10.1186/1471-2261-13-78.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
Data used in the study are provided in the supplementary file.
Competing interest
Charles Okafor, Joshua Byrnes, Simon Stewart, Paul Scuffham and Clifford Afoakwah have no conflict of interest to declare.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. CA received funding support from the Griffith University Health Group Seed Grant. SS is supported by the NHMRC of Australia (GNT1135894) and PS was the recipient of a NHMRC Fellowship (GNT1136923).
Authors’ contributions
CO, CA and JB developed the study design. CO and CA were responsible for data collection and extraction. CO undertook the data analyses and led the preparation of the initial draft. All authors (CO, JB, SS, PS and CA) contributed to the interpretation of results and drafting the manuscript. All authors reviewed the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Okafor, C., Byrnes, J., Stewart, S. et al. Cost Effectiveness of Strategies to Manage Atrial Fibrillation in Middle- and High-Income Countries: A Systematic Review. PharmacoEconomics 41, 913–943 (2023). https://doi.org/10.1007/s40273-023-01276-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-023-01276-5