Abstract
Background
The HIV epidemic remains a major public health problem. Critical to transmission control are HIV prevention strategies with new interventions continuing to be developed. Mathematical models are important for understanding the potential impact of these interventions and supporting policy decisions. This systematic review aims to answer the following question: when a new HIV prevention intervention is being considered or designed, what information regarding it is necessary to include in a compartmental model to provide useful insights to policy makers? The primary objective of this review is therefore to assess suitability of current compartmental HIV prevention models for informing policy development.
Methods
Articles published in EMBASE, Medline, Econlit, and Global Health were screened. Included studies were identified using permutations of (i) HIV, (ii) pre-exposure prophylaxis (PrEP), circumcision (both voluntary male circumcision [VMMC] and early-infant male circumcision [EIMC]), and vaccination, and (iii) modelling. Data extraction focused on study design, model structure, and intervention incorporation into models. Article quality was assessed using the TRACE (TRAnsparent and Comprehensive Ecological modelling documentation) criteria for mathematical models.
Results
Of 837 articles screened, 48 articles were included in the review, with 32 unique mathematical models identified. The substantial majority of studies included PrEP (83%), whilst fewer modelled circumcision (54%), and only a few focussed on vaccination (10%). Data evaluation, implementation verification, and model output corroboration were identified as areas of poorer model quality. Parameters commonly included in the mathematical models were intervention uptake and effectiveness, with additional intervention-specific common parameters identified. We identified key modelling gaps; critically, models insufficiently incorporate multiple interventions acting simultaneously. Additionally, population subgroups were generally poorly represented—with future models requiring improved incorporation of ethnicity and sexual risk group stratification—and many models contained inappropriate data in parameterisation which will affect output accuracy.
Conclusions
This review identified gaps in compartmental models to date and suggests areas of improvement for models focusing on new prevention interventions. Resolution of such gaps within future models will ensure greater robustness and transparency, and enable more accurate assessment of the impact that new interventions may have, thereby providing more meaningful guidance to policy makers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This review synthesised the current compartmental models for modelling prevention interventions for HIV disease into a general framework. |
We identified key modelling gaps; including that models insufficiently incorporated multiple interventions acting simultaneously, population subgroups were generally poorly represented, and inappropriate data was often utilised in model parameterisation. |
Resolution of such gaps within future models will enable more accurate assessment of the impact that new interventions may have, thereby providing more meaningful guidance to policy makers. |
1 Introduction
Human immunodeficiency virus (HIV) weakens the immune system leaving individuals vulnerable to opportunistic infections, including tuberculosis (TB), severe bacterial infections, and some cancers [1, 2]. In 2019, 1.7 million people were newly infected with HIV [3]. Current global strategies to reduce HIV transmission focus on prevention strategies, targeted to individuals at high risk for HIV [4]. However, despite an array of effective HIV prevention tools, uptake remains sub-optimal due to barriers along the HIV prevention continuum, such as low HIV risk perception [5], accessing services [6], and stigma [3, 5].
New HIV prevention strategies continue to be developed to best meet users’ needs. Multiple forms of long-acting pre-exposure prophylaxis (PrEP) products are under development and investigation; in 2021, the World Health Organization (WHO) recommended the dapivirine vaginal ring for women at high risk for HIV [7] and the US Food and Drug Administration (FDA) granted a Priority Review for injectable cabotegravir long-acting PrEP [8]. Recent years have seen promising advancements in developing HIV vaccines [9, 10], including some testing mRNA delivery of HIV vaccine antigens (NCT05001373). In addition, proof of concept has been established that broadly neutralising antibodies (bNAbs)—a promising HIV vaccine candidate—delivered as passive immunisation can protect humans against infection if the infecting strain is sensitive to the bNAb [11]. Engineered bNAbs with enhanced potency and half-life can potentially prevent infection for up to 6 months [12, 13]. The impacts of new technologies are not dependent on efficacy alone, but on acceptability and uptake as well, as is the case with oral PrEP [14].
Mathematical models can be important tools in assessing the potential of interventions to prevent infection and can consequently guide policy making [15, 16], particularly in situations where ethical or logistical concerns make real-life assessments impractical [16]. One category of models, compartmental models, are commonly utilised to study infectious diseases and identify strategies for disease control [17, 18]. In compartmental models, each individual in a population can only be in one group or compartment (for example, uninfected men aged 20–30 years with more than ten sexual partners per year not taking PrEP), with the total population being the sum of all the compartments. These models are dynamic, whereby the rate of infection for susceptible individuals varies according to the proportion infectious in the population at a given time [19, 20]. Numerical solution of these models can either be deterministic (in which chance events are ignored) or stochastic (in which events happen randomly at different rates). Compartmental models have been widely used to understand the potential impact of prevention interventions in HIV and other infectious diseases, and can play an important role in priority setting [21, 22]. Alternative modelling approaches exist, for example the more complex individual-based models where individuals are represented as a single entity [23]. However, such models are relatively less commonly utilised in published literature for HIV prevention modelling compared with compartmental models, and reproducibility of such models can be challenging [24].
Given the useful insights compartmental models can provide as new HIV prevention interventions are created, and the availability of compartmental models in published literature, we conducted a systematic review aimed at answering the following question: when a new HIV prevention intervention is being considered or designed, what information regarding it is necessary to include in a compartmental model to provide useful insights to policy makers?
To our knowledge, no previous reviews have explored this question. An HIV model review undertaken in 2011 [15] focused on key findings emerging from existing models with limited discussion of what structures (model compartments and stratification) or parameters may be utilised for future models. Other reviews have focused on specific prevention strategies, including PrEP [25], vaccination [26], and test-and-treat [27], and also omitted important considerations for robust infectious disease modelling.
Consequently, our objectives in this study were to (i) identify what HIV intervention structures—compartments, strata—and parameters are currently considered for reducing HIV incidence and how they are incorporated into compartmental models; (ii) assess the models for quality using the TRACE (TRAnsparent and Comprehensive Ecological modelling documentation) tool [28]; and (iii) identify gaps where important features of interventions are not currently represented in models. Given the current focus on HIV vaccination development, alongside new PrEP-based products and other technologies, the review scope was compartmental models capable of modelling prevention technologies in the future (e.g., bNAbs) and more specifically primary HIV prevention methods.
2 Methods
2.1 Protocol and Registration
We performed a review of published literature which adhered to the PRISMA systematic review guidance [29]. No protocol was prepared or published prior to the start of the review.
2.2 Inclusion and Exclusion Criteria
Articles published in English in the last 5 years were eligible (time limitation was set to ensure current/relevant models identified), with no restriction on countries included. Studies modelling sexual, vertical, and/or intravenous HIV transmission were included, representing the main modes of transmission [30, 31]. Three interventions were analysed: (i) circumcision (both voluntary male circumcision [VMMC] and early-infant male circumcision [EIMC]), (ii) PrEP, and (iii) HIV vaccinations (including bNAbs and other candidate HIV vaccines). This covered several modes of delivery (surgery, oral, injection [both healthcare- and self-administered]), preparation (physical/anatomical, biological, immunological), and administration frequencies (one-off, daily or on demand, at timed intervals, long-acting). In terms of mathematical model requirements, we included models which met all the following requirements: (1) were compartmental models, due to their appropriateness for population-level modelling of infectious diseases, (ii) were dynamic models, to enable analysis of the indirect effects of interventions, and (iii) were expressed as ordinary differential equations to allow comparisons between the models. We also only included models where the differential equations demonstrating inclusion of HIV prevention technologies were defined and supplied in the main text, supplementary information, or referenced documents, to allow the model to be analysed and results reproduced.
We excluded studies if they modelled within-host disease or drug dynamics. Animal studies and studies with no mathematical models were omitted. We also excluded conference abstracts, review articles, letters to the editor, and commentaries. Finally, models analysing sexually transmitted infections (STIs) other than HIV were excluded.
2.3 Search Strategy and Selection Criteria
Searches were performed on 15 July 2020 in four databases: Medline, Embase, Global Health, and Econlit. Searches using free text and headings were developed from permutations of the following terms: HIV AND (PrEP OR Circumcision OR vaccination) AND modelling (Online Resource 1, see electronic supplementary material [ESM]). The terms pertaining to mathematical models were non-specific to compartmental models to reduce risk of incorrect removal. Articles were reviewed and screened by RG and described using a PRISMA flow diagram [29]. Duplicates were removed; papers were then assessed for applicability against inclusion and exclusion criteria by sequentially assessing the title, followed by the abstract, and finally the full text.
2.4 Data Extraction and Synthesis
Data were extracted from the main text, supplementary material, and where necessary model equations from studies referenced in the main text. We extracted data on the study design (setting; population; model type; interventions modelled; modes of HIV transmission; costs or cost-effectiveness inclusion; drug resistance/risk compensation modelling; and uptake targeting by subgroup and outcomes) and model structure (interventions; onward transmission impact; adherence; parameter inclusion [including costs]; details of compartments and strata; and force of infection). A narrative synthesis was conducted to synthesise the main findings, with a thematic analysis approach used to identify key domains for review, whereby the author became familiar with the literature to develop themes and focus the review. In addition, a summary of model parameters and percentage of articles reviewed which include each parameter, dependent on article quality, was developed. Parameters were considered important to model developers if present in over 50% of included articles.
2.5 Quality Assessment
Models were evaluated for conformity to the TRACE guidelines [28] against eight criteria deemed appropriate for good practice in model development. Intervention coverage methodology (i.e., how coverage was determined in the models) was considered out of scope for critical evaluation, given the various processes, such as cost and intervention availability, that contribute to this. The TRACE guidelines aimed to assess quality in terms of problem formulation, model description, data evaluation, conceptual model, implementation verification, model output verification, model analysis, and model output corroboration. A traffic light system was developed alongside each criterion (see Online Resource 2 in the ESM). Assessment was made purely on the published material.
3 Results
Following the removal of duplicates, 837 articles were screened for relevance. As per the PRISMA flow diagram (Fig. 1), 335 articles were excluded based on title, with most studies not relevant to HIV. We also excluded 302 articles by abstract, with these articles including mostly conference abstracts, animal studies or in vivo studies. Of the remaining 200 full-text articles reviewed, 48 articles met the eligibility criteria. The main reasons for exclusion were that dynamic compartmental models were not utilised, or differential equations were not published.
3.1 Study Characteristics
3.1.1 Interventions
Forty articles modelled PrEP (83%), 26 articles modelled circumcision (either VMMC or EIMC) (54%), and five articles modelled preventative vaccination (10%). Many PrEP studies did not specify the type of PrEP formulation considered (n = 17). Oral PrEP was the most reported formulation of PrEP (n = 8), with alternative formulations including delivery through long-acting injectables [32,33,34] and vaginal rings [35]. For vaccines, two studies reviewed two or more vaccine types. One study considered three vaccine preparations (bNAbs, P5-like vaccines, idealised vaccines) [36], while another study assessed non-specific and clade-specific vaccines [37].
Only five articles solely modelled one intervention, in all cases this was circumcision. Additional interventions modelled alongside HIV prevention included antiretroviral treatment (ART) (n = 43, 90%) HIV testing (n = 12, 25%), risk reduction for people using drugs or stimulants (n = 4, 8%) [38,39,40,41], female injectable contraceptives (n = 1, 2%) [34], and gonorrhoea treatment (n = 1, 2%) [42].
3.1.2 Settings and Populations
More studies (n = 31, 65%) were based in low-and-middle-income countries (LMIC) than high-income countries (HIC) (n = 14, 29%), whilst some were based in multiple countries (across differing income categories) [37, 41, 43]. Fifteen articles modelled heterosexual transmission, 15 modelled only transmission among men who have sex with men (MSM), and four articles modelled transmission in the general population [43,44,45,46], for example modelling the sexually active population [46]. One article modelled transgender female sex workers (FSW), cis-MSM, cis-FSW, and transgender women not involved in sex work [40], whilst one model considered transgender female sex workers, their clients and regular partners [47]. Two articles modelled MSM and heterosexual populations [48, 49] with six papers also including FSWs [41, 50,51,52,53,54]. One paper included MSM in San Francisco and the general population in South Africa [37]. Two articles modelled serodiscordant couples [55, 56] and one article modelled citizens of Botswana and migrants in Botswana [57]. Among LMICs, the majority of studies considered heterosexual HIV transmission (20/31, 65%), whereas heterosexual transmission was considered in only 2/14 studies (14%) based in HICs and MSM transmission was considered in all HIC studies (14/14, 100%) (Fig. 2).
3.1.3 Modelling Methods
Thirty-two unique HIV models were identified. Nine models were included in at least two articles and were developed further to include new subgroups. Models using identical structures were also parameterised for different settings [58,59,60,61,62,63] or drug preparations [32, 33, 35]. Almost all models were deterministic; only one used a stochastic approach [64]. Three studies used the Optima HIV model, which incorporates multiple interventions and modes of transmission [41, 54, 57], whilst one study compared outcomes across three alternative models [50, 52]. All studies included sexual transmission, with a few models also modelling additional modes of transmission via sharing of intravenous needles [48, 49], vertical transmission [56], and both intravenous and vertical transmission [41, 54, 57]. Outcomes considered included infections averted, total costs, costs per infection averted, disability-adjusted life-years (DALYs) averted, and incremental cost-effectiveness ratios.
For a full list of characteristics by study, see additional files (Online Resource 3 [ESM]).
3.2 Quality Assessment
Online Resource 4 provides the traffic light assessment for each study against the eight TRACE criteria [28], with green, yellow, and red indicating that the criteria was respectively met, somewhat met, and insufficiently met (see ESM). The median number of red criteria per article was 2.0 (range 1–5), and the median number of green was 4.5 (range 2–7).
All studies provided a well justified and clearly stated research question, with over half (n = 25) of the studies deemed appropriate for answering the research questions. Shortcomings included over-simplification of HIV disease progression, insufficient regard for heterogeneity, and omission of ART use. Data quality in most studies (n = 32, 67%) was deemed only partially adequate; although most studies referenced parameters, with few relying heavily on expert opinion, they were often not relevant to the population under review. Demographic data were also not always clearly referenced. Most studies included parameter calibration (n = 45, 94%) and sensitivity analysis (n = 39,81%) but uncertainty ranges were sometimes not reported. No articles included information regarding software testing and documentation and only a few studies (n = 5, 10%) validated their predictions with other data.
3.3 Model Characteristics for Pre-Exposure Prophylaxis (PrEP)
Online Resource 5 Presents the model characteristics considered in the analysis (see ESM).
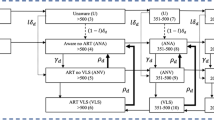
3.3.1 Model Structure to Incorporate PrEP
PrEP interventions were largely incorporated in models by moving susceptible people into a compartment or stratum at a set rate to represent PrEP use (n = 32, 80%). Alternatively, some studies (n = 8, 20%) included PrEP users only in the infection rate by factoring directly into the force of infection equation the proportion of the population taking PrEP and its impact on infection risk. People infected with HIV whilst receiving PrEP generally moved through subsequent infected stages alongside those infected whilst not on PrEP (n = 28, 70%). Alternatively, studies where infected PrEP users remained segregated following infection were able to incorporate supplementary factors such as increased testing for infected PrEP users (n = 9, 23%) and altered infectiousness levels for infected PrEP users to transmit HIV transmission (n = 7, 18%)
3.3.2 Modelling PrEP Uptake and Use
Uptake and drop-out rates for PrEP use were common parameters allowing movement between compartments or strata. Uptake was often set at a pre-determined rate to continue indefinitely or vary dependent on a fixed level of coverage (the percentage of susceptible individuals receiving PrEP) (n = 26, 65%); for example, one paper varied PrEP uptake rate so it was slower as coverage level approached target coverage [65]. Stratification of different population groups was sometimes performed to analyse the impact of targeting PrEP to subgroups (n = 34, 85%), commonly defined by age, sex, sexual preferences, and HIV risk. Less frequent parameters included the proportion of the population eligible for PrEP (n = 5, 13%, 3 models) [39, 51, 65,66,67], time when PrEP commenced (n = 6, 15%), and, for models accounting for infections while using PrEP, the HIV testing rate and rate of disease progression (n = 10, 25%).
As non-oral PrEP preparations provide persistent levels of protection, loss of protection for such delivery methods was incorporated in treatment drop-out or average treatment duration (n = 3, 8%) across one model [32, 33, 35]. Two articles (5%) utilising variations of one model [32, 33] reviewed the impact of extending the period at which drug levels persist at effective levels, thus continuing protection despite drop-out.
3.3.3 Modelling PrEP Impact on the Rate of Infection
The effect of PrEP on reducing HIV acquisition rate through sexual transmission was incorporated directly in the rate of infection or as a multiplier of it. Most studies (n = 38, 95%) included an efficacy parameter, which reduced susceptibility for those in the PrEP compartment or stratum through a reduction in overall rate of infection, or risk per sex act. The rare exception used in two models assumed complete protection, thus removing PrEP users from risk of infection (n = 2, 5%) [42, 68]. Five studies (13%) [41, 48, 49, 54, 57] utilising two models additionally considered acquisition risks through intravenous needle sharing.
Many studies did not account for PrEP adherence. Where this was considered (n = 14, 35%), approaches included incorporating adherence parameters by directly reducing risk of infection as seen in two models (n = 2, 5%) [53, 66] or stratifying PrEP users by adherence levels with accompanying forces of infection (n = 6, 15%). One model utilised across two studies (n = 2, 5%) [36, 69] assumed perfect adherence but varied intervention coverage rates to reflect imperfect use, whilst another incorporated adherence in their PrEP efficacy value (n = 1, 3%) [64]. One model included residual protection against HIV for a heterosexual population, whereby an individual missing a dose of PrEP will continue to have some level of protection, with the protection level dependent on adherence [65].
For injectable PrEP, rather than considering adherence, one model utilised in two studies (n = 2, 5%) [33, 35] included a reliability parameter representing the proportion of injections successful in yielding efficacious drug levels, with stratification of individuals with successful and unsuccessful injections and differences in applied force of infection.
A limited number of models (n = 6, 15%) incorporated the impact of PrEP on drug resistance levels, with varying model complexity. A more complex approach altered PrEP efficacy dependent on whether a drug-sensitive or drug-resistant HIV strain was being transmitted [70]. Only five models considered risk compensation (n = 5, 13%) [38, 42, 56, 71, 72]; those that did altered rates of condom use, sexual partners, and HIV testing. One study modelled increased gonorrhoea risk by incorporating compartments for gonorrhoea infection [42].
3.3.4 Modelling Costs of PrEP Use
Twenty-four studies (60%) assessed cost and cost effectiveness of PrEP. Costs included varied by study, from direct costs exclusively to indirect costs and productivity losses. Cost-effectiveness studies often incorporated cost savings due to HIV infections averted and reduced ART use (n = 7, 18%).
3.4 Model Characteristics for Circumcision
3.4.1 Model Structure to Incorporate Circumcision
The majority of models (n = 15, 58%) modelled circumcision taking place prior to entering the model in addition to circumcision of individuals within the model, with models generally having a set fraction of the population entering the model already circumcised and also a circumcision rate parameter to enable stratification of males by circumcision status. Alternatively, two models across two articles modelled circumcision taking place only prior to individuals entering the model (n = 2, 8%), either at birth [56] or prior to sexual debut [35], with both stratifying the population into circumcised or not with no circumcision rate parameter. Several articles (n = 9, 35%) did not explicitly state whether circumcision was occurring prior to entering the model or for individuals within the model; the majority of these (n = 6, 23%) across three models [45, 55, 61,62,63] altered the risk of infection to consider the proportion of males circumcised, whilst one model (n = 3, 12%) stratified males into circumcised or not and altered the risk of infection to consider the probability an individual undertaking a sexual act is circumcised [41, 54, 57].
3.4.2 Modelling Circumcision Uptake
One method for incorporating circumcision uptake was by stratifying males into circumcision status prior to entering the model, for example stratifying individuals at birth (n = 2, 8%) [35, 56]. Alternatively, models considered circumcising males following entry into the model, at a pre-determined rate (n = 15, 58%); with circumcision rate either continuing indefinitely or varying dependent on level of coverage (percentage of males circumcised). Stratification enabled targeting of subgroups (n = 13, 50%) defined by age, sexual risks, sexual preferences, and geographical location. Several models utilised stratification by HIV status to set whether circumcision could take place in the susceptible population only (n = 9, 35%) or whether infectious individuals in addition to susceptible individuals could be eligible (n = 12, 46%). Additionally, models stratifying by sexual risk were able to set eligibility as HIV-negative and high sexual risk individuals only [58], whilst one model utilised across two studies also stratified by age to emulate reaching circumcision targets defined by age group [61, 62].
3.4.3 Modelling Circumcision Impact on the Rate of Infection
Reduction of HIV acquisition rate due to circumcision was included in all models directly in the rate of infection or as a multiplier of it. Some studies utilised strata to limit the protective effect dependent on sexual positioning (n = 3, 12%, one model) [41, 54, 57], sexual orientation (n = 5,19%, two models) [36, 51, 65, 67, 69], or time period since circumcision surgery (to account for a wound healing period) (n = 2, 8%, one model) [65, 67]. One model weighted the transmission probability per sexual act in the force of infection by the fraction of time spent in wound healing [58]. One model alone incorporated the reduced transmission risk due to circumcision (n = 3,12%) [58,59,60] into the force of infection, by stratifying males by circumcision status in the infectious stages of disease. One model incorporated risk compensation by increasing the rate of partner change in the force of infection for circumcised men (n = 3, 12%) [58,59,60].
3.4.4 Modelling Costs of Circumcision
Only 11 studies (42%) assessed cost or cost effectiveness of circumcision. Included costs varied, from fixed and variable costs, to costs per surgical method used, to varying costs by age.
3.5 Model Characteristics for Vaccination
3.5.1 Model Structure to Incorporate Vaccinations
Vaccines were included in some models through incorporation of a vaccinated stratum or compartment. Some studies additionally incorporated a compartment for individuals vaccinated and also receiving PrEP [71] with an annual rate of dropping PrEP if vaccinated and compartments for different vaccine types [37]. One model segregated individuals as having a high or low immune response following vaccination, and included a complex structure involving 13 compartments for vaccinated individuals [46].
3.5.2 Modelling Vaccination Uptake
Numerous approaches, including continuous vaccination versus mass vaccination campaigns [46], were used to model vaccine uptake. Assumptions around uptake varied, including setting uptake rates to meet a defined level of coverage [36, 46], moving a fraction of susceptible individuals directly into the vaccination compartment after a certain time period [46], or varying uptake rate dependent on the number of people already vaccinated [43]. Some models incorporated targeted vaccination of subgroups based on age, sex, and sexual risk [36, 71] with a simple approach stratifying sexual risk as low or high [71] and a more complex approach stratifying by FSW and low, medium, or high sexual risk for males and females [36].
Some models did not consider vaccination drop-out (n = 3, 60%). Models that did consider retention incorporated a rate of loss of protection [37] or returned individuals to the susceptible compartment after a defined time period [46].
Two models (n = 2,40%) considered more than one vaccine type or preparation (e.g., bNAbs, P5-like vaccines, idealised vaccines) and varied uptake and efficacy by vaccine type.
3.5.3 Modelling Vaccination Impact on the Rate of Infection
Reduction of HIV acquisition rate due to vaccination was included in all models directly in the rate of infection or as a multiplier of it. However, all models assumed vaccine efficacy due to the lack of available evidence. Some studies varied efficacy based on the choice of vaccination (n = 2,40%). A minority of models were more complex, accounting for different levels of immune response over time [46] or modelling risk compensation following vaccination by varying condom use for vaccinated individuals [37, 71].
3.5.4 Modelling Costs of Vaccination
Models (n = 3, 60%) considered vaccine costs using the cost per vaccination schedule [71], per vaccine [46] or per person per year [36]. One study purely considered the savings from ART costs avoided [37].
For a full list of characteristics by study, please see additional files (Online Resource 6) in the ESM.
3.6 Combined HIV Prevention Interventions
In instances where multiple prevention interventions could be efficacious in reducing acquisition risk for individuals within a compartment, numerous models (n = 5, 10%) calculated the combined impact as the product of each intervention’s efficacy when acting independently, with multiple approaches to this. For example, one model included the following formula within the wider risk of infection equation to calculate the combined efficacy of PrEP, condoms, and circumcision:
[1-PrEP efficacy against HIV(%)] × [1-circumcision efficacy against HIV acquisition(%)] × [1-effectiveness of condoms for HIV prevention(%)] [35].
This results in a smaller rate of infection where multiple preventative measures are used in combination. Similar methodology was used across other models considering multiple interventions working collectively [32, 33, 39, 55]. An alternative approach was including parameters in the differential equations representing the reduction in HIV transmission due to prevention interventions and multiplying these by the force of infection [56]. Alternatively, one model set a baseline transmission probability per sex act for uncircumcised males to females, and then multiplied this by various factors to account for introducing preventative measures; for example, per sex act the baseline transmission probability would be increased by a multiplicative factor increment of 0.09 if the susceptible individual is taking PrEP and then by a further multiplicative factor increment of 0.4 for female-to-male transmission if the male is circumcised [67].
Some models explored how uptake of one intervention impacted uptake of another, for example, reducing PrEP use as vaccine utilisation increased [71] or via ‘product cannibalism,’ which altered uptake of differing interventions dependent on the number of products in use and user preference [36, 69], and is alternatively referred to as 'substitution’ in economic terminology and ‘migration’ in epidemiology [73].
Several models used optimisation methods to determine the optimum allocation of interventions to maximise impact (n = 4, 10%), for instance by varying risk groups receiving interventions [45], redistributing international funds [41], or expanding budgets [72].
3.7 Synthesis of Results
See additional files (Online Resource 7) in the ESM for a summary of model parameters and percentage of articles reviewed which include each parameter dependent on article quality. There was no association identified between article quality and intervention features incorporated for PrEP or circumcision. It is not possible to reliably comment on differences in characteristics included in vaccination models as few articles were included.
A number of parameters were included in a large number of studies. The only parameters included across all models were intervention uptake/coverage (n = 48, 100%) and reduction in HIV acquisition risk (n = 48, 100%). For PrEP, varying intervention uptake by risk group was included in about half of studies (n = 21, 53%). For circumcision, restricting models so the intervention occurs only at birth (n = 17, 65%) or throughout life (n = 15, 58%) and ensuring only HIV-susceptible individuals are eligible (n = 21, 81%) were included in a majority of studies. For vaccination, varying intervention uptake dependent on the number of individuals already vaccinated was included in over half of studies (n = 3, 60%).
4 Discussion
This review is the first to assimilate the information pertaining to HIV preventative interventions that should be considered when designing or implementing new solutions, for incorporation into compartmental models. The insight provided will guide future mathematical model development, and aid policy makers in determining optimal HIV prevention combination strategies.
In reviewing compartmental model structures for HIV prevention interventions, we found that most models included PrEP, with fewer considering circumcision or vaccines, and were largely based in LMICS, especially Eastern and Southern Africa. Common intervention parameters considered in the models were efficacy and intervention coverage. We also identified important model considerations dependent on the intervention being modelled. For instance, the need to vary intervention uptake by infection status (susceptible or infected) was required only where intervention use was not limited by HIV status (i.e., circumcision); interventions requiring frequent administration were more likely to vary eligibility dependent on sexual risk group (i.e., PrEP); and interventions requiring administration via healthcare staff were more likely to vary uptake dependent on number already covered (i.e., vaccinations). These factors were of importance to model developers, and by extension could be important to funders of the research. More generally, we identified that models considered efficacy impacted by intervention reliability, adherence, resistance, risk compensation, uptake, and discontinuation; and costs.
Our review identified key gaps in how models incorporated the impact of interventions on HIV transmission. We found that most models did not incorporate some key subgroups into their analysis, with no model stratifying the population by ethnicity, which impacts HIV prevalence [74], intervention access [75], and uptake [76,77,78]. Furthermore, only a small number of studies considered vertical or intravenous HIV transmission in addition to sexual transmission. Given these modes of transmission continue to contribute to new HIV cases [31], their incorporation would increase a model’s capacity to guide policy makers.
Many models assigned intervention uptake based on individual risk status, with the number in each risk level estimated predominantly from population demographics. However, there is a disparity between perceived and actual risk [79,80,81,82], which can affect uptake of prevention interventions and differs by sex [83] and ethnicity [81, 84], amongst other factors. Studies did not include separate parameters for willingness to accept an intervention or user preferences, which can affect intervention uptake [85], rather considering this within the intervention uptake parameter. This highlights that not all important drivers for intervention uptake are included explicitly in models, although they may be implicitly considered. Models also generally prevented individuals from changing sexual risk groups during their life course [86], thus limiting the ability to reassess eligibility status and move people off interventions as risks change. Consequently, although population demographics can estimate risk group numbers and thus an assumed intervention uptake rate, this likely does not fully account for complexities such as personal preference or risk perception. As prevention strategies commonly target interventions based on risk, it is important that models accurately represent these risk groups to enable useful predictions of programme impact.
Although several models considered intervention adherence, there was no instance where the level of adherence was varied by subgroup. Instead, a standard reduction of efficacy was applied to all groups receiving the intervention or alternatively adherence differences were enveloped into the differing rates of infections by risk group level. Stratification by subgroup should be considered as adherence is impacted by many factors including age [87,88,89,90], ethnicity [90], and sex/gender [88, 89].
Many studies assessed outcomes for PrEP, circumcision, and vaccines in combination with other HIV and sexual and reproductive health interventions, with efficacy of combining interventions largely estimated multiplicatively as we have described. However, other incremental outcomes can occur when combining prevention intervention. For instance, multiple interventions may produce a combined efficacy which is less than the sum of the individual programmes [91, 92] or the overall efficacy may equal the efficacy achieved by the strongest of the combined interventions when acting alone [91, 92]. The sequential order in which interventions are integrated can also impact combined efficacy [55, 93], or there may be a synergistic effect whereby combined efficacy is greater than the sum of the individual interventions’ efficacies [92]; for example, although HIV vaccines may have limited efficacy independently, one study found concomitant use of PrEP may improve immune response to boost vaccine responses [94]. As global guidelines recommend providing a combination of prevention interventions [4, 95], it is imperative that their combined effects are correctly studied and represented. To facilitate this, evidence (from sources including trial/observational/implementation research) may be needed as new interventions become available, to quantify the total effectiveness of combinations of interventions.
We found no association between article quality and the intervention features incorporated. Indeed, article quality of included studies varied; with data evaluation, implementation verification, and model output corroboration identified as areas of poorer model quality. Many models also incorporated parameter data which was not relevant to the setting, with a lack of parameter uncertainty ranges reported. Mathematical models are dependent on the quality of data informing them [96] and should ideally review outcomes over a range of credible and realistic parameter values [97]. If such data are unavailable, then particular attention needs to be given to ensure that results are relevant, including sensitivity of outcomes. Although many aspects of model structure were considered in our review, intervention coverage was deemed out of scope for critical appraisal, as models do not separate out the various processes that contribute to uptake, such as acceptability, cost, and availability. Whilst these factors are critical to the performance of a programme, it is uptake that determines the impact on transmission. The models, almost universally, highlight the role of uptake rather than how to increase it. However, as coverage is important to intervention success, reviewers of model predictions must consider coverage assumptions as dictated by model researchers and funders.
Strengths of this study include that we considered only peer-reviewed, published literature, and did not incorporate grey literature which is of more variable quality. The study reviewed multiple prevention interventions (PrEP, circumcision, and vaccinations) and although ideally a review of all interventions (including condom use) may provide additional insight, the interventions provided reasonable representation of primary HIV prevention models due to the delivery modes and intervention frequencies covered. Moreover, we were interested in developing insight into models of particular relevance to novel intervention techniques (such as emerging PrEP-based products and vaccinations) where there is ongoing research and heightening interest around their future potential to prevent HIV; comparatively lower levels of research are ongoing around other preventative methods (such as ART and testing), and relevance of modelling techniques for these interventions was deemed of lower relevance to fulfil our study aim.
This review builds on prior reviews of HIV mathematical models [15, 25,26,27]. Strengths include our inclusion of prevention interventions that were missing from prior reviews [98, 99]; performing a comprehensive review of available modelling literature run with real-life data rather than building hypothetical un-tested models [99]; reviewing models for multiple interventions rather than considering only one [25,26,27]; presenting an in-depth review of differing approaches to model structure, parameter inclusion, and risk of infection for prevention interventions and identifying gaps, rather than higher level outlines [15, 25]; and reviewing the quality of included models, which was missing in other reviews [15, 26, 27, 98]. In line with our findings, recent studies reviewing mathematical models for TB vaccinations and antimicrobial resistance similarly identified concerns with model data [100, 101], intervention definitions in models [101], and model validation [100].
This review has several limitations. Firstly, study screening and analysis was performed by only one individual (RG). Secondly, the search for this review was undertaken on 15 July 2020. An updated database search on 28 November 2022 (across all search engines except ECONLIT) identified 868 new articles published pre-screening, these were not incorporated in this analysis. Given our review identified 48 articles for inclusion from 1460 published following screening, we can estimate that around 28 additional articles may now be eligible for inclusion and an updated review to identify and analyse newer models may add to the findings of this review, particularly on vaccine models. However, to the best of our knowledge, no systematic review has been published in the interim and hence this article remains an important contribution to the field, and addresses a gap in the literature.
In this review, it was deemed fitting to consider one modelling approach alone, as the substantial differences across the various modelling types would make summarising them together inappropriate. Due to their appropriateness for infectious diseases, compartmental models alone were considered in this analysis. However, alternative mathematical model designs exist—with differing levels of complexity—which could also suitably represent HIV disease dynamics. A recent paper modelling PrEP found static models, which are simpler to create, provided a useful estimate of impact over short–medium time horizons comparable to more complex compartmental models [102]. Individual-based models, which can model stochastic changes in an individuals’ sexual network over time [103,104,105], may also be particularly valuable by better representing the complex structure of sexual partnerships and understanding the drivers of behaviour. However, such models require appreciably more data to parameterise and in terms of this review, it would have been challenging to describe and catalogue the structures and parameters for such models due to their relative lack of transparency [106]. Given the relatively higher volume of ordinary differential equation models for HIV, as utilised to describe compartmental models, and their utility in providing evidence for decision making in infectious diseases, it was deemed sufficient to include compartmental models alone to meet our study aim.
Due to the immediate relevance to policy makers in this area, this article reviewed the published literature to inspect compartmental models developed for modelling HIV prevention interventions, rather than critiquing published models against predetermined criteria. One limitation to this approach is that models are largely created to address a particular question; hence, if authors or funders (policy makers) are uninterested in the impact of ethnicity on HIV transmission and acquisition, for instance, the models may not incorporate this parameter. In this way, developed models are biased by the question they are developed to answer. However, as our aim was to identify model factors of relevance to policy makers, we believe this bias highlights those factors deemed important to the funders and policy makers. Indeed, models may include parameters which impact little on HIV disease transmission, but are considered important to include or represent in the models by authors or funders.
Further, published models generally did not distinguish whether they were developed as simple representations of reality—for instance to generate hypotheses—or as close representations of reality. During this review we did not exclude models based on their stated aims and as such all models were reviewed collectively. Although this may explain somewhat the variability in model complexity, this generalisation did not hinder our ability to identify the HIV intervention structures and parameters included in published models, and so we do not feel this negatively impacts the findings. For future studies to consider the impact of model aims, they should ideally be more explicitly outlined in published modelling papers, although the distinction around closeness to reality is potentially difficult to define.
Compared with approaches taken in other reviews of mathematical models, a weakness of our approach is that we did not include schematics and model differential equations which may enable the reader to better understand how models are built; for this we refer readers to Dorratoltaj et al. [98], which may enable the reader to better understand how models are built. We also did not review model outcome predictions to assess the potential impact of future intervention campaigns, as performed in other reviews [25, 101], nor did we compare qualitative predictions between models to determine differences based on model complexity. The consideration of how models differ and how this impacts validity is important; indeed, we have identified from other work in this series that model validation is an understudied area requiring focus [107]; however, this was beyond the scope of this review. Further, we believe the identification of parameters commonly utilised in such models, as was the focus of this review, is in itself important. This work will enable accurate models to be more quickly developed, therefore enabling accurate predictions to be established from one model rather than comparing multiple model predictions.
More generally, mathematical models have limitations, including that they are a simplification of reality, and require assumptions be made about the ‘real world’ [108]. They must strike the right balance between being as simple as possible but with the necessary complexity to remain useful [109]. These limitations are discussed more fully in a recent article by Saltelli et al. [110]. Furthermore, models provide only one form of evidence for policy makers and as such should be considered alongside intelligence such as country priorities and ethical considerations; indeed, ethics and social justice priorities may outweigh economic considerations [48]. Model outputs should be viewed in the context of their limitations and fundamental uncertainty; and with that understanding, model predictions can be appropriately factored into decisions [109, 110] and utilised to fill important gaps in research.
5 Conclusions
This review synthesised the current compartmental models for modelling prevention interventions for HIV disease into a general framework. Several gaps were identified. Critically, at present, models insufficiently incorporate multiple interventions acting simultaneously, a task which will become increasingly complex to model over time as factors such as viral suppression and long-acting PrEP use become more prevalent. Also, as prevention strategies often target interventions to those at highest risk, it is important that models improve the representation of population subgroups; for example, incorporating ethnicity and improving sexual risk group stratification. Additionally, many models use inappropriate data in parameterisation, which will affect the accuracy of model outputs. Resolution of such gaps within future models will enable more accurate assessment of the impact that new interventions may have, thereby providing more meaningful guidance to policy makers. Given the importance of models in decision making, and the number of new HIV prevention interventions in the latter stages of development, it is critical that models reliably and robustly reflect the real world and the impact of the products they seek to represent.
Abbreviations
- AIDS:
-
Acquired immune deficiency syndrome
- ART:
-
Antiretroviral therapy
- bNAbs:
-
Broadly neutralizing HIV-1 antibodies
- CE:
-
Cost-effectiveness
- EIMC:
-
Early-infant male circumcision
- HIC:
-
High income country
- HIV:
-
Human immunodeficiency virus
- IV:
-
Intravenous
- LMIC:
-
Low-and-middle-income countries
- MSM:
-
Men who have sex with men
- NA:
-
Not applicable
- PEP:
-
Post-exposure prophylaxis
- PMTCT:
-
Prevention of mother to child transmission
- PrEP:
-
Pre-exposure prophylaxis
- STI:
-
Sexually transmitted infection
- TRACE:
-
TRAnsparent and Comprehensive Ecological modelling documentation
- UNAIDS:
-
The Joint United Nations Programme on HIV and AIDS
- VMMC:
-
Voluntary medical male circumcision
- WHO:
-
World health organisation
References
HIV.gov. The Global HIV/AIDS Epidemic [Internet]. 2021 [cited 2022 Feb 9]. Available from: https://www.hiv.gov/hiv-basics/overview/data-and-trends/global-statistics.
World health organisation. HIV/AIDS [Internet]. [cited 2022 Dec 2]. Available from: https://www.who.int/health-topics/hiv-aids#tab=tab_1
UNAIDS. 90-90-90: An ambitious treatment target to help end the AIDS epidemic [Internet]. 2014. Available from: https://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf
UNAIDS. 2025 AIDS targets: Target-Setting, Impact and Resource Needs for the Global AIDS Response. Technical consultation on primary prevention [Internet]. 2019 [cited 2022 Feb 9]. Available from: https://www.unaids.org/sites/default/files/2025targets-PreventionMeeting_March2019.pdf
Mugo NR, Ngure K, Kiragu M, Irungu E, Kilonzo N. The preexposure prophylaxis revolution; from clinical trials to programmatic implementation. Curr Opin HIV AIDS. 2016;11:80–6.
World health organisation. HIV/AIDs: Key facts [Internet]. 2021 [cited 2022 Feb 9]. Available from: https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
World health Organization. WHO recommends the dapivirine vaginal ring as a new choice for HIV prevention for women at substantial risk of HIV infection [Internet]. 2021 [cited 2021 Jul 12]. Available from: https://www.who.int/news/item/26-01-2021-who-recommends-the-dapivirine-vaginal-ring-as-a-new-choice-for-hiv-prevention-for-women-at-substantial-risk-of-hiv-infection
Viiv healthcare. FDA grants Priority Review to ViiV Healthcare’s New Drug Application for cabotegravir long-acting for prevention of HIV [Internet]. 2021 [cited 2021 Oct 7]. Available from: https://viivhealthcare.com/en-gb/media/press-releases/2021/september/viiv-healthcare-announces-fda-priority-review/
Kim J, Vasan S, Kim JH, Ake JA. Current approaches to HIV vaccine development: a narrative review. J Int AIDS Soc. 2021;24(7):25793.
Leggat DJ, Cohen KW, Willis JR, Fulp WJ, deCamp AC, Kalyuzhniy O, et al. Vaccination induces HIV broadly neutralizing antibody precursors in humans. Science. 2022;378:6502.
Burton DR. Amping up HIV antibodies. Science (80- ) [Internet]. American Association for the Advancement of Science; 2021;372:1397–8. Available from: https://doi.org/10.1126/science.abf5376
Antibodies for HIV prevention [Internet]. Available from: https://www.iavi.org/phocadownload/iavi_fact_sheet_antibodies_for_hiv_prevention.pdf
Miner MD, Corey L, Montefiori D. Broadly neutralizing monoclonal antibodies for HIV prevention. J Int AIDS Soc. 2021;24(7): e25829.
Brown JL, Sales JM, DiClemente RJ. Combination HIV prevention interventions: the potential of integrated behavioral and biomedical approaches. Curr HIV/AIDS Rep. 2014;11:363–75.
Johnson LF, White PJ. A review of mathematical models of HIV/AIDS interventions and their implications for policy. Sex Transm Infect. 2011;87:629–34.
Garnett GP, Cousens S, Hallett TB, Steketee R, Walker N. Mathematical models in the evaluation of health programmes. Lancet (London, England). 2011;378:515–25.
Liang P, Zu J, Zhuang G. A literature review of mathematical models of hepatitis B virus transmission applied to immunization strategies from 1994 to 2015. J Epidemiol. 2018;28:221–9.
Ma Z, Li J. Dynamical Modeling and Analysis of Epidemics [Internet]. World Scientific Publishing Co. Pte. Ltd; 2009. Available from: https://agus34drajat.files.wordpress.com/2010/10/dynamical-modeling-and-analysis-of-epidemics.pdf
Brisson M, Edmunds WJ. Economic evaluation of vaccination programs: the impact of herd immunity. Med Decis Making. 2003;23:76–82.
Pitman R, Fisman D, Zaric GS, Postma M, Kretzschmar M, Edmunds J, et al. Dynamic transmission modeling: a report of the ISPOR-SMDM modeling good research practices task force—5. Value Health. 2012;15:828–34.
Department of Health South Africa, South African National AIDS Council. South African HIV and TB Investment Case - Summary Report Phase 1 [Internet]. Available from: http://www.heroza.org/wp-content/uploads/2016/03/SA-HIV_TB-Investment-Case-Full-Report-Low-Res.pdf
The Global Fund. Step up the fight: Investment case [Internet]. 2019. Available from: https://www.theglobalfund.org/media/8279/publication_sixthreplenishmentinvestmentcase_report_en.pdf
Nepomuceno E, Resende D, Lacerda M. A Survey of the individual-based model applied in biomedical and epidemiology. 2019.
Donkin E, Dennis P, Ustalakov A, Warren J, Clare A. Replicating complex agent based models, a formidable task. Environ Model Softw [Internet]. 2017;92:142–51. Available from: https://www.sciencedirect.com/science/article/pii/S1364815216310088
Case KK, Gomez GB, Hallett TB. The impact, cost and cost-effectiveness of oral pre-exposure prophylaxis in sub-Saharan Africa: a scoping review of modelling contributions and way forward. J Int AIDS Soc. 2019;22: e25390.
Bernard CL, Brandeau ML. Structural sensitivity in HIV modeling: a case study of vaccination. Infect Dis Model. 2017;2:399–411.
Baggaley RF, Fraser C. Modelling sexual transmission of HIV: testing the assumptions, validating the predictions. Curr Opin HIV AIDS. 2010;5:269–76.
Grimm V, Augusiak J, Focks A, Frank B, Gabsi F, Johnston ASA, et al. Towards better modelling and decision support: Documenting model development, testing, and analysis using TRACE. Ecol Modell. 2014;280:129–39.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339: b2535.
Shaw GM, Hunter E. HIV transmission. Cold Spring Harb Perspect Med. 2012;2.
Public Health Agency of Canada. HIV TRANSMISSION RISK: A SUMMARY OF THE EVIDENCE [Internet]. 2010. Available from: https://www.catie.ca/sites/default/files/HIV-TRANSMISSION-RISK-EN.pdf
Glaubius RL, Hood G, Penrose KJ, Parikh UM, Mellors JW, Bendavid E, et al. Cost-effectiveness of injectable preexposure prophylaxis for HIV prevention in South Africa. Clin Infect Dis. 2016;63:539–47.
Glaubius RL, Parikh UM, Hood G, Penrose KJ, Bendavid E, Mellors JW, et al. Deciphering the Effects of Injectable Pre-exposure Prophylaxis for Combination Human Immunodeficiency Virus Prevention. Open forum Infect Dis [Internet]. Oxford University Press; 2016;3:ofw125–ofw125. Available from: https://pubmed.ncbi.nlm.nih.gov/27703992
van Vliet MM, Hendrickson C, Nichols BE, Boucher CA, Peters RP, van de Vijver DA. Epidemiological impact and cost-effectiveness of providing long-acting pre-exposure prophylaxis to injectable contraceptive users for HIV prevention in South Africa: a modelling study. J Int AIDS Soc. 2019;22: e25427.
Glaubius R, Ding Y, Penrose KJ, Hood G, Engquist E, Mellors JW, et al. Dapivirine vaginal ring for HIV prevention: modelling health outcomes, drug resistance and cost-effectiveness. J Int AIDS Soc. 2019;22: e25282.
Smith JA, Anderson S-J, Harris KL, McGillen JB, Lee E, Garnett GP, et al. Maximising HIV prevention by balancing the opportunities of today with the promises of tomorrow: a modelling study. Lancet HIV. 2016;3:e289–96.
Dimitrov D, Kublin JG, Ramsey S, Corey L. Are clade specific HIV vaccines a necessity? An analysis based on mathematical models. EBioMedicine. 2015;2:2062–9.
Punyacharoensin N, Edmunds WJ, De Angelis D, Delpech V, Hart G, Elford J, et al. Effect of pre-exposure prophylaxis and combination HIV prevention for men who have sex with men in the UK: a mathematical modelling study. lancet HIV. Netherlands; 2016;3:e94–104.
Alsallaq RA, Buttolph J, Cleland CM, Hallett T, Inwani I, Agot K, et al. The potential impact and cost of focusing HIV prevention on young women and men: A modeling analysis in western Kenya. PLoS ONE. 2017;12: e0175447.
Cepeda J, Borquez A, Farrell M, Degenhardt L, McKetin R, Tran LT, et al. Integrating HIV pre-exposure prophylaxis and harm reduction among men who have sex with men and transgender women to address intersecting harms associated with stimulant use: a modelling study. J Int AIDS Soc [Internet]. Switzerland: John Wiley and Sons Inc. (E-mail: cs-journals@wiley.com); 2020;23 Suppl 1:e25495. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med18&NEWS=N&AN=32562365
Kelly SL, Martin-Hughes R, Stuart RM, Yap XF, Kedziora DJ, Grantham KL, et al. The global Optima HIV allocative efficiency model: targeting resources in efforts to end AIDS. Lancet HIV. 2018;5:e190–8.
Pharaon J, Bauch CT. The impact of pre-exposure prophylaxis for human immunodeficiency virus on gonorrhea prevalence. Bull Math Biol. 2020;82:85.
Medlock J, Pandey A, Parpia AS, Tang A, Skrip LA, Galvani AP. Effectiveness of UNAIDS targets and HIV vaccination across 127 countries. Proc Natl Acad Sci U S A. 2017;114:4017–22.
Afassinou K, Chirove F, Govinder KS. Pre-exposure prophylaxis and antiretroviral treatment interventions with drug resistance. Math Biosci. 2017;285:92–101.
Akudibillah G, Pandey A, Medlock J. Maximizing the benefits of ART and PrEP in resource-limited settings. Epidemiol Infect. 2017;145:942–56.
de Montigny S, Adamson BJS, Mâsse BR, Garrison LPJ, Kublin JG, Gilbert PB, et al. Projected effectiveness and added value of HIV vaccination campaigns in South Africa: A modeling study. Sci Rep. 2018;8:6066.
Bórquez A, Guanira JV, Revill P, Caballero P, Silva-Santisteban A, Kelly S, et al. The impact and cost-effectiveness of combined HIV prevention scenarios among transgender women sex-workers in Lima, Peru: a mathematical modelling study. Lancet Public Heal. 2019;4:e127–36.
Bernard CL, Owens DK, Goldhaber-Fiebert JD, Brandeau ML. Estimation of the cost-effectiveness of HIV prevention portfolios for people who inject drugs in the United States: a model-based analysis. PLoS Med. 2017;14: e1002312.
Bernard CL, Brandeau ML, Humphreys K, Bendavid E, Holodniy M, Weyant C, et al. Cost-effectiveness of HIV preexposure prophylaxis for people who inject drugs in the United States. Ann Intern Med. 2016;165:10–9.
Anderson S-J, Garnett GP, Enstone J, Hallett TB, Anderson SJG, Enstone J, Hallett TB. The importance of local epidemic conditions in monitoring progress towards HIV epidemic control in Kenya: a modelling study. J Int AIDS Soc. 2018;21:e25203.
Cremin I, McKinnon L, Kimani J, Cherutich P, Gakii G, Muriuki F, et al. PrEP for key populations in combination HIV prevention in Nairobi: a mathematical modelling study. Lancet HIV. 2017;4:e214–22.
McGillen JB, Stover J, Klein DJ, Xaba S, Ncube G, Mhangara M, et al. The emerging health impact of voluntary medical male circumcision in Zimbabwe: An evaluation using three epidemiological models. PLoS ONE. 2018;13: e0199453.
Mitchell KM, Prudden HJ, Washington R, Isac S, Rajaram SP, Foss AM, et al. Potential impact of pre-exposure prophylaxis for female sex workers and men who have sex with men in Bangalore, India: a mathematical modelling study. J Int AIDS Soc. 2016;19:20942.
Stuart RM, Fraser-Hurt N, Kerr CC, Mabusela E, Madi V, Mkhwanazi F, et al. The City of Johannesburg can end AIDS by 2030: modelling the impact of achieving the Fast-Track targets and what it will take to get there. J Int AIDS Soc. 2018;21.
Mitchell KM, Lépine A, Terris-Prestholt F, Torpey K, Khamofu H, Folayan MO, et al. Modelling the impact and cost-effectiveness of combination prevention amongst HIV serodiscordant couples in Nigeria. AIDS [Internet]. Lippincott Williams & Wilkins; 2015;29:2035–44. Available from: https://pubmed.ncbi.nlm.nih.gov/26355574
Ying R, Sharma M, Heffron R, Celum CL, Baeten JM, Katabira E, et al. Cost-effectiveness of pre-exposure prophylaxis targeted to high-risk serodiscordant couples as a bridge to sustained ART use in Kampala. Uganda J Int AIDS Soc. 2015;18:20013.
Marukutira T, Scott N, Kelly SL, Crowe S, Stoove M, Hellard M, et al. Modelling the impact of migrants on the success of the HIV care and treatment program in Botswana. PLoS ONE. 2020;15: e0226422.
Awad SF, Sgaier SK, Lau FK, Mohamoud YA, Tambatamba BC, Kripke KE, et al. Could circumcision of HIV-positive males benefit voluntary medical male circumcision programs in Africa? Mathematical Modeling Analysis. PLoS ONE. 2017;12: e0170641.
Awad SF, Sgaier SK, Tambatamba BC, Mohamoud YA, Lau FK, Reed JB, et al. Investigating voluntary medical male circumcision program efficiency gains through subpopulation prioritization: insights from application to Zambia. PLoS ONE. 2015;10: e0145729.
Awad SF, Sgaier SK, Ncube G, Xaba S, Mugurungi OM, Mhangara MM, et al. A reevaluation of the voluntary medical male circumcision scale-up plan in Zimbabwe. PLoS ONE. 2015;10: e0140818.
Blaizot S, Huerga H, Riche B, Ellman T, Shroufi A, Etard J-F, et al. Combined interventions to reduce HIV incidence in KwaZulu-Natal: a modelling study. BMC Infect Dis. 2017;7:522.
Blaizot S, Maman D, Riche B, Mukui I, Kirubi B, Ecochard R, et al. Potential impact of multiple interventions on HIV incidence in a hyperendemic region in Western Kenya: a modelling study. BMC Infect Dis. 2016;16:189.
Blaizot S, Riche B, Maman D, Mukui I, Kirubi B, Etard J-F, et al. Estimation and short-term prediction of the course of the HIV epidemic using demographic and health survey methodology-like data. PLoS ONE. 2015;10: e0130387.
MacFadden DR, Tan DH, Mishra S. Optimizing HIV pre-exposure prophylaxis implementation among men who have sex with men in a large urban centre: a dynamic modelling study. J Int AIDS Soc. 2016;19:20791.
Cremin I, Hallett TB. Estimating the range of potential epidemiological impact of pre-exposure prophylaxis: run-away success or run-away failure? AIDS 20155;29:733–8
Drabo EF, Hay JW, Vardavas R, Wagner ZR, Sood N. A cost-effectiveness analysis of preexposure prophylaxis for the prevention of HIV among Los Angeles county men who have sex with men. Clin Infect Dis United States. 2016;63:1495–504.
Cremin I, Morales F, Jewell BL, O’Reilly KR, Hallett TB. Seasonal PrEP for partners of migrant miners in southern Mozambique: a highly focused PrEP intervention. J Int AIDS Soc. 2015;18:19946.
Gromov D, Bulla I, Silvia Serea O, Romero-Severson EO. Numerical optimal control for HIV prevention with dynamic budget allocation. Math Med Biol. 2018;35:469–91.
Smith JA, Garnett GP, Hallett TB. The Potential Impact of Long-Acting Cabotegravir for HIV Prevention in South Africa: A Mathematical Modeling Study. J Infect Dis [Internet]. United States; 2021;224:1179–86. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=prem&NEWS=N&AN=32492704
Shen M, Xiao Y, Rong L, Meyers LA, Bellan SE. The cost-effectiveness of oral HIV pre-exposure prophylaxis and early antiretroviral therapy in the presence of drug resistance among men who have sex with men in San Francisco. BMC Med. 2018;16:58.
Adamson B, Garrison L, Barnabas RV, Carlson JJ, Kublin J, Dimitrov D. Competing biomedical HIV prevention strategies: potential cost-effectiveness of HIV vaccines and PrEP in Seattle, WA. J Int AIDS Soc. 2019;22: e25373.
Li J, Peng L, Gilmour S, Gu J, Ruan Y, Zou H, et al. A mathematical model of biomedical interventions for HIV prevention among men who have sex with men in China. BMC Infect Dis. 2018;18:600.
Foss AM, Vickerman PT, Heise L, Watts CH. Shifts in condom use following microbicide introduction: should we be concerned? AIDS [Internet]. 2003;17. Available from: https://journals.lww.com/aidsonline/Fulltext/2003/05230/Shifts_in_condom_use_following_microbicide.15.aspx
What Is the Impact of HIV on Racial and Ethnic Minorities in the U.S.? [Internet]. HIV.gov. [cited 2022 Jun 7]. Available from: https://www.hiv.gov/hiv-basics/overview/data-and-trends/impact-on-racial-and-ethnic-minorities
CDC. HIV and African American People [Internet]. 2022. Available from: https://www.cdc.gov/hiv/pdf/group/racialethnic/africanamericans/cdc-hiv-africanamericans.pdf
Huang Y-LA, Zhu W, Smith DK, Harris N, Hoover KW. HIV Preexposure Prophylaxis, by Race and Ethnicity - United States, 2014-2016. MMWR Morb Mortal Wkly Rep. 2018;67:1147–50.
Brantley ML, Rebeiro PF, Pettit AC, Sanders A, Cooper L, McGoy S, et al. Temporal trends and sociodemographic correlates of PrEP uptake in Tennessee, 2017. AIDS Behav. 2019;23:304–12.
Kanny D, Jeffries WL 4th, Chapin-Bardales J, Denning P, Cha S, Finlayson T, et al. Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men-23 Urban Areas, 2017. MMWR Morb Mortal Wkly Rep. 2019;68:801–6.
Sidebottom D, Ekström AM, Strömdahl S, Sidebottom D, Ekstrom AM, Stromdahl S. A systematic review of adherence to oral pre exposure prophylaxis for HIV—how can we improve uptake and adherence? BMC Infect Dis. 2018;18(1):581.
Seekaew P, Pengnonyang S, Jantarapakde J, Meksena R, Sungsing T, Lujintanon S, et al. Discordance between self-perceived and actual risk of HIV infection among men who have sex with men and transgender women in Thailand: a cross-sectional assessment. J Int AIDS Soc. 2019;22: e25430.
Baidoobonso S, Bauer GR, Speechley KN, Lawson E. HIV risk perception and distribution of HIV risk among African, Caribbean and other Black people in a Canadian city: mixed methods results from the BLACCH study. BMC Public Health. 2013;13:184.
Stringer EM, Sinkala M, Kumwenda R, Chapman V, Mwale A, Vermund SH, et al. Personal risk perception, HIV knowledge and risk avoidance behavior, and their relationships to actual HIV serostatus in an urban African obstetric population. J Acquir Immune Defic Syndr. 2004;35:60–6.
Kibombo R, Neema S, Ahmed FH. Perceptions of risk to HIV infection among adolescents in Uganda: are they related to sexual behaviour? Afr J Reprod Health. 2007;11:168–81.
Maughan-Brown B, Venkataramani AS. Accuracy and determinants of perceived HIV risk among young women in South Africa. BMC Public Health. 2017;18:42.
Warren EA, Paterson P, Schulze WS, Lees S, Eaklel R, Stadler J, et al. Risk perception and the influence on uptake and use of biomedical prevention interventions for HIV in sub-Saharan Africa: a systematic literature review. PLoS ONE. 2018;13:6.
Rozhnova G, Heijne J, Bezemer D, van Sighem A, Presanis A, De Angelis D, et al. Elimination prospects of the Dutch HIV epidemic among men who have sex with men in the era of preexposure prophylaxis. AIDS [Internet]. Lippincott Williams & Wilkins; 2018;32:2615–23. Available from: https://pubmed.ncbi.nlm.nih.gov/30379687
Barclay TR, Hinkin CH, Castellon SA, Mason KI, Reinhard MJ, Marion SD, et al. Age-associated predictors of medication adherence in HIV-positive adults: health beliefs, self-efficacy, and neurocognitive status. Health Psychol. 2007;26:40–9.
Mallayasamy S, Chaturvedula A, Fossler MJ, Sale ME, Hendrix CW, Haberer JE. Assessment of demographic and socio-behavioral factors on adherence to HIV pre-exposure prophylaxis using a markov modeling approach. Front Pharmacol. 2019;10:785.
Madrasi K, Chaturvedula A, Haberer JE, Sale M, Fossler MJ, Bangsberg D, et al. Markov mixed effects modeling using electronic adherence monitoring records identifies influential covariates to HIV preexposure prophylaxis. J Clin Pharmacol England. 2017;57:606–15.
Spinelli MA, Glidden DV, Anderson PL, Gandhi M, Cohen S, Vittinghoff E, et al. Brief report: short-term adherence marker to PrEP predicts future nonretention in a large PrEP demo project: implications for point-of-care adherence testing. J Acquir Immune Defic Syndr. 2019;81:158–62.
Long EF, Stavert RR. Portfolios of biomedical HIV interventions in South Africa: a cost effectiveness analysis. J Gen Intern Med. 2013;28:1294–301.
Walensky RP. Combination HIV prevention: the value and interpretation of mathematical models. Curr HIV/AIDS Rep. 2013;10:195–8.
Wingood GM, Rubtsova A, DiClemente RJ, Metzger D, Blank M. A new paradigm for optimizing HIV intervention synergy: the role of interdependence in integrating HIV prevention interventions. J Acquir Immune Defic Syndr. 2013;63(Suppl 1):S108–13.
Excler J-L, Rida W, Priddy F, Gilmour J, McDermott AB, Kamali A, et al. AIDS vaccines and preexposure prophylaxis: is synergy possible? AIDS Res Hum Retroviruses. 2011;27:669–80.
UNAIDS. FAST-TRACKING COMBINATION PREVENTION: TOWARDS REDUCING NEW HIV INFECTIONS TO FEWER THAN 500 000 BY 2020 [Internet]. 2015. Available from: https://www.unaids.org/sites/default/files/media_asset/20151019_JC2766_Fast-tracking_combination_prevention.pdf
Egger M, Johnson L, Althaus C, Schöni A, Salanti G, Low N, et al. Developing WHO guidelines: time to formally include evidence from mathematical modelling studies. F1000Research. 2017;6:1584.
Turnovsky SJ. On the role of small models in macrodynamics. J Econ Dyn Control. 2011;35:1605–13.
Dorratoltaj N, Nikin-Beers R, Ciupe SM, Eubank SG, Abbas KM. Multi-scale immunoepidemiological modeling of within-host and between-host HIV dynamics: systematic review of mathematical models. PeerJ. 2017;5: e3877.
Akpa OM, Oyejola BA. Modeling the transmission dynamics of HIV/AIDS epidemics: an introduction and a review. J Infect Dev Ctries Italy. 2010;4:597–608.
Birkegård AC, Halasa T, Toft N, Folkesson A, Græsbøll K. Send more data: a systematic review of mathematical models of antimicrobial resistance. Antimicrob Resist Infect Control. 2018;7:117. https://doi.org/10.1186/s13756-018-0406-1.
Harris RC, Sumner T, Knight GM, White RG. Systematic review of mathematical models exploring the epidemiological impact of future TB vaccines. Hum Vaccin Immunother [Internet]. 2016/07/22. Taylor & Francis; 2016;12:2813–32. Available from: https://pubmed.ncbi.nlm.nih.gov/27448625
Grant H, Foss AM, Watts C, Medley GF, Mukandavire Z. Is modelling complexity always needed? Insights from modelling PrEP introduction in South Africa. J Public Health (Oxf). 2020;42:e551–60.
Jenness SM, Sharma A, Goodreau SM, Rosenberg ES, Weiss KM, Hoover KW, et al. Individual HIV risk versus population impact of risk compensation after HIV preexposure prophylaxis initiation among men who have sex with men. PLoS ONE. 2017;12: e0169484.
Jenness SM, Goodreau SM, Rosenberg E, Beylerian EN, Hoover KW, Smith DK, et al. Impact of the centers for disease control’s HIV preexposure prophylaxis guidelines for men who have sex with men in the United States. J Infect Dis. 2016;214:1800–7.
Goodreau SM, Rosenberg ES, Jenness SM, Luisi N, Stansfield SE, Millett GA, et al. Sources of racial disparities in HIV prevalence in men who have sex with men in Atlanta, GA, USA: a modelling study. Lancet HIV. 2017;4:e311–20.
Müller B, Balbi S, Buchmann CM, de Sousa L, Dressler G, Groeneveld J, et al. Standardised and transparent model descriptions for agent-based models: Current status and prospects. Environ Model Softw [Internet]. 2014;55:156–63. Available from: https://www.sciencedirect.com/science/article/pii/S1364815214000395
Rueda ST, Terris-Prestholt F, et al. Health Economics Research on Non-Surgical, Biomedical HIV Prevention: Identifying Gaps and Proposing a Way Forward. Pharmacoeconomics. 2023;In Print.
Richardson BC. Richardson BC, Joscelyn KB, Saalberg JH, editors. Limitations on the use of mathematical models in transportation policy analysis1979. 1979.
Rojas-Vallejos J. Strengths and limitations of mathematical models in pandemicsthe case of COVID-19 in Chile. Medwave. 2020;20: e7876.
Saltelli A, Bammer G, Bruno I, Charters E, Di Fiore M, Didier E, et al. Five ways to ensure that models serve society: a manifesto. Nature England. 2020;582:482–4.
Acknowledgements
We would like to thank the London School of Hygiene and Tropical Medicine librarian team for assistance with search strategy development. We sincerely thank the reviewers and editors, whose comments helped improve and clarify this manuscript. This study was made possible by the support of the American People through the US President’s Emergency Plan for AIDS Relief (PEPFAR) through the United States Agency for International Development (USAID). The contents of this paper are the sole responsibility of the authors and do not necessarily reflect the views of PEPFAR, USAID, or the United States Government. The views expressed in this article do not necessarily represent the decisions, policy or views of UNAIDS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Authors' contributions
Study conceptualisation: RG, GM, FTP. Search strategy: RG. Record screening and data extraction: RG. Formal analysis: RG. Writing (original draft): RG. Reviewing results and contributing to writing the manuscript: PI, GM, FTP, MQ. Writing (review and editing): All authors.
Funding
USAID Grant: AID-OAA-A-16-00032.
Competing interests
MQ reports current employment at Evidera, but does not work in the HIV prevention area in this role.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Giddings, R., Indravudh, P., Medley, G.F. et al. Infectious Disease Modelling of HIV Prevention Interventions: A Systematic Review and Narrative Synthesis of Compartmental Models. PharmacoEconomics 41, 693–707 (2023). https://doi.org/10.1007/s40273-023-01260-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-023-01260-z