Abstract
Objective
We aimed to calculate the efficiency of the EmERGE Pathway of Care in five European HIV clinics, developed and implemented for medically stable people living with HIV.
Methods
Participants were followed up for 1 year before and after implementation of EmERGE, between April 2016 and October 2019. Micro-costing studies were performed in the outpatient services of the clinics. Unit costs for outpatient services were calculated in national currencies and converted to US$ 2018 OECD purchasing parity prices to enable between clinic comparisons in terms of outcomes and costs. Unit costs were linked to the mean use of services for medically stable people living with HIV, before and after implementation of EmERGE. Primary outcome measures were CD4 count and viral load; secondary outcomes were patient activation (PAM13) and quality of life (PROQOL-HIV). Out-of-pocket expenditure data were collected.
Results
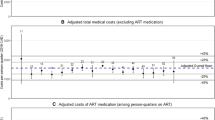
There were 2251 participants: 87–93% were male, mean age at entry was 41–47 years. Medically stable people living with HIV had outpatient visits in four sites which decreased by 9–31% and costs by 5–33%; visits and costs increased by 8% in one site, which had to revert back to face-to-face visits. Antiretroviral drugs comprised 83–91% of annual costs: the Portuguese site had the highest antiretroviral drug costs in US$ purchasing parity prices. Primary and secondary outcome measures of participants did not change during the study.
Conclusions
EmERGE is acceptable and provided cost savings in different socio-economic settings. Antiretroviral drug costs remain the main cost drivers in medically stable people living with HIV. While antiretroviral drug prices in local currencies did not differ that much between countries, conversion to US$ purchasing parity prices revealed antiretroviral drugs were more expensive in the least wealthy countries. This needs to be taken into consideration when countries negotiate drug prices with pharmaceutical vendors. Greater efficiencies can be anticipated by extending the use of the EmERGE Pathway to people with complex HIV infection or other chronic diseases. Extending such use should be systematically monitored, implementation should be evaluated and funding should be provided to monitor and evaluate future changes in service provision.


Similar content being viewed by others
References
Giansanti D. The role of the mHealth in the fight against the Covid-19: successes and failures. Healthcare (Basel). 2021;9(1):58. https://www.mdpi.com/2227-9032/9/1/58 Accessed 15 Apr 2022
Taylor D, Lunny C, Loli P, Warje O, Geldman J, Wong T, et al. Effectiveness of text messaging interventions on prevention, detection, treatment, and knowledge outcomes for sexually transmitted infections (STIs)/HIV: a systematic review and meta-analysis. Syst Rev. 2019;8:12. https://doi.org/10.1186/s13643-018-0921-4 Accessed 15 Apr 2022
Cooper V, Clatworthy J, Whetham J, EmERGE Consortium. mHealth interventions to support self-management in HIV: a systematic review. Open AIDS J. 2017;11:119–32. https://openaidsjournal.com/VOLUME/11/PAGE/119/ Accessed 15 Apr 2022
Chidambaram S, Erridge S, James Kinross J, Purkayastha S, on behalf of the PanSurg Collaborative. Observational study of UK mobile health apps for COVID-19. Lancet Digital Health. 2020;2:e388–90. https://www.thelancet.com/journals/landig/article/PIIS2589-7500(20)30144-8/fulltext Accessed 15 Apr 2022
Cheney C. How to use telehealth in cancer care during the coronavirus pandemic and beyond. HealthLeaders, May 19, 2020. https://www.healthleadersmedia.com/clinical-care/how-use-telehealth-cancer-care-during-coronavirus-pandemic-and-beyond. Accessed 15 Apr 2022.
Humer E, Pieh C, Kuska M, Barke A, Doering BK, Gossmann K, et al. Provision of psychotherapy during the COVID-19 pandemic among Czech, German and Slovak psychotherapists. Int J Environ Res Public Health. 2020;17(13):4811. https://www.mdpi.com/1660-4601/17/13/4811 Accessed 15 Apr 2022
Chausa P, Gárate FJ, Cáceres C, Wallitt E, Whetham J, Gómez EJ, EmERGE Consortium. EmERGE platform: a new mHealth solution for people living with HIV. In: Henriques J, Neves N, de Carvalho P, editors. XV Mediterranean Conference on Medical and Biological Engineering and Computing. MEDICON 2019. IFMBE Proceedings. Cham: Springer, vol. 76. https://link.springer.com/chapter/10.1007%2F978-3-030-31635-8_99. Accessed 15 Apr 2022.
Beck EJ, Mandalia S, Yfantopoulos P, Jones CI, Bremner S, Whetham J, et al., on behalf of the EmERGE Consortium. Efficiency of the EmERGE pathway to provide continuity of care for Spanish people living with medically stable HIV. Enferm Infecc Microbiol Clin. 2021:S0213-005X(20)30422-5. https://doi.org/10.1016/j.eimc.2020.11.018. Accessed 15 Apr 2022
Beck EJ, Mandalia S, Yfantopoulos P, Jones CI, Bremner S, Whetham J, et al. The efficiency of the EmERGE pathway to provide continuity of care for medically stable people living with HIV in Belgium. Acta Clin Belg. 2021 Nov;21:1–10. https://doi.org/10.1080/17843286.2021.2004697. Accessed 15 Apr 2022
Beck EJ, Mandalia S, Yfantopoulos P, Jones C, Bremner S, Whetham J, et al., on behalf of the EmERGE Consortium. The cost of care for people living with stable HIV in Croatia and the efficiency of EmERGE. Croat Med J. 2021;62:562–6. http://www.cmj.hr/2021/62/6/34981686.htm Accessed 15 Apr 2022
Beck EJ, Mandalia S, Yfantopoulos P, Jones CI, Bremner S, Fatz D, et al. The efficiency of the EmERGE Pathway of Care for people living with HIV in England. AIDS Care. 2022. https://doi.org/10.1080/09540121.2022.2040723. Accessed 15 Apr 2022
Beck, EJ, Mandalia S, Yfantopoulos P, Jones CI, Bremner S, Whetham J, et al. The efficiency of the EmERGE platform for people living with medically stable HIV in Portugal. Porto Biomed J (in press).
Beck EJ, Shields JM, Tanna G, Henning G, de Vega I, Andrews G, et al. Developing and implementing national health identifiers in resource limited countries: why, what, who, when and how? Glob Health Action. 2018;11(1):1440782. https://www.tandfonline.com/doi/full/10.1080/16549716.2018.1440782 Accessed 15 Apr 2022
Hyle EP, Naidoo K, Su AE, El-Sadr WM, Freedberg KA. HIV, Tuberculosis, and non-communicable diseases: what is known about the costs, effects, and cost-effectiveness of integrated care? J Acquir Immune Defic Syndr. 2014;67(0 1):S87–95. https://pubmed.ncbi.nlm.nih.gov/25117965/ Accessed 15 Apr 2022
Marcus JL, Chao CR, Leyden WA, Xu LF, Quesenberry C, Klein D, et al. Narrowing the gap in life expectancy between HIV-infected and HIV-uninfected individuals with access to care. J Acquir Immune Defic Syndr. 2016;73(1):39–46. https://insights.ovid.com/jaids-acquired-immune-deficiency-syndromes/jaids/2016/09/010/narrowing555 gap-life-expectancy-hiv-infected/6/00126334 556 557 Accessed 15 Apr 2022
World Health Organization. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. Geneva: World Health Organization; 2015. http://apps.who.int/iris/bitstream/10665/186275/1/9789241509565_eng.pdf?ua=1 563 564 Accessed 15 Apr 2022
Autenrieth CS, Beck EJ, Mallouris C, Stelzle D, Mahy M, Ghys P. Global and regional trends of people living with HIV aged 50 and over: estimates and projections for 2000–2020. PLoS ONE. 2018;13(11): e0207005. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0207005 571 572 Accessed 15 Apr 2022
Beck EJ, Gill W, De Lay PR. Protecting the confidentiality and security of personal health information in low- and middle-income countries in the era of the SDGs and big-data. Glob Health Action. 2016;9:32089. https://www.tandfonline.com/doi/full/10.3402/gha.v9.32089 580 581 Accessed 15 Apr 2022
Whitten PS, Mair FS, Haycox A, May CR, Williams TL, Hellmich S. Systematic review of cost effectiveness studies of telemedicine interventions. BMJ. 2002;324:1434–7. https://www.bmj.com/content/324/7351/1434 Accessed 15 Apr 2022
Hailey D. The need for cost-effectiveness studies in telemedicine. J Telemed Telecare. 2005;11(8):379–83. https://doi.org/10.1177/1357633X0501100801 Accessed 15 Apr 2022
de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev. 2012;12:CD007459. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD007459.pub2/abstract 599 600 Accessed 15 Apr 2022
Public Health England. Guidance, before-and-after study: comparative studies. 2020. https://www.gov.uk/guidance/before-and-after-study-comparative-studies. Accessed 15 Apr 2022.
OECD. Purchasing power parities (PPP) 2018, Paris France. https://data.oecd.org/conversion/purchasing-power-parities-ppp.htm. Accessed 15 Apr 2022.
Waldrop G, Doherty M, Vitoria M, Ford N. Stable patients and patients with advanced disease: consensus definitions to support sustained scale up of antiretroviral therapy. Trop Med Int Health. 2016;1(9):1124–30. https://onlinelibrary.wiley.com/doi/full/10.1111/tmi.12746 Accessed 15 Apr 2022
Beck EJ, Yfantopoulos P, Mandalia S. EU deliverable 3.3. costs and unit costs for EmERGE clinical sites, 29 April 2020. EU Grant Agreement No: 643736.
León A, Cáceres C, Fernández E, Chausa P, Martin M, Codina C, et al. New multidisciplinary home care telemedicine system to monitor stable chronic human immunodeficiency virus-infected patients: a randomized study. PLoS One. 201121;6(1):e14515. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0014515 Accessed 15 Apr 2022
UNAIDS. Manual for costing HIV facilities and services. Geneva, Switzerland, 23rd May 2011. http://www.unaids.org/en/media/unaids/contentassets/documents/document/2011/20110523_manual_costing_HIV_facilities_en.pdf. Accessed 15 Apr 2022.
UNAIDS. Workbook for the collection of cost information on HIV facilities and services. Geneva, Switzerland, 23rd May 2011. http://www.unaids.org/en/media/unaids/contentassets/documents/document/2011/20110523_workbook_cost_info_en.pdf. Accessed 15 Apr 2022.
Beck EJ, Mandalia S, Yfantopoulos P. EU Deliverable 3.4. Cost-efficiency of the mHealth Pathway at the five EmERGE sites. 29 April 2020. EU Grant Agreement No: 643736.
Central Intelligence Agency. The world factbook: country comparison GDP (purchasing power parity). Lanley, Virginia, USA. https://www.cia.gov/the-world-factbook/field/real-gdp-per-capita/country-comparison. Accessed 15 Apr 2022.
West BT, Welch KB, Galecki AT. Linear mixed models: a practical guide using statistical software. Boca Raton (FL): Chapman & Hall/CRC; 2007.
SAS Version 9.4. Cary (NC): SAS Institute Inc.; 2014.
Beck EJ, Mandalia S, Gaudreault M, Brewer C, Zowall H, Gilmore N, et al. The cost-effectiveness of HAART, Canada 1991–2001. AIDS. 2004;18:2411–9. https://journals.lww.com/aidsonline/pages/articleviewer.aspx?year=2004&issue=12030&article=00008&type=Fulltext Accessed 15 Apr 2022
Badri M, Maartens G, Mandalia S, Bekker L-G, Penrod JR, Platt RW, et al. Cost-effectiveness of highly active antiretroviral therapy in South Africa. Plos Med. 2006;3: e4. http://www.plosmedicine.org/article/info:doi/10.1371/journal.pmed.0030004 Accessed 15 Apr 2022
Mandalia S, Mandalia R, Lo G, Chadborn T, Sharott P, Youle M, et al., for the NPMS-HHC Steering Group. Rising population cost for treating people living with HIV in the UK, 1997–2013, PLoS One. 2010;5(12):e15677. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0015677 Accessed 15 Apr 2022
Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40:1918–30. https://europepmc.org/article/PMC/1361231 Accessed 15 Apr 2022
Duracinsky M, Herrmann SE, Berzins B, Armstrong AR, Kohli R, Le Coeur S, et al. The development of PROQOL-HIV: an international instrument to assess the health-related quality of life of persons living with HIV/AIDS. J Acquir Immune Defic Syndr. 2012;59:498–505. https://www.researchgate.net/publication/51977525_The_development_of_PROQOL708-HIV_An_international_instrument_to_assess_the_health709-related_quality_of_life_of_persons_living_with_HIVAIDS Accessed 15 Apr 2022
Anonymous. Societal perspective. In: Kirch W, editor. Encyclopedia of public health. Dordrecht: Springer; 2008.
Jones CI, Bremner S, Whetham J. EU D6.2. Report on clinical outcomes; patient empowerment and quality of life analyses; patient experience & usability. April 2020. EU Grant Agreement No: 643736.
Marent B, Henwood F; EmERGE Consortium. Platform encounters: a study of digitised patient follow-up in HIV care. Sociol Health Illn. 2021;43(5):1117–35. https://onlinelibrary.wiley.com/doi/10.1111/1467-9566.13274 Accessed 15 Apr 2022
Hall JL, McGraw D. For telehealth to succeed, privacy and security risks must be identified and addressed. Health Aff. 2014;33(2):216–21. https://www.healthaffairs.org/doi/10.1377/hlthaff.2013.0997 Accessed 15 Apr 2022
UNAIDS. The privacy, confidentiality and security assessment tool: protecting personal health information. Geneva 14th February 2019. http://www.unaids.org/en/resources/documents/2019/confidentiality_security_assessment_tool. Accessed 15 Apr 2022.
Beck EJ, Mandalia S, DongmoNguimfack B, Pinheiro E, ‘t Hoen E, Boulet P, et al. Does the political will exist to bring quality-assured and affordable drugs to low- and middle-income countries? Glob Health Action. 2019;12(1):1586317. https://doi.org/10.1080/16549716.2019.1586317 Accessed 15 Apr 2022
Beck EJ, Mandalia S, Sangha R, Youle M, Brettle R, Gompels M, et al., for the NPMS-HHC Steering Group. Lower healthcare costs associated with the use of a single-pill ARV regimen in the UK, 2004-2008. PloS One. 2012;7(10):e47376. Accessed 15 Apr 2022
Bor J, Kluberg SA, LaValley MP, Evans D, Hirasen K, Maskew M, et al. One pill, once a day: simplified treatment regimens and retention in HIV care. Am J Epidemiol. 2022. https://doi.org/10.1093/aje/kwac006. Accessed 15 Apr 2022
WHO/International Bank for Reconstruction and Development/The World Bank. Tracking universal health coverage: 2017 global monitoring report, 2017. https://www.who.int/publications/i/item/9789241513555. Accessed 15 Apr 2022.
Acknowledgements
The authors are grateful for all the people living with HIV that were part of the EmERGE study at the five sites, the staff in each of the sites that enabled the study to be performed and successfully completed, as well as the support from other colleagues of the EmERGE Consortium. The authors also thank the reviewers and editors for their comments, which substantially improved the paper.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
Funding was provided by Horizon 2020 (Grant no. 643736).
Conflict of interest
The authors have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Ethics approvals were obtained for each of the five clinics involved with the study, including: Institutional Review Board of the Institute of Tropical Medicine, Antwerp, Belgium; Ethics Committee of the University Hospital for Infectious Diseases, Dr. Fran Mihaljevic, Zagreb, Croatia; Comite Etico de lnvestigacion Clinica del Hospital Clinic de Barcelona, University of HC-IDIBAPS, Barcelona, Spain; Comissao de Etica para a Saude, Hospital Capuchos, Centro Hospitalar De Lisboa Central, EPE (HC-CHLC), Lisbon, Portugal; South East Coast-Brighton & Sussex Research Ethics Committee, Brighton and Sussex University Hospitals NHS Trust, Brighton, UK.
Consent for publication and Availability of data and materials
Consent was obtained from participants to participate in the Study, and their consent for the publication and availability of data and materials
Authors’ contributions
EJB, SM and PY developed the health economic aspects of the EMERGE Project in collaboration with AL, FG, LA, JB, MdFB and JW; PY, EJB, SM, AL, MJM, FG, MW, AL, IB, SZ, JB, ASC, ET, GR, MdFB, DF, JV and JW were responsible for the data collection; EJB, SM and PY were responsible for the analyses; EJB and SM were the lead authors in collaboration with PY, AL, MJM, FG, MW, LA, IB, SZ, JB, ASC, ET, GR, MdFB, DF, JV and JW, who all reviewed and commented on drafts of the paper.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Beck, E.J., Mandalia, S., Yfantopoulos, P. et al. Efficiency of the EmERGE Pathway of Care in Five European HIV Centres. PharmacoEconomics 40, 1235–1246 (2022). https://doi.org/10.1007/s40273-022-01193-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-022-01193-z