Abstract
Context
Obesity impacts both individual health and, given its high prevalence, total health care spending. However, as medical technology evolves, health outcomes for a number of obesity-related illnesses improve. This article examines whether medical innovation can mitigate the adverse health and spending associated with obesity, using statins as a case study. Because of the relationship between obesity and hypercholesterolaemia, statins play an important role in the medical management of obese individuals and the prevention of costly obesity-related sequelae.
Methods
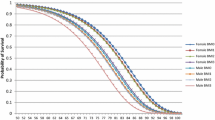
Using well-recognized estimates of the health impact of statins and the Future Elderly Model (FEM)—an established dynamic microsimulation model of the health of Americans aged over 50 years—we estimate the changes in life expectancy, functional status and health care costs of obesity due to the introduction and widespread use of statins.
Results
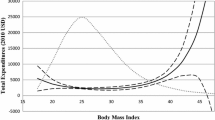
Life expectancy gains of statins are estimated to be 5–6 % greater for obese individuals than for healthy-weight individuals, but most of these additional gains are associated with some level of disability. Considering both medical spending and the value of quality-adjusted life-years, statins do not significantly alter the costs of class 1 and 2 obesity (body mass index [BMI] ≥30 and ≥35 kg/m2, respectively) and they increase the costs of class 3 obesity (BMI ≥40 kg/m2) by 1.2 %.
Conclusions
Although statins are very effective medications for lowering the risk of obesity-associated illnesses, they do not significantly reduce the costs of obesity.




Similar content being viewed by others
Notes
Body mass index is defined as the ratio between the mass of individuals, expressed in kilograms, and the square of height, expressed in metres.
Authors’ calculations with Medical Expenditure Panel Survey (MEPS) data. A MEPS respondent is defined as a statin user if he or she filled at least one prescription associated with the ‘HMG-CoA reductase inhibitor’ therapeutic subclass during a given year, or a prescription of Simcor, Advicor or Vytorin (which combine statins with other active ingredients). Therapeutic classes in the MEPS correspond to Multum Lexicon variables from Cerner Multum, Inc.
This interpretation is consistent with the Health and Retirement Survey (HRS) questionnaire, which asks respondents if they were ever diagnosed with a condition.
Since the HRS is biennial, we simulate health and costs over 2-year periods.
Therapeutic classes in the MEPS correspond to Multum Lexicon variables from Cerner Multum, Inc.
Authors’ calculations with MEPS data.
This is consistent with the Future Elderly Model (FEM) health transition models, which are estimated only for live individuals.
As detailed in Sect. 2.2.1, statistical significance refers to the 95 % confidence intervals with regard to the clinical uncertainty of the effectiveness of statins.
By doing so, we assume that the direct costs of statin therapy for the elderly will be stable at their 2010 levels in the future. This is consistent with the remainder of the FEM’s cost projections, which surmise that the costs of treatments remain proportional over time. The 2010 values, however, constitute a higher bound for the future cost of statin prescriptions, given the patent expiration for atorvastatin in 2011 and the forthcoming patient expiration for rosuvastatin in 2016. The 2010 prescription costs are converted into 2009 dollars, the base year for the FEM’s costs projections, using the US City Average Consumer Price Index (CPI) from the Bureau of Labor Statistics.
These are computed with the present values presented in Table 1. For instance, the medical care cost of class 2 obesity in the ‘with statins’ scenario ($24.5) corresponds to the difference between the total medical costs in individuals with a body mass index (BMI) of 35 and those with a BMI <25 in the ‘with statins’ column ($485.5 and $460.9, respectively).
References
Fryar CD, Carrol MD, Ogden CL. Prevalence of overweight, obesity, and extreme obesity among adults: United States, Trends 1960–1962 Through 2009–2010. National Center for Health Statistics: Hyattsville; 2012.
James WPT, Jackson-Leach R, Mhurchu CN, Kalamara E, Shayeghi M, Rigby NJ, Nishida C, Rodgres A. Chapter 8: overweight and obesity (high body mass index). In: Ezzati M, Lopez AD, Rodgers A, Murray CJL. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. Volume 1. Geneva: World Health Organization; 2004, p. 497–596.
Colditz GA. Economic costs of obesity. Am J Clin Nutr. 1992;55(2 Suppl):503S–7S.
Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: how much, and who’s paying? Health Aff. 2003;Suppl Web Exclusives:W3-219–26.
Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff. 2009;28(5):w822–31.
Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J Health Econ. 2012;31(1):219–30.
Chen YH, Feng B, Chen ZW. Statins for primary prevention of cardiovascular and cerebrovascular events in diabetic patients without established cardiovascular diseases: a meta-analysis. Exp Clin Endocrinol Diabetes. 2012;120(2):116–20.
Cholesterol Treatment Trialists Collaborators, Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380(9841):581–90.
de Vries FM, Denig P, Pouwels KB, Postma MJ, Hak E. Primary prevention of major cardiovascular and cerebrovascular events with statins in diabetic patients: a meta-analysis. Drugs. 2012;72(18):2365–73.
Gutierrez J, Ramirez G, Rundek T, Sacco RL. Statin therapy in the prevention of recurrent cardiovascular events: a sex-based meta-analysis. Arch Intern Med. 2012;172(12):909–19.
Mills EJ, Wu P, Chong G, Ghement I, Singh S, Akl EA, et al. Efficacy and safety of statin treatment for cardiovascular disease: a network meta-analysis of 170,255 patients from 76 randomized trials. QJM. 2011;104(2):109–24.
Taylor F, Huffman MD, Macedo AF, Moore TH, Burke M, Davey Smith G, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;1:CD004816.
Grabowski DC, Lakdawalla DN, Goldman DP, Eber M, Liu LZ, Abdelgawad T, et al. The large social value resulting from use of statins warrants steps to improve adherence and broaden treatment. Health Aff. 2012;31(10):2276–85.
Michaud PC, Goldman DP, Lakdawalla DN, Zheng Y, Gailey AH. The value of medical and pharmaceutical interventions for reducing obesity. J Health Econ. 2012;31(4):630–43.
Livingston EH. The incidence of bariatric surgery has plateaued in the US. Am J Surg. 2010;200(3):378–85.
Goldman DM, et al. Health status and medical treatment of the future elderly: final report. Santa Monica: RAND Corp; 2004.
Bhattacharya J, Shang B, Su CK, Goldman DP. Technological advances in cancer and future spending by the elderly. Health Aff. 2005;24 Suppl 2:W5R53–66.
Lakdawalla DN, Goldman DP, Shang B. The health and cost consequences of obesity among the future elderly. Health Aff. 2005;24 Suppl 2:W5R30–41.
Goldman DP, Zheng Y, Girosi F, Michaud PC, Olshansky SJ, Cutler D, et al. The benefits of risk factor prevention in Americans aged 51 years and older. Am J Public Health. 2009;99(11):2096–101.
Bhattacharya J, Sood N. Who pays for obesity? J Econ Perspect. 2011;25(1):139–58.
Merrill RM, Richardson JS. Validity of self-reported height, weight, and body mass index: findings from the National Health and Nutrition Examination Survey, 2001–2006. Prev Chronic Dis. 2009;6(4):A121.
Macroeconomics and Health. Investing in health for economic development. Geneva: World Health Organization; 2001. p. 2001.
Sugiyama T, Tsugawa Y, Tseng CH, Kobayashi Y, Shapiro MF. Different time trends of caloric and fat intake between statin users and nonusers among us adults: gluttony in the time of statins? JAMA Intern Med. 2014;174:1038–45.
Kaestner R, Darden M, Lakdawalla D. Are investments in disease prevention complements? The case of statins and health behaviors. J Health Econ. 2014;36:151–63.
Wei L, Ebrahim S, Bartlett C, Davey PD, Sullivan FM, MacDonald TM. Statin use in the secondary prevention of coronary heart disease in primary care: cohort study and comparison of inclusion and outcome with patients in randomised trials. Bmj. 2005;330(7495):821.
Acknowledgments
The authors did not receive financial support for conducting this study. Étienne Gaudette has no conflicts of interest to declare. Dana Goldman is a Partner at Precision Health Economics, a life sciences consulting company. Neeraj Sood has consulting relationships with Precision Health Economics and Bates White. Both firms have clients from the pharmaceutical industry. Andrew Messali is employed as a part-time consultant for Allergan, Inc. Allergan, Inc. played no role in funding or conducting this research.
Étienne Gaudette is the guarantor for the overall content of this article. He designed the simulation specifications and performed the analyses. Andrew Messali performed the literature review. Étienne Gaudette and Andrew Messali wrote the article. Neeraj Sood and Dana Goldman gave advice on the design of the study, the analyses that were performed and the interpretation of the results. All authors reviewed draft versions of the article and gave permission for the final version to be published.
The authors are grateful to Bryan Tysinger, Jeff Sullivan and Duncan Ermini Leaf for their expert technical help, and to the National Institute on Aging for its support through the Roybal Center for Health Policy Simulation (grant no. P30AG024968) and through Award Number P01AG033559. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gaudette, É., Goldman, D.P., Messali, A. et al. Do Statins Reduce the Health and Health Care Costs of Obesity?. PharmacoEconomics 33, 723–734 (2015). https://doi.org/10.1007/s40273-014-0234-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-014-0234-y