Abstract
Background
The results of animal experiments show that quinolone antibacterial drugs may permanently damage the soft tissues of the weight-bearing joints of young animals. Out of safety concerns, using quinolones in children has always been controversial.
Objective
The aim of this study was to assess the risk of using quinolones in children and provide evidence for clinicians to support decision making.
Data Sources
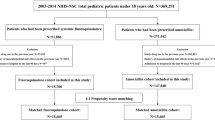
The MEDLINE (Ovid), EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL), International Pharmaceutical Abstracts (Ovid), CINAHL, CNKI, VIP, and WanFang Data databases were searched from inception to 8 September 2021.
Study Selection
All types of studies that reported the safety data of quinolones in children, including clinical trials and observational studies.
Data Extraction
Data extraction and cross-checking were completed by two independent reviewers using a pilot-tested standardized data extraction form.
Results
The overall incidence rate of adverse drug events (ADEs) in children using systemic quinolones was 5.39% and the most common ADEs were gastrointestinal reactions (incidence rate, 2.02%). Quinolone-induced musculoskeletal ADEs in children were uncommon (0.76%). Meta-analysis results showed that the risk of musculoskeletal ADEs in children using quinolones was higher than children in the control group (51 studies; rate ratio [RR] 2.03, 95% confidence interval [CI] 1.82–2.26; p < 0.001; I2 = 18.6%; moderate-quality evidence). However, the subgroup analysis results showed that differences might only be observed in children who were followed up for 2 months to 1 year (2–6 months: RR 2.56, 95% CI 2.26–2.89; 7 months to 1 year: RR 1.35, 95% CI 0.98–1.86). Moreover, children (adolescents) aged between 13 and 18 years might be sensitive to the musculoskeletal toxicity of quinolones (RR 2.69, 95% CI 2.37–3.05; moderate-quality evidence) and the risk of levofloxacin-induced musculoskeletal ADEs might be higher (RR 1.33, 95% CI 1.00–1.77; low-quality evidence).
Conclusions
Although the existing evidence shows that quinolone-induced musculoskeletal ADEs seem to be only short-term and reversible, and no serious skeletal and muscular system damage cases have been reported in children, quinolones should be avoided unless necessary in children because the incidence rate of quinolone-related ADEs is not low and they are broad-spectrum antibiotics that will induce the emergence of resistant strains if used frequently.



Similar content being viewed by others
References
Patel K, Goldman JL. Safety concerns surrounding quinolone use in children. J Clin Pharmacol. 2016;56(9):1060–75.
Gough A, Barsoum NJ, Mitchell L, McGuire EJ, de la Iglesia FA. Juvenile canine drug-induced arthropathy: clinicopathological studies on articular lesions caused by oxolinic and pipemidic acids. Toxicol Appl Pharmacol. 1979;51(1):177–87.
Tatsumi H, Senda H, Yatera S, Takemoto Y, Yamayoshi M, Ohnishi K. Toxicological studies on pipemidic acid. V. Effect on diarthrodial joints of experimental animals. J Toxicol Sci. 1978;3(4):357–67.
Simonin MA, Gegout-Pottie P, Minn A, Gillet P, Netter P, Terlain B. Proteoglycan and collagen biochemical variations during fluoroquinolone-induced chondrotoxicity in mice. Antimicrob Agents Chemother. 1999;43(12):2915–21.
Kastner M, Rahm U, Baumann-Wilschke I, Bello A, Stahlmann R. Concentrations of the des-F(6)-quinolone garenoxacin in plasma and joint cartilage of immature rats. Arch Toxicol. 2004;78(2):61–7.
Kappel EM, Shakibaei M, Bello A, Stahlmann R. Effects of the Des-F(6)-quinolone garenoxacin (BMS-284756), in comparison to those of ciprofloxacin and ofloxacin, on joint cartilage in immature rats. Antimicrob Agents Chemother. 2002;46(10):3320–2.
Machida M, Kusajima H, Aijima H, Maeda A, Ishida R, Uchida H. Toxicokinetic study of norfloxacin-induced arthropathy in juvenile animals. Toxicol Appl Pharmacol. 1990;105(3):403–12.
von Keutz E, Rühl-Fehlert C, Drommer W, Rosenbruch M. Effects of ciprofloxacin on joint cartilage in immature dogs immediately after dosing and after a 5-month treatment-free period. Arch Toxicol. 2004;78(7):418–24.
Etminan M, Guo MY, Carleton B. Oral fluoroquinolone prescribing to children in the United States from 2006 to 2015. Pediatr Infect Dis J. 2019;38(3):268–70.
Neame M, King C, Riordan A, Iyer A, Kneen R, Sinha I, Hawcutt DB. Seizures and quinolone antibiotics in children: a systematic review of adverse events. Eur J Hosp Pharm. 2020;27(2):60–4.
Bradley JS, Jackson MA. The use of systemic and topical fluoroquinolones. Pediatrics. 2011;128(4):e1034–45.
The use of systemic fluoroquinolones. Pediatrics. 2006;118(3):1287–1292.
Kubin R. Safety and efficacy of ciprofloxacin in paediatric patients—review. Infection. 1993;21(6):413–21.
Dixit A, Karandikar MV, Jones S, Nakamura MM. Safety and tolerability of moxifloxacin in children. J Pediatr Infect Dis Soc. 2018;7(3):e92–101.
Hampel B, Hullmann R, Schmidt H. Ciprofloxacin in pediatrics: worldwide clinical experience based on compassionate use—safety report. Pediatr Infect Dis J. 1997;16(1):127–129, 160–162.
Chyský V, Kapila K, Hullmann R, Arcieri G, Schacht P, Echols R. Safety of ciprofloxacin in children: worldwide clinical experience based on compassionate use. Emphasis on joint evaluation. Infection. 1991;19(4):289–96.
Schaad UB, Wedgwood-Krucko J. Nalidixic acid in children: retrospective matched controlled study for cartilage toxicity. Infection. 1987;15(3):165–8.
Adam D. Use of quinolones in pediatric patients. Rev Infect Dis. 1989;11(Suppl 5):S1113–6.
Jackson MA, Schutze GE. The use of systemic and topical fluoroquinolones. Pediatrics. 2016;138(5): e20162706.
Brown EG, Wood L, Wood S. The medical dictionary for regulatory activities (MedDRA). Drug Saf. 1999;20(2):109–17.
Neubert A, Dormann H, Prokosch HU, et al. E-pharmacovigilance: development and implementation of a computable knowledge base to identify adverse drug reactions. Br J Clin Pharmacol. 2013;76(Suppl 1):69–77.
Sterne J, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366: l4898.
Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355: i4919.
Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. 2011. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 27 Oct 2021.
The Joanna Briggs Institute. Joanna Briggs Institute reviewers’ munual: 2016 edition. Austrialia: The Joanna Briggs Institute; 2016. Joanna Briggs Institute. Critical appraisal tools. https://joannabriggs.org/ebp/critical_appraisal_tools. Accessed 16 July 2020.
Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Cochrane Handbook for Systematic Reviews of Interventions(Version 6.2, 2021): Chapter 8: Assessing risk of bias in a randomized trial. 2021. https://training.cochrane.org/handbook/current/chapter-08. Accessed 16 Dec 2021.
Gorelik E, Masarwa R, Perlman A, et al. Fluoroquinolones and cardiovascular risk: a systematic, review meta-analysis and network meta-analysis. Drug Saf. 2019;42(4):529–38.
Wallach JD, Wang K, Zhang AD, et al. Updating insights into rosiglitazone and cardiovascular risk through shared data: individual patient and summary level meta-analyses. BMJ. 2020;368: l7078.
Wang D, Mou ZY, Zhai JX, Zong HX, Zhao XD. Application of Stata software to test heterogeneity in meta-analysis method [in Chinese]. Zhonghua Liu Xing Bing Xue Za Zhi. 2008;29(7):726–9.
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193–206.
Petitti DB. Approaches to heterogeneity in meta-analysis. Stat Med. 2001;20(23):3625–33.
Melsen WG, Bootsma MC, Rovers MM, Bonten MJ. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin Microbiol Infect. 2014;20(2):123–9.
Higgins J, Thomas J, Chandler J, et al. Jonathan J Deeks, Julian PT Higgins, Douglas G Altman; on behalf of the Cochrane Statistical Methods Group. Cochrane Handbook for Systematic Reviews of Interventions: Chapter 10: analysing data and undertaking meta-analyses (version 6.2, updated July 2021). 2021.
US Dept of Health and Human Services, Food and Drug Administration. Guidance for industry and FDA staff: pediatric expertise for advisory panels. 2003. https://www.fda.gov/media/72451/download. Accessed 27 Aug 2021.
Hardin AP, Hackell JM. Age limit of pediatrics. Pediatrics. 2017;140(3): e20172151.
Liu J, Li L, Li S, et al. Sodium-glucose co-transporter-2 inhibitors and the risk of diabetic ketoacidosis in patients with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Obes Metab. 2020;22(9):1619–27.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339: b2700.
Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
Zimbabwe BSAD. Multicenter, randomized, double blind clinical trial of short course versus standard course oral ciprofloxacin for Shigella dysenteriae type 1 dysentery in children. Pediatr Infect Dis J. 2002;1(12):1136–41.
Zhang YQ, Huang B, Liu JH, et al. Efficacy of ciprofloxacin in the treatment of pediatric severe infections. Chin J Antibiot. 2005;30(7):416–9.
Goldblatt EL, Dohar J, Nozza RJ, et al.. Topical ofloxacin versus systemic amoxicillin/clavulanate in purulent otorrhea in children with tympanostomy tubes. Int J Pediatr Otorhinolaryngol. 1998;46(1-2):91-101.
Salam MA, Dhar U, Khan WA, Bennish ML. Randomized comparison of ciprofloxacin suspension and pivmecillinam for childhood shigellosis. Lancet. 1998;352:522–7.
Laoprasopwattana K, Khwanna T, Suwankeeree P, Sujjanunt T, Tunyapanit W, Chelae S. Ciprofloxacin reduces occurrence of fever in children with acute leukemia who develop neutropenia during chemotherapy. 2013;1(3):e94–e98.
Treggiari M, Retsch-Bogart G, Mayer-Hamblett N, et al. Comparative efficacy and safety of four randomized regimens to treat early Pseudomonas aeruginosa infection in children with cystic fibrosis. J Cyst Fibros. 2010;1:S54.
Leach A, Wood Y, Gadil E, Stubbs E, Morris P. Topical ciprofloxin versus topical framycetin-gramicidin-dexamethasone in Australian aboriginal children with recently treated chronic suppurative otitis media: a randomized controlled trial. Pediatr Infect Dis J. 2008;1(8):692–98.
Wang ShM. Efficacy of ofloxacin eye drops in treating acute conjunctivitis in children. Journal of North Pharmacy. 2014;1:24–5.
Wang MF. To observe the clinical effect of cefaclor in treatment of children with urinary tract infection. World Latest Med Inf. 2015;5:98–9.
Tang F, Huang JH. Analysis of ofloxacin in the treatment of 58 children with bacillary dysentery. Pract Clin Med. 2002;3(6):91–2.
Sun F, Zhang XH. Clinical observation of 0.5% levofloxacin eye drops on children’s bacterial conjunctivitis. Contemp Med. 2009;15(22):146.
Shu XM. The clinical effect of ofloxacin eye drops combined with ganciclovir eye drops in the treatment of children with acute conjunctivitis. China Mod Med. 2018;25(32):128–30.
Shao W, Zhang FL. Observation on the curative effect of levofloxacin eye drops in the treatment of 172 children with acute conjunctivitis. Inner Mongolia J Tradit Chin Med. 2013;32(5):87–8.
Ouyang K, Li L, Tan Zh. Observation on the clinical efficacy and side effects of ofloxacin in the treatment of 154 children with acute bacillary dysentery. J Clin Exp Med. 2008;11:48–9.
Liu ChL. The safety analysis of tobramycin eye drops in the application of bacterial infection of external eye diseases in children. Chin Foreign Med Res. 2017;15(3):138–40.
Lin M, Guan CL, Zhang ShK, Su DM. Clinical effect of tobramycin eye drops in the treatment of bacterial infections of external eye diseases in children. Int Med Health Guid News. 2014;20(6):824–6.
Li WL, Mai BW. A clinical comparative study of two types of antibiotics-assisted glucocorticoid combined with intravenous drip in the treatment of children with RMP. Chin J Control Endem Dis. 2017;32(5):547–8.
Li JL. Analysis of the clinical efficacy of norfloxacin and Yunnan Baiyao Topical in the treatment of newborn. Mod Diagn Treat. 2014;16:3684–5.
Li ChP. Clinical effect of andrographolide injection combined with levofloxacin on treating infantile diarrhea. J Clin Med Pract. 2018;22(1):14–7.
Lei YL. Clinical analysis of ofloxacin ear drops in the treatment of children with acute suppurative otitis media. Med Equip. 2015;11:127–127.
Jin YZ. Observation and protective measures of 0.5% levofloxacin eye drops in the treatment of children with acute bacterial conjunctivitis. China Health Care Nutr. 2012;22(6):1379–80.
Huang YX, Zhang MQ, Chen JN. Effect of levofloxacin eye drops and ganciclovir eye drops on acute conjunctivitis in children. J Qiqihar Med Univ. 2019;40(21):2444–5.
Hu ZhQ. Observation of therapeutic effect of ofloxacin on 30 children with mycoplasma pneumonia. Anthol Med. 2001;20(6):845–6.
Hu GH, Hu ChY. Ofloxacin in the treatment of 30 children with Freund’s resistant bacillary dysentery. Her Med. 2005;24(5):399–400.
Fu JJ, Lin P. The effect of cefixime granules in the treatment of children with acute gonococcal urethritis. Shenzhen J Integr Tradit Chin West Med. 2018;28(23):119–20.
Feng YY, Wang XH, An W. Clinical observation of ofloxacin and ciprofloxacin in the treatment of infantile typhoid fever. J Med Forum. 1999;09:22–3.
Dai XY. Observation on the clinical effect of high-concentration levofloxacin eye drops in the treatment of stye in children. For All Health. 2017;11(6):186–7.
Cruciani M, Concia E, Navarra A, et al. Prophylactic co-trimoxazole versus norfloxacin in neutropenic children—perspective randomized study. Infection. 1989;1(2):65–9.
Mair EA, Moss JR, Dohar JE, Antonelli PJ, Bear M, LeBel C. Randomized clinical trial of a sustained-exposure ciprofloxacin for intratympanic injection during tympanostomy tube surgery. Ann Otol Rhinol Laryngol. 2016;1(2):105–114.
Noel GJ, Blumer JL, Pichichero ME, et al. A randomized comparative study of levofloxacin versus amoxicillin/clavulanate for treatment of infants and young children with recurrent or persistent acute otitis media. Pediatr Infect Dis J. 2008;1(6):483–89.
Park AH, White DR, Moss JR, Bear M, LeBel C. Phase 3 trials of thermosensitive ciprofloxacin gel for middle ear effusion in children with tubes. Otolaryngol Head Neck Surg. 2016;1(2):324–31.
Sáez-Llorens X, McCoig C, Feris JM, et al. Quinolone treatment for pediatric bacterial meningitis: a comparative study of trovafloxacin and ceftriaxone with or without vancomycin. Pediatr Infect Dis J. 2002;21(1):14–22.
Saez-Llorens X, Rodriguez A, Arguedas A, et al. Randomized, investigator-blinded, multicenter study of gatifloxacin versus amoxicillin/clavulanate treatment of recurrent and nonresponsive otitis media in children. Pediatr Infect Dis J. 2005;1(4):293–300.
Cao XT, Kneen R, Nguyen TA, Truong DL, White NJ, Parry CM. A comparative study of ofloxacin and cefixime for treatment of typhoid fever in children. The Dong Nai Pediatric Center Typhoid Study Group. Pediatr Infect Dis J. 1999;18(3):245–8.
Sher L, Arguedas A, Husseman M, Pichichero M, et al. Randomized, investigator-blinded, multicenter, comparative study of gatifloxacin versus amoxicillin/clavulanate in recurrent otitis media and acute otitis media treatment failure in children. Pediatr Infect Dis J. 2005;24(4):301–08.
Zhang XZ. Effect comparison of ofloxacin eye drops on children with acute conjunctivitis. China Med Her. 2011;8(27):146–8.
Zhang XK. Analysis of the effect of piperacillin sodium and tazobactam sodium on serum CRP and ESR levels in children with bacterial pneumonia. J North Pharm. 2019;16(4):61–2.
Zhang DJ. Evaluation of the clinical efficacy and safety of the combined regimen of moxifloxacin and montelukast in the treatment of mycoplasma pneumonia in children. Chin J Mod Drug Appl. 2021;15(03):144–6.
Yuan LZh. Clinical analyse of 55 cases of ofloxacin treatment in children shigella flexneri. Hebei Med. 2004;10(5):421–2.
Yu D, Wang Y, Fan WT, Mu XH, Liao W. The treatment research of quinolones using in refractory mycoplasma pneumonia. Prog Mod Biomed. 2014;14(15):2939–42.
Xu JH. Analysis of clinical effect of two eye drops in children with acute conjunctivitis. Syst Med. 2020;5(10):54–6.
Wang YX. Observation on clinical curative effect of 60 children with acute gastroenteritis. Med Inf. 2014;9:479–479.
Jin P. Comparison of the effect of ofloxacin and chloramphenicol in the treatment of suppurative otitis media. Chin Community Doctors. 2017;33(4):75–6.
Jiang H. Critical analysis of 45 cases of bacillary dysentery in children treated with ciprofloxacin and smecta. Diet Health. 2021;15:83.
Wirth S, Emil SGS, Engelis A, et al. Moxifloxacin in pediatric patients with complicated intra-abdominal infections: results of the MOXIPEDIA randomized controlled study. Pediatr Infect Dis J. 2018;1(8):e207–e213.
Torrelo A, Grimalt R, Masramon X, Albareda Lopez N, Zsolt I. Ozenoxacin, a new effective and safe topical treatment for impetigo in children and adolescents. Dermatology. 2020;1(3):199–207.
Spektor Z, Pumarola F, Ismail K, et al. Efficacy and safety of ciprofloxacin plus fluocinolone in otitis media with tympanostomy tubes in pediatric patients: a randomized clinical trial. JAMA Otolaryngol Head Neck Surg. 2017;143(4):341–9.
An XY, Qi WB, Zhou F, Chen HF, Wei YM. Analysis of the efficacy and adverse reactions of ciprofloxacin on neonatal nosocomial infection. Med Aesthet Cosmetol. 2014;8:459–60.
Macfadyen C, Gamble C, Garner P, et al. Topical quinolone vs. antiseptic for treating chronic suppurative otitis media: a randomized controlled trial. Trop Med Int Health. 2005;1(2):190–97.
Sanfilippo CM, Allaire CM, DeCory HH. Besifloxacin ophthalmic suspension 0.6% compared with gatifloxacin ophthalmic solution 0.3% for the treatment of bacterial conjunctivitis in neonates. Drugs R D. 2017;17(1):167–175.
McDonald MB, Protzko EE, Brunner LS, et al. Efficacy and safety of besifloxacin ophthalmic suspension 0.6% compared with moxifloxacin ophthalmic solution 0.5% for treating bacterial conjunctivitis. Ophthalmology. 2009;1(9):1615–23.
Lichtenstein SJ, Rinehart M, Levofloxacin Bacterial Conjunctivitis Study G. Efficacy and safety of 0.5% levofloxacin ophthalmic solution for the treatment of bacterial conjunctivitis in pediatric patients. J AAPOS. 2003;1(5):317–24.
Schwartz RH. Once-daily ofloxacin otic solution versus neomycin sulfate/polymyxin B sulfate/hydrocortisone otic suspension four times a day: a multicenter, randomized, evaluator-blinded trial to compare the efficacy, safety, and pain relief in pediatric patients with otitis externa. Curr Med Res Opin. 2006;1(9):1725–36.
Petrilli AS, Dantas LS, Campos MC, Tanaka C, Ginani VC, Seber A. Oral ciprofloxacin vs. intravenous ceftriaxone administered in an outpatient setting for fever and neutropenia in low-risk pediatric oncology patients: randomized prospective trial. Med Pediatr Oncol. 2000;1(2):87–91.
Ye Y, Chen Y, Lu JL. Comparison of clinical efficacy of azithromycin and norfloxacin in the treatment of acute gastroenteritis in children. Drug Eval Res. 2018;41(2):272–4.
Dai YH, Ye MY. Comparative analysis of clinical effects of azithromycin and norfloxacin in the treatment of acute gastroenteritis in children. China Med Pharm. 2018;8(20):48–50.
Zhang D, Guo R. Comparison of the effects of azithromycin and pefloxacin in the treatment of acute gastroenteritis in children. China Pract Med. 2016;11(17):193–4.
Lu YH. Comparison of the effects of azithromycin and pefloxacin in the treatment of children with acute gastroenteritis. World Latest Med Inf. 2019;19(18):133–43.
Li X, Liu HY, Deng B, Sun JY. Study on chemotherapy regimen for severe tuberculosis in children. Health Must Read. 2021;14:219.
Xing XQ. The effect of high-concentration levofloxacin eye drops combined with ear tip bloodletting in the treatment of stye. Pract Clin Med. 2019;20(12):42–3.
Zhu ChM, AiH Z, Chen ShY. Clinical efficacy and side effect of ciprofloxacin in comparison with pipemidic in the treatment of acute bacillary dysentery of 46 children. J Pediatr Pharm. 2000;3:18–32.
Huang YY. Observation on the curative effect of ciprofloxacin in the treatment of 36 children with typhoid fever. Guizhou Med J. 2001;25(4):363–4.
Wang JX, Liu ChL, Luode Ch, Dai YL, Ju R, Li K. Clinical study of ciprofloxacin in the treatment of 41 children with bacillary dysentery. Med J Natl Defend Forces Northwest China. 1999;20(4):309–10.
Guan X, Chen X. Clinical observation of gatifloxacin in the treatment of 60 neonates with bacterial conjunctivitis. Tibet Med. 2016;37(02):31–2.
Guo F. Efficacy of lomefloxacin ear drops in the treatment of acute suppurative otitis media. Friends Health. 2020;14:87.
Zhao YH. Observation on the curative effect and side effects of ofloxacin in the treatment of 154 children with acute bacillary dysentery. Chongqing Med. 2003;32(11):1550–1.
Richard DA, Nousia-Arvanitakis S, Sollich V, Hampel BJ, Sommerauer B, Schaad UB. Oral ciprofloxacin vs. intravenous ceftazidime plus tobramycin in pediatric cystic fibrosis patients: comparison of antipseudomonas efficacy and assessment of safety with ultrasonography and magnetic resonance imaging. Cystic Fibrosis Study Group. Pediatr Infect Dis J. 1997;1(6):572–8.
Nie JH. Comparative analysis of ofloxacin and cefoperazone in the treatment of typhoid fever. Chin J Prim Med Pharm. 2005;12(9):1248–9.
Zhou XR, Yin FL, Zhang ChL, Jia LX. Observation of the curative effect of azithromycin in the treatment of children with acute gastroenteritis. Mother Baby World. 2021;10:129.
Zhao DSh. The effect of azithromycin in the treatment of mycoplasma pneumonia. Yiyao Qianyan. 2012;2(10):131–2.
Yang H, Wu DX, Wu HF. Analysis of ofloxacin in the treatment of 45 children with bacterial dysentery. Chin J Coal Ind Med. 2000;3(3):272.
Sheng L. Tratment of bacillary dysenteryin children by ciprofloxacin. Anhui Med J. 2007;28(3):229–30.
Shao HM. Efficacy of ciprofloxacin in neonatal nosocomial infection and analysis of its adverse drug reaction. Chin J Clin Pharmacol. 2013;29(1):25–7.
Secmeer G, Kanra G, Figen G, Akan O, Ceyhan M, Ecevit Z. Ofloxacin versus co-trimoxazole in the treatment of typhoid fever in children. 1997;1(2):218–221.
Moulin F, Raymond J, Bergeret M, et al. Échees du traitement antibiotique des salmonelloses sévères de l'enfant et utilisation des quinolones. Archives de pédiatrie. 1995;2(4):317–3.
Zhong WY. Analysis and research on the efficacy of piperacillin sodium and tazobactam sodium in the treatment of children with bronchopneumonia. Diet Health. 2018;5(23):86–7.
Zhao ZhX. Analysis of clinical treatment effect of acute gastroenteritis in children. Med Inf. 2012;25(9):122–3.
Chen Zh, Wang DF, Lu WN, Liang L. Comparison of the effects of tobramycin eye drops and ofloxacin eye drops in the treatment of children with acute conjunctivitis. Contemp Med Symp. 2016;14(12):175–6.
Ji FZh. Selection of topical antibiotics for staphylococcus aureus infectious skin diseases. Dermatol Venereol. 2018;40(1):107–8.
Tao XG, Duan YY, Dong LL, Liu XL, Pei BF, Ma ShL, et al. Safety and effectiveness of levofloxacin and doxycycline in children with refractory mycoplasma pneumonia. Central South Pharm. 2021;19(5):1025–8.
Alrwisan A, Antonelli PJ, Winterstein AG. Quinolone ear drops after tympanostomy tubes and the risk of eardrum perforation: a retrospective cohort study. Clin Infect Dis. 2017;64(8):1052–8.
Kim Y, Paik M, Khan C, Kim YJ, Kim E. Real-world safety evaluation of musculoskeletal adverse events associated with Korean pediatric fluoroquinolone use: a nationwide longitudinal retrospective cohort study. Sci Rep. 2019;9(1):20156.
Noel GJ, Bradley JS, Kauffman RE, et al. Comparative safety profile of levofloxacin in 2523 children with a focus on four specific musculoskeletal disorders. Pediatr Infect Dis J. 2007;26(10):879–91.
Chen JH, Liu Zh, Liang DD. Study on clinical comparison of tobramycin eye drops and ofloxacin eye drops in the treatment of children with acute conjunctivitis. Chin J Mod Drug Appl. 2019;13(3):80–1.
Zeng WH. Pharmacoeconomic evaluation of 5 treatment options for bacterial pneumonia in children. Shenzhen J Integr Tradit Chin West Med. 2015;25(15):187–8.
Chen JB. Clinical observation of 86 cases of acute gastroenteritis in children. Mod Diagn Treat. 2012;23(9):1501–2.
Ye SZ. Research of clinical application of ofloxacin ear drops in the treatment of acute suppurative otitis media. China Pract Med. 2016;11(32):63–4.
Xu YX, Li ChL, Yang G, et al. Clinical analysis of ofloxacin ear drops in children with acute suppurative otitis media. Chin J Mod Drug Appl. 2019;13(6):135–6.
Tang ShJ, Ni YF. Observation on the efficacy and safety of ciprofloxacin in the treatment of children’s bacillary dysentery. Chin J Prim Med Pharm. 2001;8(4):357–8.
Sun XH, Zhao Y. Efficacy of different medication methods in the treatment of infantile dacryocystitis. Guide China Med. 2020;18(2):29–30.
Liu YG, Lin N, Li Q, Huang YY. Remote effect of ciprofloxacin on osteoarticular condition in children. Chin J Appl Clin Pediatr. 2000;15(1):48–9.
Liu XB. Clinical research on urinary system diseases in pediatrics. China Health Nutr. 2016;26(13):104–5.
Li Y. Follow-up observation on the effect of norfloxacin on neonatal bone dysplasia. J Pediatr Pharm. 1998;4(2):23–4.
Chalumeau M, Tonnelier S, D'Athis P, Tréluyer JM, et al. Fluoroquinolone safety in pediatric patients: a prospective, multicenter, comparative cohort study in France. Pediatrics. 2003;111(6 Pt 1):e714–719.
Yu PH, Hu CF, Liu JW, et al. The incidence of collagen-associated adverse events in pediatric population with the use of fluoroquinolones: a nationwide cohort study in Taiwan. BMC Pediatr. 2020;1(1):64.
Alban J. Urinary tract infections in children: experience with nalidixic acid. Curr Ther Res Clin Exp. 1970;12:577–9.
Cheesbrough JS, Mwema FI, Green SD, Tillotson GS. Quinolones in children with invasive salmonellosis. Lancet. 1991;338:127.
Dutta P, Rasaily R, Saha MR, Mitra U, Lahiri M, Et A. Ciprofloxacin for treatment of severe typhoid fever in children. Antimicrob Agents Chemother. 1993;37(May):1197–9.
Palmejar AR, Kuhn RJ, Kanga JF. Retrospective evaluation of the safety of oral ciprofloxacin in pediatric patients with cystic fibrosis. Palmejar.1990;25: CP–8.
Peltola H, Ukkonen P, Saxen H, Stass H. Single dose and steady state pharmacokinetics of a new oral suspension of ciprofloxacin in children. Pediatrics. 1998;101:658–62.
Sideri G, Kafetzis DA, Vouloumanou EK, Papadatos JH, Papadimitriou M, Falagas ME. Ciprofloxacin in critically ill children. 2011;1(4):635–639.
Vinh H, Wain J, Hanh VT, Nga CN, White NJ, Et A. Two or three days of ofloxacin treatment for uncomplicated multidrug resistant typhoid fever in children. Antimicrob Agents Chemother. 1996;40:958–61.
Wang WH. Adverse reactions and nursing care of children with intravenous ciprofloxacin. Shandong Med J. 2002;42(4):59.
Shen ShR, Guo XY. Ciprofloxacin in the treatment of 50 cases of severe bacillary dysentery. Chin J Appl Clin Pediatr. 2001;16(3):171–2.
Qian SY, Chen XN, Fan XM, Qi YJ, Geng R, Wu JCh, et al. Use of ciprofloxacin children With severe infections in pediatric intensive care unit. Chin J Emerg Med. 2001;10(3):161–3.
Ma ShJ. Observation on the curative effect of integrated traditional Chinese and western medicine in children with toxic dysentery. Chin J Ethnomed Ethnopharm. 2012;21(20):37–37.
Lu CL. Talking about the application of quinolones in children urgently need to be regulated. Chin J Ethnomed Ethnopharm. 2010;19(6):51–2.
Liu JX. Clinical observation of levofloxacin in the treatment of drug-resistant bacillary dysentery in children. J Gannan Med Univ. 2009;29(4):619.
Li P. The clinical use of quinolones in pediatrics and the study of experimental cartilage toxicity. Fudan University. 2004.
Li LSh. Analysis of levofloxacin in treatment of 38 children with typhoid fever. Proc Clin Med. 2010;19(1):31–2.
Hao YG, Li RX. Talking about the adverse reactions of intravenous ciprofloxacin in children. J Pract Med Tech. 2002;9(7):550–550.
Chen XQ, Zhang L. Clinical application of quinolones in pediatric infectious diseases. Clin Med Eng. 2011;18(05):795–6.
Infant overdose of nalidixic acid causes benign intracranial hypertension. Pharm Progr. 1991;(01):59–62.
Di ChY, Qu LP, Bao Y. Observation on the efficacy of fosfomycin plus ofloxacin in the treatment of drug-resistant bacillary dysentery in children. Chin Community Doctors. 2005;21(11):30.
Jick S. Ciprofloxacin safety in a pediatric population. 1997;1(1):130–133, 133–134, 160–162.
Johansson A, Berglund L, Gothefors L, Sjostedt A, Tarnvik A. Ciprofloxacin for treatment of tularemia in children. 2000;1(5):449–453.
Kim Y, Park GW, Kim S, et al. Fluoroquinolone and no risk of Achilles-tendinopathy in childhood pneumonia under eight years of age-a nationwide retrospective cohort. J Thorac Dis. 2021;1(6):3399–3408.
Tsunekazu H, Shigekazu K, Kan-Etsu O, Yutaka K. Clinical studies on norfloxacin in the field of pediatrics. Jpn J Antibiot. 1990;43(5):842–51.
Iwai N, Nakamura H, Miyazu M, Katayama M, Kasai K. Basic and clinical studies on norfloxacin in the pediatric field. Jpn J Antibiot. 1990;1(9):1629–48.
Pariente-Khayat A, Vauzelle-Kervroedan F, D'Athis P, et al. Retrospective survey of fluoroquinolone use in children. Arch Pediatr. 1998;1(5):484–8.
Ishikawa J, Matsuura T, Nagai H, Kida K, Matsuda H, Murase M. Clinical effect of norfloxacin in pediatric field. Jpn J Antibiot. 1990;1(5):877–83.
Leibovitz E, Piglansky L, Raiz S, et al. Bacteriologic and clinical efficacy of oral gatifloxacin for the treatment of recurrent/nonresponsive acute otitis media: an open label, noncomparative, double tympanocentesis study. Pediatr Infect Dis J. 2003;1(11):943–9.
Orenstein DM, Pattishall EN, Noyes BE, Kurland G, Hartigan ER, Yu VL. Safety of ciprofloxacin in children with cystic fibrosis. Clin Pediatr (Phila). 1993;1(8):504–6.
Stass H, Lettieri J, Vanevski KM, et al. Pharmacokinetics, safety, and tolerability of single-dose intravenous moxifloxacin in pediatric patients: dose optimization in a phase 1 study. J Clin Pharmacol. 2019;59(5):654–67.
Chien S, Wells TG, Blumer JL, Kearns GL, et al. Levofloxacin pharmacokinetics in children. J Clin Pharmacol. 2005 Feb;45(2):153–60.
Arguedas A, Dagan R, Pichichero M, Leibovitz E, et al. An open-label, double tympanocentesis study of levofloxacin therapy in children with, or at high risk for, recurrent or persistent acute otitis media. Pediatr Infect Dis J. 2006;25(12):1102–9.
Arguedas A, Sher L, Lopez E, Sáez-Llorens X,et al. Open label, multicenter study of gatifloxacin treatment of recurrent otitis media and acute otitis media treatment failure. Pediatr Infect Dis J. 2003;22(11):949–56.
Pradhan KM, Arora NK, Jena A, Susheela AK, Bhan MK. Safety of ciprofloxacin therapy in children: magnetic resonance images, body fluid levels of fluoride and linear growth. Acta Paediatr. 1995;1(5):555–60.
Zhang LN. Analysis and exploration of neonatal allergic reaction to antibacterial drugs. Baojianwenhui. 2021;22(16):157–8.
Zhang JT. Analysis of adverse drug reactions in children’s clinical medication. China J Pharm Econ. 2013;S3:395–6.
Zhang DF, Chen MJ. Analysis of the clinical use of quinolones in pediatric infectious diseases. Mod Health Med Innov Res. 2008;5(20):88–90.
Yu AH, Han TZh, Yang Sh, Wang JL, Luo ShF, Yang LG, et al. Observation on the safety of norfloxacin to children. Chin J Pediatr. 1991;04:223–4.
Yang ShF. Norfloxacin-induced elevation of intracranial pressure in 17 infants. Chin J New Drugs Clin Remedies. 1992;02:85.
Yang M, Qian SY. Analysis of the application of quinolones in severe infections in children. Chin J Emerg Med. 2018;27(11):1271–5.
Wang GT, Zeng TC. Effect of ciprofloxacin in newborns with ventilator-associated pneumonia. J Pediatr Pharm. 2004;10(1):25–37.
Li BH. Observation of the curative effect of ciprofloxacin in the treatment of 231 cases of infectious diarrhea. J Hubei Med Staff Coll. 1999;2:14–5.
Jiang SW. The effect of the third-generation quinolones on the bones and joints of children. J Clin Res. 1997;14(3):183.
Dong FQ. Analysis of adverse reactions of quinolones in pediatrics. Pract Clin J Integr Tradit Chin West Med. 2013;13(07):91.
H S, Lettieri J, Vanevski K, et al. Safety, tolerability and pharmacokinetics (PK) of single dose intravenous moxifloxacin in pediatric patients. Clin Pharmacol Ther. 2019;(1):S97–S98.
Redmond A, Sweeney L, MacFarland M, Mitchell M, Daggett S, Kubin R. Oral ciprofloxacin in the treatment of pseudomonas exacerbations of paediatric cystic fibrosis: clinical efficacy and safety evaluation using magnetic resonance image scanning. J Int Med Res. 1998;1(6):304–312.
Smith C, Sierra C, Robbins J, Cobbina E. Enteral ciprofloxacin or levofloxacin for ventilator-associated tracheobronchitis in children. Crit Care Med. 2021;49(1 Suppl 1):491.
Lang R, Goshen S, Raas-Rothschild A, et al. Oral ciprofloxacin in the management of chronic suppurative otitis media without cholesteatoma in children: preliminary experience in 21 children. Pediatr Infect Dis J. 1992;1(11):925–9.
Morita H, Tomoda T, Araki K, et al. Clinical efficacy and safety of norfloxacin tablets in pediatrics. Jpn J Antibiot. 1990;1(5):884–9.
Moulin F, Sauvé-Martin H, Marc E, et al. Ciprofloxacine après échec des β-lactamines dans les salmonelloses de l’enfant. Archives de pédiatrie. 2003;10(7):608–14.
Okada K, Kagami S. Clinical study on norfloxacin in children. Jpn J Antibiot. 1990;1(5):890–4.
Okada T, Furukawa S. Clinical evaluation of norfloxacin in pediatrics. Jpn J Antibiot. 1990;1(5):895–900.
Raymond J, Moulin F, Badoual J, Gendrel D. Eradication of convalescent-phase Salmonella carriage in children with two oral doses of pefloxacin. Eur J Clin Microbiol Infect Dis. 1994;1(4):307–10.
Yildirim P. Association patterns in open data to explore ciprofloxacin adverse events. Appl Clin Inform. 2015;1(4):728–47.
Zheng YF, Yuan L, Su DQ, Zhuo ZhQ. Quinolones combined with fiberoptic bronchoscopy in the treatment of refractory Mycoplasma pneumoniae pneumonia in children. Chin Pediatr Emerg Med. 2020;27(11):871–3.
Chang ChM. Observation on the efficacy of ganciclovir in the treatment of lower respiratory tract infections in children. J Clin Pulm Med. 2010;15(12):1820–1.
Lipman J, Gous AG, Mathivha LR, et al. Ciprofloxacin pharmacokinetic profiles in paediatric sepsis: how much ciprofloxacin is enough? Intensive Care Med. 2002;1(4):493–500.
Kuno K, Ogawa A, Nakao Y, Hayakawa F, Ando Y, Kito O. Bacteriological and clinical studies on norfloxacin in the field of pediatrics. Jpn J Antibiot. 1990;1(5):842–51.
Khan DM, Bhutta ZA. Ciprofloxacin in multi-resistant infections in childhood: an audit. J Pak Med Assoc. 1995;1(6):147–50.
Hidenori M, Toshiaki A, Koji U, Chizuru N, Tatsuhiko S, Ryochi F. Clinical evaluation of norfloxacin in children. Jpn J Antibiot. 1990;43(5):790–8.
Atasoy H, Erdem G, Ceyhan M, Ecevit Z, Kanra G. Hypertension associated with ciprofloxacin use in an infant. Ann Pharmacother. 1995;29:1049.
Mukherjee A, Dutta P, Lahiri M, Sinha S, Bhattacharya SK, Et A. Benign intracranial hypertension after nalidixic acid overdose in infants. Lancet. 1990;335(8705):1602.
Nabben FAE. Transient neurological symptoms and ocular abnormalities in a child during treatment with nalidixic acid. Ned Tijdschr Geneeskd. 1971;115(17):751–2.
Upton C. Sleep disturbance in children treated with ofloxacin. BMJ. 1994;309(6966):1411.
Zhang SZh, Wu XZh. Two cases of toxic hepatitis in children caused by norfloxacin. Pract J Clin Med. 1993;01:79.
Vignesh AP, Srinivasan R, Karanth S. A case report of severe corneal toxicity following 0.5% topical moxifloxacin use. 2015;1(1):63–65.
Jiang JZh. Norfloxacin causes severe headache in children. Adverse Drug React J. 1999;1(3):191.
Lantner RR. Ciprofloxacin desensitization in a patient with cystic fibrosis. 1995;1(6 Pt 1):1001–1002.
van der Laan LE, Schaaf HS, Solomons R, et al. Probable levofloxacin-associated secondary intracranial hypertension in a child with multidrug-resistant tuberculosis. Pediatr Infect Dis J. 2016;1(6):706–708.
Zhang H. A case of convulsion caused by overdose of norfloxacin in a child. Chongqing Med. 2003;32(5):546.
Zhai HQ, Shen DX. A case report of poisoning by mistakenly taking the veterinary drug norfloxacin. China Mod Doctor. 2008;46(13):137.
Wu SY. A case of benign intracranial hypertension caused by ciprofloxacin. Journal Of HuBei Minzu University(Medical Edition) 2001;18(3):21.
Lotti T, Mirone V, Imbimbo C, Russo A. Ciprofloxacin in the treatment of urinary tract infections. J Int Med Res. 1987;1(4):240–44.
Ouni B, Fathallah N, Slim R, Brahim A, Ben Salem C. Anaphylactic shock secondary to oral ofloxacin administration with cross-reactivity to levofloxacin and ciprofloxacin. Therapie. 2018;1(6):555–56.
Silverstein BE, Morris TW, Gearinger LS, DeCory HH, Comstock TL. Besifloxacin ophthalmic suspension 0.6% in the treatment of bacterial conjunctivitis patients with Pseudomonas aeruginosa infections. Clin Ophthalmol. 2012;6(1):1987–96.
Auerbach JS, Hom J. Ciprofloxacin-induced immunoglobulin A disease. Am J Emerg Med. 2010;1(5):641.
Dhavaleshwar A, Nayak V, Hande M, Pai R. Topical moxifloxacin-induced toxic epidermal necrolysis and Stevens-Johnson syndrome. J Postgrad Med. 2019;1(2):125–26.
Dubini M, Marraccini P, Pignatti P. Multiple drug allergy: a case of anaphylaxis to levofloxacin but tolerance to ciprofloxacin. Ann Allergy Asthma Immunol. 2016;1(5):465.
Jacobs JC Jr, Shea KG, Oxford JT, Carey JL. Fluoroquinolone use in a child associated with development of osteochondritis dissecans. BMJ Case Rep. 2014;2014:bcr2014204544.
Knorr JP, Moshfeghi M, Sokoloski MC. Ciprofloxacin-induced Q-T interval prolongation. Am J Health Syst Pharm. 2008;1(6):547–51.
van den Oever HL, Versteegh FG, Thewessen EA, van den Anker JN, Mouton JW, Neijens HJ. Ciprofloxacin in preterm neonates: case report and review of the literature. Eur J Pediatr. 1998;1(10):843–45.
Erdem G, Staat MA, Connelly BL, Assa'Ad A. Anaphylactic reaction to ciprofloxacin in a toddler: successful desensitization. Pediatr Infect Dis J. 1999;1(6):563–64.
Moffett BS, Rosenstein BJ, Mogayzel PJ Jr. Ciprofloxacin-induced renal insufficiency in cystic fibrosis. J Cyst Fibros. 2003;2(3):152–4.
Dawson PA, Emerson JA. Compartment syndrome secondary to antibiotic use: a case report. PM and R. 2014;1:S268–9.
Wildenbeest JG, Said I, Jaeger B, van Hest RM, van de Beek D, Pajkrt D. Neonate with Mycoplasma hominis meningoencephalitis given moxifloxacin. Lancet Infect Dis. 2016;16(11):e261–6.
Ramesh M, Parthasarathi G, Mohan B, Harugeri AB. Sparfloxacin induced toxic epidermal necrolysis. Indian J Dermatol Venereol Leprol. 2003;69(3):235–6.
Ji YY, Lu ShG. Pipemidic acid caused increase of intracranial pressure in 2 cases. Academic J Chin PLA Med School. 1991;02:105.
Gao LP. The therapeutic effect of ciprofloxacin on neonatal meningitis caused by gram-negative bacteria. World Notes Antibiot. 1995;03:205–6.
Jiang M, Li ChJ. A case of extrapyramidal reaction caused by breast milk intake of levofloxacin. Chin J Misdiagn. 2007;7(12):2929.
Hu HSh. A case report of infant methemoglobinemia caused by oral administration of ciprofloxacin hydrochloride. J Jinggangshan Med Coll. 1998;(Z1):100.
Yue ShL, Jiang YX, Li G, Zhang HX, Li LJ. Analysis of 1 case of infant Stevens-Johnson syndrome caused by moxifloxacin sodium chloride injection. China Pharm. 2020;23(9):1811–2.
Gao QN. Adverse reactions of norfloxacin. Clin Med. 2000;04:60–1.
Okubo T, Ito A, Takahashi H, et al. Clinical evaluation on the usefulness and safety of norfloxacin in a twice-a-day regimen against upper respiratory tract infections. Jpn J Antibiot. 1987;1(5):983–94.
Nakano E, Ichikawa Y, Ishibashi M, et al. Clinical experience of enoxacin in the treatment of nongonococcal urethritis. Hinyokika Kiyo. 1987;1(2):305–309.
Lauwers S, Vincken W, Naessens A, Pierard D. Efficacy and safety of pefloxacin in the treatment of severe infections in patients hospitalized in intensive care units. J Antimicrob Chemother. 1986;17 Suppl B:111–15.
Sun Ch, Li Y, Ma ShL. Clinical analysis and literature review of levofloxacin in the treatment of neonatal burkholderia cepacia infection. J Pediatr Pharm. 2020;26(11):31–4.
Stahlmann R, Lode H. Safety considerations of fluoroquinolones in the elderly: an update. Drugs Aging. 2010;27(3):193–209.
Ball P, Stahlmann R, Kubin R, Choudhri S, Owens R. Safety profile of oral and intravenous moxifloxacin: cumulative data from clinical trials and postmarketing studies. Clin Ther. 2004;26(7):940–50.
Adefurin A, Sammons H, Jacqz-Aigrain E, Choonara I. Ciprofloxacin safety in paediatrics: a systematic review. Arch Dis Child. 2011;96(9):874–80.
Bradley JS, Kauffman RE, Balis DA, et al. Assessment of musculoskeletal toxicity 5 years after therapy with levofloxacin. Pediatrics. 2014;134(1):e146–53.
Sheng ZhG, Li QQ, Peng ShQ. Research progress on cartilage toxicity and mechanism of quinolone antibacterial drugs. Chin Pharm J. 2007;10:723–5.
Sendzik J, Lode H, Stahlmann R. Quinolone-induced arthropathy: an update focusing on new mechanistic and clinical data. Int J Antimicrob Agents. 2009;33(3):194–200.
Yee CL, Duffy C, Gerbino PG, Stryker S, Noel GJ. Tendon or joint disorders in children after treatment with fluoroquinolones or azithromycin. Pediatr Infect Dis J. 2002;21(6):525–9.
Sansone JM, Wilsman NJ, Leiferman EM, Conway J, Hutson P, Noonan KJ. The effect of fluoroquinolone antibiotics on growing cartilage in the lamb model. J Pediatr Orthop. 2009;29(2):189–95.
Zabraniecki L, Negrier I, Vergne P, et al. Fluoroquinolone induced tendinopathy: report of 6 cases. J Rheumatol. 1996;23(3):516–20.
Alves C, Mendes D, Marques FB. Fluoroquinolones and the risk of tendon injury: a systematic review and meta-analysis. Eur J Clin Pharmacol. 2019;75(10):1431–43.
Salvi AE, Metelli GP, Bosco A, Berizzi A, Hacking SA, Cantalamessa A. Spontaneous bilateral Achilles tendon rupture in a patient treated with oral levofloxacin. J Orthop Traumatol. 2007;8(2):86–90.
van der Linden PD, van Puijenbroek EP, Feenstra J, et al. Tendon disorders attributed to fluoroquinolones: a study on 42 spontaneous reports in the period 1988 to 1998. Arthritis Rheum. 2001;45(3):235–9.
Rose L, Coulter MM, Chan S, Hossain J, Di Pentima MC. The quest for the best metric of antibiotic use and its correlation with the emergence of fluoroquinolone resistance in children. Pediatr Infect Dis J. 2014;33(6):e158–61.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author reports no conflicts of interest in this work.
Funding
This work was supported by the Sichuan Province Science and Technology Plan Project (No. 2020YFS0035).
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent to publication
Not applicable.
Availability of data and materials
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Code availability
Not applicable.
Author Contributions
Siyu Li conceptualized and designed the study, conducted the systematic review, analyzed the data, drafted the initial manuscript, and reviewed and revised the manuscript. Zhe Chen conceptualized and designed the study and reviewed and revised the manuscript. Lingli Zhang conceptualized the study and reviewed and revised the manuscript. Zheng Liu, Yuqing Shi, Miao Zhang and Jiaqi Ni conducted the systematic review, including screening of abstracts and full text, extracting data and assessing study quality. As pediatric clinical experts, Liang Huang and Yu Zhu gave their clinical opinions in the study process and manuscript writing. Hailong Li, who specializes in statistics, participated in data processing and analysis. All authors critically revised the manuscript for important intellectual content, approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, S., Chen, Z., Huang, L. et al. Safety of Quinolones in Children: A Systematic Review and Meta-Analysis. Pediatr Drugs 24, 447–464 (2022). https://doi.org/10.1007/s40272-022-00513-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-022-00513-2